Complications secondary to oxygen-ozone therapy are rare, but they have been described in medical literature. There are only two cases of infectious complications after oxygen-ozone therapy. Our aim is to describe a rare case of purulent complication that was secondary to oxygen-ozone therapy for the treatment of lower back pain. We report the clinical improvement with conservative treatment for a local complication after percutaneous oxygen-ozone treatment. According to the clinical improvement of our patient, conservative treatment should be considered before any aggressive surgery.
En la literatura médica se han descrito un número escaso de complicaciones secundarias al tratamiento con ozonoterapia, habiéndose descrito únicamente 2 casos de índole infeccioso tras la terapia percutánea con ozonoterapia. Presentamos el caso de una complicación infecciosa secundaria a ozonoterapia para el tratamiento de una lumbalgia crónica, así como la posterior evolución clínica con tratamiento antibiótico y drenaje de los abscesos. Según la mejoría clínica de la paciente, se deben agotar las posibilidades menos invasivas antes de cualquier cirugía agresiva.
Back pain is one of the most common problems worldwide. Nearly 70% of adults suffer from back pain at some point during their lives and most cases do not have any recognizable cause in imaging studies. Instead, it is usually attributed to muscle or ligamentous lesions.1,2 Percutaneous injections and surgery are the optional treatments once pharmacological treatments and rehabilitation have failed.3 Few complications have been reported after percutaneous treatment with ozone. We present a new complication following percutaneous oxygen-ozone therapy, as well as the clinical outcome following treatment with antibiotics and percutaneous drainage.
Case reportThe patient was a 54-year-old woman who had no medical history of interest. Due to acute, right, lower back (or lumbar) pain, which was unrelated to physical exertion and trauma, she began treatment with corticosteroids and paravertebral percutaneous oxygen-ozone therapy. After 6 cycles of lumbar paravertebral injections of oxygen-ozone therapy, the patient reported a significant clinical improvement. Two months later, the patient returned to the emergency department of the hospital due to right lumbar pain radiating to the left lower limb, with a duration of 5 days. Physical examination found an antalgic posture with flexion of the right lower limb, pain upon pressure on the right paravertebral muscles from L2 to the sacrum, and negative bilateral Lasègue. Laboratory tests revealed leukocytosis (18.800μl) and elevated C-reactive protein (18.81mg/dl).
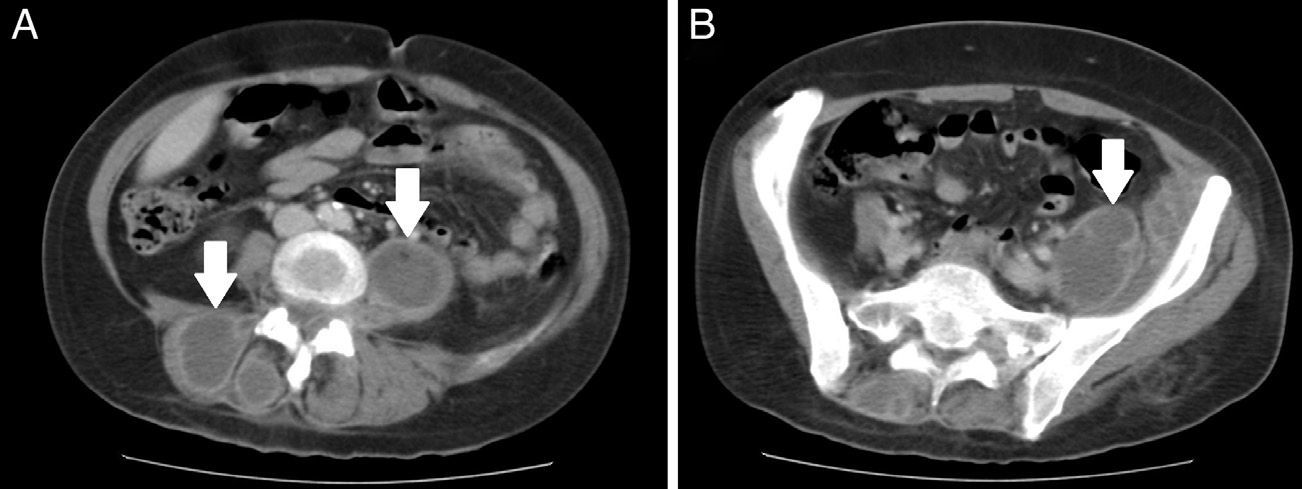
ResultsAn ultrasound scan found the presence of a right lumbar, hypoechoic lesion along the paravertebral musculature, with dimensions of 2.8cm×16cm at the sacral level. A computed tomography (CT) scan showed a lesion with peripheral contrast uptake that extended along the left iliopsoas muscle and a right paravertebral mass with similar characteristics, consistent with an abscess or hematoma (Fig. 1). After placing 2 ultrasound-guided percutaneous drainages under local anesthesia, the material obtained through puncture was referred for culture and antibiogram, and empiric antibiotic treatment with metronidazole and gentamicin was initiated. Cultures of the infected focus showed Gram-positive cocci, with presence of methicillin-sensitive Staphylococcus aureus, so we continued treatment with 1g of intravenous cloxacillin every 6h.
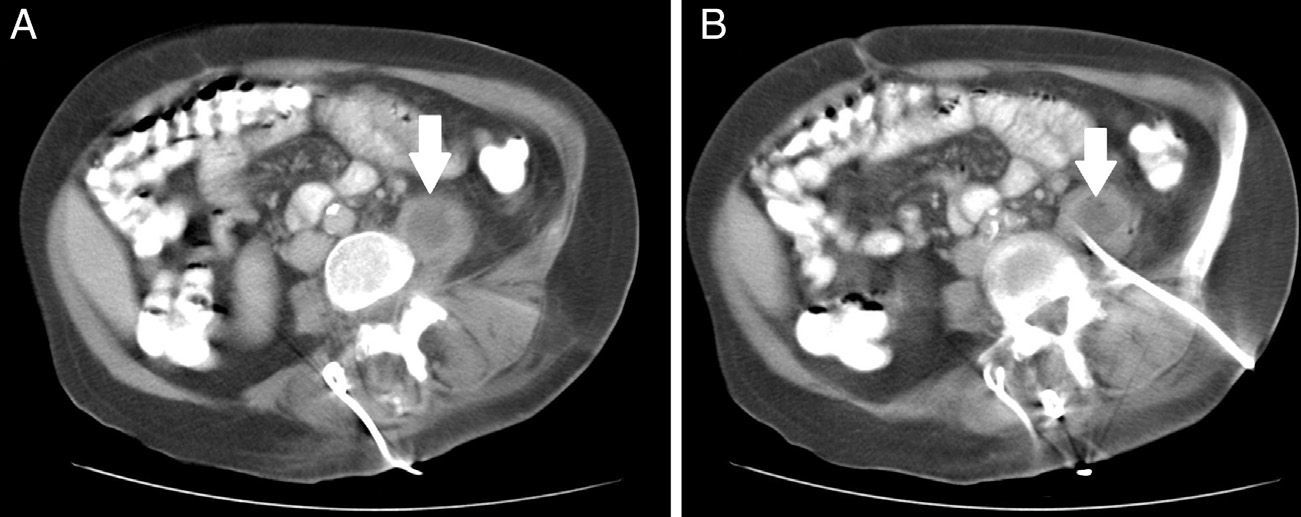
Ten days after starting treatment, a new CT scan showed the disappearance of the right, posterior, paravertebral collection, as well as a significant reduction of the abscess in the left iliopsoas muscle (Fig. 2). After another 15 days, a new CT scan confirmed the resolution of the abscess in the iliopsoas muscle. Three months later, the patient is asymptomatic.
DiscussionOxygen-ozone therapy has become an alternative or additional treatment option for patients with low back pain,1,2 although there is a low level of evidence to support its use because there are very few high-level studies which have demonstrated its superiority in subacute and chronic back pain.4 There are several mechanisms of action which explain the effectiveness of ozone, such as analgesic, anti-inflammatory and antioxidant action on proteoglycans.2,3,5 The therapeutic effects of intradiscal ozone administration include reducing the volume of disk hernia and an analgesic and anti-inflammatory effect.5 Ozone is administered as an oxygen-ozone gas mixture in nontoxic concentrations ranging from 1 to 40μg of ozone per milliliter of oxygen. Several methods of percutaneous injection can be used.2 Evidence of oxygen-ozone therapy regarding back pain is derived from randomized controlled trials and observational studies, which have estimated that it is an effective and safe procedure.6
Secondary complications derived from oxygen-ozone therapy are rare. The 2 most severe complications described so far are acute septicemia, following treatment of a herniated lumbar disk,5 and an unexpected death, caused by gas embolism during oxygen-ozone therapy by autohemotransfusion for psoriasis.7 There have also been other complications, such as vitreous-retinal hemorrhages with bilateral visual loss,8 headaches related to pneumocephalus, paresthesias and hypoesthesias in the ipsilateral lower limb, suggesting a lesion of the spinal nerve, vertebrobasilar stroke, altered sensation in the lower limb, subcutaneous hematoma at the site of the puncture,2 worsening of symptoms, abdominal bloating, abdominal pain, low back pain and dyspnea.6 Despite the complications described, the risk associated with oxygen-ozone therapy for disk hernia is 0.1%, with low adverse effects at therapeutic concentrations of 10–40μg/ml.6
There have only been 2 reports of infectious complications after ozone therapy. Gazzeri et al. reported a volume increase of the left iliopsoas muscle and a paravertebral abscess at the L2 level, which were associated with acute pneumonia. The patient died due to sepsis secondary to disseminated infection by Escherichia coli.5 In our case, Staphylococcus aureus (S. aureus) was isolated. Bo et al. reported the presence of an anterior epidural collection secondary to S. aureus and located at the C1–C4 level.9
Infectious complications following oxygen-ozone therapy are infrequent but potentially severe; therefore, a high index of suspicion is necessary for their diagnosis. Infection is a common risk for any invasive procedure, so sterility must be a priority for any process involving punctures. According to the present clinical case, other, less invasive options must be explored before deciding on any aggressive surgery.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Menéndez P, García A, Peláez R. Absceso paravertebral e intraabdominal secundario a ozonoterapia por lumbalgia. Rev Esp Cir Ortop Traumatol. 2014;58:125–127.