Clinical and functional outcomes of the knee after unicompartmental knee arthroplasty (UKA) and its correlation with lower limb mechanical axis correction.
Material and methodsWe have reviewed the outcome of 29 UKA, corresponding to 29 patients, with an average follow-up of 4.5 years (3–6 years). The distribution was, 21 women and 8 men, 11 unicompartmental osteoarthritis, 17 femoral condyle necrosis and 1 tibial plateau necrosis, and 27 medial versus 2 lateral affected compartments.
The clinical–functional situation of the knees was assessed through the Knee Society Score (KSS), and the mechanical axis through long standing film. To calculate the statistical non-parametric correlation between the different parameters, Spearman's coefficient was used.
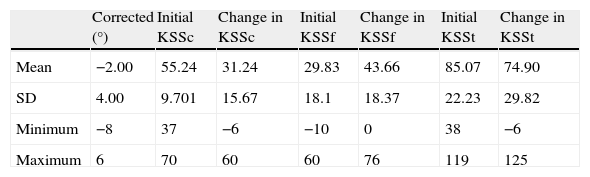
ResultsIn the last review, the increases in the mean clinical KSS and functional KSS were significantly different, with +31.24 (±15.7) and +43.66 (±18.4) points, respectively.
The mean change in the femorotibial angle was 2±4°. We did not find any correlation with statistical significance between the average increases obtained in KS scores and the alignment of the knee before and after the surgery; the thickness of the inserted polyethylene; the variation of the posterior tibial inclination; Insall–Salvati's index.
There was no statistically significant association between the variation in the total KS score and the type of implant or the surgical technique used.
ConclusionWe did not find any correlation between the clinical results and the radiological measurements in this population.
Valoración clínica y funcional de la rodilla tras artroplastia unicompartimental de rodilla (AUR) y su relación con la corrección del eje mecánico del miembro inferior y otros parámetros quirúrgicos.
Material y métodosHemos revisado la evolución de 29 AUR en 29 pacientes, con un seguimiento medio de 4,5 años (3–6 años). La distribución fue de 21 mujeres por 8 varones, 11 gonartrosis unicompartimentales postmeniscectomía por 17 necrosis condíleas femorales y 1 necrosis tibial, 27 AUR mediales y dos laterales.
Se evaluó el estado clínico-funcional de las rodillas intervenidas mediante el índice de la sociedad americana de rodilla (KSS) y los ejes mediante radiografía en carga y se calculó su correlación estadística.
ResultadosEn el último control, la ganancia fue estadísticamente significativa, en los índices KSS clínico (31,24±15,7) y en KSS funcional (43,66±18,4) puntos.
La corrección media del ángulo femorotibial fue de 2°±4°. No se encontró asociación significativa entre la variación en el KSS y el grado de alineación de la rodilla pre y postoperatorio, el grosor del polietileno elegido, la variación de la caída posterior tibial, el índice de Insall-Salvati ni el implante o técnica empleada.
ConclusionesSe observa la mejora clínica y funcional sin correlación con la corrección angular u otros parámetros quirúrgicos en esta serie.
Unicompartmental arthroplasty of the knee (UAK) is a method used when osteoarthritis in the knee joint is limited to one single femorotibial compartment. This orthopaedic technique involves replacing the joint surfaces of only one knee compartment—the external or the internal.
Because of its approach as a technique and as an implant, this type of orthopaedic solution has not been without ups and downs in its development, being fervently admired at some stages and, at others, rejected outright, as the current models were evolving. The revision rate for the first implants was very high (10% at 2 years).1 Series published during the 1980s reflected no decrease in the incidence of revisions, and it was only as of the 1990s that implant survival increased to values of 13–16 years for 90% of the implants.2 Between then and now, survival rates have reached figures of 81% at the 10-year follow-up3 for some prosthetic models—approaching those for total knee replacement (TKR)—thanks to steady improvements in implant design and manufacture, careful selection of patients, and refinement of the surgical technique.
The indications for this technique are quite strict: besides clinico-radiographic evidence that only one femorotibial compartment is involved, it is considered for non-obese patients with low functional demand who have an acceptable range of motion (minimum 5–90°) in one stable and normally aligned knee (maximum 15° of varus/valgus, passively correctable). For this reason, the majority of authors warn of the short-term risks of hypercorrection.4,5
The primary objective of this study was a pre- and post-operative, clinico-functional comparison of the patients who underwent unicompartmental arthroplasty of the knee on the Orthopaedic Surgery and Traumatology Service at our hospital between 2004 and 2008.
As secondary objectives, we examined the correlation between mechanical axis correction and the improvement obtained in clinico-functional scores, as well as other clinical and surgical aspects.
Materials and methodsThis was a retrospective longitudinal study that began with development of a protocol/survey to be filled out by each of the patients selected. The protocol contains information on the following: affiliation, anthropometric data (age, BMI, etc.), implants (size, technique), radiographic measurements (AP+LAT knee, ISI, Moore–Harvey, positioning, long X-rays of LE for mechanical and anatomical axes), KSS (clinical, functional, total), satisfaction, and conversion to TKR.5,6
The clinico-functional evaluation tool used was the Knee Society Score (KSS),7,8 which is accepted around the world for pre- and post-operative assessment of the knee.
All patients who underwent surgery during the study time frame (2004–2008) were assessed prior to surgery; afterwards, they followed the protocol for routine check-ups for this type of prosthesis, the study parameters being assessed at each visit. This protocol included at least 2 visits in the first year—the first one at 2–3 months and the second 1 year after the surgery; the remaining check-ups were annual. At these visits, just like the pre-operative visits, a medical history, physical examination, and X-rays were done on the patients.
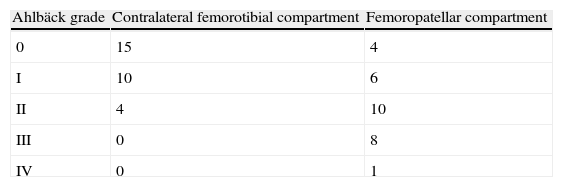
Twenty nine patients—21 females and 8 males, with a follow up between 3 to 6 years, were finally included in this study. The diagnoses were bone necrosis in 18 patients (17 femoral and 1 tibial) and osteoarthritis of the knee in 11 patients. The medial compartment was the one most affected, with 27 cases. As for patient assessments: knees with no symptoms of instability, minimum mobility of 5–95°, passively correctable deviations in the weight-bearing axis (measured by long standing X-rays of LE), radiographic osteoarthritis of the knee (asymptomatic) in the femoropatellar and contralateral femorotibial articulation (by anteroposterior [AP] and lateral [LAT] X-rays [XR] of the knee and axial patellar views), according to the Ahlbäck classification (Tables 1 and 2).
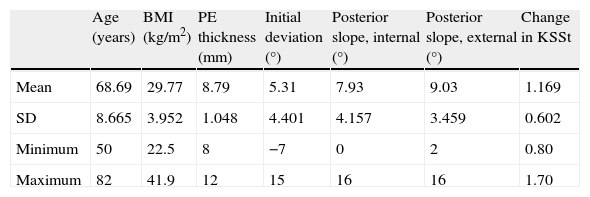
Characteristics of the patients operated.
| Age (years) | BMI (kg/m2) | PE thickness (mm) | Initial deviation (°) | Posterior slope, internal (°) | Posterior slope, external (°) | Change in KSSt | |
| Mean | 68.69 | 29.77 | 8.79 | 5.31 | 7.93 | 9.03 | 1.169 |
| SD | 8.665 | 3.952 | 1.048 | 4.401 | 4.157 | 3.459 | 0.602 |
| Minimum | 50 | 22.5 | 8 | −7 | 0 | 2 | 0.80 |
| Maximum | 82 | 41.9 | 12 | 15 | 16 | 16 | 1.70 |
Posterior slope: posterior tibial slope; SD: standard deviation; BMI: body mass index; KSS: Knee Society Score; PE: polyethylene.
In radiographic angle calculations, we used the Moore–Harvey method for posterior slope and the Insall–Salvati method for patellar height. We took the varus angle to be corrected as the initial deviation, assigning positive values for varus and negative values for valgus.
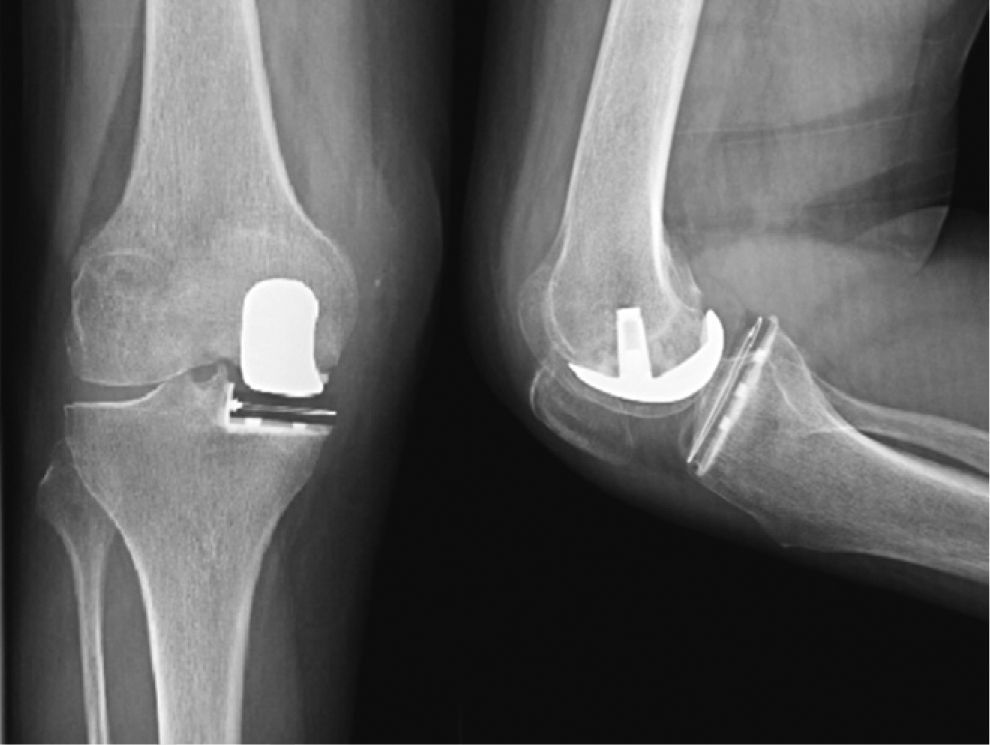
With regard to surgical technique,9 all procedures were performed with spinal anaesthesia and an ischaemia cuff at the root of the thigh; a mini-midvastus approach was used in all cases except in 2 cases with external compartment involvement, where an external parapatellar approach was used, the incision being made with the knee in 110° of flexion. Femoral reamers were used in the 8 cases where this technique was an option, and manual osteotomy under a cutting guide was used in the rest. The femoral components were cemented in all cases, and in the case of the tibia 10 metallic trays were implanted, 3 screwed and cemented and the rest cemented, per 19 polyethylene inserts all cemented. The same implant was used in all cases (ACCURIS, Smith and Nephew, Memphis, TN, US) (Fig. 1).
The statistical analysis was performed with the SPSS Statistics 19 computer system (IBM), and non-parametric tests, such as the Spearman's rho or the Mann–Whitney U test, were used because it did not follow a normal distribution. P values of <.05 were considered statistically significant.
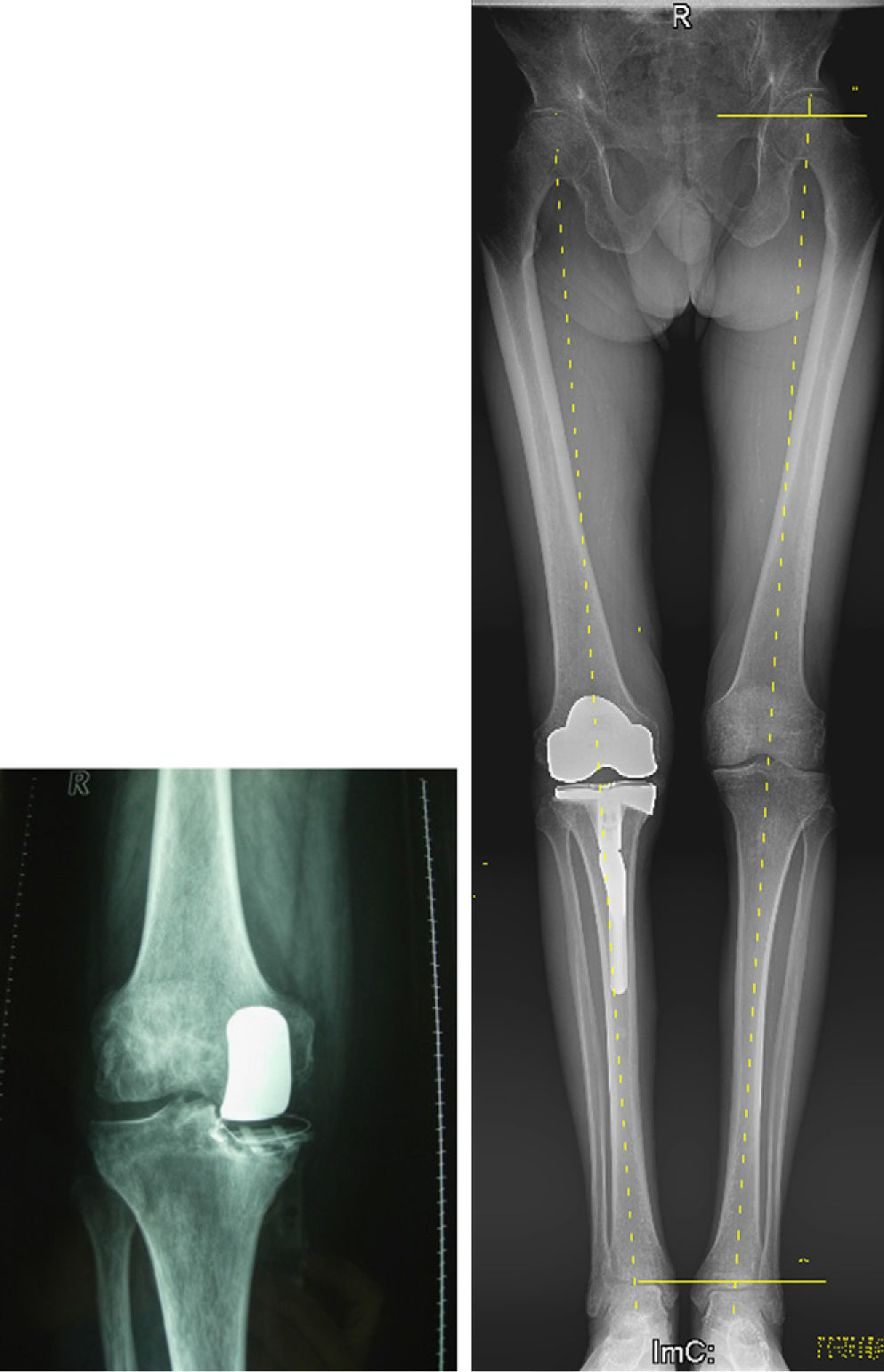
ResultsThe mean mechanical axis correction in the lower limb was 2° (±4), which gives us an idea of the surgeons’ limited attempts at hypercorrection—except in 1 case of a patient whose score was worse, where 8° of varus was reduced. The results obtained reflect a post-operative clinical improvement (P<.005) (primary objective) (Table 3).
Change in KSS following surgery.
| Corrected (°) | Initial KSSc | Change in KSSc | Initial KSSf | Change in KSSf | Initial KSSt | Change in KSSt | |
| Mean | −2.00 | 55.24 | 31.24 | 29.83 | 43.66 | 85.07 | 74.90 |
| SD | 4.00 | 9.701 | 15.67 | 18.1 | 18.37 | 22.23 | 29.82 |
| Minimum | −8 | 37 | −6 | −10 | 0 | 38 | −6 |
| Maximum | 6 | 70 | 60 | 60 | 76 | 119 | 125 |
SD: standard deviation; KSS: Knee Society Score.
During the immediate post-operative as well as the follow-up period, there were no infections or complications with the healing process.
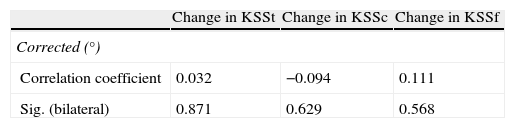
With regard to the secondary objectives, no statistically significant correlation was found (Spearman's rho) between the change in KSS and the degree of mechanical axis correction (Table 4).
With regard to the other secondary objectives, we also found no statistically significant correlations between the KSS values obtained and
- •
the diagnosis that prompted the surgery (P=.74) (Spearman's rho correlation coefficient: osteoarthritis of the knee=74.91±12.1 and necrosis=75.47±5.6);
- •
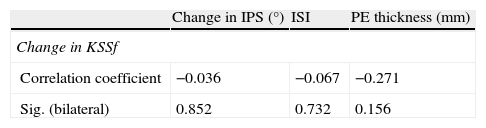
the thickness of the polyethylene insert (Spearman's rho correlation coefficient: −0.271±0.1);
- •
the posterior tibial slope (Spearman's rho correlation coefficient: −0.036±0.8);
- •
the patellar height per Insall–Salvati index (Spearman's rho correlation coefficient: −0.067±0.7);
- •
the body mass index (BMI) (Spearman's rho correlation coefficient: −0.061±0.7);
- •
the patient's age (Spearman's rho correlation coefficient: −0.074±0.7); or
- •
the surgical technique used (P=.4) (Table 5).
Table 5.Change in KSS and internal posterior tibial slope, Insall–Salvati index, and polyethylene thickness (Spearman's rho).
Change in IPS (°) ISI PE thickness (mm) Change in KSSf Correlation coefficient −0.036 −0.067 −0.271 Sig. (bilateral) 0.852 0.732 0.156 IPS: internal posterior tibial slope; KSS: Knee Society Score; PE: polyethylene; ISI: Insall–Salvati index.
Only 1 case required prosthetic revision during the study and follow-up period—a 76-year-old male patient who began to have steadily increasing pain 9 months after surgery. Clinical and radiographic evaluations revealed collapse of the all-polyethylene tibial component in the context of an aseptic loosening. Patient underwent a primary total knee replacement with posterior-stabilised prosthesis 13 months after the first surgery (Fig. 2).
DiscussionUp to the day the study was completed, having thoroughly searched the literature in the PubMed database, we found no review, research, or article analysing the hypothesis under which we began the study. However, some notable authors on the subject had made reference to some of our study's primary and secondary objectives.
Parratte10 affirms that KSS values and 12-year survival rates for arthroplasties in patients diagnosed with osteonecrosis are similar to those for arthroplasties in patients with osteoarthritis of the knee.
Hernigou11,12 describes how excessive tibial slope affects prosthesis stability and anterior cruciate ligament integrity, as well as patellar impingement. This author also warns of the association between hypercorrection and contralateral degeneration and an inferior functional outcome, even though, in that study, no reference is made to our objective, as is establishing how the degrees corrected in the mechanical axis affect the clinico-functional evaluation of the operated knee. Confirming the previous studies, Ritter13 states that hypercorrection will increase radiographic impingement, although this may not be a good predictor of the need for prosthesis replacement.
We have shown, however that patients experience a statistically significant improvement with this type of implant, as reflected in the post-operative KSS values being higher than the pre-operative values.
We were not able to demonstrate any of our study's secondary objectives, owing to the absence of statistical significance stemming from a very scattered distribution; this made us think that, even if we were to significantly increase the sample size, we would not obtain this correlation. This was so to such an extent that, in our sample, the arguments of the original hypothesis appear to behave as independent phenomena.
The mean mechanical axis correction was 2°—exactly what the surgical technique recommends; however, because there was no control group where this recommendation was not followed and the patients were overcorrected, we were not able to verify the true effect of excessive correction. There was a case where 8° of varus was reduced, however, and this patient, who underwent a greater axis correction, also obtained a worse score—so much worse that the global KSS calculated was 6 points lower than the pre-operative score (from 119 down to 113).14 This detail makes us suspect that, in reality, undue efforts to bring the limb into normal alignment through unicompartmental arthroplasty of the knee are doomed to failure. True, we can report only one single case, but it is a noteworthy case.
In series where the cases were carefully selected, the results obtained are similar to those in series with total arthroplasty in terms of satisfaction and survival, with reduced cost, lower morbidity, and shorter hospital stay, as well as greater mobility in the knee.
The reason for increased mobility and greater patient satisfaction is that this technique is more sparing of normal knee kinematics because the ligaments are kept intact.3
Having attempted to analyse the reasons for non-confirmation of the original secondary hypotheses, we can highlight (1) a small sample size, (2) limited follow-up, (3) intra-operative technical errors stemming from the steep learning curve initiated in 2004 for most of the orthopaedic surgeons who performed the arthroplasties in this study (11 surgeons for 29 prostheses), and (4) the few cases of hypercorrection or undue correction, greater than 3°.
Because of the resurgence in popularity of the unicondylar knee prostheses, basically owing to minimally invasive techniques,15–18 it is important to understand the advantages and drawbacks of this technique compared to those it competes with in terms of indications—total arthroplasty and high tibial osteotomy.
When the unicondylar technique is compared with total arthroplasty, 75% of patients feel that this knee is “more normal” than their contralateral total19,20; this is because only 1/3 of the knee is replaced, so it is closer to the normal knee, in terms of biomechanics, than in a total arthroplasty. There is also greater range of motion and less blood loss.
When unicompartmental arthroplasty was compared with tibial osteotomy, the results were significantly superior in terms of survival and patient satisfaction, with a follow-up of 3.5–15 years.21,22
The advantages of this type of prosthesis are a greater reserve of residual bone,23,24 a better mobility arc, less blood loss, and lower cost.25,26Among the drawbacks of this type of implant are poor instrumentation and design (pertaining more to the early models) and the failure of uncemented systems due to their poor fixation—the undersurface macrostructure design of tibial components is crucial to their ability to withstand shearing and eccentric weight-bearing. In turn, we cannot forget that unicompartmental prostheses have lower survival rates than total prostheses owing to multiple factors, such as (1) premature loosening of the tibial component, (2) the impact the femoral shield has on the patella—with anterior knee pain or compromise of the contralateral compartment, an early osteoarthritis developing—and, basically, (3) the need for accelerated prosthesis replacement using a primary total prosthesis and, in some cases, the need for revision.27–29
In conclusion, unicondylar knee arthroplasty is a solution that affords good functional results in patients with femorotibial unicompartmental involvement only—up to the 6-year follow-up, in our study. We must be very careful in selecting patients as well as in the surgical technique, for if both of these aspects are handled conscientiously, there will be significant, post-operative clinico-functional improvement. Seeking to bring the limb into normal alignment using this technique, at the cost of an undue correction of the mechanical axis, appears to be doomed to failure and even to deterioration with respect to the patient's initial condition. It appears that the initial diagnosis that prompted the intervention has no impact on the future clinical or functional progress of the patient's operated knee. The strict indications regarding the patient's age and BMI are the subject of controversy, while the other indications remain the same. Patellar height, posterior tibial slope, and implant thickness—provided that a minimum height is maintained—have proven to have no impact on functional progress of the patient who has undergone this procedure. In our hands, we obtain results with this technique that are similar to those published for wider series.
Level of evidenceEvidence level IV.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical DisclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Dr. Carlos Álvarez González, for his collaboration on the release of images for the patients treated.
Please cite this article as: Arguello-Cuenca JM, et al. Valoración clínico funcional tras artroplastia unicompartimental de rodilla. Influencia de la corrección del eje mecánico. Rev esp cir ortop traumatol. 2012;56(1):32-37.