Posterior spinal instrumentation and fusion with pedicle screws inserted by free-hand technique and controlled by multimodal intraoperative monitoring is the most common technique in adolescent idiopathic scoliosis surgery. Pneumothorax is a described complication of this kind of procedure. Triggered electromyography is used to identify pedicle wall breakthrough and prevent neurological injuries. We report 2 clinical cases in which unilateral decrease in triggered electromyography values associate with ipsilateral pneumothorax. Postoperative chest radiographs need to be done in order to diagnose a pneumothorax. However, routinely performing a chest radiograph has been questioned because of the low incidence of this surgical complication. As a result of the association described in this article, we consider that when a unilateral decrease in triggered electromyography values is detected, a hidden pneumothorax should be suspected and ruled out.
La artrodesis posterior instrumentada con tornillos pediculares mediante manos libres y con monitorización neurofisiológica intraoperatoria es la técnica quirúrgica más común en cirugía de escoliosis idiopática del adolescente. Una complicación descrita durante este tipo de intervenciones es el neumotórax. La estimulación de los tornillos pediculares es la técnica neurofisiológica empleada para la detección del mal posicionamiento de los mismos y para prevenir lesiones neurológicas iatrogénicas. Presentamos 2 casos clínicos en los que la caída unilateral de los umbrales de los tornillos pediculares se asocia a neumotórax ipsilateral. Para detectar un neumotórax, hay que realizar una radiografía de tórax postoperatoria. Sin embargo, esta práctica ha sido cuestionada debido a la baja incidencia de esta complicación. A raíz de la asociación descrita en este trabajo, consideramos que ante un descenso o asimetría en los umbrales de los tornillos pediculares debemos sospechar y descartar la existencia de un neumotórax.
Posterior arthrodesis instrumented with pedicle screws is the surgical treatment of choice for patients with adolescent idiopathic scoliosis (AIS). The misplacement rate of thoracic pedicle screws varies greatly in the literature, some series reporting up to 30% of screws implanted using the hands-free technique.1 Poorly placed screws can cause potentially serious neurological and visceral injuries.1,2
The free-hand technique3 with intraoperative neurophysiological monitoring (INM) is the most widely used surgical technique in AIS, with less intraoperative radiological exposure than its alternatives. INM has become an essential tool as it has been shown to reduce the incidence of neurological injury in surgery to treat deformity.4 Triggered electromyography for pedicle screw placement is used to detect medial breaches in the vertebral pedicle. It consists of applying a single electrical stimulus to the screw and recording the motor response in the muscle corresponding to the root of the level stimulated. The sensitivity and specificity values described in the literature to detect screw misplacement by means of this technique are 0.78 and 0.94 respectively.5,6
Pneumothorax is one of the complications described during instrumented posterior arthrodesis in patients with AIS. It can occur as a consequence of vertebral pedicle breaches or large dissections between the transverse processes.7 The incidence of pneumothorax described in the literature in patients undergoing surgery for AIS varies between 0.3% and 3.3% and is related to the number of fused levels, proximal location of the thoracic curve and the need for intraoperative blood transfusion.2 Although this is a rare complication, it is essential that it is identified early and treated appropriately to resolve a condition that is potentially fatal.
The aim of this work was to describe the association between the onset of pneumothorax and a decrease in ipsilateral thoracic pedicle screw thresholds during AIS surgery. The secondary aim was to propose a plausible pathophysiological mechanism for this possible relationship.
Clinical cases and resultsWe present two cases of patients undergoing surgery for AIS who developed a pneumothorax associated with an ipsilateral decrease in thoracic pedicle screw thresholds (PST) as a surgical complication.
In our centre, we have been performing all surgery to treat deformity under INM since 2006. The protocol includes motor evoked potentials (MEP), somatosensory evoked potentials (SSEP), continuous electromyogram (EMG) and PST. To obtain the PST, we use a stimulator cathode placed over the head of the screws and a 12 mm monopolar needle inserted in the ipsilateral paraspinal musculature, which acts as an anode. The parameters for recording responses are stimuli with a frequency of 1 Hz and a duration of 0.5 ms with increasing intensity until a repeatable compound action potential is obtained in the corresponding myotome muscle. For PST of thoracic level T2-T6, electrodes are placed on the intercostal musculature at the mid-axillary line. At the T6-T12 levels, the electrodes are placed on the intercostal musculature or on the abdominal oblique muscle. Lumbar levels L1-L5 are recorded in the adductor longus, vastus lateralis, tibialis anterior and abductor hallucis muscles. We have included double stimulation of pedicle screws in our monitoring protocol for the last 2 years:
- •
Immediately after implanting the screw.
- •
After all the screws have been implanted, while the main surgeon shapes the rods, the assistant applies further stimulation before starting the correction manoeuvres.
The first patient in whom we identified a pneumothorax was before we started to use double stimulation. The second patient was when we were already using double stimulation. In our centre, all patients undergoing surgery for AIS remain in the postoperative resuscitation unit for 24 h where a chest X-ray is performed one hour after the end of the surgery.
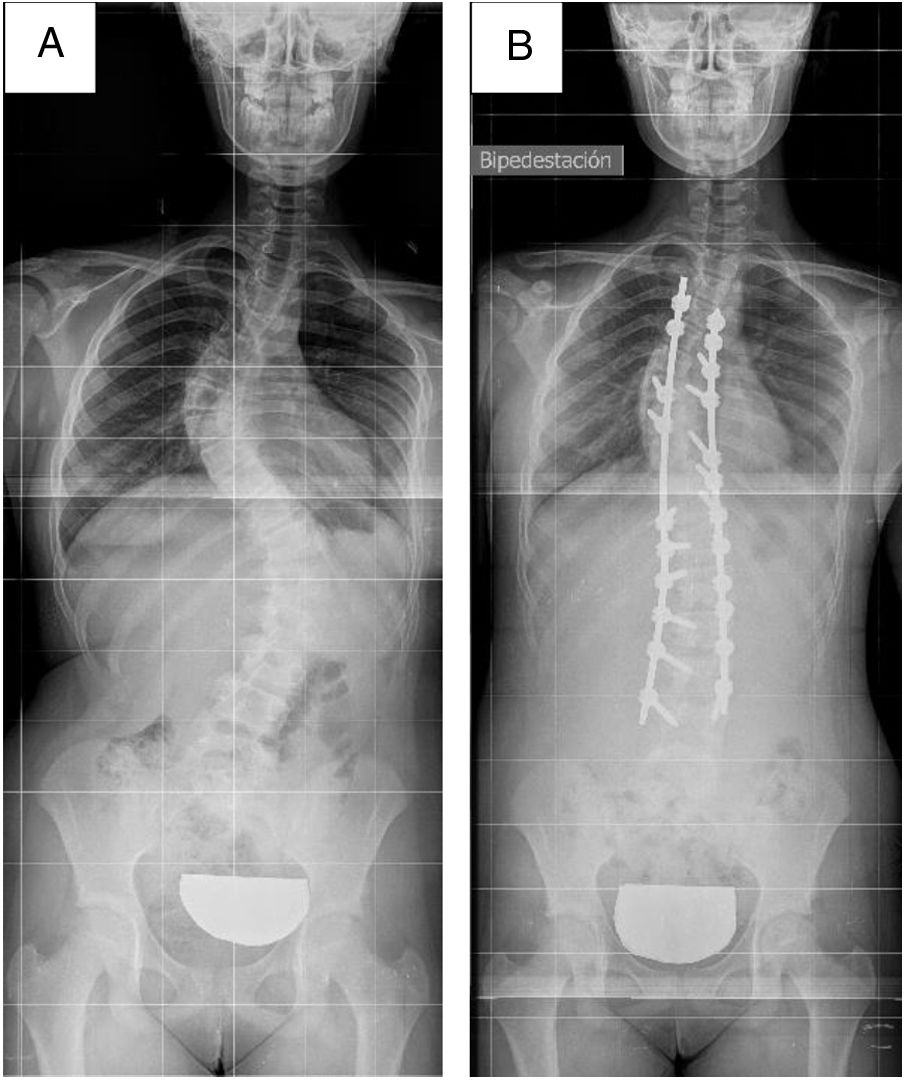
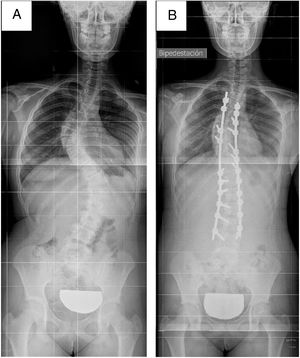
Patient 1A healthy 11-year-old female patient diagnosed with AIS Lenke 3CN8 (thoracic curve T4-T10 of 66° and lumbar curve T11-L4 of 63°) with no previous surgical interventions. She underwent Ponte osteotomies, correction and T4-L4 instrumented arthrodesis with autologous local bone and demineralised bone matrix.
In this patient, the thresholds were recorded after the screws were implanted, after the Ponte osteotomies were performed and after satisfactory anteroposterior and lateral fluoroscopy. Left thoracic PST (concavity) ranged from 12 to 20 mA. The left lumbar PST (convexity) exceeded 20 mA. On the right side, the lumbar PST (concavity) exceeded 15 mA while the thoracic PST (convexity) were 2 mA at T12, 3.5 mA at T11, 6 mA at T5, T7 and T8 and 8 mA at T4. These decreased PST were not accompanied by altered MEP or SSEP.
When low PST were recorded, the right thoracic pedicle screws were checked, and no breaches were identified on palpation. If an explanation for these values was not found, a surface stimulus was performed, as a test, on the transverse processes of T11 and T12, recording thresholds of 3 mA and 2 mA, respectively. In view of this finding and given the absence of alterations on palpation and radioscopy, we decided to consider the decrease in thresholds as a technical artifact and to continue with the surgery.
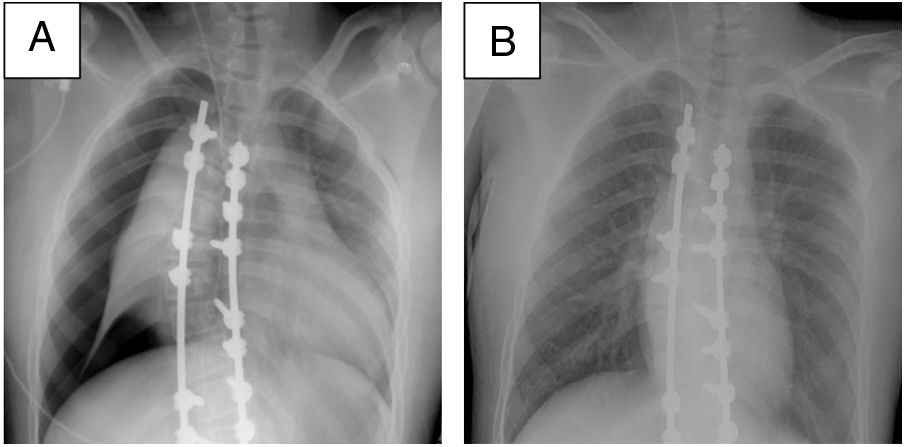
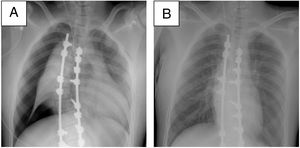
An episode of arterial hypotension was detected during the correction manoeuvres and surgical manipulation was stopped until blood pressure readings returned to normal. Once surgery was resumed, the patient remained stable until the end of the intervention and was extubated without complications. During the patient’s stay in the postoperative resuscitation unit, in accordance with the centre's protocol, a chest X-ray was performed revealing a right tension pneumothorax. We decided to place a chest drain, which was removed on the third postoperative day after resolution of the complication (Figs. 1 and 2).
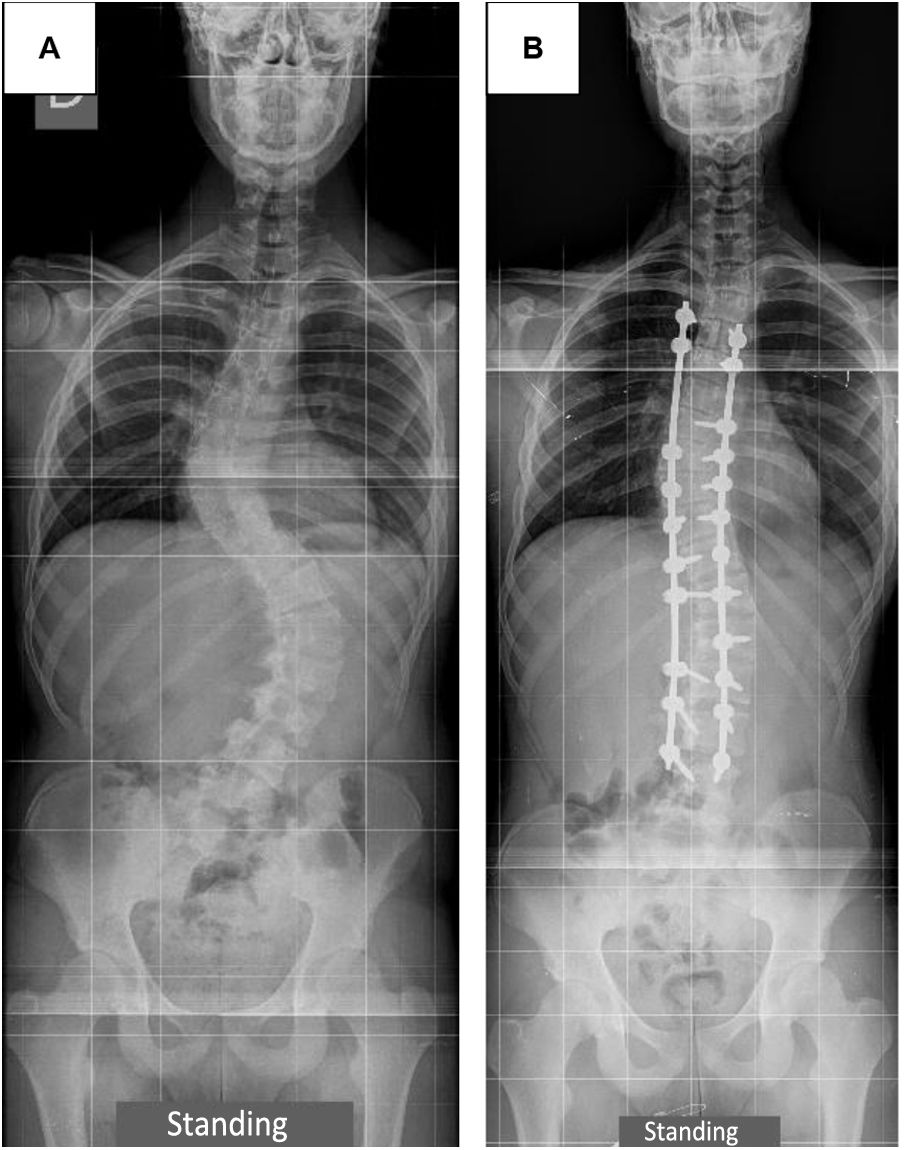
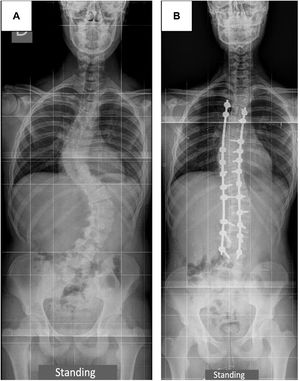
A 16-year-old male patient with no previous history of interest with a diagnosis of AIS Lenke 6CN8 (thoracic curve T4-T10 of 63° and lumbar curve T11-L4 of 69°, Risser 4) with no previous surgical interventions. He was treated with Ponte osteotomies, correction and T4-L4 instrumented arthrodesis.
Air aspiration was noted prior to the start of surgery, during placement of a central venous catheter. However, the patient remained stable throughout the surgery, showing no signs of pneumothorax.
Following our current protocol, the pedicle screws were stimulated on 2 occasions separated by a variable time interval. All lumbar PST ranged between 26 mA and 30 mA in the 2 stimulations, with no significant variations. Left thoracic PST (concavity) ranged from 16 mA to 50 mA, again with no significant variation. In the first stimulation, the right thoracic PST (convexity) recorded values between 15 mA and 50 mA. At the second stimulation, the PST remained stable at T9 and decreased by 15 mA at T4 and T5, 13 mA at T8, 3 mA at T10 and T12, and 1 mA at T11. Despite this general decrease in the right PST, the values remained above a pathological threshold (range 12 mA–37 mA). Due to the satisfactory radioscopic control, the correct palpation of the pedicle tract and the non-pathological values of the PST, we decided to proceed with surgery. There were no alterations in MEP or SSEP throughout the entire operation.
Decreased right PST and air aspiration at the access to the central line meant we had to rule out pneumothorax early, although the patient showed no haemodynamic alterations during the procedure. The chest X-ray confirmed the diagnosis of right tension pneumothorax. Clinical suspicion enabled early treatment with the implantation of a chest drain, which was kept in place for 48 h. The patient made satisfactory progress with no further incidents (Fig. 3).
DiscussionCorrection of deformity by instrumentation with pedicle screws is a widespread technique in surgical practice.1,2,4 However, it is not without risk. The proximity of vital structures makes it a priority to detect possible injury to these structures.
In this regard, INM has become mandatory practice as it facilitates the detection of iatrogenic neurological injuries in early stages. Although pedicle screw stimulation is systematically performed in this type of procedure, the range of threshold values to be considered susceptible to medial cortical perforation ranges from 5 mA to 10 mA in the literature.
In addition to neurological injuries, pneumothorax is another complication associated with AIS.2 Its detection requires a postoperative chest X-ray. The requirement for routine postoperative chest X-ray in patients undergoing surgery for AIS has been questioned recently,7 given the low reported incidence of pneumothorax in the literature.
This clinical note is the first to present the association between a decrease in PST and the onset of pneumothorax. In patient 1, we consider that the most likely cause of pneumothorax was a wide intertransverse dissection in the thoracic convexity. This complication had haemodynamic repercussions in the form of an episode of hypotension during the corrective manoeuvres. In patient 2, we believe that the pneumothorax occurred in relation to manipulation during central venous access and exposure to prolonged positive pressure from intubation. In this case, no haemodynamic disturbance was identified. Only the experience of the first patient with lower-than-expected PST resulted in clinical suspicion of pneumothorax and early resolution. If we had not had this suspicion, the chest X-ray would have been performed one hour after the end of surgery according to our centre's resuscitation protocol.
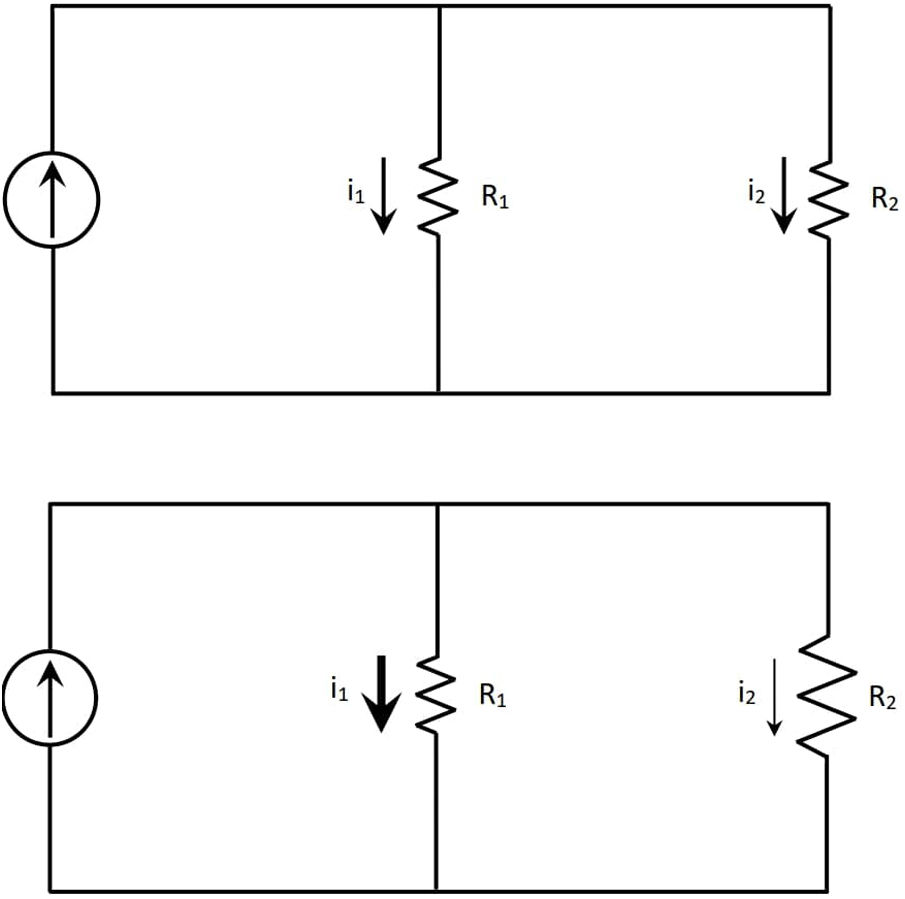
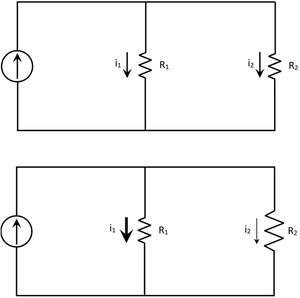
We believe that this alteration of the PST in the presence of a pneumothorax can be explained according to Ohm’s and Kirchoff’s laws. Resistance is the property of a material to resist an electric current.9 According to Ohm’s law,9 a current will flow through all available paths inversely proportional to the resistance offered by each of them. In the case of interest, the intensity of the generated pulse will flow through all the paths from the cathode to the anode. To simplify the interaction,10 we will consider 2 paths:
- -
Path 1: causing stimulation to the adjacent nerve root.
- -
Path 2: traversing all paths that would not cause stimulation of the nerve root (including those that pass through lung tissue).
When a pneumothorax occurs, the resistance of path 2 increases as the resistance offered by the air is greater than that of the lung tissue11 and, therefore, the current flowing through this path decreases. According to Kirchoff's first law,12 in order for all the intensity to return to the source, path 1 supports higher intensity causing the detection of root activation with lower intensity stimuli (decrease in threshold values) (Fig. 4).
ConclusionsA decrease in the threshold values of thoracic pedicle screw stimulation in patients undergoing surgery for AIS by posterior instrumentation with pedicle screws may be associated with the development of pneumothorax. This relationship and its mechanism have not been previously described in the literature. Our 2 cases suggest that in the presence of marked asymmetry in thoracic PST or unilaterally decreased thoracic PST, pneumothorax should be suspected, and early diagnostic methods (chest X-ray) and therapeutic measures (chest drain) should be considered.
Level of evidenceLevel of evidence V.
Please cite this article as: Madrid C, Gómez-Rice A, Cordón S, Sanz-Barbero E, Zúñiga L. Alteración en los umbrales de estimulación de tornillos pediculares torácicos secundaria a neumotórax en cirugía por escoliosis idiopática del adolescente. A propósito de dos casos. Rev Esp Cir Ortop Traumatol. 2021;65:471–475.