Coccydynia is a term that refers to pain in the region of the coccyx. Most cases are associated with abnormal mobility of the coccyx which may trigger a chronic inflammatory process leading to degeneration of this structure. Non-surgical management remains the gold standard treatment for coccydynia, consisting of decreased sitting, seat cushioning, coccygeal massage, stretching, manipulation, local injection of steroids or anaesthetics, and postural adjustments.
Materials and methodsA retrospective study of 23 patients who underwent treatment for coccydynia and failed to respond to conservative management. They were treated by radiologically guided infiltration of the ganglion blockade impar and/or caudal blockade with 1% lidocaine 60–80mg triamcinolone. Of these 23 patients, 21 were available for clinical review and completed a questionnaire giving their assessment of the effect of the infiltration of the ganglion impar block and/or caudal block.
ResultsGood results were obtained in 16 of the 21 patients with coccydynia due to trauma. In five patients the results were moderate or poor, although none described worse pain after the operation. They are no complications after the infiltration.
ConclusionGanglion impar block and/or caudal block offered satisfactory relief of pain in the majority of patients regardless of the cause of their symptoms.
La coccigodinia es un término referido al dolor en la región del cóccix. La mayor parte de casos se asocian a una movilidad anormal del cóccix que puede provocar un proceso crónico inflamatorio que conduce a la degeneración de esta estructura. El tratamiento conservador debe ser de elección en este cuadro, y puede consistir en terapias manuales (masajes, estiramiento, manipulación y postural) inyecciones locales de esteroides o anestésicos.
Material y métodosEstudio retrospectivo de una cohorte histórica de 23 pacientes con clínica de coccigodinia traumática sin respuesta a tratamiento médico. Se trataron con infiltración del ganglio impar y/o bloqueo caudal con lidocaina 1% y triancinolona 60–80mg bajo control radioscópico. De estos 23 pacientes, 21 estaban disponibles y completaron un cuestionario de evaluación del efecto de la infiltración del ganglio impar el bloque y/o el bloque caudal.
ResultadosSe consideraron excelentes los resultados obtenidos en 16 de los 21 pacientes con coccigodinia traumática. En cinco pacientes los resultados eran moderados o pobres, aunque ninguno describiera aumento o empeoramiento del dolor después de las infiltraciones. El procedimiento no se asoció a complicaciones mayores.
ConclusiónEl bloqueo del ganglio impar y/o el bloqueo caudal conllevó un control del dolor coccígeo en la mayoría de pacientes.
Although the aetiology of coccydynia is varied, the most common mechanism for its occurrence is trauma due to falls in a sitting position, with immediate onset of clinical signs, but cases have been reported with a latency period of months and years.1 Other causes triggering this condition are the period of expulsion in childbirth,2 infections and tumours in the perianal region,3 disk hernias, inflammatory disease of the pelvis, dysplasias, etc. In consequence, the treatment of coccydynia should not be initiated until its aetiology has been determined.
In most cases, the pathogenesis of coccydynia involves a subluxation with a hypermobile coccyx and it has been posited that this pathological instability may give rise to chronic inflammatory changes perpetuating the condition.4
The cornerstones for treatment are based on analgesic therapy and on three major techniques, namely infiltrations, manipulation and surgery. Infiltrations of the ganglion impar and caudal blocks are the techniques most often used, with good results in 75% of cases. Resection of the coccyx has a poor reputation and is aimed solely and exclusively at invalidating instabilities not relieved by other means.
The rationale for the present paper is based on a major absence of medical evidence on the best ways to treat this entity. The goal of this article was to assess the effectiveness of treatment for coccydynia refractory to conventional medical treatment through infiltration of the ganglion impar and, in cases where there was no response to this block, to assess the effectiveness of the association of the blocking of the ganglion impar and caudal blocking with local anaesthetics and triamcinolone.
Materials and methodsRetrospective observational study of a historic cohort carried out during the years 2007–2010 at a Chronic Pain Unit, assessing the post-treatment outcome after infiltration with local anaesthetics and corticosteroids in patients with chronic post-traumatic pathology of the coccyx. The inclusion criteria were for all patients diagnosed as having chronic coccydynia with a history of trauma and who received multiple medical treatments without improvement in their clinical condition. The exclusion criteria were the presence of uncontrolled metabolic and degenerative diseases, complicated deep infections and the refusal to accept the technique.
During the study period, infiltration of the ganglion impar was performed on 23 patients suffering from chronic coccydynia with a history of trauma and resistant to conventional medical treatment. In cases of absence of response to blocking of the ganglion impar (8 cases), a second infiltration was applied to the ganglion impar, on this occasion associated with a caudal block. Monitoring continued for a period of 6 months, with a self-assessment survey responded by 21 patients. The mean age of the cohort was 42.45±9.94 years (range: 24–68 years). Sixteen cases (76.19%) were female. Seven cases presented a body mass index greater than 30.
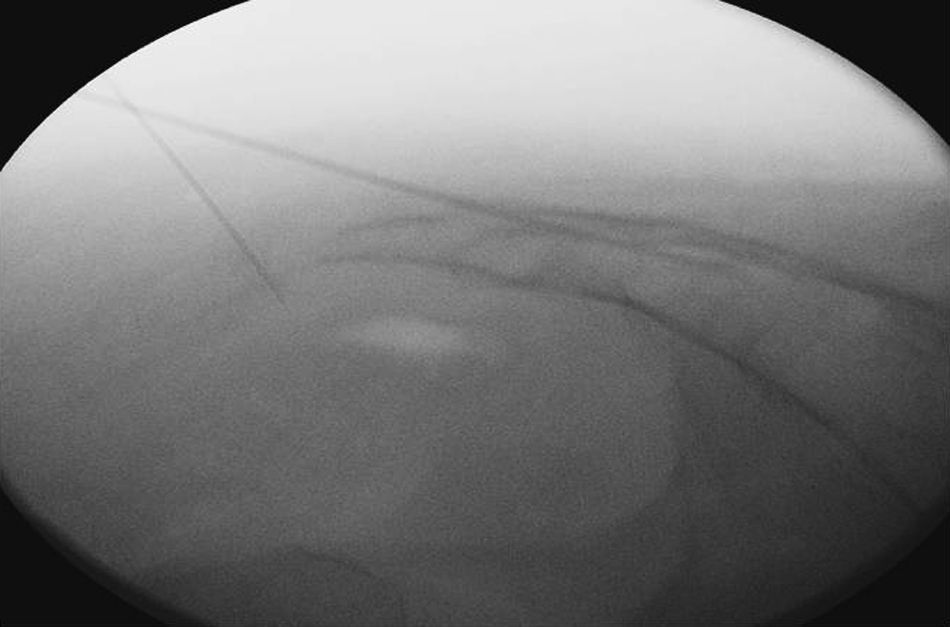
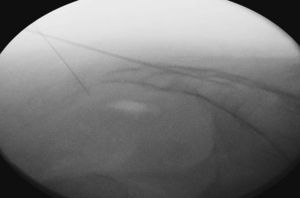
The procedure was performed under local anaesthesia and anaesthetic monitoring under aseptic conditions and in pronus decubitus position with a pelvic pad to apply diagnostic blocking of the ganglion impar and/or caudal under radioscopic control with local anaesthesia and triamcinolone. Radiology was used to locate the sacral hiatus and an 18G Tuohy needle was inserted perpendicularly to the sacral plane until it bumped into the anterior cortical plane, at which point, after withdrawing the needle a few millimetres, we angled it horizontally and advanced cephalically to traverse the sacrococcygeal ligament and locate the peridural space. After verification by fluoroscopy and prior injection of contrast, we applied aspiration and confirmed the absence of emergence of cerebrospinal fluid or blood. For the blocking of the ganglion impar or ganglion of Walther, the punctures were made through the sacrococcygeal ligament or a transdiscal approach through a coccygeal disc (Figs. 1 and 2). The sacrococcygeal ligament and the coccygeal discs were located using the image intensifier in a lateral projection. This projection also helped locate the first or second coccygeal disc. The procedure was performed with 22G spinal needles or 18G Tuohy needles. If the technique is performed with radiofrequency, a 14G introducer is used to insert the 15cm radiofrequency needles with a 10mm active tip. To traverse the sacrococcygeal membrane and the sacrum, it is necessary to use an 18G metallic needle with a stylet. The puncture is effected at all times with the image intensifier in lateral position, so that the view of the sacrum and coccyx are as anatomical as possible and the rectal ampulla can be viewed. The tip of the needle must pass beyond the sacrum and this must be verified radiologically and using contrast (Iohexol®). Once the needle has passed beyond the anterior face of the coccyx, contrast is injected and a check is made that it spreads into the right place (Fig. 2). Particular caution must be taken when inserting the needle and it should be done gradually under radioscopic control, as the safety space to the posterior rectal wall is 5mm. Occasionally, the manoeuvres for the injection of contrast may cause a reproduction of the pain habitually felt by the patient. However, this latter sign does not seem very reliable.
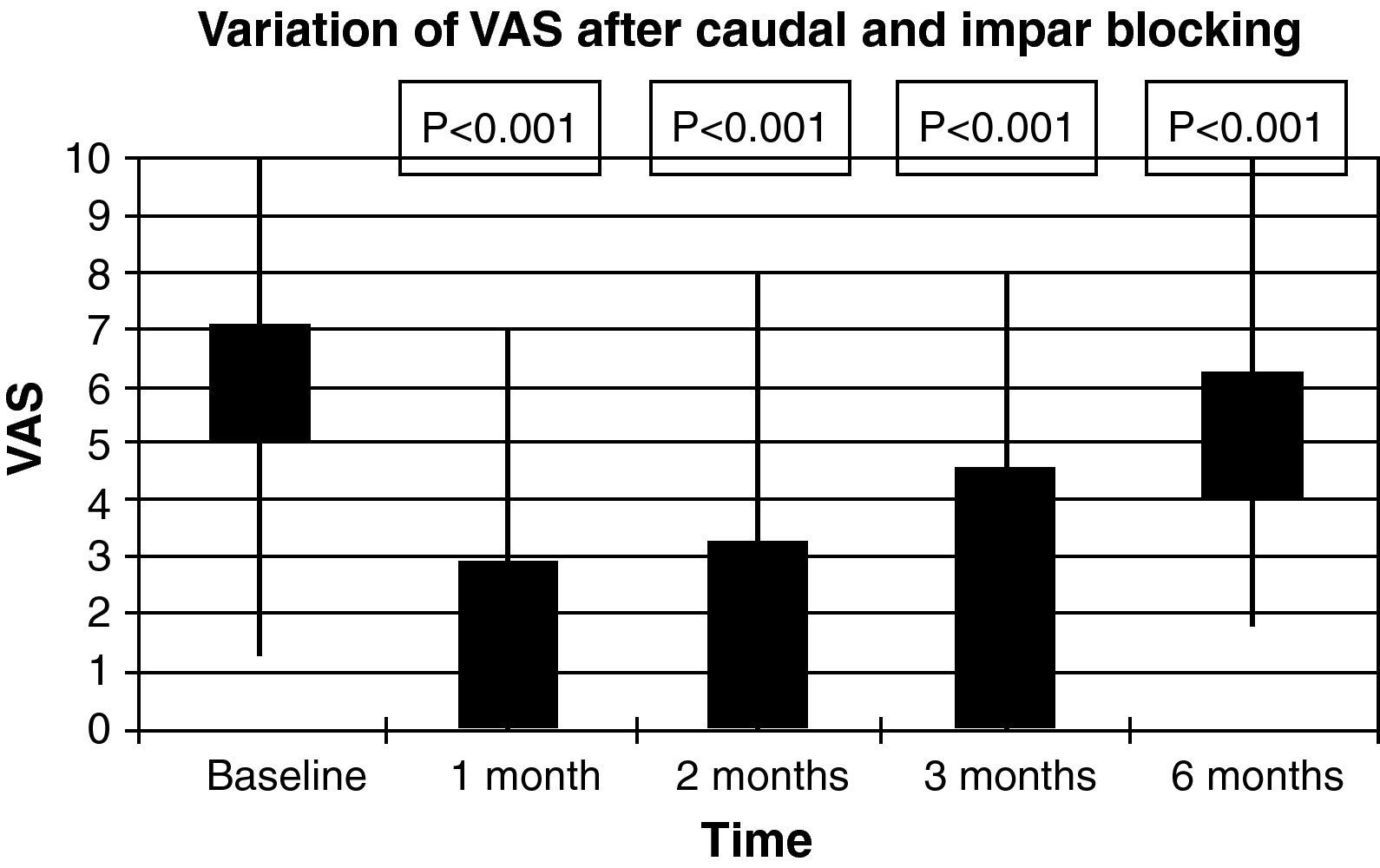
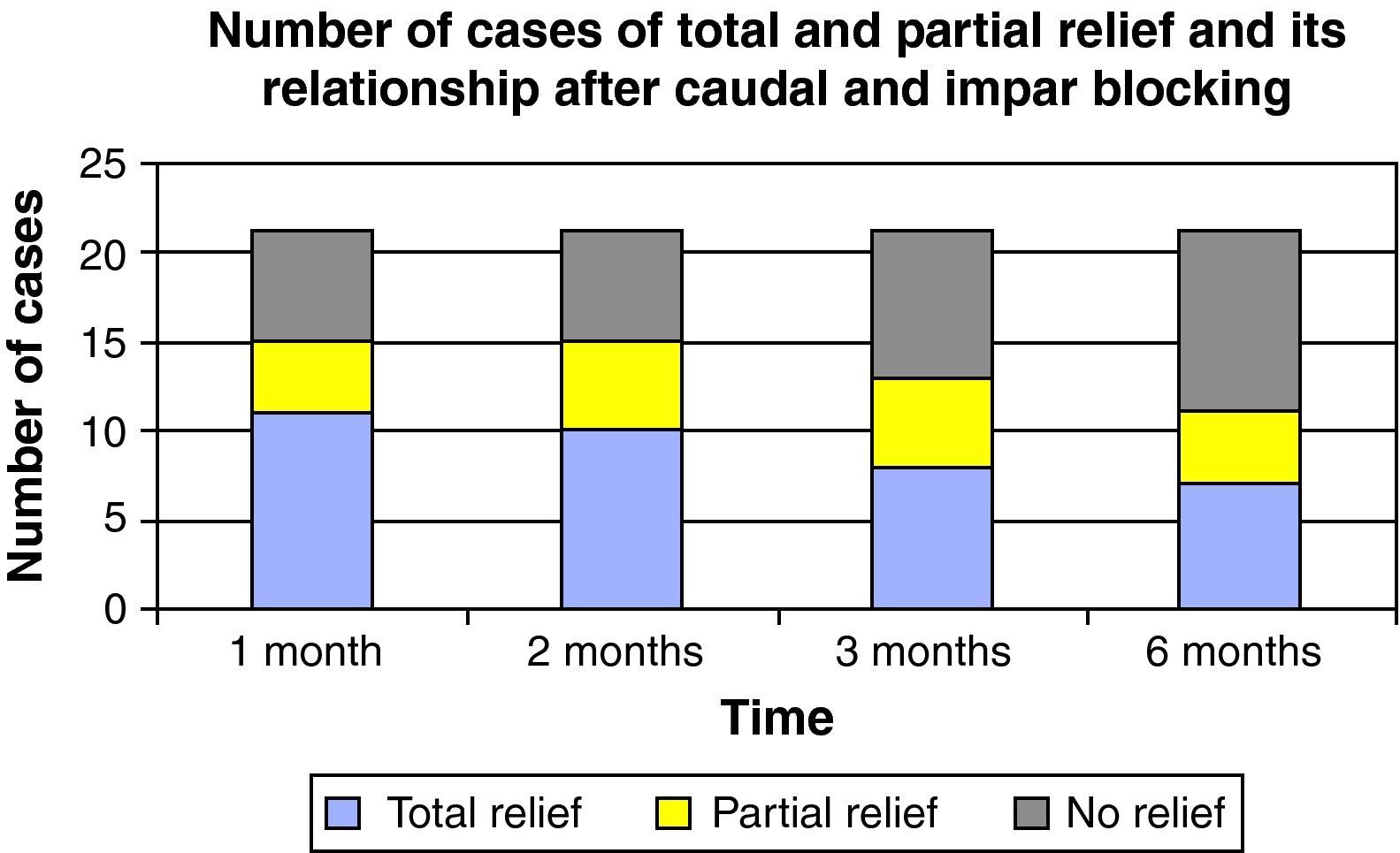
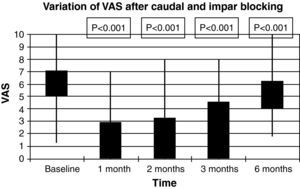
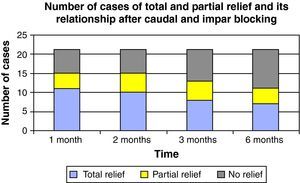
All patients presented a history of trauma in the coccygeal area and the examinations carried out were complementary X-rays, pain assessment using the visual analogue scale (VAS) at baseline and at 1, 2, 3 and 6 months, analgesic treatment using the WHO analgesic ladder, inability to engage in daily activity and gainful employment as well as the demographic variables of age, gender and body mass index. The efficacy of the caudal and ganglion impar blocking was assessed by a reduction of more than 50% in the baseline value, and complete relief or an excellent outcome was recorded when the reduction in the VAS was greater than 80%; if it was between 50% and 80%, it was recorded as partial relief or moderate outcome; when the VAS reduction was less than 50%, it was listed as a poor outcome or technical failure; the time until reappearance of the pain was also recorded.
A descriptive bivariant analysis was conducted using Student's t-test (quantitative variables) or the χ2 test (qualitative variables). The ANOVA test with Bonferroni's correction was used for multiple comparisons. Values of P<0.05 were considered to be statistically significant. The data were processed using release 7 of the Stata programme (Stata Corp., Collage Station, TX).
ResultsTechnical success in the performance of the ganglion impar block was 100%, without the onset of major complications and all the patients tolerated the procedure. The effectiveness of the ganglion impar block in reducing VAS scores to at least 50% was 60.94% (13 cases). In the eight cases that did not respond to the initial infiltration, a further infiltration of the ganglion impar and caudal block was carried out, with a positive response being obtained in 37.50% (3 cases). The mean time until the onset of pain and inclusion on the interventionist protocol at our unit was 17.22±14.21 months, with no statistically significant differences being found between the success of the technique and the time until onset of the coccydynia (p=0.502).
The diagnosis was fundamentally based on clinical presentation and a simple sacrococcygeal X-ray; in five cases, an axial magnetic resonance tomography was taken of the area in two cases. No dynamic radiology study was performed in any case. No patient was included on the first step of the WHO analgesic ladder; 80.95% of patients were regularly taking non-steroidal anti-inflammatory drugs associated with tramadol or codeine. The rest of the cohort presented a medical prescription for low-dose major opiates. The mean VAS score prior to the procedure was 7.09±1.3. VAS one month after the block was 2.95±2.23, after 2 months, it was 3.27±2.20, after three months it was 4.59±2.19, while it was 6.23±1.81 after 6 months (please see Fig. 3 and the statistical significances), con statistically significant differences in every month in the study (p<0.005). Fig. 4 shows the results (total, partial and no relief) for the months in the study. In one case, the procedure was followed by complete but transient relief lasting for a few hours; in this patient, blockage was repeated with thermocoagulation by radiofrequency. Six months after the infiltration, 6 patients required repetition of the technique due to re-appearance of the pain. The reduction in analgesic medication was observed in 76.20% of the cohort. In no case was any side effect observed, except for pain at the puncture site lasting for 2–3 days after the procedure.
There is considerable consensus that treatment in the face of coccydinia must be conservative, based on non-steroidal anti-inflammatory drugs for at least two months, and, following any subsequent failure in this treatment, it must be based on a variety of manual techniques and infiltration with steroids.5 The manual techniques to treat coccydynia are quite diverse, such as massage of the elevator muscles of the anus, manipulation of the coccyx in extension, stretching of the elevator muscles of the anus and the sacroiliac muscles; these techniques are applied rectally with an average of 3–4 sessions administered over two weeks. Interventionist treatments consist essentially in interspinal or caudal epidural infiltrations and peri-coccygeal infiltrations.6,7 In our health area, there is no specific clinical unit or department taking charge of this pathology. Patients arriving at the Pain Unit for this condition have mostly not received any manual rehabilitation therapies, their imaging studies are varied and treatment with a range of different analgesics has tended to last for months or years. The creation of a clinical route and a multidisciplinary unit comprising traumatologists, rehabilitation experts, surgeons and anaesthesiologists might entail better attention and a considerable saving in health-care expenditure.
The ganglion impar or ganglion of Walther is a single retroperitoneal structure located at the level of the sacrococcygeal union (paravertebral sympathetic chain), innerving the perineum, the distal rectum, the anus, the terminal urethra, the vulva and the distal third of the vagina. The first person to describe the blocking of this structure was Plancarte in 1990 through the anococcygeal ligament.8 Nebad used curved needles to facilitate the approach.9 The sacrococcygeal route was described by Wemm.10 This block has been used successfully in cancer-related perineal pain refractory to conventional therapy.8
As used in our paper, infiltration with local anaesthetics and corticosteroids to block the ganglion impar in traumatic coccydynia resistant to treatment with various analgesics has a high success rate. Symptomatic relief after 6 months was achieved in 60% of patients, and this increased to 76% when a joint block was applied to the ganglion impar and the caudal ganglion. These data are in line with those reported in the series by Datir,6 Plancarte,8 Rubio11 and Abejon.12 Plancarte et al. suggested that those patients with unsatisfactory outcomes, whether through incomplete relief of pain or the presence of residual somatic symptoms after a first infiltration of the ganglion impar, should be treated with epidural infiltration of steroids through the peridural caudal route and blocking of the ganglion impar. Of the eight cases with poor response to the initial block, this strategy enabled us to obtain a significant improvement in three of them.
The origin of coccyx pain is not well understood and, although it is not infrequent for it to co-exist with a history of trauma, the cause of the pain is unknown in approximately one third of cases. It is postulated that the key to its aetiology lies in an excessive instability of this bone that favours inflammation in the ligamentous and muscular structures related to this bone,13 so an infiltration of corticosteroids may lead to spectacular improvement in this condition. The results of infiltration with local anaesthetics and corticosteroids may take some time to have an effect, so any evaluation must be made 2 to 3 weeks after the procedure. This instability may be triggered by a prior trauma in the area or other local causes. A discreet trauma-related periostitis usually co-exists alongside fibrositis and traumatic myositis of the peri-coccygeal musculature. Dislocations represent the traumatic lesion par excellence, originated by repetitive microtraumas, arthritis in the sacrococcygeal joint and postural defects in the lumbosacral column. The diagnostic algorithms and treatment differ from one centre to another.14
The time elapsing between the trauma and the onset of pain in the coccyx seems to be determinant: if it is less than three months, the responsibility of the trauma is highly likely.15 Through a logistic regression analysis, the study by Mitra et al.16 found a relationship between infiltration with steroids and the time to onset of coccygeal pain and thus that patients with a clinical situation lasting for more than six months respond worse to the therapy. In our series, our data disagree with the existence of that time-based relationship.
In our cohort, obese patients with a body mass index of more than 30 and with coccydynia were considered to have a traumatic aetiology as the mere fact of sitting down is viewed as repetitive micro-trauma.15 We did not find any statistically significant differences in the obesity variable with respect to the efficacy of the different blocks in those cases with a clear history of trauma.
This block occasionally produces temporary relief and it is frequent to have to repeat the technique, thus in our experience it was necessary to apply a second infiltration session in 7 of the 16 patients who initially responded, 6 months after the first, due to re-appearance of pain in the coccyx, although all the patients reported that the pain was less intense that what they had suffered prior to the previous infiltration. Various published article find that approximately one third of patients may present a further acute situation after several months free of any symptoms. In the event of recurrence of pain, it is logical to propose a second infiltration and, if this is effective for longer than the first, the treatment has good potential to cure the patient. The overall efficacy of the infiltration treatment is 76% two months after the procedure and diminishes to 52% after six months. Therefore, we consider this conservative treatment, based on the blocking of the ganglion impar and caudal block, to be the first-line therapy in cases of chronic coccydynias with poor response to analgesic and anti-inflammatory treatment. In refractory cases or when the improvement is very temporary, this block has been applied with neurolytic substances or thermocoagulation using radiofrequency with good results. In these cases, patients must be informed of the possibility that permanent areas of anaesthesia and hypoaesthesia may appear. Local or regional neuromodulation techniques (implantation of stimulators in the posterior cords and spinal perfusion techniques) have also been used.
Radioscopic control is imperative for performing this infiltration, but several authors nowadays use imaging methods such as ultrasonography and axial tomography.17,18 This block is considered to be easy to perform, technically simple and safe, with the most feared complication of these techniques is the accidental perforation of the rectum. In successful cases of ganglion impar blocking after diagnostic blocks with local anaesthetics and the re-appearance of the pain, the group of Agarwal-Kozlowski et al.18 carried out chemical ablation with ethanol without noteworthy complications using puncture guided by axial tomography, reporting excellent results, but we are of the opinion that, before indicating this technique with neurolytic agents, a repeat attempt should be made with corticosteroids and/or radiofrequency.
Surgical treatment consists in partial or total coccigoidectomy, a radical procedure that must be reserved only for those cases where all the previous treatments fail and there is no well-founded hope of improvement by other means.19 Trollegaard et al.20 published a series of 41 patients after surgery in cases refractory to medical treatment, with excellent results in pain control (in excess of 80%) without any major complications. The study by Hodges et al.5 differs from the previous one, finding a high incidence, estimated at 27%, of infections in the surgical area.
ConclusionConservative treatment for traumatic coccydynia based on a multimodal strategy using analgesics and anti-inflammatory drugs, associated with blocking of the ganglion impar and occasionally supplemented by peridural caudal blocking, may be highly effective in cases of hard to control pain. In cases where the pain re-appeared, consideration must be given to applying a permanent block of the ganglion impar using radiofrequency or neurolytic agents.
Level of evidenceLevel of evidence II.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Cortiñas Sáenz M, et al. Infiltración del ganglio impar y caudal en el manejo de la coccigodinia traumática rebelde al tratamiento analgésico convencional. Rev Esp Cir Ortop Traumatol. 2011;55(5):340–5.