Total hip arthroplasty (THA) using uncemented stems is a popular practice in the last decades.
The implant survivorship is critical and a less than 10% revision at 10 years is been proposed for commercialisation and use.
ObjectiveTo analyse the clinicoradiological results of an uncemented hydroxiapatite covered wedge stem with a 5 years minimum follow up.
Material and methodsProspective study, patients aged from 21 to 75 years were included. All patients received an Element stem (Exactech) and uncemented cup with crosslink poly and 32mm metal head, and posterior approach with piriformis retention was used.
Scheduled clinical and radiographic evaluation at 3 weeks, 3–6 month, year and subsequent years using Harris Hip Score and Merle d’Aubigné Postel. Intraoperative and during follow up complications were recorded.
ResultsOne hundred and fourteen total hip replacements in 104 patients: 54 females and 50 males (52%/48%). Follow-up of 5.7 years (range, 5–6.2years). Average age 56.8years (range, 42–75years).
Clinical evaluation the Merle d’Aubigné score improved 6.8 points and from the initial Harris Hip Score 47.3–93.1 points at last follow up.
Radiographic evaluation shows osteointegration in all stems. And in 6 cases (5.3%) at 3 months subsidence was detected, average 1.4mm (range 0–2.6mm) with no clinical manifestation, 3 cases of subsidence were associated to intraoperative fractures (1 greater trochanter and 2 in the calcar area, all resolved with wire cerclaje).
Subjective evaluation: 86 cases (82.6%) excellent, 9 patients (8.6%) good, 6 cases (5.9%) satisfactory and 3 cases (2.9%) poor. All poor results linked to the intraoperative complications.
No patient lost during follow up period.
No femoral pain dislocation or aseptic or loosening detected. All implants were in situ at last follow up.
ConclusionsThe radiological results confirm the benefits of this type of stem with good osteointegration.
The clinical and subjective results are promising.
With good surgical technical and without complications the risk of aseptic loosening should be absent or minimal.
La artroplastia total de cadera (ATC) con vástagos no cementados es popular en las últimas décadas.
La supervivencia de un implante es crítica, con una tasa de revisión menor al 10% a 10años como límite para su aceptación y comercialización.
ObjetivosAnalizar los resultados clínico-radiográficos con un vástago en forma de cuña no cementado con recubrimiento completo de hidroxiapatita (HA) y con seguimiento mínimo de 5 años.
Material y métodosEstudio prospectivo. Utilización de vástago Element (Exactech) y copa no cementada con inserto crosslink pared posterior elevada y cabeza metálica de 32mm. Se realizó un abordaje posterolateral con retención del músculo piriforme.
Seguimiento clínico a las 3 semanas, a los 3 y 6 meses, al año y años subsiguientes.
Evaluación radiográfica base en el postoperatorio inmediato y comparación con los controles. Se registraron las complicaciones intraoperatorias y en los seguimientos.
ResultadosCiento catorce ATC en 104 pacientes: 54 mujeres y 50 hombres (52/48%), con seguimiento de 5,7 años (rango, 5-6,2 años) y con 56,8 años de promedio de edad (rango, 42-75 años).
Evaluación inicial score Merle d’Aubigné pobre con mejora postoperatoria de 6,8 puntos. Score de Harris inicial de 47,3 puntos y, a la última consulta, de 93,1 puntos.
Evaluación radiográfica: osteointegración de todos los vástagos. Hundimiento: 6 casos (5,3%) a 3meses de cirugía, promedio de 1,4mm (rango, 0-2,6mm) sin repercusión clínica hasta la actualidad.
En 3 casos de hundimiento hubo fracturas intraoperatorias: una del trocánter mayor (se realizó un cerclaje tipo mochila) y 2 por fractura proximal en el área del calcar (tratadas con cerclaje circular).
Evaluación subjetiva: 86 casos (82,6%) excelente, 9 pacientes (8,6%) buena, 6 casos (5,9%) satisfactoria y 3 casos (2,9%) pobre. Los resultados pobres coincidieron con pacientes que tuvieron las complicaciones mencionadas.
No se detectó dolor femoral anterior. No se produjeron luxaciones o aflojamientos sépticos. No hubo pérdida de pacientes en el período de seguimiento. Todos los implantes se encuentran in situ al momento del último seguimiento.
ConclusionesLa evaluación y el seguimiento radiográfico confirman buena osteointegración del vástago. Los resultados clínicos y subjetivos son prometedores. Con una buena técnica quirúrgica y sin complicaciones, el riesgo de aflojamiento aséptico impresiona ser mínimo o ausente.
Total hip arthroplasty (THA) has greatly evolved since its introduction by Sir John Charnley in 1959, and has become the most successful procedure of orthopaedic surgery. At present each year a million patients receive a THA.1
Throughout this time stem designs and cementation techniques have changed and as a result there has been an improvement in surgical outcomes of primary surgery at 10 years, with a drop in revision of the initial technique from 19% to under 1% with polished stems and the modern cementation technique being a mixture of using vacuum, gun cementation, pulsed lavage pistol and centralisers.2
The concept of cementless fixation arose from an attempt to reduce the rate of loosening (Morscher)3 with the appeal of obtaining a direct union of the bone implant (biological attachment) and long-lasting stability.
Depending on the design and elastic properties of an implant pressures will be transmitted. The concept of a wedged stem is intended as fixation in a metaphysary area and the reduction of the possibility of stress shielding with loss of bone stock. Full coverage with a hydroxiapatite (HA) with osteoinductive properties and with new trabecular bone formation4,5 compensates for the possible imperfect femoral canal fill, achieving a stable fixation even in the presence of initial micromovements and good clinical and radiological outcomes.6–9
The survival of an implant is critical, and guidelines published in the United Kingdom recommend a revision rate of 10% at 10 years as the limit to their acceptance and production.9 In accordance with these criteria, national registers in other countries (Scandinavia, Australia, FDA) carry out the follow-up of implants and their performance.
We must remember that new implants are constantly being produced, at the rate of approximately 5 new designs per year. Surgeons are faced with a wide range of stems without sufficient clinical results and follow-up to be able to take an evidence-based decision on them.1,9–11
ObjectivesThe aim of our study was to analyse the clinicoradiological results of an uncemented hydroxiapatite covered wedge stem with a 5-year minimum follow-up.
Material and methodsA prospective study of hip prosthesis from operations performed in our hospital using an uncemented wedge stem with full HA coverage, of Novation Element® (Exactech, Inc, U.S.A.) type, with a minimum 5-year follow-up.
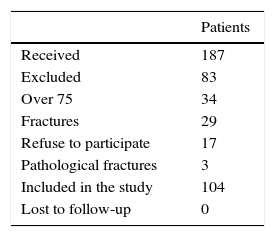
Inclusion criteria were patients aged between 21 and75 years with primary arthrosis, osteo/avascular necrosis and with no previous hip operations. Exclusion criteria were: patients aged over 75, patients with fractures, tumour disease or metastasis and patients who did not wish or could not attend follow-up sessions (Table 1).
During the study period, we carried out 114 THA on 104 patients: 54 women and 50 men (52%/48%), with a follow-up of 5.7 years (range: 5–6.2 years). Mean age was 56.8 (range: 42–75years).
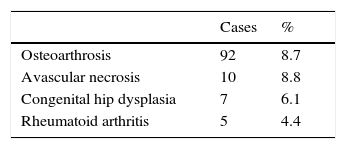
Initial diagnoses were arthrosis, avascular necrosis, dysplasia of the hip and rheumatoid arthritis (Table 2).
The operations were performed in a single institution by surgeons exclusively dedicated to hip surgery and with a common approach.
All patients agreed to participate in the study and signed specific consent form for the procedure and study.
With regard to antibiotic prophylaxis, all patients received 1g of cefazolin, which was administered every 8h for 24h. In patients allergic to this drug vancomycin was administered, 1g every 12h from 24h after surgery. A posterolateral approach was used with piriformis retention and reinsertion of the cup and short external rotators (complete flap) using the Pellicci12 technique during closure. The acetabular component chosen was uncemented, modular, line to line, and with highly crosslinked polyethylene with 10 posterior rim. 32mm cobalt chromium heads were used.
All the patients received prophylaxis for thromboembolic disease. 220mg of dabigatran was administered for 30 days after surgery.
Excepting contraindication, physiotherapy began on the first day after surgery, with sitting and walking exercises with a frame or sticks, depending on the functional ability of each patient, and following a protocol of accelerated rehabilitation.
Check-ups with X-rays were programmed 15 and 45 days after hospital discharge and subsequently at 3 and 6 months and then annually.
Intraoperative, hospital stay and follow-up complications were recorded.
Clinical and radiographic study methodsClinical assessments according to the Merle d’Aubigné Postel scale modified by Charnley13 and Harris Hip Score,14 for pre and postoperative assessments.
A subjective assessment was also carried out on personal patient satisfaction, referring to their overall appreciation of the procedure and their expectations of it, on a scale of 1–10, where a score of 1–3 was a poor outcome, 4–5 was satisfactory, 6.8 good and 9–10 excellent.
Radiographic evaluationAssessment of the acetabular cup was made but was not the main aim of this study. The pre and postoperative X-rays were digital and standardised for magnification in 1.2 corresponding to the preoperative planning templates used. The focus was on the pubic bone. We proceeded with a serried radiographic assessment with measurement of the following parameters:
On an acetabular level:
- •
Acetabular inclination angle.
- •
Appearance of radiolucent lines (DeLee and Charnley areas).15
- •
Cup migration (defined by the variation of over 5 degrees).16
- •
Screw breakages.
The acetabular component was considered integrated in accordance with the non appearance of signs of loosening, progressive radiolucent lines, screw breakage and migration.16
On stem level:
- •
Osteolisis (progressive localised reabsorption or endostal erosion).17
- •
Calcar reabsorption.17
- •
Presence of radiolucent lines.18
- •
Cortical hypertrophy.17,18
- •
Subsidence (comparing the distance from the stem shoulder to the lesser trochanter).19,20
- •
Pedestal formation l and appearance of heterotopic ossifications.
- •
Subsidence was considered to have taken place with progression after its detection in 3 serial X-rays. For definition of fixation Engh21 criteria were used.
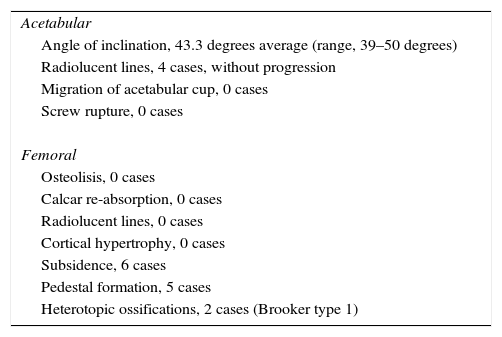
Comparative radiographic assessment based on X-ray obtained in the immediate postoperative period showed osteointegration of stems in all follow-up periods. Subsidence was detected in 6 cases (5.3%) within the first 3 months after surgery, with an average of 1.4mm (range from 0.1 to 2.6mm) with no clinical repercussions to date and patients are continuing with periodic reviews. In 3 cases where subsidence presented intraoperative fractures were detected: one due to a greater trochanter injury (wire “back-pack” type cerclage was performed) and two due to a proximal fracture in the calcar area (treated with circular cerclage). In 3 cases a reduction of weight-bearing during the rehabilitation period was made up to 4 weeks after surgery (Table 3).
Radiographic evaluation.
| Acetabular |
| Angle of inclination, 43.3 degrees average (range, 39–50 degrees) |
| Radiolucent lines, 4 cases, without progression |
| Migration of acetabular cup, 0 cases |
| Screw rupture, 0 cases |
| Femoral |
| Osteolisis, 0 cases |
| Calcar re-absorption, 0 cases |
| Radiolucent lines, 0 cases |
| Cortical hypertrophy, 0 cases |
| Subsidence, 6 cases |
| Pedestal formation, 5 cases |
| Heterotopic ossifications, 2 cases (Brooker type 1) |
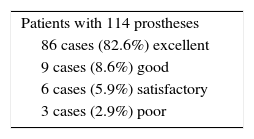
Subjective assessment results were as follows: 86 cases (82.6%) excellent, 9 good (8.6%), satisfactory (5.9%) and 3 poor (.29%). The poor results coincided with the patients who had the before-mentioned associated complications (one greater trochanter fracture and two proximal calcar fractures) (Table 4).
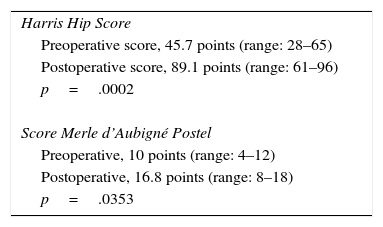
The Harris Hip Score and Merle d’Aubigné Postel scale results are contained in Table 5.
No anterior femoral pain was detected. There were no luxations or septic loosening in any components. No patients were lost to follow-up. All implants were in place at the last follow-up review.
DiscussionProsthesis designs have improved in shape and coating and as a result the use of uncemented materials in THA is increasingly greater for a larger number of patients.1,9–11 Not all uncemented stem designs are optimal or achieve similar outcomes. There is great interest in determining early markers of failure to rapidly limit the use of designs offering poor results.
In the case of the wedge stem we present, primary fixation is in the metaphysic due to shape and self-blocking properties. As a result the axial load becomes radial and the compressive strength transfers the load in a more balanced manner in the proximal metaphysic. Stress shielding is thus limited, as is anterior femoral pain secondarily.22,23 The joint space is also sealed, blocking the migration of particles and preventing proximal osteolisis.
Wedge-shaped designs are associated with high long-term rates of success. Good function and clinical tolerance have been recorded with a varied degree of subsidence.10,15,16,24,25
Coating the uncemented stems with HA was proposed in order to take advantage of the oseinductor ability and ensure rapid osteointegration with the generation of bone joining the femoral stem without the formation of fibrous tissue and thereby providing stability and duration in the long term.23–25 Several studies have shown that bone union occurs during the first 3 months and persists over time, even with the disappearance of the HA coating or the inclusion of it in the newly formed bone.23
Survival rates with complete HA coating are excellent. In the Norwegian Arthroplasty Register 1987–200410 the rate was <1% of revisions at 4.5 years and 2.4% revisions at 10 years achieving a result of 4.9% revisions at 15 years out of a total of 5130 implanted stems.
This result of a survival rate of 95.1% at 15 years is comparable to the best of cemented stems examined to date.10
In wedge-shaped stem design with full hydroxiapatite coverage, Pellegrini et al.26 achieved 2% revisions at 6.5 years and Hozack et al.27 obtained 100% fixation, with 98% of patients pain free. In the case of the Bicontact® stems and the modified Zweymuller® design, 97.6% and 96% survivorship were reported respectively at 10 years.28,29
Radiographic assessment may reveal osseous radiographic signs of re-adaptation and failure following the implant of an uncemented femoral stem. On observation of these signs and above all, with the comparison of periodic studies it may be defined whether a prosthesis is stable with bone growth, stable with fibrous growth or unstable. Engh et al.21 described the signs of osteo integration classifying them into greater or lesser. The absence of radiolucency around the implant, atrophy or rounding of femoral calcar and the presence of welding area or bony bridges between the stem and the endosteum mark good osteointegration but these criteria were described for full coverage, cylindrical stems. To define the case of the stem which we used we would have to add the finding of progressive demarcation of the implant-bone interphase, subsidence of the implant with progression over time and the re-absorption of the femoral calcar area. The design has an excellent correlation with surgical findings and the presence of visible signs of failure from an X-ray concurred with the real situation of the implant.
Furthermore, the observation of these signs has predictive value if they early enough. Khalily et al.29 have demonstrated the presence of radiolucency around the porous area of the stem provide 100% sensitivity and 55% specificity in prediction of future revision surgery for the next 8 years.
Systematic follow-up and control mean that information may be acquired regarding the behaviour of implants and provide information for making decisions about use, and for early detection of failure.29,30
Since fixation design and method of THA determines stability which consequently has an influence on implant survival, the problem currently existing is that many new implants are introduced onto the market without having proven good performance (Sheth et al.31). This has led to the suspension in usage of implants with extremely high levels of failure, such as the Charnley Elite Plus®, or the metal-on-metal surface prosthesis (Hauptfleisch et al.32).
In order to prevent disasters of this type of situation occurring, national guidelines and registers for patient protection have been developed.1,9–11 An analysis also needs to be made regarding the practice of phased introduction into the pharmaceutical sector, with small controlled groups to detect early indications of failure, as suggested by McCulloch et al.33 and Schemitsch et al.34
Stem subsidence has been suggested as an early prognostic factor of loosening,35,36 with 1.2mm in Roentgen steriophotogrammetric analysis (RSA)studies and ≤1.5mm measured with EBRA37 or ≤2mm with digital radiographies and ad hoc software.36,37 The results obtained in our series, with a mean subsidence of 1.4mm, are within the expected and acceptable range according to the literature, to prevent late aseptic loosening. Furthermore, the detection of subsidence in only 5.5% of cases, without progression in follow-up 3 months after surgery, suggests that the prostheses are self-stabilising due to their wedge shape and the implant-bone union induced. Also, initial fixation in the other patients was not affected.36–39
In a review of the literature regarding stem subsidence at 2 years follow-up, White et al. reported values of 0.29 to 4.5mm±1.5mm.40
Campbell et al.24 reported subsidence values of 0.58mm at 2 years with the use of the Corail® (DePuy, U.S.A.) stem during the first 6 months of implantation. We should point out that a similar pattern was found in our cases during the first 3 months after surgery, but without any progression or appearance of new cases. These data appear to be linked to the low incidence of initial subsidence with a good rate of long-term implant survival. It is important to add that 2 out of 6 cases which presented with subsidence had fractures during implantation which were successfully treated with cerclage. Partial weight-bearing entailed during the 45 days of physiotherapy after surgery. To date none of the patients have reported any pain or any reduction in their everyday activities.
This review of the outcome of a specific femoral implant underlines the need to provide series offering this type of information to contrast with the data only available from today's arthroplasty registers.24,33,34
The guidelines from the United Kingdom9 recommend a revision rate of ≤10% at 10 years for uncemented stems as the cut-off number for not using a particular stem. In our series there was no revision surgery at 5 years of follow-up and this is consistent with that suggested by international guidelines.9–11
The survival mean obtained in our series is comparable with other high survival stems,38 such as CLS Spotorno®11,17,41,42 and Corail®10,11,40–42 and even better than the 8% reported with LCU Link.®11,38,42
Clinical outcomes are promising, with 91% excellent or good satisfaction in subjective evaluation. There was a considerable improvement in function, reflected in the scores evaluated and non patients stated they suffered from pain in the femoral diaphysis as have been reported in similar designs, such as Corail® or LCU Link.®40–42
With regard to modification of Harris14 and Merle d’Aubigné Postel13 pre and postoperative function scores, statistically significant improvements were observed.
At the date of the last follow-up revision, no patients had been lost to the series, nor had there been any revised implants.
LimitationsThis study is a prospective, non comparative work and follow-up is mid-term. Our advantage was that the operations were performed by a team solely dedicated to hip replacement surgery.
Conclusions- 1.
Evaluation and radiographic follow-up confirmed the benefits of this type of uncemented stem design with good osteointegration.
- 2.
Clinical and subjective results of patients with excellent and good scores are promising.
Evidence level IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Godoy-Monzon D, Buttaro M, Comba F, Zanotti G, Piccaluga F, Neira-Borrajo I. Resultados de un vástago con cobertura completa de hidroxiapatita con un seguimiento mínimo de 5 años. Rev Esp Cir Ortop Traumatol. 2017;61:390–396.