The purpose of this study was to compare postoperative clinical and radiological results in adolescent idiopathic scoliosis curves treated by posterior arthrodesis using autogenous bone graft from iliac crest (CI) versus only local autograft bone (HL).
Patients and methodsA retrospective matched cohort study was conducted on 73 patients (CI n=37 and HL n=36) diagnosed with adolescent idiopathic scoliosis and treated surgically by posterior arthrodesis. The mean post-operative follow-up was 126 months in the CI group vs. 66 months in the HL group. The radiographic data collected consisted of preoperative, postoperative, and final follow-up antero-posterior and lateral full-length radiographs. Loss of correction and quality of arthrodesis were evaluated by comparing the scores obtained from the Spanish version of the SRS-22 questionnaire.
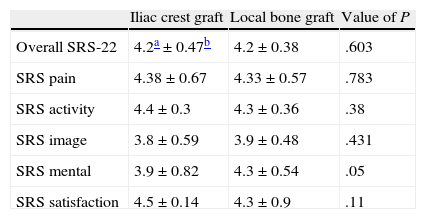
ResultsThere were significant differences in the post-operative results as regards the correction of the Cobb angle of the main curve (HL 61±15% vs. CI 51±14%, P<.004); however, a greater loss of correction was found in the local bone group (CI 4.5±7.3° vs. HL 8.5±6.3°, P=.02). There were no significant differences as regards the correction of the Cobb angle of the main curve at the end of follow-up. There were no clinical differences between the two groups in the SRS-22 scores.
ConclusionAt 5 years of follow-up, there was a statistically significant greater loss of radiographic correction at the end of final follow-up in the local bone graft group. However, clinical differences were not observed as regards the SRS-22 scores.
El objetivo de este trabajo es determinar si los resultados clínicos y radiológicos obtenidos en cuanto a corrección a largo plazo se mantienen de forma similar usando injerto de cresta ilíaca (CI) o solo el hueso local (HL) en los pacientes intervenidos con escoliosis idiopática del adolescente.
Pacientes y métodosSe efectuó un estudio retrospectivo de cohortes homogéneas de 73 pacientes (CI n=37 y HL n=36) con escoliosis idiopática intervenidos mediante artrodesis por vía posterior con un seguimiento medio de 126 meses en el grupo CI y 66 meses en el grupo HL. Se compararon los resultados en cuanto a corrección quirúrgica y pérdida de la misma según las mediciones de los ángulos de Cobb en telerradiografías antero-posteriores y laterales preoperatorias, postoperatorias y finales, y se valoraron los resultados clínicos mediante el cuestionario SRS-22.
ResultadosEn el grupo HL la corrección postoperatoria resultó significativamente mayor 61±15% vs. 51±14% del grupo CI (p<0,004). Durante la evolución el grupo CI presentó una pérdida de corrección media de 4,5±7,3° respecto a los 8,5±6,9° del grupo HL, (p=0,02). La corrección final obtenida se iguala entre ambos grupos, 42±18% vs. 46±17% (p=0,3). No se observa correlación clínica en la muestra respecto a los resultados del SRS-22.
ConclusionesLos pacientes intervenidos en los que se emplea injerto de CI tienen una pérdida de corrección inferior a los pacientes en los que se emplea injerto de HL aunque no parece existir correlación clínica de esta pérdida de corrección.
The use of iliac crest (IC) autograft to obtain a correct arthrodesis (or fusion) represents the gold standard in the surgical correction of adolescent idiopathic scoliosis (AIS). However, the morbidity associated with obtaining it1,2 leads us to wonder whether this is really necessary in order to maintain surgical correction.
Pain at the donor site can occur in up to 24% of cases at 4 years, along with up to 15% of associated functional deficits.3,4 Other complications, such as hematomas, seromas and wound dehiscence, have also been observed in these patients, with these morbidities being proportional to the volume of graft extracted.5
The use of allografts has proven effective. However, they entail a risk of disease transmission and are dependent on the availability of tissue banks.6–8 Bone substitutes could represent an alternative to autografts and allografts, but they are very costly.9,10
Some studies have recently reported comparable data regarding the consolidation of arthrodesis in patients undergoing surgery due to lumbar pain in whom only bone from the surgical field was used, without additional IC, and with no increase in the rate of pseudoarthrosis (or nonunion).11 No losses of correction or pseudoarthrosis associated with the use of grafts from the surgical field have been observed in patients undergoing surgery due to scoliosis.12
There are no published studies comparing the clinical and radiographic results between patients suffering adolescent idiopathic scoliosis in whom iliac crest graft was used versus those in whom the graft came only from the posterior elements. The purpose of the present study was to compare the results with regard to the achievement of arthrodesis and maintenance of surgical correction in patients suffering idiopathic scoliosis who underwent surgery using autografts from the surgical field versus a control group in whom an additional IC graft was used.
Patients and methodsThis was a retrospective cohort study which collected data from 73 patients diagnosed with AIS (aged between 10 and 18 years) who underwent surgery between 1992 and 2008, and who underwent a posterior correction by a single senior surgeon (EI). Two homogeneous cohorts of patients with AIS were analyzed, which had similar ages, magnitudes and types of curves. In the first cohort we used an IC graft (IC group) whereas in the other cohort we only used grafts from the posterior elements (only local bone group [LB]). The tendency to take iliac crest grafts has been abandoned over time, so even though both groups overlapped chronologically in time, the current trend towards using iliac crest grafts was reduced. Therefore, the mean follow-up time in the IC group was longer.
We excluded patients with clinical and radiological follow-up under 2 years, as well as those in whom a double approach was used. We also excluded patients who required reoperation due to infection of the surgical wound in order to eliminate infection as a cause of pseudoarthrosis.
Surgical techniqueIn this study we used a midline posterior approach with subperiosteal dissection. We resected spinous processes at their base, along with inferior surfaces of the superior vertebrae and the exposed cartilage of the superior surface of the inferior vertebrae. We also removed the soft parts, periosteum and articular cartilage, reserving the bone for its subsequent use. In some cases we performed Chevron osteotomies in the most rigid areas of the curve.
We used multisegmental hook instrumentation (Cotrel Dobousset®, Medtronic Sofamor Danek, Memphis, USA), as well as hybrid (Isola® DePuy Spine Raynham, USA). In the IC group we extracted the autologous IC graft and mixed it with local graft obtained from the spinous processes and joint facets after cleaning them of soft tissue. In the LB group we only used material extracted from the surgical field for grafts. We did not use a brace in the postoperative period and patients were not allowed flexion or weight bearing for the first 6 months.
Study of resultsWe obtained radiographs of all patients in anteroposterior and lateral standing during the preoperative and postoperative (at 3 months) periods, and at the end of the evolution. The Cobb angle of the main curve, coronal imbalance, T5T12 kyphosis and L1S1 lordosis were measured in all cases. We calculated the percentage of correction and evaluated the loss of correction of the main curve using the differential: final Cobb – postoperative Cobb. We considered losses above 10° to be “suggestive” of instability or pseudoarthrosis.13,14
We used the Spanish validated version of the SRS-22 test for clinical evaluation at the end of evolution. We compared values in both groups for each of the sections of the test. Furthermore, we also compared the results among patients who had lost more surgical correction with those of the rest of the sample.
In addition, we also recorded any complications.
The null hypothesis was that there would be no differences regarding the loss of correction between both groups and that the clinical results would be comparable.
Statistical analysisThe statistical analysis was carried out using the SPSS® v.15.0 software package, through a comparison of means for independent variables with a Student t significance level of P=.05.
ResultsDemographic dataThe IC group was composed of 26 females and 11 males, with a mean age of 15.1±2.1 years and a mean follow-up period of 126.4±61.21 months. The most common types of curves according to the Lenke classification were type I with 62% and type III with 15%.
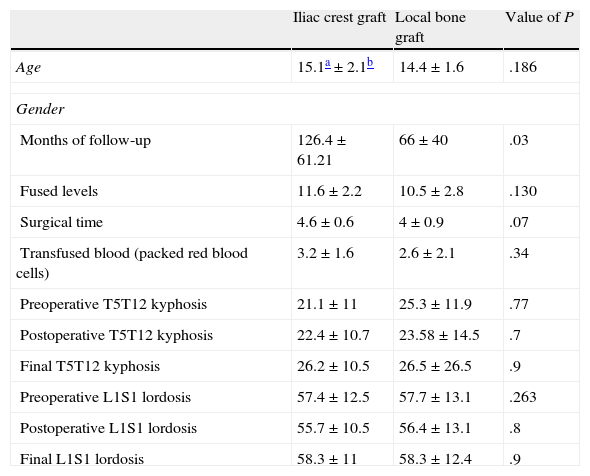
The local bone graft group was composed of 34 females and 2 males, with a mean age of 14.4±1.6 years and a mean follow-up period of 66±40 months. The most common types of curves were type I and type III (28% and 30%, respectively). There was a non-significant trend towards a lower number of fused levels, transfused blood units and shorter operative time in the local graft group (Table 1).
General data in the sagittal plane.
| Iliac crest graft | Local bone graft | Value of P | |
| Age | 15.1a±2.1b | 14.4±1.6 | .186 |
| Gender | |||
| Months of follow-up | 126.4±61.21 | 66±40 | .03 |
| Fused levels | 11.6±2.2 | 10.5±2.8 | .130 |
| Surgical time | 4.6±0.6 | 4±0.9 | .07 |
| Transfused blood (packed red blood cells) | 3.2±1.6 | 2.6±2.1 | .34 |
| Preoperative T5T12 kyphosis | 21.1±11 | 25.3±11.9 | .77 |
| Postoperative T5T12 kyphosis | 22.4±10.7 | 23.58±14.5 | .7 |
| Final T5T12 kyphosis | 26.2±10.5 | 26.5±26.5 | .9 |
| Preoperative L1S1 lordosis | 57.4±12.5 | 57.7±13.1 | .263 |
| Postoperative L1S1 lordosis | 55.7±10.5 | 56.4±13.1 | .8 |
| Final L1S1 lordosis | 58.3±11 | 58.3±12.4 | .9 |
Although there were differences regarding the more predominant female gender in the iliac crest graft group, these differences were not significant (Fisher=0.012).
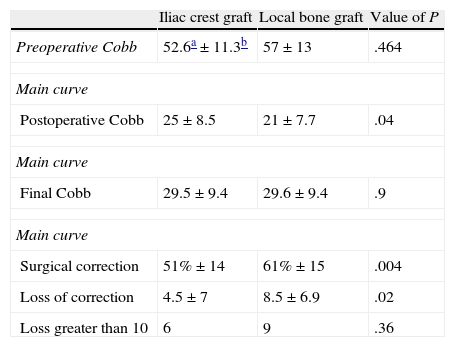
There were no significant differences regarding the magnitude of the major curve (IC 52.6±11.3° vs LB 57±13°; P=.46) and the secondary curve (IC 35±12° vs LB 36±10°; P=.7).
Radiographic resultsThe overall loss of correction was 6±7°, with a significantly greater loss taking place in the group in which no IC graft was used (LB 8.5±6.9 vs IC 4.5±7.3; P=.02). We found statistically significant differences regarding postoperative correction, with values of 51±14% in the IC group vs 61±15% with a P=.004. In addition, we also found a positive correlation between the loss of correction and the surgical correction obtained with a Pearson p of 0.34 and P<.05. The final correction obtained was similar between both groups: 42±18% vs 46±17%; P=.3 (Table 2).
Loss of correction of main curve.
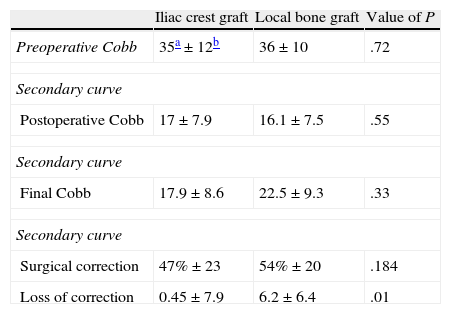
Correction of the secondary curve (Table 3) was greater in the group with local bone graft, but without significant differences (54.14±20 in the LB group vs 47.06±23 in the IC group; P=.1). Loss of correction of the secondary curve was higher in the local bone graft group, as was the case in the main curve (6.2±6 LB vs 0.45±7 IC; P=.01).
Loss of correction of secondary curve.
There were no significant differences in terms of kyphosis or lordosis between both groups at the various times of the study (Table 1).
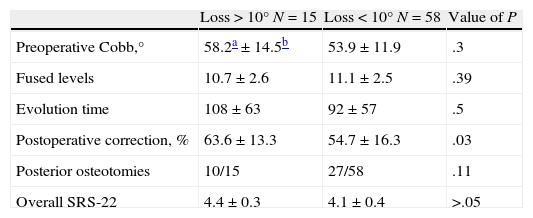
Considering those patients who lost more than 10° correction during the follow-up period, out of a total of 15 cases, 6 belonged to the IC group and 9 belonged to the LB group, with no significant differences being observed (χ2=0.36). None of them had to be reoperated due to pain or breakage of instrumentation. When comparing the group of patients who had lost more than 10° (Table 4) with the rest of the sample, we observed that these patients presented a significantly higher postoperative correction. No differences were observed with respect to the evolution time or the number of fused levels.
Comparative data between patients with greater losses of correction and the rest of the sample.
We obtained evaluation tests at the end of the clinical evolution. These clinical results showed no significant differences between the two groups, as shown in Table 5. Neither were there any differences when we considered those patients in both groups who presented a correction greater than 10°, compared to the group with losses less than 10°. Thus, such correction losses were not reflected clinically.
ComplicationsComplications occurred in 6 patients, 4 cases of superficial infection which were resolved with intravenous antibiotic therapy, 1 dura mater tear which was conservatively treated with hydration and rest, and 1 mild progression of the curve under the instrumentation which did not require surgery. There was 1 case of instrumentation rupture at the proximal level in a patient who had a loss of correction of 9°. The patient was monitored and no subsequent loss of correction was observed, so she was treated conservatively.
DiscussionThe objective of surgical treatment of scoliosis is to correct the curve, balance the spine and obtain a good arthrodesis in order to maintain the correction. Different types of approaches, grafts and implants have been used for this purpose. For years, IC grafts have been frequently used because their osteogenic capacity makes them an ideal material to ensure arthrodesis. However, the morbidity associated with their extraction, such as pain in the donor area in up to 24% of cases, as well as functional deficits in up to 15% of cases,1–3,5 lead us to question whether its extraction is really necessary, especially given the availability of new, more rigid, multisegmental fixation systems.12,13
Some authors have shown the osteoconductive efficacy of other, alternative allografts. The literature contains reports of results similar to those obtained with IC autografts.6,7 However, these studies only have an evidence level 4, and there is still a risk of transmission of infectious diseases.4 Some studies have reported a lower rate of fusion when using allografts. In a prospective study of 2 groups of patients which compared the use of allografts versus no graft, Betz et al.13 found no significant differences between both groups. They concluded by stressing the importance of proper dissection, complete elimination of soft tissues in the fusion area, meticulous decortication of the posterior elements and the use of more rigid instrumentation as the most influential factors in obtaining adequate arthrodesis, rather than the type of graft employed.
So far, bone substitutes4,9 such as a demineralized bone matrix have yielded good results due to their osteoinductive and osteoconductive properties, so their use could be an alternative to existing grafts. However, some studies do not support their use in isolation compared to autografts,10 and their elevated cost also restricts their widespread use.
The use of bone grafts from the posterior elements may be an effective alternative, although there are still some doubts regarding their viability. Miura et al.11 conducted studies with patients undergoing surgery due to lumbar pain who underwent instrumented circumferential fusion and who received grafts from laminar and articular portions and observed a radiological fusion rate of 100% at 12 months. Violas et al.12 conducted a study of the effectiveness of grafts from the posterior elements for the preservation of the arthrodesis with a follow-up period of 6 years. They obtained grafts from the lamina, transverse and spinous processes of the non-instrumented vertebrae and applied them to the articular after decorticating them. They did not observe any losses of correction of the principal or secondary curves in their series.
It is not always simple to obtain a definitive diagnosis of nonunion. The presence of nonunion is accepted in those patients in whom it is observed intraoperatively and in those cases where a rupture of the instrumentation takes place. However, some authors13,14 have proposed a lack of radiographic union and the loss of over 10° during evolution as possible criteria of nonunion. Should all cases which have lost over 10° be considered as failures? Price et al. observed between 15% and 25% of losses over 10°, although only 2% of these cases required a new intervention due to persistence of pain or progression of the curve.15 The clinical results regarding the SRS-22 test support this theory, with similar results obtained among the groups of patients with losses over and under 10°. There was a single case of instrumental breakage which lost a total of 9° at the end of the evolution and was treated conservatively. On the other hand, the surgical correction of the sagittal and coronal planes of AIS patients did not seem to be reflected in the results of the SRS-22 test.16
According to the present results, the series in which the iliac crest graft was used, which was done earlier in the learning curve of the main surgeon (EI), obtained significantly lower surgical corrections than the cohort in which the iliac crest graft was no longer used. There was a significant correlation in the series between the surgical correction and the loss thereof at the end of evolution (Pearson 0.34; P<.05). Therefore, this could be a confounding factor, not reported to date. In other words, patients undergoing surgery at later dates (in whom IC grafts were no longer used), obtained greater corrections and, therefore, also lost more correction. In future work we shall analyze this observation separately. In addition, new questions arise regarding the influence of extended releases on the loss of correction since we observed a relationship between them, as previously reported.17 It remains to be determined whether the loss of correction will increase even further in the local bone group throughout the evolution, thus increasing the existing differences.
ConclusionsAfter a mean follow-up period of 5 years for both groups, we obtained correction losses in patients in whom we had not used IC grafts, although with a difference under 4°. These losses had no clinical correlation, as shown by the SRS-22 test results. We did not find any correction losses in relation to gender and type of instrumentation in the series.
Level of evidenceLevel of evidence iii.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mardomingo A, Sánchez-Mariscal F, Álvarez P, Pizones J, Zúñica L, Izquierdo E. ¿Es el autoinjerto del campo quirúrgico suficiente para la obtención de una buena artrodesis en paciente con escoliosis idiopática del adolescente? Rev Esp Cir Ortop Traumatol. 2013;57:318–323.