To create an experimental structural scoliosis model in mice to evaluate the efficacy of shape-memory metals to gradually correct the deformity over time.
Materials and methodsExperimental scoliosis was generated in 3 week-old mice by means of a suture between the left scapula and pelvis for 8 weeks. They were then randomized into two groups: a control group, in which the suture was cut, and another, in those that also had a Nitinol straight memory-wire implant fixed to the column. Serial X-rays were performed to determine the efficacy of the Nitinol in the correction of the scoliosis. In a second time, the histological changes at apical vertical body level and the adjacent discs were evaluated pre- and post-correction.
ResultsA mean 81.5° kyphoscoliosis was gradually induced. In the control group, after cutting the suture, an initial reduction in the deformity was observed, but later it remained stable throughout the time (54° at two weeks). In the Nitinol group, a gradual reduction was observed in the scoliosis angle value, to a mean of 8.7° at two weeks. The curvature of the apical vertebral body and adjacent discs was partially corrected after two weeks of correcting the deformity.
ConclusionThis scoliosis model has demonstrated the efficacy of a straight Nitinol wire fixed to the spinal column in the gradual correction of kyphoscoliosis and in the changes in its adjacent structures.
Creación de un modelo experimental de escoliosis estructurada en ratas para evaluar la eficacia de los metales con memoria de forma para corregir gradualmente la deformidad a lo largo del tiempo.
Material y métodoSe generó una escoliosis experimental en ratas de 3 semanas mediante una sutura entre escápula y pelvis izquierdas durante 8 semanas, tras lo cual fueron aleatorizadas en 2 grupos: control, en los que se cortó la sutura, y nitinol, en los que además se implantó un alambre recto con memoria de forma anclado a la columna. Se realizaron radiografías seriadas para determinar la eficacia del nitinol en la corrección de la escoliosis. En un segundo tiempo, evaluamos los cambios histológicos a nivel del cuerpo vertebral apical y discos adyacentes pre y poscorrección.
ResultadosSe indujo una cifoescoliosis progresiva media de 81,5°. En el grupo control, tras cortar la sutura, se produjo una reducción inicial de la deformidad pero luego permaneció estable a lo largo del tiempo (54° a las 2 semanas). En el grupo nitinol se observó una reducción progresiva del valor angular de la escoliosis, hasta 8,7° de media a las 2 semanas. El acuñamiento del cuerpo vertebral apical y de los discos adyacentes se corregía parcialmente tras 2 semanas de corrección de la deformidad.
ConclusiónEn este modelo de escoliosis, un alambre recto de nitinol anclado a la columna ha demostrado eficacia para la corrección gradual de la cifoescoliosis, y de los cambios estructurales asociados a la misma.
Scoliosis is a complex deformity of the spine which often requires treatment in order to control its progression during growth. This treatment is mainly limited to the use of braces and surgical interventions. Treatment with braces is noninvasive and preserves the growth of the vertebral column, but has limited results for the control of the curve and a negative psychosocial impact which may affect compliance by patients.1–3 Surgical treatment through an instrumented spinal arthrodesis (or fusion) offers good results regarding correction of the deformity, but involves a highly invasive procedure, and entails risks associated with instantaneous correction of the deformity and the biomechanical alteration of a fused spine, since the loss of growth potential can lead to a significant reduction in thoracic height and affect lung development adversely. The disadvantages of the surgical treatment of scoliosis have promoted a growing interest in the development of new strategies for managing severe scoliosis in young children without resorting to spinal fusion. Techniques which do not involve fusion have theoretical advantages over vertebral arthrodesis, including the preservation of potential for spinal growth, mobility and function.4 They also achieve good clinical outcomes after the initial procedure and the first retensing procedures, but become less effective over time.5
Nitinol is one of the so-called “intelligent metals”. It is an alloy consisting of 50% nickel and 50% titanium, which has the properties of superelasticity (behaving like a spring) and shape memory (it can be deformed when cooled but will recover its original shape when heated). These properties of nickel–titanium alloys, along with their good biocompatibility make them interesting materials for novel applications in the biomedical field, especially for correcting deformities.6,7
The objective of this work is to open a line of research aimed toward avoiding the complications and morbidity associated with the current surgical treatment of scoliosis by using the properties of shape-memory metals. To this end we set 3 goals: (1) to create a structured scoliosis in the spine of experimental animals, based on a tested model; (2) to achieve a gradual correction of the previously created deformity through the implementation of a shape-memory wire; and (3) to analyze the structural changes occurring in the vertebrae and intervertebral discs following the generation and subsequent correction of scoliosis.
Materials and methodsPhase 1: Comparative radiographic study phase during the modulation of vertebral growth through the use of shape-memory metals.
We used 23 male, Sprague-Dawley rats aged between 20 and 22 days. This protocol was approved by the Animal Experimentation Ethics Committee of the Universidad Autonoma of Madrid.
Generation of deformity: we used a modification of the method described by Sarwark et al. to create kyphoscoliosis.8 Firstly, we induced general anesthesia by an intraperitoneal injection of a dilution of ketamine, xylazine and atropine. Next, we obtained dorsoventral and lateral radiographs of the spine. We shaved the back of the animals and applied 4% chlorhexidine to clean the surgical field. We used amoxicillin-clavulanate for antibiotic prophylaxis and Oculos® ointment for eye protection. Induction of scoliosis was performed using an asymmetric suture between the left scapula and pelvis. This was done through 2 incisions of 1cm in the interscapular area and the base of the tail. Using a No. 0, non-absorbable suture (Prolene®, Ethicon Inc), we performed a double stitch in the bottom of the scapula, passing the suture again surrounding the neck of the scapula. Both ends of the suture were passed subcutaneously to the second incision at the base of the tail. With the end of the suture needle we made a double stitch surrounding the left sacroiliac joint. By tying the suture we instantly induced right convex scoliosis. The wounds were sutured with 3/0 thread and we then obtained dorsoventral and lateral radiographs. The rats were allowed to grow with this suture for 8 weeks.
Pain control was carried out through administration of subcutaneous meloxicam (3mg/kg/day) during the first 48h.
The rats were anesthetized every 2 weeks by intraperitoneal injection of ketamine, xylazine and atropine, in order to obtain dorsoventral and lateral radiographs. The angular values of kyphosis and scoliosis were measured using the Cobb method.
Deformity correction: at 8 weeks of suturing, the animals were randomized into 2 groups: nitinol (n=9) and control (n=9). In the control group we cut the Prolene® suture through a 1cm incision between the 2 previous incisions, under general anesthesia. In the nitinol group, through a posterior longitudinal incision, we cut the suture and implanted a nickel-titanium wire (NeoSentalloy®, 0.018“x0.018” F100, GAC International Inc, Japan) along the concavity, from the superior limit vertebra to the inferior limit vertebra, according to the preoperative radiograph.
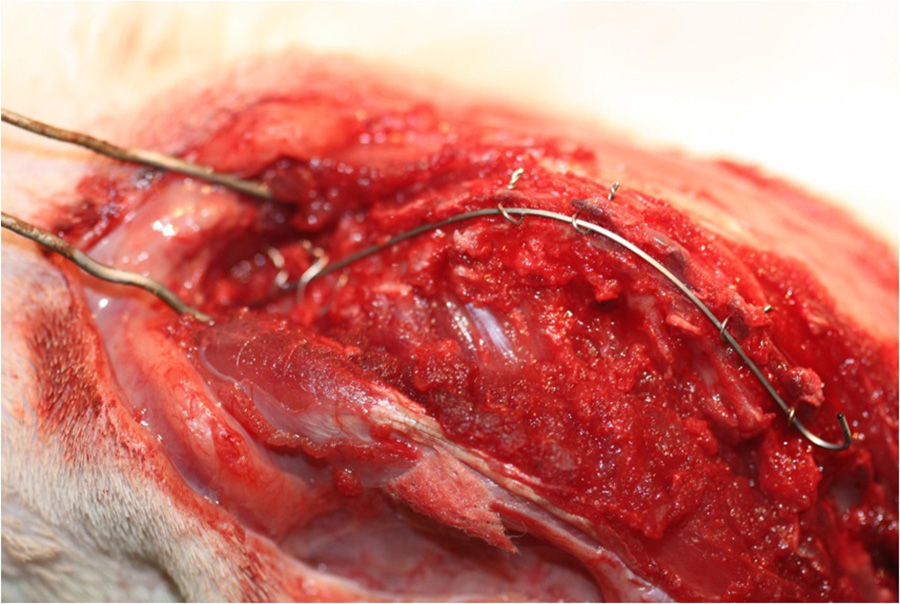
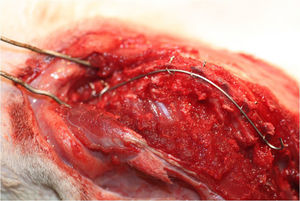
The wire was fixed to the column by creating 2 orifices in the spinous process using a microdrill, in the 2 inferior limit vertebrae and the 2 vertebrae at the apex. Creating these perforations in the spinous of the 2 superior limit vertebrae was impossible because the spinous process at this level is very thin and, therefore, easily broken. At this level we created a loop with 0.2mm steel wire between the spinous process and the transverse process.
A 0.2mm steel wire was passed through the holes created in the spinous, and the nitinol wire was placed lengthwise between them. By tightening the steel wires we obtained a good anchorage of the nitinol wire (Fig. 1), but we did not tighten it excessively in order to allow movement between the column and the nitinol wire.
After the procedure, we administered buprenorphine (0.05mg/kg/day) subcutaneously for pain control and amoxicillin-clavulanate (150mg/kg/day) intramuscularly for 3 days to prevent infection of the surgical wound and urinary tract. The animals were monitored daily by the veterinarian of the animal center throughout the duration of the experiment.
We obtained radiographs from animals in the immediate postoperative period, at 24h, 72h, 1 week and 2 weeks under general anesthesia. We studied the angular values of kyphosis and lordosis using the Cobb method.
Phase 2: comparative histological study phase after the generation and gradual correction of scoliosis with shape-memory metals.
In this second phase of the study we used quantitative parameters to analyze the structural changes taking place in the apical vertebra of the deformity (vertebral wedging) and adjacent discs (disk wedging) upon generation of scoliosis and after its subsequent correction. We used 15 male S-D rats aged between 20 and 22 days. We reproduced the same experimental scoliosis model described in the radiographic phase 1 of the study in all specimens. This was done by performing a suture between the scapula and left pelvis. The sutures were maintained for 8 weeks, after which we obtained dorsoventral and lateral radiographs of each animal and then randomized them into 2 groups: control and nitinol. At that moment we performed the second surgical procedure to cut the suture and implant the nickel-titanium wire. At 2 weeks after the second surgery we proceeded to sacrifice the animals by inhalation of carbon monoxide in an airtight chamber and extract their spines, in a specimen including the thoracic and lumbar regions. This fragment was inserted in neutral buffered formalin at 4% for 48h. We selected the apical vertebra of the deformity after removing the majority of the paravertebral soft tissues and with the help of radiographs. We used a scalpel to cut the column fragment including the apical vertebra, cranial and caudal intervertebral discs to the apical vertebra and half of the adjacent vertebral bodies. This fragment was inserted in neutral buffered formalin at 4% for its histological study. Following decalcification by immersion in Cal-Rite® for 72h at room temperature, we carved the pieces through a cut in the coronal plane, at the central part of the vertebral body. We then proceeded to embed the specimens in paraffin to form a block which could be cut with a manual microtome into 5 micron sections. These sections were placed in the preparation and stained with hematoxylin-eosin.
The histological parameters studied were the angle of the apical vertebral body and adjacent discs, as well as the length of the concave and convex sides of the body and discs. Angulation was calculated taking the line formed by the endplate as a reference, whilst for lengths we used the point of union between the endplate and the annulus fibrosus. Angulation was measured using the software package Surgimap Spine® (Nemaris Inc.), whereas for lengths we used the micrometer scale of an optical microscope.
Statistical methodsStatistical analysis was performed using the software package SPSS version 11.5. We applied a significance level of P=.05 and bilateral contrast for all tests. Variables with a temporal evolution were analyzed using the ANOVA test with repeated measures along with the Greenhouse–Geisser test. We used the Bonferroni post-test to explore possible differences between 2 and 2 moments. Comparisons between continuous variables were performed using nonparametric tests with the Mann–Whitney U test.
ResultsPhase 1: Comparative radiographic study phase during the modulation of vertebral growth using shape-memory metals.9
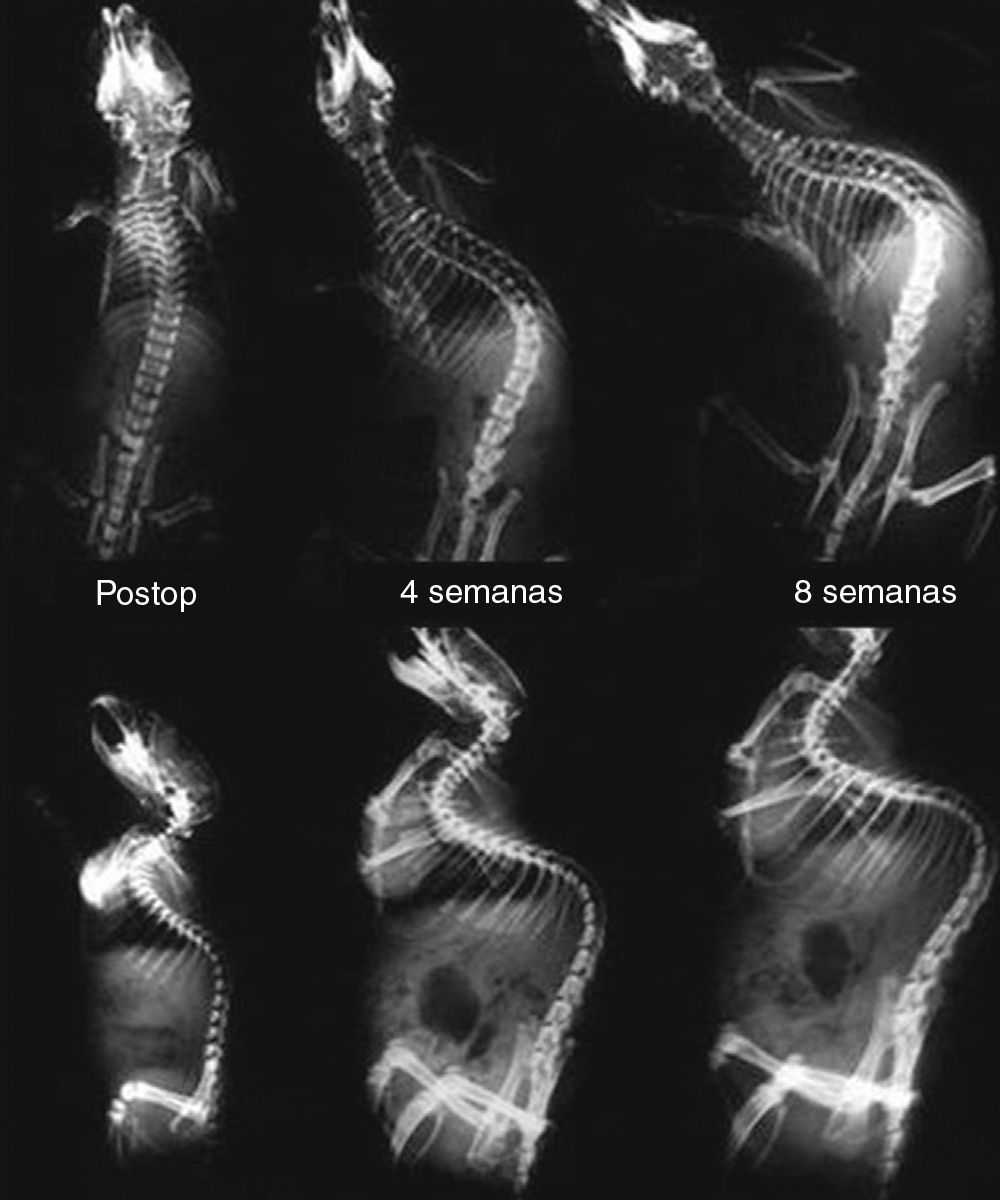
Generation of deformity: during the initial period of asymmetric suture we generated a convex kyphoscoliosis curve toward the right side in the thoracolumbar region in all rats except for 3, with radiographic features of structured scoliosis, such as translation of the apical vertebra of the sacral vertical line, wedging of the vertebral bodies and rotation at the apical level (Fig. 2).
The initial radiographs showed a straight column in all animals. A mean scoliosis of 35.5° was generated after the suture, which progressed to a mean value of 81.5° after 8 weeks.
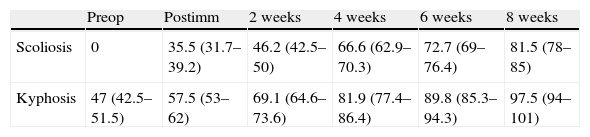
In the lateral plane, all rats presented a normal sagittal profile, with a mean value of 47° kyphosis before suture. After the suture, the mean value of kyphosis was 57.5°, which progressed to 97.5° at 8 weeks (Table 1). The progression of deformity in both planes was statistically significant.
Angular values (mean and confidence interval) of scoliosis and kyphosis generated in the first phase through the suture of the scapula to the pelvis.
| Preop | Postimm | 2 weeks | 4 weeks | 6 weeks | 8 weeks | |
| Scoliosis | 0 | 35.5 (31.7–39.2) | 46.2 (42.5–50) | 66.6 (62.9–70.3) | 72.7 (69–76.4) | 81.5 (78–85) |
| Kyphosis | 47 (42.5–51.5) | 57.5 (53–62) | 69.1 (64.6–73.6) | 81.9 (77.4–86.4) | 89.8 (85.3–94.3) | 97.5 (94–101) |
Postimm: immediate postoperative; Preop: preoperative.
We were not able to generate scoliosis in 3 animals. In 2 cases due to a loosening of the suture and in 1 to a “cut-out” phenomenon of the suture at the level of the scapula. Two rats died due to hypothermia and excessive bleeding in the immediate postoperative period of the initial scoliosis-generation surgery.
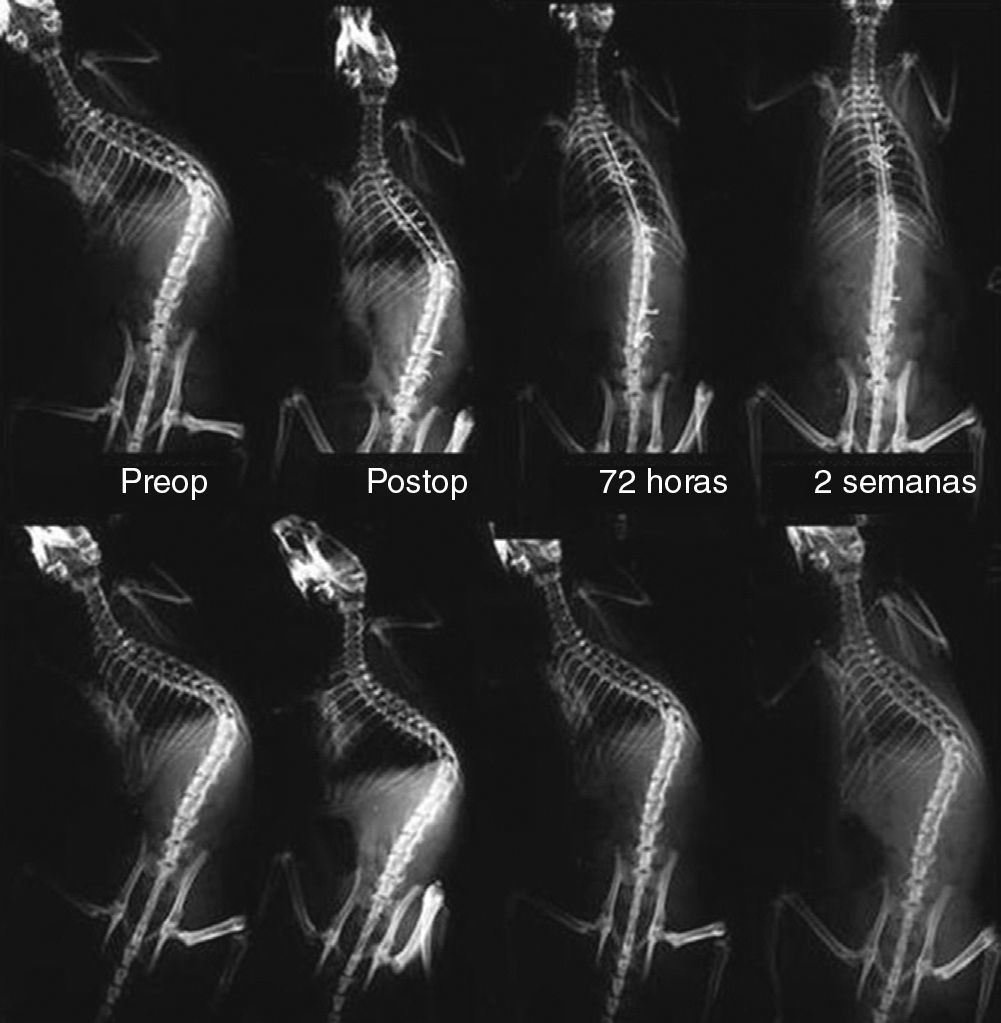
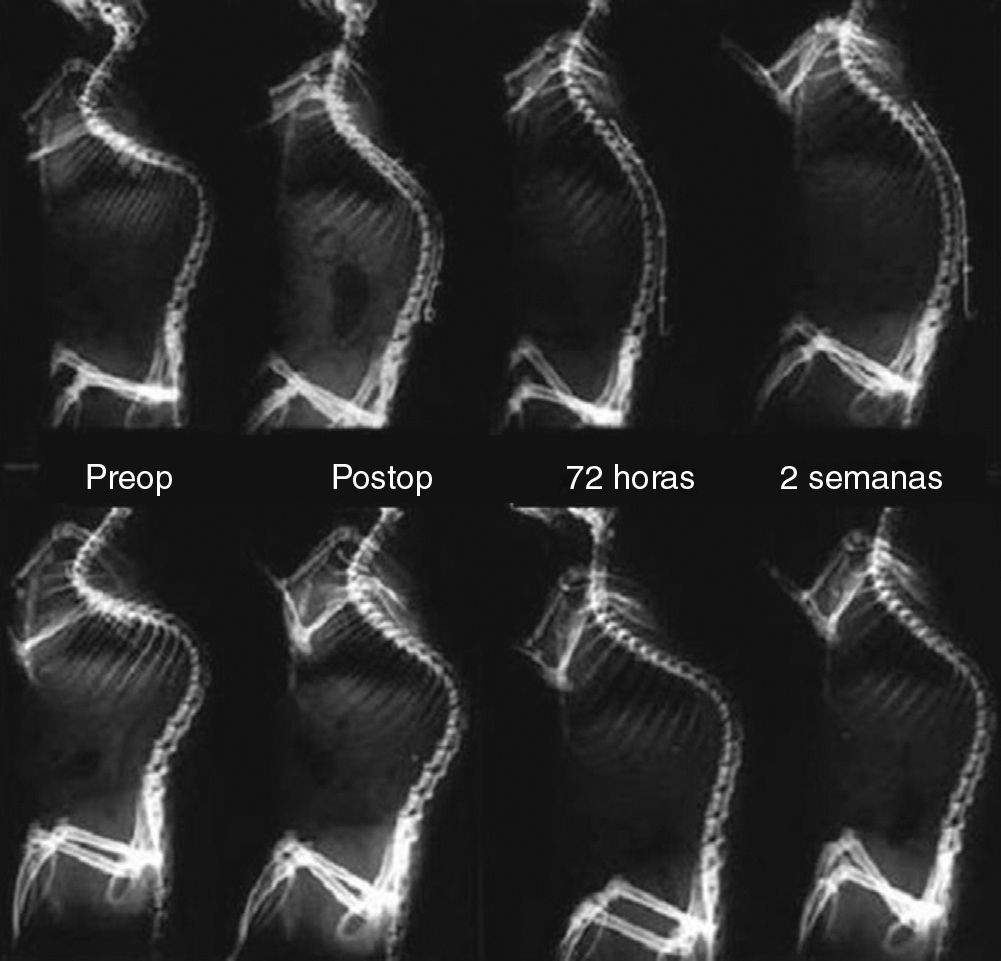
Deformity correction: rats in the nitinol group showed a greater overall correction of kyphoscoliosis than control rats during the treatment period. After randomizing the animals, there were no statistically significant differences in the values of kyphosis (P=.52) and scoliosis (P=.23) between the animals in the nitinol group and the control group.
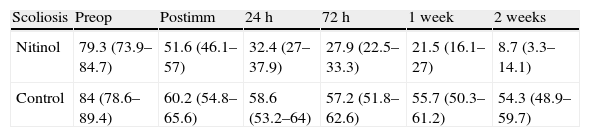
The mean initial value of scoliosis in the nitinol group was 79.3° (CI: 73.9–84.7) and final scoliosis was 8.7° (CI: 3.3–14.1). We observed a gradual correction throughout the follow-up period (Table 2). In the control group, the mean initial scoliosis was 84° (CI: 76.3–91.6) and the final scoliosis was 54.3° (CI: 46.6–70). In this group there was an initial decrease of scoliosis after the suture was cut, but, unlike the nitinol group, the deformity remained stable over time after the initial reduction of the curve, with highly significant differences between groups being registered (P<.001).
Angular values (mean and confidence interval) of scoliosis during the correction through implantation of a nitinol wire anchored to the spine, comparatively between the nitinol and the control group.
| Scoliosis | Preop | Postimm | 24h | 72h | 1 week | 2 weeks |
| Nitinol | 79.3 (73.9–84.7) | 51.6 (46.1–57) | 32.4 (27–37.9) | 27.9 (22.5–33.3) | 21.5 (16.1–27) | 8.7 (3.3–14.1) |
| Control | 84 (78.6–89.4) | 60.2 (54.8–65.6) | 58.6 (53.2–64) | 57.2 (51.8–62.6) | 55.7 (50.3–61.2) | 54.3 (48.9–59.7) |
Postimm: immediate postoperative; Preop: preoperative.
From the outset, the correction of scoliosis after cutting the suture and implanting the nitinol wire differed between both groups. In the nitinol group, scoliosis was corrected from 79.3° to 51.5° on average (27.8 correction) after implanting the nickel-titanium wire and cutting the suture, whilst the mean scoliosis in the control group was corrected from 84° to 60.2° (23.8 correction) after just cutting the suture.
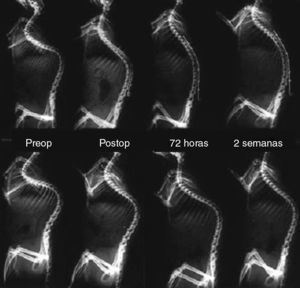
During the 2 weeks of the correction period, the rats in the nitinol group gradually obtained a mean additional 42.8° correction, whereas control animals showed a mean correction of 6° (Fig. 3). The differences between both groups were significant (P<.001) (Table 2).
Comparative, serial dorsoventral radiographs between the nitinol group (top) and the control group (bottom), before implantation of the nitinol wire, in the immediate postoperative period, at 72h and 2 weeks after surgery. Note the gradual correction of scoliosis in the nitinol group throughout the 2 weeks of treatment. In comparison, in the control group there is an initial reduction of the deformity, which then remains stable during follow-up.
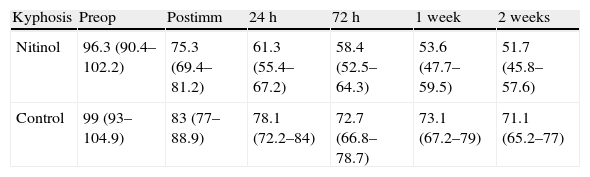
In the sagittal plane, nitinol group rats showed an increased correction of kyphosis compared to control rats (Fig. 4). The mean value of kyphosis in the control group after randomization was 96.3° (CI: 90.4–102.2), which was corrected to 75.3° (CI: 69.4–81.2) after cutting the suture and implanting the wire, and to a mean value of 51.7° (CI: 45.8–57.6) at 2 weeks after corrective surgery. Correction of kyphosis in the control group was lower, with an initial mean kyphosis value of 99° (CI: 93–104.9) which was corrected to 83° (CI: 77–88.9) on average after cutting the suture and to 71.1° (CI: 65.2–77) at 2 weeks (Table 3). These differences were statistically significant (P<.001). None of the rats died during corrective surgery or during the follow-up period.
Comparative serial lateral radiographs between the nitinol group (top) and the control group (bottom), before implantation of the nitinol wire, in the immediate postoperative period, at 72h and 2 weeks after surgery. Note a greater correction of kyphosis in the nitinol group than in the control group.
Angular values (mean and confidence interval) of kyphosis during the correction through implantation of a nitinol wire anchored to the spine, comparatively between the nitinol and the control group.
| Kyphosis | Preop | Postimm | 24h | 72h | 1 week | 2 weeks |
| Nitinol | 96.3 (90.4–102.2) | 75.3 (69.4–81.2) | 61.3 (55.4–67.2) | 58.4 (52.5–64.3) | 53.6 (47.7–59.5) | 51.7 (45.8–57.6) |
| Control | 99 (93–104.9) | 83 (77–88.9) | 78.1 (72.2–84) | 72.7 (66.8–78.7) | 73.1 (67.2–79) | 71.1 (65.2–77) |
Postimm: immediate postoperative; Preop: preoperative.
Phase 2: comparative histological study phase, after generation and subsequent gradual correction of scoliosis with shape-memory metals.
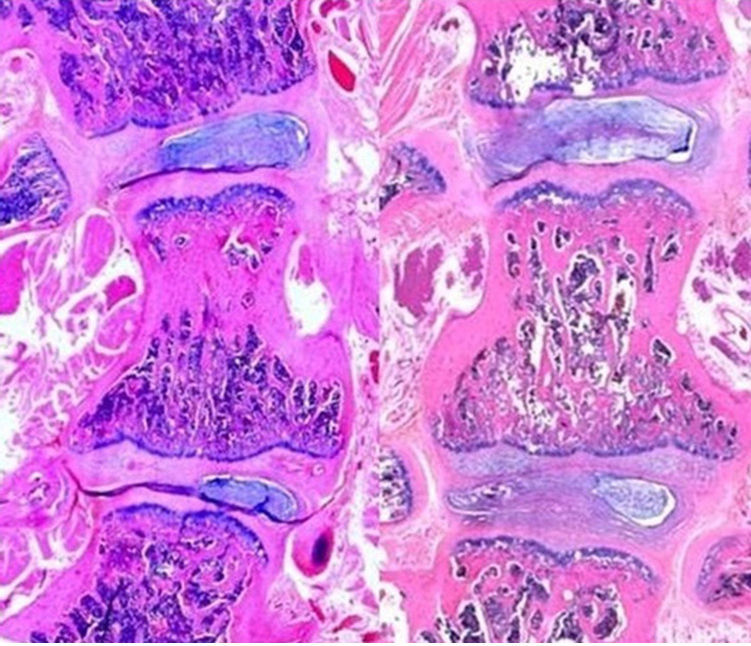
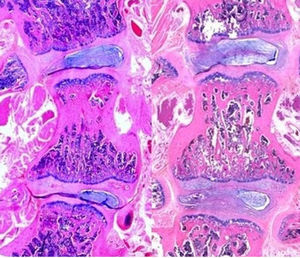
Fig. 5 shows the differences between 2 histological preparations; the left image is from a rat in the control group and the right image is from a rat in the nitinol group. At a first glance, it is possible to see the differences in the angulation of the vertebral body and adjacent intervertebral discs between the 2 groups. The control group image shows a wedging of the vertebral body and adjacent discs, that is, the parallelism between the vertebral endplates has been lost. In the nitinol group, after correcting the deformity, the angulation of the vertebral bodies and discs is reduced, thus indicating that correction of the deformity also partially corrected the histological changes generated by induction of kyphoscoliosis.
Photograph of histological preparations; the section on the left belongs to a control group rat (after generating scoliosis), whereas the section on the right belongs to a nitinol group rat (after correcting the deformity). Note the difference in angulation of the apical vertebral body and the adjacent intervertebral discs between groups.
Both groups were similar following randomization of the animals, with a mean Cobb angle of 65.33° in the nitinol group and 67.5° in the control group (P=.485).
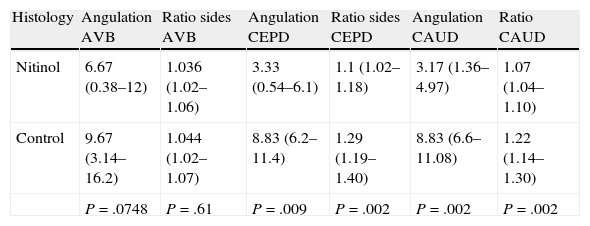
Table 4 shows the angulation and ratio values resulting from dividing the length of the convex side between the length of the concave side, at the level of the vertebral body, and of the adjacent intervertebral discs.
Values of corresponding to angulation (in degrees) and ratio resulting from the division of the length of the convex and the concave sides, at the level of the apical vertebral body and the cephalic and caudal intervertebral discs in the nitinol and control groups.
| Histology | Angulation AVB | Ratio sides AVB | Angulation CEPD | Ratio sides CEPD | Angulation CAUD | Ratio CAUD |
| Nitinol | 6.67 (0.38–12) | 1.036 (1.02–1.06) | 3.33 (0.54–6.1) | 1.1 (1.02–1.18) | 3.17 (1.36–4.97) | 1.07 (1.04–1.10) |
| Control | 9.67 (3.14–16.2) | 1.044 (1.02–1.07) | 8.83 (6.2–11.4) | 1.29 (1.19–1.40) | 8.83 (6.6–11.08) | 1.22 (1.14–1.30) |
| P=.0748 | P=.61 | P=.009 | P=.002 | P=.002 | P=.002 |
AVB: apical vertebral body; CAUD: caudal disk; CEPD: cephalic disk.
The results show that the mean length of the convex side of the vertebral body was greater than that of the concave side in both groups. This translates into an angulation of the vertebral body and a ratio greater than 1. In the control group, the mean angulation of the vertebral body was 9.67° and the ratio was 1.044, whereas in the nitinol group the mean angulation was 6.67° and the ratio was 1.036. The differences observed between both groups regarding the parameters of the vertebral body were not statistically significant.
These differences were more evident at the level of the intervertebral discs than in the apical vertebral body. In the cephalic intervertebral disk to the apical vertebra, the angulations of the discs were 8.83° in the control group and 3.33° in the nitinol group (P=.009), whereas the length ratios of the sides were 1.29 and 1.1, respectively (P=.002). In the caudal disk to the apical vertebra, the angulations of the discs were 8.83° in the control group and 3.17° in the nitinol group (P=.002), whereas the length ratios of the sides were 1.22 and 1.07, respectively (P=.002). Therefore, the length of the convex side of both intervertebral discs was greater than that of the concave side, resulting in an angulation of the intervertebral disk and a ratio greater than 1. However, after correction of the deformity there was a reduction of the angle and ratio, with these differences being statistically significant.
DiscussionThe usual surgical treatment of scoliosis involves instrumented posterior spinal arthrodesis (or fusion). This achieves a significant and instantaneous correction of the deformity through a series of surgical maneuvers and with the aid of modern spinal instrumentation which enables the application of considerable forces to the vertebrae. However, these techniques entail a potential risk of neurological damage because an instantaneous correction of the deformity may cause spinal cord ischemia or through direct damage caused during the placement of implants in the spine. Moreover, spinal fusion adversely affects the development of the thorax and lungs.
The development of “smart metals” with superelasticity and shape memory has introduced a new treatment philosophy: gradual and progressive correction over time, in order to maintain the spine under permanent corrective forces.
The implant used in this study was a straight, orthodontic wire made of a nickel and titanium alloy which applied a flexion force of 100g. The initial condition of the wire was below its transition temperature (32°C) in the martensite phase. In this phase, the wire presented very little resistance and could be easily deformed, thus facilitating its anchoring to the spine. Once the wire was heated above 32°C, it changed to the austenite phase, recovering its original shape and rigidity. If there were any limitations to recovering its shape, the wire applied a constant, corrective force.
In the present study, the shape-memory wire was able to generate a gradual correction of scoliosis over time, rather than instantaneously, without fusion, because of the plastic behavior of the column when kept under permanent force. Moreover, it was capable of producing a partial correction of the structural changes in vertebrae and intervertebral discs which were produced upon the generation of scoliosis. This approach has the theoretical advantage of avoiding the risk of neurological damage associated with instant correction, as well as maintaining the growth of the spine. The main difference of our study with other studies was the ability to induce a gradual correction, not only during surgery and the heating of the wire, but throughout the entire postoperative period. Preliminary results of the radiographic study phase of this work have been published previously9 by the same group of authors.
There are very few authors who have investigated the advantages of shape-memory metals for the correction of scoliosis. The first attempt was carried out in Germany10; a nitinol wire was fixed on to the convex side a model consisting of 8 plastic vertebrae with a curved shape. When heated, the wire became shortened and the plastic model became straightened. Veldhuizen et al.11 designed a device consisting of a bar with shape memory programmed into a curved shape and anchored to the spine of a cadaver using pedicular screws and hooks. When the bar was heated to 50°C it produced a scoliosis curve of 45°.
Sanders et al.12 used 6 goats in whom they had previously generated experimental scoliosis. They instrumented the animals with a nitinol bar of 6mm diameter. When the bar became activated, it corrected the scoliosis. The curves measured 41° on average before implementation, 33° after placing the bar and 11° after heating the bar. However, the authors did not analyze whether there was a correction after heating the bar, over a certain period of time. A similar study was conducted in monkeys,13 in which 2 shape-memory bars were anchored to the spine with transpinous wires. This achieved a good instant correction of the previously-generated scoliosis, but failed to obtain additional and gradual correction after surgery.
Various authors have used curvilinear nitinol bars to generate scoliosis in healthy animals. Wever et al.14 used a curved nitinol bar, anchored to the vertebrae by pedicular screws in T12, L2 and L4, to progressively bend the spine of 6 pigs. They managed to generate a scoliosis with a mean value of 40° in the immediate postoperative radiographs, which remained constant throughout the follow-up period.
Various studies15–17 conducted by the same group of authors have evaluated the effectiveness of anterior vertebral staples with shape memory to correct scoliosis created previously in goats. The results reflected a poor capacity of the staples to correct the deformity.
To the best of our knowledge, the only application of nitinol bars in humans was that carried out by Wang et al.,18,19 as a temporary intraoperative tool. After placing pedicular screws as anchor points in the spine of patients with adolescent idiopathic scoliosis, they used a nitinol bar anchored to the screws which, when heated, tended to recover its original, rectilinear shape, thus acting as a temporary correction element. During the same surgical procedure, they then replaced it with a conventional bar. These authors demonstrated that the use of these temporary bars reduced surgical time and blood loss and improved the correction achieved compared to the use of traditional bars alone.
During the second phase of the study, we noted that the length of the convex side of the vertebral body and adjacent intervertebral discs was greater than that of the concave side. That is, generating experimental scoliosis produced a series of structural changes in the vertebral bodies and intervertebral discs which became reversed after the correction of the deformity, although pre-postcorrection differences were statistically significant at the level of the discs. This observation leads us to believe that the intervertebral discs have a greater ability to accommodate corrective forces than the vertebral body, with a more rapid reversibility of any structural changes. These histological changes were also observed by Sarwark et al.,8 who established that the magnitude of the deformity generated was proportional to the structural changes which took place in the vertebrae and intervertebral discs.
Following the completion of this work and the observation of the results obtained, we believe that shape-memory metals may have a potential future application in the treatment of scoliosis. This would be based on the development of a new philosophy of gradual correction over time, through the interaction of the corrective forces generated by the NiTi wire and the plastic properties of the spine.
Level of evidenceLevel of evidence I.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
FinancingThis work was financed through a SECOT 2010 research grant from the Spanish Society of Orthopedic Surgery and Traumatology.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sánchez-Márquez JM, Sánchez Pérez-Grueso FJ, Fernández-Baíllo N, Gil-Garay E, Antuña-Antuña S. Modulación del crecimiento de columnas escolióticas en animales de experimentación mediante el uso de barras de metal inteligente. Rev Esp Cir Ortop Traumatol. 2013;57:310–317.