Sleep deprivation is usually present in residents during their training programme. The purpose of our study was to analyse the cognitive performance of a group of orthopaedic residents before and after 24h on call duty.
MethodsWe include orthopaedic residents and their cognitive functions were evaluated by the following tests: Continuous Performance Test (CPT 2), Digit Spam (Versión 5), 1 letter Fonologic Fluence y Pasat Test. All the tests were done after a sleeping period at home of at least 6h and after being on call (sleeping less than 3h).
ResultsNineteen residents were included in the study. The median age was 27±1.89 and 15 were male. The mean hours of sleeping at home was 6.5 (range 6–8) and after on call duty was 1.5 (range 0.5–3). Statistical difference were found in CPT 2 test en terms of correct answers (p=0.007), omissions (p=0.004) and perseverations (p=0.036). No significant differences were found in the other tests.
ConclusionSleep deprivation after 24h on call duty affects cognitive performance of orthopaedic residents, increasing the number of errors and omissions.
La falta de sueño suele presentarse regularmente en los residentes de especialidades médicas durante su proceso de formación. El objetivo principal de nuestro estudio fue comparar las funciones cognitivas basales y después de la privación de sueño posguardia en residentes de ortopedia y traumatología.
Material y métodosSe han incluido en el estudio a residentes de ortopedia y traumatología y se evaluaron la atención y funciones cognitivas a través de los siguientes test: Continuous Performance Test (CPT 2), Digit Spam Directo e Inverso (Versión 5), Fluencia Fonológica de 1 letra y Pasat Test. Todas las evaluaciones basales se realizaron después de un periodo de descanso en domicilio de al menos 6h y las evaluaciones posguardia fueron realizadas en residentes con menos de 3h de sueño.
ResultadosDiecinueve residentes fueron incluidos en el estudio. La edad media de la serie fue de 27±1,89 años y 15 eran de sexo masculino. El promedio de horas de sueño basal fue de 6,5h (rango 6–8) y posguardia de 1,5h (rango 0,5–3). En la evaluación de CPT2 se han encontrado diferencias significativas en el número de aciertos (p=0,007), número de omisiones (p=0,004) y perseveraciones (p=0,036) a la consigna planteada. No hemos encontrado diferencias significativas en los otros test.
ConclusiónLa falta del sueño posterior a una guardia de 24h de ortopedia y traumatología afecta la atención de los residentes, aumentando el número de errores y omisiones.
Sleep deprivation induces attention deficit, low cognitive performance and deterioration in the capacity for exercising judgement.1,2 This situation regularly occurs for residents of medical specialities who throughout their training have to perform obligatory and active 24h on call duty followed by the continuation of regular employment duties the following day. Long working days combined with a lack of sleep in medical training programmes have come under scrutiny for several years.3 The strongest arguments against them are medical errors and putting the patient's safety at risk.4 As a result, in USA and Europe the maximum working hours per week have been stipulated for all residents.5,6 However, many people consider that the working hour restriction in the resident programmes has damaged the professional training of residences with no benefit for patients.7–10
Over the last decade different studies have attempted to determine whether a lack of sleep affects the performance of residences and health professionals.11–13 It has been reported that being on call duty without being able to sleep increases the number of errors made and reduces the individual's capacity to pay attention and react to levels which are comparable to a 0.5g/l alcohol/blood level.14 Many articles published over the last few years analyse the relationship between a lack of sleep and cognitive and practical abilities in different residencies (internal medicine, family care, general surgery or cardiovascular surgery) in USA and Europe. Few records exist, however, with regards to orthopaedic residents in particular.11–13
The main objective of our study was to compare baseline cognitive functions and post on call duty sleep privation functions in orthopaedic residents.
Materials and methodsFirst, 2nd, 3rd, and 4th year resident orthopaedic students from a single university hospital in Argentina (South America) were included in the study. They met the following inclusion criteria: they performed active 24h on call duty and their post on call duty activity continued for at least 8h. The following residents were excluded from the study: those who refused to participate in the process or who did not sign the informed consent form, those who presented with insomnia or sleep disturbances, those under medical treatment with drugs which could interfere in their normal circadian cycle (anti-histamines, muscle relaxants, tranquilisers, antidepressants), those who were pregnant or had visual or hearing difficulties which would have complicated taking the tests. All participants were not allowed to have consumed energy drinks, carbonated drinks or coffee 5h prior to the assessment. The 1st and 2nd year residents were classified as junior residents and the 3rd and 4th years as senior residents.
Each orthopaedic on call duty of the hospital comprises: a medical specialist in orthopaedics, a senior resident and 2 junior residents. They are in charge of outpatient consultations (on average 150 consultations), control hospitalised patients (on average 45 patients) and perform surgical activity on demand. All activity performed by junior residents is supervised by a senior resident and medical specialist.
Assessment of performance regarding attention and cognitive functions were included in the following tests: Continuous Performance Test (CPT 2), Digit Span Direct and Reverse (version 5) Test, 1 letter Phonological Fluency Test and the Pasat Test. All tests were performed on Thursdays and Fridays between 13.00 and 15.00h by two separate assessors specialised in neuroscience (C.F. and L.Z). The order of the baseline and post on call duty assessments was randomly defined for each participant so as not to be biased towards either of the 2 phases and therefore avoid any previous knowledge of the tests. All the baseline assessments were made following a period of rest at home of at least 6h and post on call duty assessments in residents with less than 3h of sleep. The components of the neurocognitive assessments are described below.
CPT 2: assesses overall attention capacity, impulsivity and inhibitory response of participants. It provides information on the capacity for sustained attention (ability to focus on a task for a prolonged period of time), flexibility and selective attention (ability to respond to the presence of relevant/discriminatory stimuli). This is a computerised, individually administered test with presentation of letters on the screen (one per time) for 15min. The participant's task will be to press the space bar (only once) of the keyboard as fast as possible each time a letter appears on the screen and not press it when the letter “X” appears. As the exercise progresses the time of letter presentation also varies. Scores are given for correct moves, omission errors (not clicking on the space bar when required to), commission errors (pressing the space bar when not required) and perseverations (pressing the space bar more than once, not realising the error). Scores range from 0% to 100%, with 0% a perfect result and 100% the worst result possible.15,16
Digit Span Direct and Inverted response (version 5): this is used to measure sustained attention and the working memory. Participants are presented with a series of digits (for example, “8.4”) which they have to repeat in the order in which they appear. They begin with two series of 2 digits, then two series of 3 digits and so on successively until one series fails. In a second instance the participant is asked to repeat the sequences again but this time in reverse order to which they hear them, thus increasing the number of digits. The number of correct sequences repeated by each participant is collected.17
Phonological Fluency Test (one letter): this assesses the speed of processing verbal information. The subject is asked to say the greatest number of words beginning with a certain letter for 1min, omitting names and word groups. The number of correct words is counted. If the letters “F”, “S” or “A” were used by this sample, these were varied for the baseline and post on call duty test to prevent any learning effect.18
Pasat Test: this test combines assessment of two cognitive components, working memory and the speed of processing auditory information, in addition to mathematical calculation skills. The test requires the use of sound reproduction. The subject is informed that they will hear a series of digits of a number which will be presented to them every 3s. They must listen for the first two digits, add them up and give an answer. When they hear the following number they must add it to the one they have just heard previously. They will continue adding the following number to the previous one. They will not be asked to give a total accumulative number, but the sum of the two numbers which are consecutively given. At least one practice number will be given prior to performing the complete test.19
The differences between the baseline scores and the post on call duty scores were compared with the t test for the paired data. A lineal regression model of random effects with random origin for estimating a measure of association between the scores and on call duty was used, considering the natural grouping of the measurements of the same individual. The model co-efficients was presented with their 95% confidence intervals. Statistical analysis was made using version 12 STATA software.
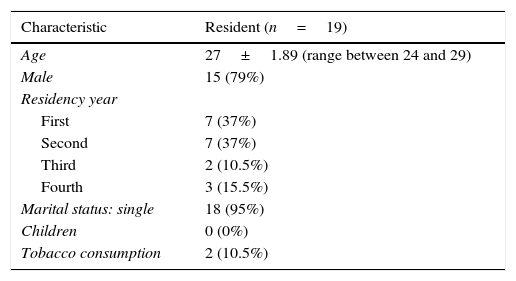
ResultsOut of a total of 37 orthopaedic residents from the university hospital, 19 were included in the study. The mean age of the series was 27±1.89 (range 24–32h) and 15 were male. The average hours of baseline sleep (at home) was 6.5h (range 6–8h) and post on duty call was 1.5h (range 0.5–3) (Table 1).
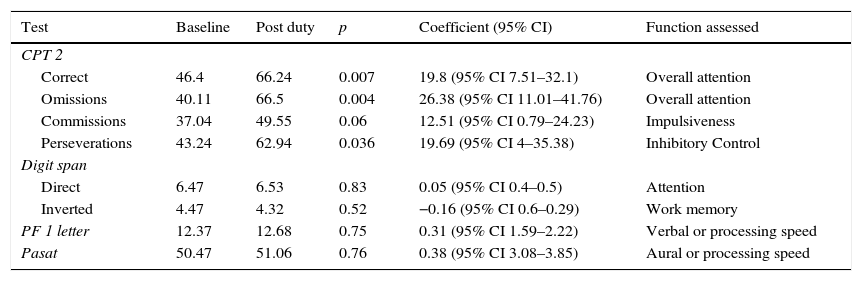
The successes obtained under baseline conditions of appropriate sleep and after an active on call duty of 24h in the residents analysed demonstrated a statistically significant differences in favour of the first group (p=0.007). The number of omissions to the test put forward was considerably higher when the test was made after on call duty (p=0.004), as was the number of perseverations (p=0.036). We did not record any differences regarding commission errors (p=0.06) (Table 2).
Results of the neurological test in baseline state (>6h sleep) and post duty (<3h sleep).
| Test | Baseline | Post duty | p | Coefficient (95% CI) | Function assessed |
|---|---|---|---|---|---|
| CPT 2 | |||||
| Correct | 46.4 | 66.24 | 0.007 | 19.8 (95% CI 7.51–32.1) | Overall attention |
| Omissions | 40.11 | 66.5 | 0.004 | 26.38 (95% CI 11.01–41.76) | Overall attention |
| Commissions | 37.04 | 49.55 | 0.06 | 12.51 (95% CI 0.79–24.23) | Impulsiveness |
| Perseverations | 43.24 | 62.94 | 0.036 | 19.69 (95% CI 4–35.38) | Inhibitory Control |
| Digit span | |||||
| Direct | 6.47 | 6.53 | 0.83 | 0.05 (95% CI 0.4–0.5) | Attention |
| Inverted | 4.47 | 4.32 | 0.52 | −0.16 (95% CI 0.6–0.29) | Work memory |
| PF 1 letter | 12.37 | 12.68 | 0.75 | 0.31 (95% CI 1.59–2.22) | Verbal or processing speed |
| Pasat | 50.47 | 51.06 | 0.76 | 0.38 (95% CI 3.08–3.85) | Aural or processing speed |
CPT 2: results are expressed in scores of 0–100, with 0 being the best possible result and 100 the worst; PF: phonological fluency; CI: confidence interval.
Digit Span Test: no significant differences were found between the two groups analysed (p=0.83) (Table 2).
Pasat Test: no significant differences were present between the two groups analysed (p=0.76) (Table 2).
Phonological Fluency: the average results of the series analysed were: 12.37 words under baseline conditions and 12.68 under post on call duty conditions. No significant difference was found (p=0.75) (Table 2).
DiscussionLong working days, 24h duty and obligation to continue working until the following day were and continue being a constant in many orthopaedic residents’ programmes. The said rules are accepted as normal by residents, ward doctors and those in charge of training programmes. Different approaches and changes in this regard have been put forward in countries such as USA, which, from 2003 stipulated a maximum of 30h of continuous work or a maximum of 80h weekly for all residents, or Spain, where a weekly schedule of not over 48h was fixed for associates and doctors in training.5,6 However, sleep deprivation and the tiredness factor in doctors who are in training continues to be an issue under debate.
Sleep deprivation undoubtedly leads to alterations and affects our neurocognitive abilities.20 The alteration of the circadian rhythm and lack of rest affects concentration, memory and psychomotor activity, increasing the possibility of committing errors.21 Results in the medical area are, however, contradictory. On the one hand, Arnedt et al. reported that the response capacity of resident paediatricians after a 24h on call duty is comparable to having blood/alcohol of 0.5g/l and Barger et al. concluded that the long working days for residents increased the number of errors, complications and lapses in attention.13,14 Furthermore, Rothschild et al. did not find a higher percentage of complications in the procedures performed after having performed resident duty hours of 24h.4
The results of the lack of sleep, particularly in surgical performance (psychomotory activity) are even more ambiguous. Sharpe et al. reported that there were no differences in terms of complications and readmissions of patients to surgery of those performed by doctors who had been on duty for 24h the previous night.22 However, Obrien et al. demonstrated a lack of cognitive response of orthopaedic surgeons who had slept less than 4h, without specifying whether this would have repercussions on the surgical output.10
We decided to analyse the response to the lack of sleep specifically in a group of orthopaedic residents of a single university hospital. The authors were unaware of any report in Spain regarding the effect of sleep deprivation in the orthopaedic residents. A total of 19 residents were assessed, 14 were in their first and second years (1st and 2nd year) and 5 were in their last years (3rd and 4th year). We found a difference regarding attention, impulsiveness and inhibitory response when the residents were assessed after an active duty of 24h through the CPT2 test. We found that sleep had increased the number of errors and omissions recorded which corresponded to a lack of attention due to lowered information processing. The increase in the number of perseverations is usually due to a lack of inhibition, associated with a change in the frontal lobe, which in this case was physiological due to a lack of sleep. Regarding commissions (pressing the space bar more times than was necessary), no significant differences were found. This pattern is generally more common in compulsive disorders than in those associated with attention deficit. In addition, the Digit Span, PF and Pasat tests did not show up any differences, possibly due to the fact that the sensitivity of said assessments is lower in that of a healthy population.
Getting used to tiredness over time was reported, as was personal individual vulnerability due to lack of sleep.21 The effect of becoming used to this could be regarded as represented in the results obtained from different years, but our sample size does not permit us to reach any definitive conclusions in this regard. A larger sample-sized study thus needs to be carried out to obtain more definitive results.
Due to logical ethical questions it has not been possible to carry out prospective, randomised and comparative studies on patients surgically treated by doctors who were well rested and those who had had less than 3h sleep. For this reason, tests were performed with simulators in different surgical specialties such as cardiovascular surgery, surgery of the thorax, abdominal surgery or laparoscopy.23–28 Outcomes are very different, with articles which describe sleep deprivation as a preponderant factor for a reduced psychomotor response and a higher rate of errors, whilst others find no difference whatsoever and some publications even consider this a positive factor.23,25–28
In 2014, a systematic review of 135 articles on working hours being restricted to 80h per week for residents was published, and concluded that no improvements were consistently associated with resident well-being, and that they had recorded a negative impact on the performance in certification exams.6 Analysis of the first group of surgical specialist residents who were trained with the new hour restrictions reduced their contact with patients and the time spent in surgery.7 Moreover, exhaustion and thoughts about giving up did not diminish even under the new paradigm of the working hour reduction.29 Residents of internal medicine, family care, paediatrics, general surgery and orthopaedics in the USA concluded that the working hour restrictions had not improved the level of attention or resident training.6–9 Specifically in the area of orthopaedics, a systematic review was published in 2015, which aimed at determining the effect of the working hour restriction on quality of life, patient safety, education and surgical abilities of residents. Although it is difficult to obtain a specific outcome, an improvement in quality of life (reduction in fatigue and increase in hours of sleep) was observed, but a reduction in the development of surgical skills was also noted.30 There is no doubt that the areas of “surgical faculties” is where the most negative effects were noted from timetable restrictions in residents’ training programmes.7,30,31 For this reason the European Union proposed the modification for surgical specialties, adding the “48+12” option. With this, 12h are added to the official timetable but are reserved for training activities, with no performing of night duty or routine work.19,32
We are aware of our study limitations with its small sample only from one university hospital, and no analysis of practical capacity, but we do however believe that the design and methodology of the study render our outcome valid in the little researched area of orthopaedic residents. We believe there is the need for several multicentre studies which include the objective assessment of medical practice outcome in order to observe the real effect of lack of sleep in this group of residents.
ConclusionLack of sleep after a 24h on call duty in orthopaedics affects residents’ attention, increasing the number of errors and omissions. However, seemingly, working memory and speed of procedure are not affected. We believe the right balance in residents’ programmes needs to be discussed between the authorities of the medical community, residents and educators, in order for patient safely and that of residents or be guaranteed, without their training being affected.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Albergo JI, Fernández MC, Zaifrani L, Giunta DH, Albergo L. ¿Cómo afecta la privación de sueño durante una guardia de 24 horas las funciones cognitivas de los residentes de ortopedia y traumatología? Rev Esp Cir Ortop Traumatol. 2016;60:113–118.