To determine the incidence of surgical site infection in knee prosthesis surgical procedure for a follow-up period of one year in twelve hospitals in Madrid region.
Material and methodA prospective study was carried out from January to December 2009 using a national surveillance system called Indicadores Clínicos de Mejora Continua de Calidad. Primary and revision knee joint replacements in patients operated on in the previous year were included. Criteria used to define surgical site infection and patient risk index categories were those established by the Centers for Disease Control and Prevention and National Nosocomial Infections Surveillance. The incidence rates were worked out crude and adjusted by hazard ratio.
Results2088 knee prosthesis procedures were analysed. The overall incidence of surgical site infection was 2.1%. Sixty-five percent of the infections were organ/space. Sixty percent of the infections were identified in the early postoperative period. Of all surgical site infections, 41.9% were microbiologically confirmed. Antibiotic prophylaxis was implemented correctly in 63.3% of the cases. The most important cause of inappropriate prophylaxis was an unsuitable duration in 85.7% of the cases. The presurgical preparation was carried out correctly in 50.3% of surgical operations. The incidence of knee arthroplasty infection was twice as high as in the National Healthcare Safety Network and similar to national rates.
DiscussionIn this study, the incidence of infection was within the range of infection rates in other published European studies. Surveillance and control strategies of health care for associated infections allow us to assess trends and the impact of preventive measures.
Determinar la incidencia de infección de localización quirúrgica en el procedimiento prótesis de rodilla, durante un año de seguimiento en 12 hospitales madrileños.
Material y métodoEstudio prospectivo de enero a diciembre de 2009, utilizando el programa Indicadores Clínicos de Mejora Continua de Calidad. Se incluyeron prótesis de rodilla primarias y de revisión intervenidas el año previo. Se utilizaron criterios de infección de localización quirúrgica y categorías por índice de riesgo de los Centros para el Control y Prevención de Enfermedades y del National Nosocomial Infections Surveillance. Se calcularon tasas crudas y ajustadas por índice de riesgo.
ResultadosSe analizaron 2.088 procedimientos quirúrgicos de prótesis de rodilla. La tasa global de infección de localización quirúrgica fue del 2,1%. El 65% de las infecciones fueron de órgano/espacio. El 60% de las infecciones se identificaron precozmente. Se obtuvo confirmación microbiológica en el 41,9% de los casos. La profilaxis quirúrgica fue adecuada en el 63,3%, siendo la principal causa de inadecuación su duración en el 85,7%. La preparación prequirúrgica fue correcta en el 50,3% de los pacientes. La tasa de infección en artroplastias de rodilla fue dos veces superior a la esperada según el National Healthcare Safety Network y similares a las tasas nacionales.
DiscusiónLa tasa de infección de nuestro estudio se encuentra dentro del rango de las tasas de infección descritas en otros estudios europeos ya publicados. Las estrategias de vigilancia y control de las infecciones asociadas a la asistencia sanitaria permiten evaluar tendencias y el impacto de las medidas de prevención.
The aim of knee arthroplasty is to restore knee function and relieve pain in patients who require this surgical treatment. This procedure has represented a significant health-care advance over the last few decades. Technological development, the progressive ageing of the population and prolonging the life of patients with underlying diseases increase the number of patients who are candidates for this type of surgery. Consequently knee replacement surgery is currently a common practise in the majority of Spanish hospitals.1–3
Although prosthesis infection is rare, it is the most important complication. It also has a great social impact as it is a serious adverse effect on the patient and carries considerable economic and welfare costs for the health system. Infections associated to health care mean an increase in morbidity; they lengthen hospital stays, increase diagnostic tests and the use of antibiotics. Knee revision due to infection is estimated to cost twice as much as for an aseptic one and triple or quadruple that of a primary total knee arthroplasty, and this is mainly due to prolonged and repeated hospitalisation.4,5
It was estimated that 450,000 knee arthroplasties were carried out in the U.S. during 2005. During the period 1990–2005, the increase in knee prosthesis was over threefold and the predicted increase for the year 2030 is between 7 and 8 times that. The percentage of knee prosthesis infection in 2005 was 1.4% and this complication determined 16.8% of arthroplasty reviews. It is estimated that the knee infection rate will be 6.8% for 2030.6
In Spain, the annual estimate for knee arthroplasties is 25,000, with a mean infection rate of 2.5%; the population with risk factors associated to the indication of arthroplasty is a patient group that is constantly growing.1,7 The main reason for knee prosthesis is indicated is osteoarthritis, affecting about 14% of females and 5.7% of males in Spain, which together with a longer lifespan and ageing of the population, make an increase for this type of intervention foreseeable.8 According to the EPISER study (a study of the prevalence of rheumatic diseases in the Spanish population), the prevalence of symptomatic knee osteoarthritis in Spain rises to 33.7% of people aged over 70 years old and it is estimated that 2% of people over 55 years old have severe pain in their knees that makes surgery their only option. In the work of Allepuz et al,8 knee arthroplasty rates between 1994 and 2005 showed an increase from 2.6 to 15.5 interventions per 10,000 inhabitants, with a yearly percentage change of 16.1% (CI 95%: 14.3–17.9) with an estimated cost for knee arthroplasty of €7000–8000.9
The aim of our study was to determine the incidence of surgical site infection in knee prosthesis procedures, for a follow-up period of 1 year in 12 hospitals in the Madrid area. This was attained from the data obtained using the national surveillance system INCLIMECC (Clinical Indicators of Continuous Quality Improvement).10 We analysed variables such as the degree of preoperative antibiotic prophylaxis and pre-surgical patient preparation.
Material and methodA prospective, observational study was carried out on a cohort of patients operated on for the same surgical procedure in 12 hospitals over a year, using the surveillance programme for hospital-acquired infection INCLIMECC. The study period was from the 1st January to 31st December 2009.
Study populationAll patients operated on for knee prosthesis procedures (Codes CIE-9: 00.80; 00.81; 00.82; 00.83; 00.84; 81.54; 81.55), who had been admitted for at least 48h, were included. The procedures included primary replacements carried out during the study period, as well as the readmissions due to reinterventions/ complications of the aforementioned surgical procedure during the previous year. There were 12 hospitals attached to the Madrid Health Service that provided the data, 10 of which were teaching hospitals. Hospital distribution by number of hospital beds was: 2 with more than 1000 beds, 3 with 501–1000 beds and 7 with fewer than 500 beds.
Data collectionData collection was carried out by nursing staff who belonged to the Preventative Medicine sector and had specific training for this. The collection was contrasted and validated by doctors from the Preventative Medicine sector.
The sources used were clinical histories, nursing notes, diagnostic techniques and microbiological results of tests performed on the patients, as well as the information supplied by the medical and care team of the areas surveyed. We used the hospital-acquired infection criteria established by the Centres for Disease Control and Prevention in 2008.11 We considered a surgical infection as any infection that occurred in the year following a surgical procedure with implants (prosthetic material). Surgical infections were classified as superficial, if they affected the skin and subcutaneous skin tissue, deep if they affected the deep soft tissues of the incision, and organ-space when the infection affected any part of the body different to that of the skin incision, fascia or muscle layers opened or handled during the surgical operation.
Surgical antibiotic prophylaxis was classified as adequate or inadequate according to each hospital's protocols as approved by their corresponding committees. Prophylaxis was considered inadequate by choice when the antibiotic used was different to that recommended in the protocol, inadequate by start-up when it was administered more than 60min before surgery or after it, inadequate by duration when prophylaxis was continued for more than 24h after surgery or inadequate due to the method of administration.10
Pre-surgical preparation of the patient is a set of measures applied routinely and according to each Hospital's own criteria, so as to reduce bacterial contamination of the patient's tissues. Such preparation includes, amongst other things, assessing whether the skin should be shaved at the surgical site, whether the patient bathes or showers the day before surgery and antisepsis of the surgical field. This was classified as correct if each hospital's current protocol was totally complied with, and incorrect if the protocol was not totally followed; patients were considered not prepared if they did not comply with all the requirements; and preparation was indicated as “no record” if there was no clinical history information.
A specially designed data collection file format was used, which included information on demographic variables, risk factors (intrinsic and extrinsic), surgical interventions performed, information on diagnosed infections and antibiotic treatment used. The information was transcribed onto a database of the INCLIMECC programme with a uniform structure for all the participating hospitals.
Data analysisIn the descriptive analysis of the population's characteristics and stays, we calculated absolute frequencies and percentages for the qualitative variables and mean and standard deviation for quantitative variables, using the SPSS 15.0 programme.
The National Nosocomial Infection Surveillance (NNIS) risk index is the ideal method to stratify and establish comparisons between surgical infection rates in each of the surgical procedures, as it combines known, demonstrated surgical infection risk factors. These include the degree of contamination in the surgery undertaken (clean, clean-contaminated, contaminated and dirty), the duration of the surgical procedure (percentile 75 of the duration of the intervention in minutes) and the patient's physical condition measured with the American Society of Anaesthesiology (ASA) anaesthetic-surgical risk score. Our patients were stratified into 4 infection risk levels using these criteria and the incidence of surgical infection in each group was calculated.12 The incidence of infection was defined as the number of new infections per 100 interventions during the study period. Crude rates, specific for each surgical procedure, and rates adjusted by the NNIS risk index were calculated.
A comparative analysis with the national and adjusted American rates by risk index was also carried out. For each procedure, we calculated the rate observed and the expected one according to the data published by the National Healthcare Safety Network (NHSN) and all those in the national INCLIMECC network (64 hospitals) were calculated by indirect standardisation.13 The ratio between the rate observed and that expected – standardised infection ratio (SIR) – is interpreted as a relative risk. It is the global indicator that the majority of authors suggest for comparison with reference standards, such as those published by the NNIS.14,15 This comparison was performed for the group of participating hospitals. Indirect standardisation was carried out with the Epidat 3.1 computer programme.
ResultsA total of 2088 knee prosthesis procedures were analysed, with 120min as the percentile 75 of the duration of the intervention. The percentage of patients operated on who were male was 24.6% and 75.4% were females, with a mean age of 71 years (±8 years).
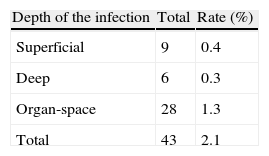
The global infection rate in the surgical site, which included primary and revision prosthesis, was 2.1%. There was 65% rate of organ or space infections. The surgical wound infection rate according to its depth is shown in Table 1. The distribution of the overall infection rate according to the number of hospital beds was 2.1% in hospitals with fewer than 500 beds, 1.5% in those with 501–1000 and 2.4% in those with more than 1000 beds.
Sixty per cent of infections were diagnosed in the first month after surgery. There was microbiological confirmation in 41.9% of cases (18/43), with staphylococci being cultivated in 61% of the isolated microbiologicals (11/18). There were 5 cases of Staphylococcus epidermidis, 3 of methicillin-resistant Staphylococcus, 2 of Staphylococcus aureus and 1 case of other Staphylococci.
A total of 1.6% of patients were operated on and they did not receive preoperative prophylaxis even though it was indicated. The percentage of adequate surgical prophylaxis according to indication, election of antibiotic, start-up, method and duration, with respect to all the patients receiving it was 63.3%. The main cause of antibiotic prophylaxis inadequacy was its excess duration, which occurred in 85.7% of cases. Other causes of inadequacy were produced by start-up in 8.6% of occasions, by antibiotic choice in 4.9% and by indication in 0.08%.
With regards to the pre-surgical preparation variable, the percentage of patients correctly prepared was 50.3%, there was no record for 47.8% and the rest were either not prepared for surgery or the preparation was incorrect.
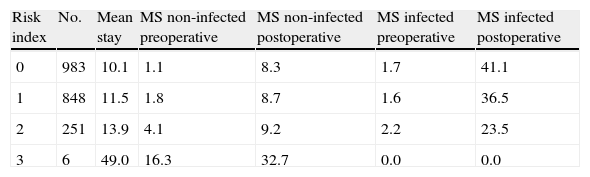
The mean stay of patients operated on for knee prosthesis was 10 days, and with a mean preoperative stay of two days. In patients who developed a surgical infection, there was a mean increase of 28 days in the postoperative stay. This postoperative stay was multiplied by 5 in the group of infected patients with a zero risk index and by 4 in the group one risk index. Table 2 presents the hospital stay by risk index for infected and non-infected patients.
Hospital stay by risk index (days).
| Risk index | No. | Mean stay | MS non-infected preoperative | MS non-infected postoperative | MS infected preoperative | MS infected postoperative |
| 0 | 983 | 10.1 | 1.1 | 8.3 | 1.7 | 41.1 |
| 1 | 848 | 11.5 | 1.8 | 8.7 | 1.6 | 36.5 |
| 2 | 251 | 13.9 | 4.1 | 9.2 | 2.2 | 23.5 |
| 3 | 6 | 49.0 | 16.3 | 32.7 | 0.0 | 0.0 |
MS: mean stay.
Revision surgeries represented 9.8% of the interventions and the rest were primary ones. In 88% of surgeries, the NNIS risk index was zero or one. The infection rates of the surgical site according to the NNIS risk index (0, 1, 2 and 3) were 1.9%, 2.0%, 2.8% and 0% respectively.
We observed an increase in the infection rate as the NNIS index risk increased. However, there were no infections in risk group 3, as this only included 6 patients.
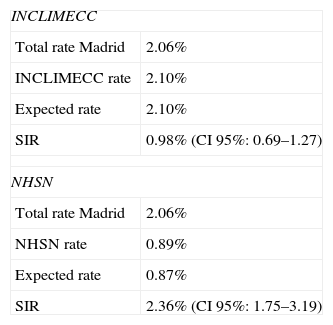
Table 3 presents the comparison between the infection rate in the participating hospitals from the Community of Madrid and those of the INCLIMECC group throughout Spain, as well as the comparison with the data published by NHSN. The overall infection rate in knee arthroplasties in the group of participating hospitals in the Community of Madrid was twice as high as expected according to the rates published by the U.S. surveillance system. Compared to the national data, the SIR was very close to one, given that the rates are practically the same.
Comparison of the infection rates between the hospitals in Madrid with INCLIMECC (Spain) and NHSN.
| INCLIMECC | |
| Total rate Madrid | 2.06% |
| INCLIMECC rate | 2.10% |
| Expected rate | 2.10% |
| SIR | 0.98% (CI 95%: 0.69–1.27) |
| NHSN | |
| Total rate Madrid | 2.06% |
| NHSN rate | 0.89% |
| Expected rate | 0.87% |
| SIR | 2.36% (CI 95%: 1.75–3.19) |
INCLIMECC: Indicators of Continuous Quality Improvement; NHSN: National Healthcare Safety Network; SIR: standardised infection ratio.
Infection associated to health care, defined as that which develops during the patient's hospitalisation, continues being an important problem in Spanish hospitals. The population with risk factors associated to the indication of arthroplasty (rheumatoid arthritis, diabetes, obesity, repeated replacements) is a growing group of patients that require and will require hospital care.1
Surgical infection is usually contracted during the intervention itself due to the contamination of the incision by micro-organisms from the patient's skin itself (endogenous source). Infections produced from an exogenous source are less frequent and more rarely do we find the source to be haematogenous, from a bacteria of any origin, which is why the probability of developing a prosthetic infection decreases as time elapses from the time of implant.16 In our analysis, 60% of infections were produced in the month after surgery. This is similar to other studies, where 71% of prosthesis infections appeared in the first 3 months.1
Infection risk appears with the skin incision and is greatest at the end of the intervention. Consequently, it is important to administer antibiotics before surgery, so as to maintain suitable concentrations in the tissues during the surgical procedure; as it is a procedure carried out with ischemia, it should not be necessary to repeat prophylaxis if the surgery is prolonged.17
The most frequent cause of inadequacy in our results was duration, by its prolongation. Given that surgical antibiotic prophylaxis (SAP) hopes to attain the best antimicrobial levels in the operative field, their use after the surgical incision is closed is unnecessary and does not report any benefits, whilst the prolongation of antibiotic prophylaxis can be an additional risk in developing bacterial resistance by providing excessive treatment.18 That is the basis for the importance of making SAP adequate to the protocol without prolonging doses unnecessarily, as well as minimising the number of patients who do not receive it even though it is indicated. Because of the aforementioned, we should not expect an improvement in the infection rate after correcting SAP inadequacy, which was previously for excessive duration. Even when excessive antibiotherapy is used, an infection should not occur from this incorrect practise, as the patient has antibiotic cover during the period of greatest risk.18 However, Herruzo et al.,19 found that the prolongation of prophylaxis multiplied the surgical infection site by 1.5 in a multivariate analysis of a sample of more than 7000 patients.
Pre-surgical preparation is one of the preventative measures for surgical infection that is carried out to reduce the infection risk, based on direct scientific evidence or on theoretical justification. In our study pre-surgical preparation was adequate in half of the patients intervened; this figure is possibly underestimated and would improve if it were correctly recorded in the clinical history. We find it extremely curious that the information is not recorded in 47.9% of interventions. To obtain this data we checked on the ward before surgery and in the patient's clinical history, but there was no specific record or it was not heterogeneous. This aspect will possibly improve with the implementation of surgical verification lists that encourage strategies relating to patient's safety.20
In our study, the general trend of the different hospital centres towards outpatient control before hospitalisation helped programmed admission, with a mean pre-surgical stay of 2 days. However, this can still be improved, as they are programmed surgeries.
In our data, surgical infection prolonged hospital admission, by increasing its duration 4 or 5 times. Consequently, any measures to reduce the infection incidence rate would also contribute to reducing the mean stay, together with its associated costs.
Every day there are a greater number of joint prosthesis interventions as there are more degenerative diseases, brought about by an ageing population and the changes in indication criteria, which seem to have expanded. There has been an increase in the number of candidates for this procedure given the good functional results, the significant improvement in pain and the technological advances that have made this intervention a therapeutic option increasingly less limited by age. For this reason, we recommend a surveillance system to assess prosthesis results.8,21
Knee prosthesis infection is a complication that very probably causes readmission, as it requires cleanup surgery and prosthesis removal. This adverse effect, attributable to a specific intervention, would be detected if there was continuous follow-up after surgery.18,22
Cumulative incidence is a nosocomial infection measurement that depends on the amount of surveillance after hospital discharge and this follow-up can vary amongst hospitals.23 We must also appreciate that there is a time-based criteria that would explain some of these discrepancies in the interpretation of prosthetic infection data. In surveillance, an infection is only considered nosocomial and recorded as such if the prosthesis-associated infection occurs in the year after the surgery; in contrast, with regards to care, all prosthesis-associated infectious processes after this time has elapsed would mean new hospital admissions, diagnostic tests, treatments and re-interventions for postoperative infection.11 Different authors have reported that 64% of periprosthetic infections appear the year after the surgery.24 Because of all this, we recommend that there should be surveillance of at least a year for certain surgical procedures and specifically in prosthesis surgery.
Although our study period was for a year, we included infections detected in arthroplasties carried out in the previous year. We therefore expect that the infection rates should compensate the follow-up of less than a year of some of the primary surgeries during the study period. In any case, the follow-up of this procedure continued in 2010 and its results can be compared later, assessing the possible effect of implementing certain preventative measures such as the surgical verification lists.
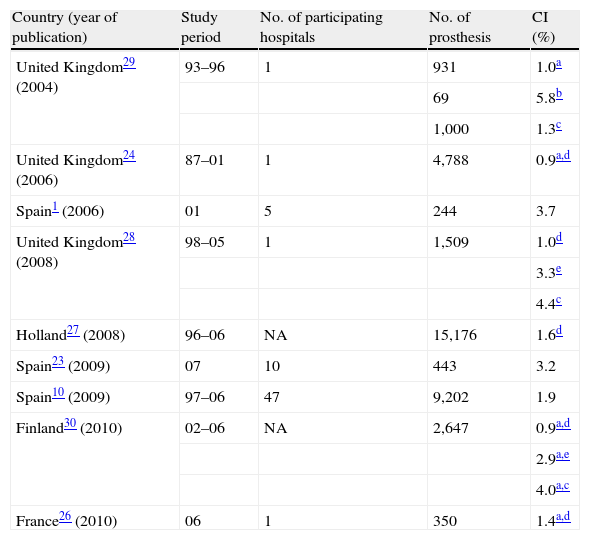
On the other hand, there is heterogeneity between the studies published according to the surveillance carried out between primary arthroplasties or if revision arthroplasties are included, such as is our case. This fact would mean an increase in rates, given that (as other authors have pointed out) infection in revision arthroplasties is greater than in primary1 because an intervention on a joint with a history of previous arthroplasty has been identified as an infection related risk factor.25 Another factor that would contribute to the variability between studies is that some infection data exclude superficial infection, which is included in our study.26 The hospitals mentioned in the scientific literature could vary in size, the population they care for and patient care practises.27–30 The infection rate in our study lies within the infection rate range described in European literature, as can be seen in Table 4.
Studies on the infection incidence rate in knee prosthesis.
| Country (year of publication) | Study period | No. of participating hospitals | No. of prosthesis | CI (%) |
| United Kingdom29 (2004) | 93–96 | 1 | 931 | 1.0a |
| 69 | 5.8b | |||
| 1,000 | 1.3c | |||
| United Kingdom24 (2006) | 87–01 | 1 | 4,788 | 0.9a,d |
| Spain1 (2006) | 01 | 5 | 244 | 3.7 |
| United Kingdom28 (2008) | 98–05 | 1 | 1,509 | 1.0d |
| 3.3e | ||||
| 4.4c | ||||
| Holland27 (2008) | 96–06 | NA | 15,176 | 1.6d |
| Spain23 (2009) | 07 | 10 | 443 | 3.2 |
| Spain10 (2009) | 97–06 | 47 | 9,202 | 1.9 |
| Finland30 (2010) | 02–06 | NA | 2,647 | 0.9a,d |
| 2.9a,e | ||||
| 4.0a,c | ||||
| France26 (2010) | 06 | 1 | 350 | 1.4a,d |
CI: cumulative incidence; NA: not available.
In our study, the micro-organisms most commonly isolated amongst infections with a positive microbiological result were Staphylococcus epidermidis and Staphylococcus aureus. This is similar to data provided by other studies.1,30
It is important for a health centre to know its own infection rates and the compliance level of the processes associated to them.18 The study of infection associated to health care is complex and requires a methodological approach that allows us to obtain reliable, representative and comparable information. Many of the infections associated to health care are preventable. The efforts to prevent them start by knowing about the main factors responsible for these infections and how to intervene to prevent or reduce the risk that they occur. Many of the prevention measures are not expensive and are generally less aggressive than what is involved in looking after a patient with an infection.6,19
FundingThe project was financed by the Ministry of Health of the Community of Madrid, within the grants for Autonomous Communities to implement National Health System strategies in Patient Safety of the Ministry of Health and Social Policy in 2009 (Royal Decree 16/06/2009).
Conflict of interestsThe authors have no conflict of interests to declare.
Evidence levelEvidence level IV.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
INCLIMECC Working Group of the Community of Madrid: Hospital de la Cruz Roja San José y Santa Adela: González Solana I, González Davicce E, Martínez Huedo MA, Rosales Statkus ME. Hospital Universitario Fundación Alcorcón: Rodríguez Caravaca G, Guillén Sierra MC, Arredondo Provecho AB. Hospital Infanta Leonor: de Juan García S, de la Hoz González C, Muñoz Sanz V, Zazo Morais L. Hospital Universitario de Fuenlabrada: García Puente E, de Arriba Guisande I. Hospital Universitario de Getafe: Sayalero Martín MT, Moreno Gomila C, Carrión Gil M, Fernández Vizoso MR, Guerrero Carmona J. Hospital Infanta Sofía: García Fernández C, Saa Requejo CM, Rodríguez Rodríguez V. Hospital Universitario de Móstoles: Vicente Pérez A, Valencia Martín J, Galindo Olmos C, García Contreras M, Martín López AM, Muñoz Rey E. Hospital Universitario 12 de Octubre: Jaén Herreros F, Alonso Fernández C, Calzada Mezquita F, Gil Martínez MP, Rabadán Doreste A, Torres Rodríguez JL, Sanz M. Hospital Universitario Príncipe de Asturias: Díez Pérez R, Rodríguez Navas ML. Hospital del Niño Jesús: Pérez Gorricho B, Soler Francés MV. Hospital Universitario La Princesa: Figuerola Tejerina A, Gálvez Parejo A, Gimeno Maestro J. Hospital Universitario Severo Ochoa: Martínez Mondéjar B, Motilla Martínez E, Fragoso de Castro P, Yepes Díaz MT. Hospital Universitario Ramón y Cajal: Monge Jodra V, Díaz-Agero Pérez C, Pita López MJ, Robustillo Rodela A, Gil Recamal A, Gómez Pizarroso P, Palancar Cabrera A, Valdeón García MA, Valencia Monreal H. Hospital del Sureste: Sainz de los Terreros Soler L, Saquete París RM.
Please cite this article as: Jaén F, et al. Estudio multicéntrico sobre la incidencia de infección en prótesis de rodilla. Rev esp cir ortop traumatol. 2012;56(1):38-45.
see Appendix A.