To evaluate the results of the uncemented meridian femoral stem in primary total hip arthroplasty.
Material and methodA prospective study was performed on 109 cases, with a mean age of 64 years (range: 30–80) and follow-up of 6.5 years (range: 5–12). The study included, a clinical assessment using the scales of Harris and Merle D’Aubigné, quality of life with SF-12 and WOMAC, radiographic results and analysis of complications.
ResultsThe Harris and Merle D’Aubigné scales increased from 40.9 to 86.7 and from 8.4 to 10.5, respectively, with 81% satisfactory functional results. Thigh pain (17%) was associated with insufficient femoral filling. There are 7 femoral fractures during surgery, associated with an age greater than 65 years and a metaphyseal adjustment >90%, and 3 of which had to be revised. There were another 5 stems with unstable fibrous fixation, associated with insufficient metaphyseal and/or diaphyseal adjustment, and all with an indication for revision. The mean survival of the stem at 7.5 years due to aseptic causes was 94.7%.
Discussion and conclusionsExcessive filling carries a risk of metaphyseal fractures during surgery, which could affect the results. Insufficient filling can compromise the secondary fixation of the stem.
Evaluación del vástago no cementado Meridian en prótesis total de cadera primaria.
Material y métodoEstudio prospectivo de 109 casos con una edad media de 64 años (rango: 30–80) y un seguimiento de 6,5 años (rango: 5–12). Valoración clínica con escalas de Harris y Merle D’Aubigné, calidad de vida con SF-12 y Womac, resultados radiográficos y análisis de complicaciones.
ResultadosLa escala de Harris y Merle D’Aubigné se incrementó de 40,9 a 86,7 y de 8,4 a 10,5, con el 81% de resultados funcionales satisfactorios. El dolor en muslo (17%) se asociaba a insuficiente relleno femoral. Hubo 7 fracturas femorales intraoperatorias asociadas a una edad mayor de 65 años y un ajuste metafisario >90%, debiendo revisarse tres. Hubo otros 5 vástagos con fijación fibrosa inestable asociados a un ajuste metafisario y/o diafisario insuficiente, y todos con indicación de revisión. La supervivencia del vástago a 7,5 años por causas asépticas fue del 94,7%.
Discusión y conclusionesEl excesivo relleno tiene el riesgo de fractura metafisaria intraoperatoria pudiendo afectar a los resultados. El insuficiente relleno puede comprometer la fijación secundaria del vástago.
Although not free from complications,1 total hip prosthesis has been shown to be an effective treatment with satisfactory results. For this reason, various systems have had frequent changes in design or materials and innovations tending to improve the results of arthroplasty. The problems associated with uncemented stems included fractures of the calcar, varus positioning and thigh pain.2,3 Femoral PCA stems (Porous Coated Anatomic, Stryker, Mahwah, USA) have been used since 1983 and another three successive versions4 were designed through their study: PCA series E, Meridian and Citation. The difference in uncemented Meridian stem design and technique was that the preparation of the femur was done with independent milling for the metaphysis and the diaphysis. The theoretical goal was to improve the fit in order to favour osseointegration at that level, combined with a diaphyseal adjustment to provide primary mechanical stability and enable integration through progressive transmission of metaphyseal-diaphyseal loads.5 To this was added the aim of providing increased offset with respect to other models,6 with the equally theoretical advantage of improving the abductor forces by increasing the lever arm of the musculature.
The goal of this study has been to analyze the clinical and radiological results of this stem model, with a post-operative follow-up of at least 5 years. The hypothesis consisted of a consideration that, by facilitating both the metaphyseal and the diaphyseal adjustments, the gradual transmission of the forces from proximal to distal favoured osseointegration of the implant and reduced discomfort in the thigh.
Material and methodsThe prospective study was carried out in a cohort of 109 patients treated consecutively between December 1998, and January 2000, for primary total hip prosthesis (THP) using the uncemented Meridian femoral prosthesis (Stryker-Howmedica, Mahwah, USA). The project received ethical approval from the institution's CIRB and patients were furnished with information before giving their informed consent. The inclusion criteria were: adult age and painful degeneration of the hip that was a candidate for THP. There were no exclusion criteria other than a prior infection or a history of another ipsilateral intervention. No patients were found to meet the exclusion criterion. The mean age was 64 years (range: 30–80 years), with 64 women (58.7%) and 45 men (41.3%). There were no cases of bilateralism and the right side was affected in 64 cases (58.7%) and the left side in 45 (41.3%). The mean weight was 81.3kg (range: 67–105kg), mean height was 166cm (range: 158–185cm) and the mean body mass index was 27.3kg/cm2 (range: 24.1–36.9kg/cm2). The diagnosis was primary arthrosis in 88 cases (80%), post-traumatic in 13 cases (12%), arthrosis with signs of avascular necrosis of the femoral head in 4 cases (4%), rheumatoid arthritis in 3 cases (3%) and pathological fracture of the neck of the femur due to intraosseal lipoma in a 35-year-old male (1%).
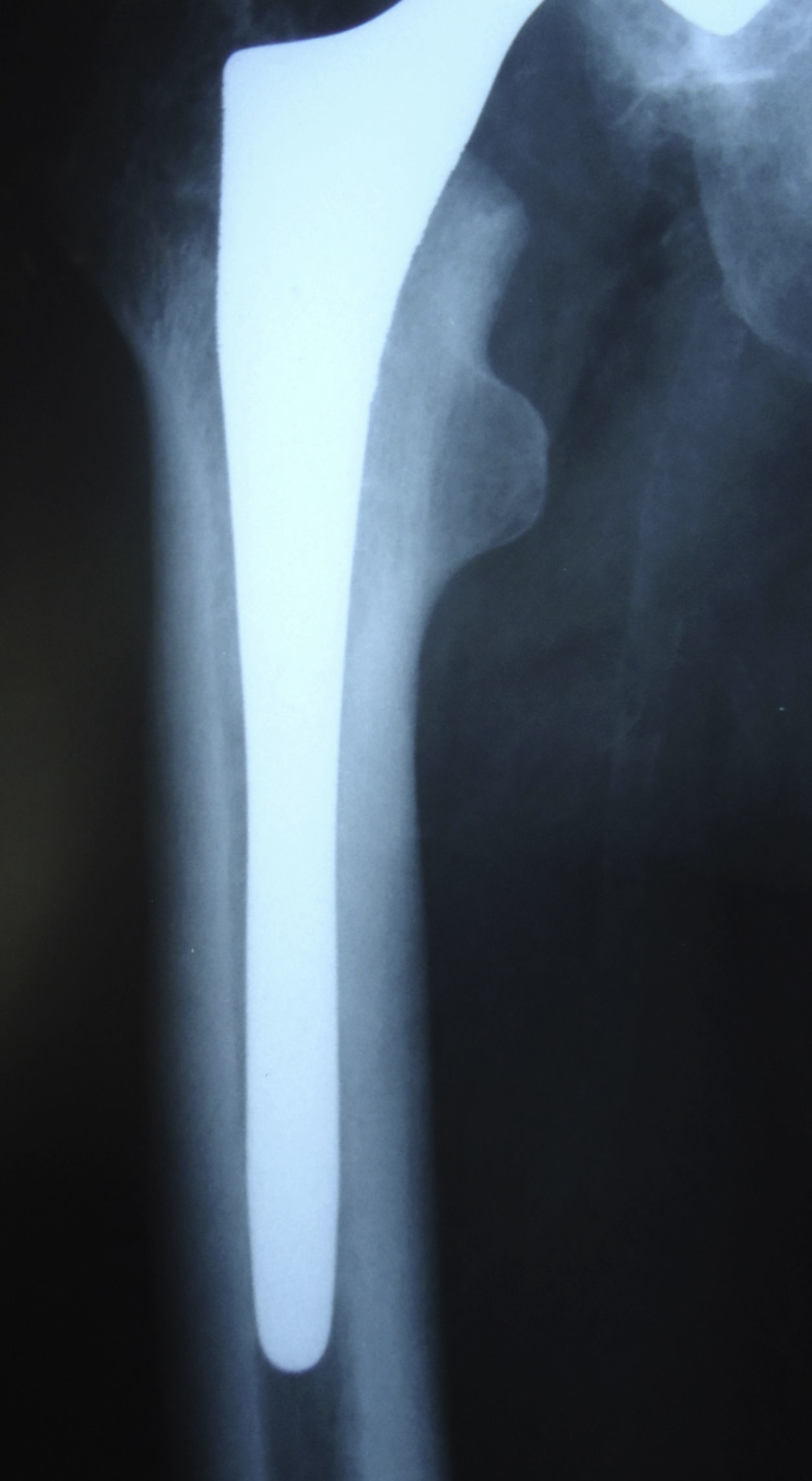
Design of the implantThe uncemented Meridian stem (Stryker-Howmedica, Mahwah, USA) was manufactured in chrome-cobalt alloy. The metaphyseal portion had a trapezoidal cross-section with blunt edges, porous coating and hydroxyapatite on the proximal circumference. The diaphyseal portion was straight with longitudinal grooves and polished in order to reduce the growth of cortical bone around it and so diminish the formation of a pedestal; its tip was rounded and slotted to reduce its rigidity. It had a neck at 132° to lateralize the prosthesis with a view to favouring joint mechanics and reduce the wear on the polyethylene. The offset varied from 25 to 67mm, depending on the size of the stem. The instrumentation used has been described elsewhere.6 First of all, sequential diaphyseal milling was performed until a fit was obtained, the size of which corresponded to a range of metaphyseal reamings; the size of the last ream used to ensure a adequate proximal fit that defined the size of the definitive stem.
ProcedureThe surgical procedures were performed by three surgeons. All the cases were operated on in the theatre with laminar flow and spinal anaesthesia was used with Hardinge's modified lateral approach. In all cases, a Meridian stem (Stryker-Howmedica) was used with an uncemented hemispherical Vitalock acetabulum (Stryker-Howmedica), made from titanium with a porous coating and the possibility of screwing. At that time, our centre routinely used complementary fixation with two screws, applied to 98 cases (90%) of this cohort. The insert was made from high molecular weight polyethylene without any bulges and was sterilized using gamma rays. The head of the femur was made from chrome-cobalt, with a diameter of 28mm. All of them received prophylactic antibiotics (1g IV of cephazolin prior to surgery and then three other doses every 8hours) and anti-thromboembolic medication (subcutaneous low molecular weight heparin for up to 30 days following the procedure) as per the standard protocol. Post-operative progress was similar, with most patients being allowed to sit up after 24hours and rehabilitation beginning on the second day of weight-loading with a walking frame, except in the case of calcar fracture, in which case weight-loading was deferred for one month, and in the two cases of fracture of the major trochanter when it was deferred for two months.
EvaluationIn all cases, clinical and radiographic assessments were made before and after surgery and after 3 and 6 months, one year and then annually for a minimum of 5 years. The evaluation was made by the surgeon in question using two scales. Using the Harris scale,7 results were classified as excellent (90–100), good (80–89), so-so (70–79) or poor (69 or less). On the Merle D’Aubigné and Postel scale,8 results were either excellent (11–12), good (9–10), so-so (8) or poor (7 or less). Thigh pain was categorized as absent, slight, moderate or severe, following the same criterion as for the pain variable on the Harris scale. Post-operatively from the sixth month on, a subjective evaluation was conducted using the SF-12 general quality of life questionnaire (physical and mental sections)9 and the specific Womac questionnaire10 for lower limbs (with a positive score), as well as a visual analogue scale (VAS) for satisfaction ranging from 0 to 10.
The radiographic evaluation was standardized using an anteroposterior projection under load and an axial projection of the hip.
At the femoral level, the proximal fill was defined11 by the ratio between the width of the stem and that of the medullary canal on the upper edge of the lesser trochanter, classified as satisfactory if equal to or greater than 80% on the anteroposterior plane and 70% in the axial plane, and unsatisfactory if it was less. The diaphyseal fill was calculated at 2cm proximal to the tip of the stem with the same criteria. A stem was considered to have subsidence when the distance between the tip of the trochanter major and the upper external metaphyseal edge of the stem had increased by more than 5mm on the final radiography with respect to that of the third post-operative month. The presence of remodelling factors, such as calcar resorption, cortical hypertrophy or formation of a pedestal, was recorded as were the weld points, radiotransparent lines or osteolysis, as per the areas defined by Gruen et al.12 In line with Engh et al.,13 femoral fixation was classified as stable with osseointegration, stable with fibrous or unstable fixation, considered to be when there were radiotransparent lines larger than 2mm thick in the porous proximal area, subsidence of more than 5mm or a change of position of more than 3° in the stem. For peri-prosthetic femoral fractures, the Vancouver classification,14,15 specific for intra-operative fractures, was used.
At the acetabular level, the acetabular abduction angle was evaluated. Variation in the position of the acetabular component was assessed in the last X-rays in comparison with the third post-operative month, following the measurements described by Martell et al.16 Migration was considered to exist if the centre of rotation varied horizontally or vertically by more than 3mm or if there was a variation of more than 5° in the acetabular abduction angle. The presence of radiotransparent lines or osteolysis was recorded in accordance with the three areas of DeLee and Charnley.17 Following González Della Valle,18 the acetabular component was considered to be loosened if there was migration, complete radiolucence of more than 1mm or osteolysis covering at least one area.
Statistical analysisThe SPSS 15.0 computer software package was used. To assess the statistical relationships between qualitative variables, the chi square test and Fisher's exact test were used, whereas Student's t test and the Mann–Whitney U test were used for continuous variables. For correlations, Spearman's test was used. In order to calculate the survival analysis using the Kaplan–Meier method, the endpoint considered was surgical revision or unstable fixation. Values of p equal to or less than 0.05 were considered significant.
ResultsAll patients were available for post-operative follow-up for a minimum of 5 years. At the last assessment, the mean follow-up was 6.5 years (range: 5–12 years). The mean score on the Harris scale increased (p=0.01) from 40.9 (range: 22–62) points before the operation to 86.7 (range: 31–100) points after it, with 60 results (55%) of excellent in the final assessment, 34 (31.2%) of good, 2 (1.9%) were so-so and 13 (11.9%) poor. Using the Merle D’Aubigné scale, it increased (p=0.01) from 8.4 (range: 2–8) points pre-operatively to 10.5 (range: 4–12) at the last assessment, with a categorization of functional results significantly similar (p=0.001) to that obtained using the Harris scale. There was a significant relationship between the need for surgical revision and the score on the scales from Harris (p=0.01) or Merle D’Aubigné (p=0.02). Thigh pain was absent in 91 patients (83.5%), was mild and occasional in 11 (10.1%), moderate in 3 (2.7%) and severe in 4 (3.7%). Cases with moderate or severe pain were significantly associated (p=0.001) with an insufficient femoral fill or unstable stem. Cases with osseointegration or stable fibrous fixation did not report any pain in the thigh or this was mild and occasional.
At the last assessment, the quality of life under the SF-12 questionnaire was 64.6 (range: 32–71) for the physical factor and 71.2 (range: 35–79) for the mental factor. Using the Womac questionnaire, the mean value was 39.7 (range: 5–48). With the satisfaction VAS, the mean value obtained was 7.7 (range: 1–10). A significant relationship (p=0.001) was found between the subjective quality of life assessments and the objective hip scales.
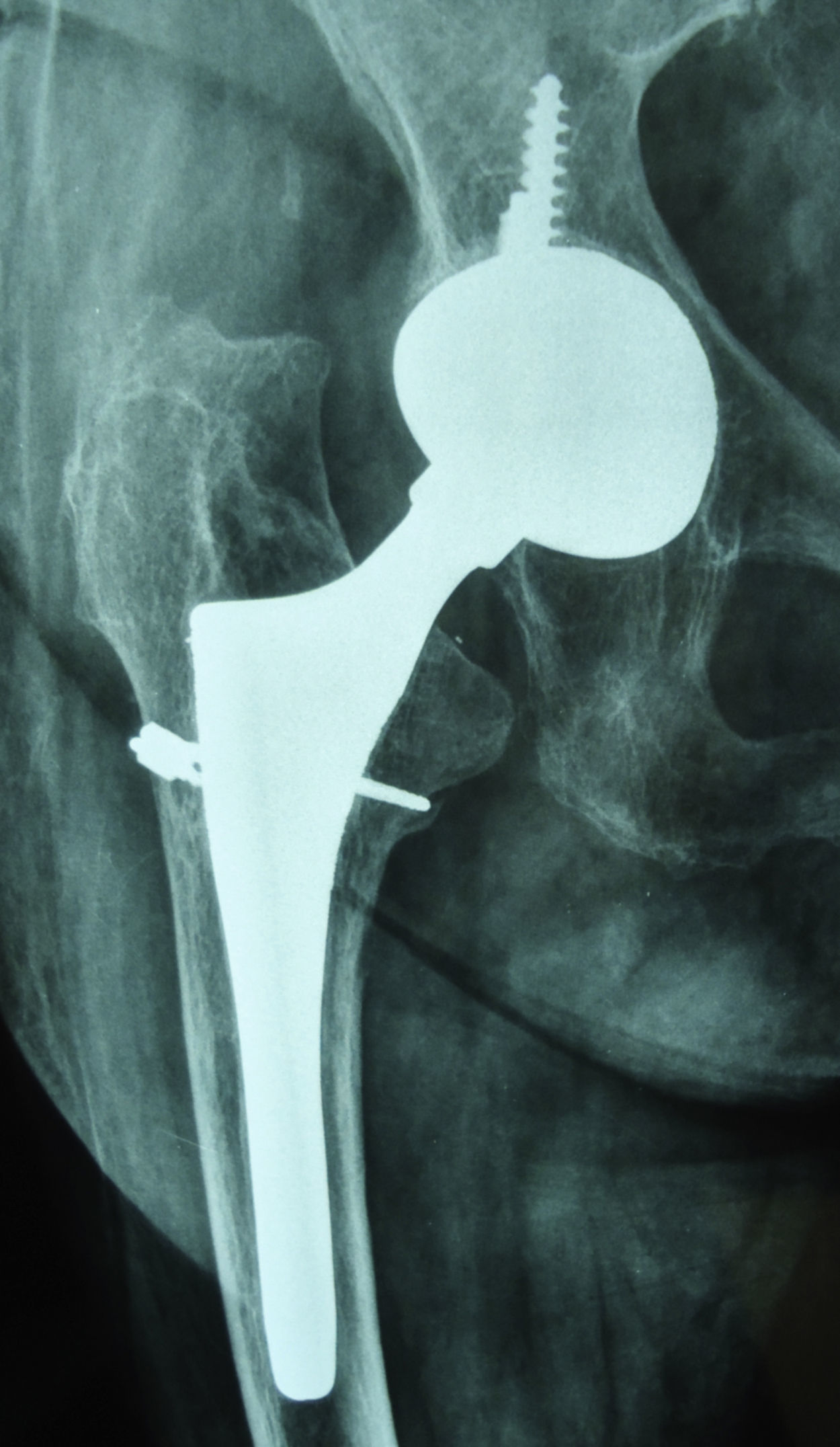
Intra-operative complications included 7 femoral fractures (6.4%). In two cases, these were type A2 (incomplete longitudinal fractures of the trochanter major, without displacement), detected on the post-operative X-ray, and load-bearing was not allowed for 60 days. In one of these fractures, the final functional outcome was good with osseointegration of the stem. In the other A2 case, secondary displacement of the fracture occurred with luxation of the prosthesis after 10 weeks, requiring revision for bone synthesis using a plate, without replacement of the stem as it was considered stable; although the stem remained stable in the last X-ray assessment after 9 years, it was classified as a poor result because of the revision. The other 5 fractures were type B2 (linear at the level of the calcar, with moderate displacement) all were detected intra-operatively and treated with wire cerclage. Of these 5, the functional outcome was not affected in three cases (one excellent, two good), with two stems presenting osseointegration and one stable fibrous fixation. The other two cases of B2 fracture presented subsidence of the stem 9 months (Fig. 1) and 11 months after surgery, with both requiring revision of only this component and considered as poor outcomes. Intra-operative fractures occurred in 6 patients with primary arthrosis and one with rheumatoid arthritis, all over 65 years of age (range: 65–79) and, in the 5 cases detected during surgery, the fracture produced during insertion of the definitive stem. We found a significant relationship between age over 65 years and appearance of fracture (p=0.001).
Another 5 patients had unstable stems, with radiotransparent lines >2mm in the polished portion (areas 2, 3 and 5), all with insufficient femoral fill and stable acetabulum. In two of these, revision was performed on only the stem 67 and 69 months after the primary surgery and those two were considered poor outcomes. The other three patients with aseptic loosening of the stem, detected after 70, 74 and 81 months, rejected further surgery despite moderate pain, but were considered as failures and therefore as poor results.
There were another two cases of deep infection requiring revision of both components at two different times after 3 and 11 months; their outcomes were considered poor.
In the series as a whole, there were 86 stems with osseointegration (78.9%) (Fig. 2), 16 with stable fibrous fixation (14.6%) and 7 unstable fibrous fixation (6.5%). There was deficient metaphyseal femoral fill in 11 cases (10.1%) and diaphyseal femoral fill in 9 (8.2%). Insufficient fill was significantly related to the presence of moderate or severe pain in the thigh (p=0.001) and to unstable femoral fixation (p=0.03). In the 7 cases with intra-operative fracture, metaphyseal femoral fill was greater than 90%. Over the whole series there was no significant relationship between femoral fill (satisfactory or unsatisfactory) and the occurrence of fracture (p=0.32), but when we consider the sub-group with metaphyseal fill >90%, we find a significant relationship (p=0.001) between this kind of fill and the occurrence of fracture. The signs of bone remodelling found were atrophy of the calcar in 19 cases (17.4%), cortical hypertrophy in 12 cases (11.1%) and incomplete pedestal in 10 cases (9.2%).
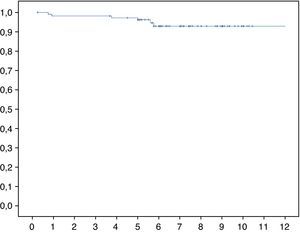
With respect to the acetabular component, the mean value of the acetabular abduction angle at the last radiographic assessment was 44° (range: 40–48°). No acetabulum had changed position with respect to the X-ray three months after the surgery. There were 3 acetabula with signs of aseptic loosening (2.7%), in all of which only this component was revised 42, 65 and 78 months after the primary surgery.
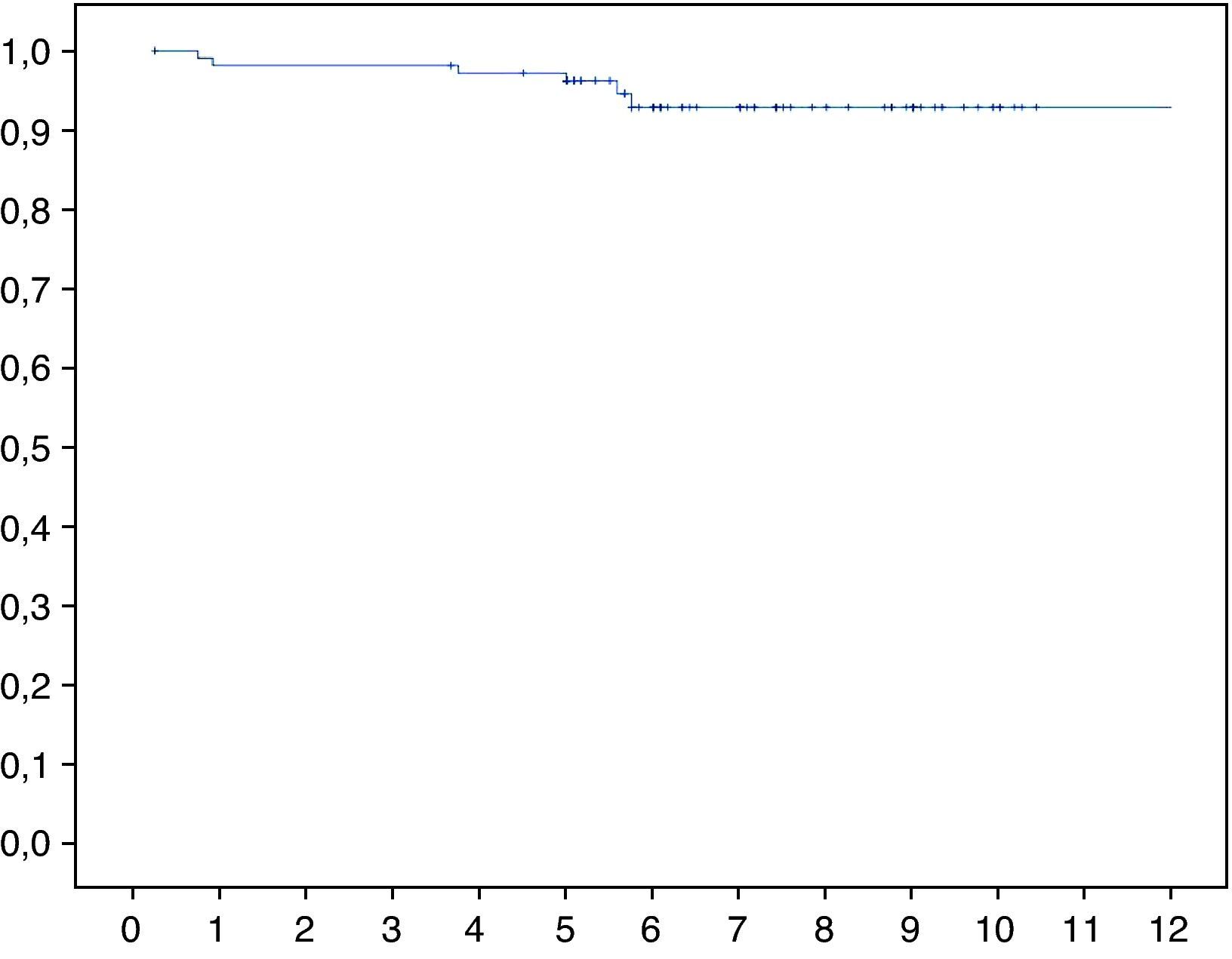
Considering the 4 cases of femoral revision and the three who rejected revision surgery, the mean survival of the stem after 7.5 years for aseptic causes was 94.7% (95% CI: 93–98) (Fig. 3).
DiscussionThe purpose of our study was fundamentally focused on the clinical and radiographic outcomes of the femoral component in the medium and long term, using the uncemented Meridian stem with both metaphyseal and diaphyseal adjustment.
The limitations of the present study include heterogeneity in the primary diagnosis and the participation of multiple surgeons. Nonetheless, the diagnosis does not seem to have had any influence on the poor outcomes as most of these occurred in cases of primary arthrosis, the most frequent aetiology in our series (80%). The influence of the surgeon is difficult to assess, although all three had a long experience in hip surgery.With uncemented systems, the function of femoral reaming is to adapt the bone bed to the ideal size of the stem so as to have intimate contact and immediate stability, as well as to favour secondary fixation by osseointegration. In many of the systems, reaming is only metaphyseal, transferring most of the loads to this area. With the Meridian system and design, milling is also diaphyseal, in an attempt to achieve primary mechanical stability on the diaphysis to facilitate integration of the metaphyseal portion, as well as gradual diaphyseal fixation with progressive load transfer from proximal to distal.6 Satisfactory long-term outcomes have been described with the PCA anatomical stem, with only metaphyseal reaming,3,4 but there are few studies using the evolved Meridian stem.5,6,18–20
In our work, satisfactory functional results were 81% of the cases, less than the 88–98% reported in other series with the same stem.5,6,19 Furthermore, we found a 94.7% survival of the stem after 7.5 years for aseptic causes, somewhat lower than in those other series (97–100%). Most of the unsatisfactory outcomes in our series were due to pain in the thigh or the need for revising the stem. We found 7 patients (6.4%) with moderate or severe thigh pain, a level similar to other series6,19 and associated, as with other authors,6 to insufficient femoral fill.
In the present study, there were 7 stems with mechanical failures (6.4%), higher than the 0–3% of other series5,6,19 with the same stem. Two of our cases were due to subsidence of the stem in patients who had suffered an intra-operative fracture treated with cerclage. The other 5 were stems with unstable fibrous fixation, associated with insufficient femoral fill, with an under-dimensioned stem. This association was also reported by other authors5 using the Meridian stem in the medium and long term, although some6 found cases of stable fibrous fixation still with insufficient fill, albeit with only three years’ follow-up.
The most frequent complication in our series was intra-operative fracture with 7 cases (6.4%), of which 5 were at the level of the calcar on insertion of the definitive stem. All except one occurred after the learning curve of the first 30 prostheses. With other models of uncemented stems, the incidence of intra-operative femoral fractures is highly variable,21–23 from 3 to 20%, with most of them at the calcar level and with scant displacement.24 Using the Meridian stem, the intra-operative femoral fracture rates5,19,20 range from 2 to 9.5%. In the literature, the aetiology of intra-operative femoral fractures is multifactorial,25 including patient-related factors such as poor bone quality, implant design or instrumentation and also factors relating to the surgical technique such as over-dimensioning of the stem. In our series, we found that all the fractures occurred in patients aged over 65 years, although on its own this does not seem to justify the fracture insofar as most studies on uncemented hip arthroplasties are performed on elderly individuals, habitually with a scant incidence of fractures. The other risk factor for fracture in our series was metaphyseal fill of more than 90%. The only comparative study found on intra-operative fractures with Meridian stems21 report that there was no relationship between the occurrence of a fracture and age, prior diagnosis, bone quality or the geometry of the proximal femur; albeit not significant, however, they did find a tendency to fracture in cases with the greatest metaphyseal fill by the stem. They suggest that the surgeon's attempt to obtain the best possible adjustment may lead to the choice of an oversized stem, although they also say that it might be due to the design of the reams or the implant. Using the Meridian stem in short-term series,6,21 the results were not affected by fracture, whereas in the medium- and long-term series5,19 they found subsidence and stem revision in 12 to 15% of fractures. The mechanical outcome of the stem following an intra-operative fracture is controversial. With other stem models, some authors25 report that the results are not affected if the fracture is treated immediately with cerclage, while others26,27 indicate that subsidence is frequent in the event of a fracture, even if it is treated with cerclage or is free from displacement.
In our study, the aseptic survival of the Meridian stem in the medium- and long-term was somewhat lower than that in other series, with a similar level of intra-operative fractures and a higher rate of mechanical failures. With the limitations inherent to our study, the outcomes with this stem model suggest that the search for an excessive metaphyseal adjustment between the bone bed and the stem presents risk of intra-operative fracture of the femur, potentially affecting the results. On the other hand, the achievement of an insufficient metaphyseal and/or diaphyseal adjustment may affect secondary stability of the stem in the medium or longer term.
Level of evidenceLevel of evidence IV.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors will declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Sanz-Reig J, et al. Resultados del vástago femoral no cementado Meridian. Estudio prospectivo de 109 casos. Rev esp cir ortop traumatol. 2011;55(5):346–351.