Juvenile osteochondritis dissecans (JOCD) is an acquired joint disease of unknown aetiology that affects skeletally immature patients and has the potential to progress to osteoarthritis. Recent studies have reported a high prevalence of vitamin D deficiency in patients with osteochondral lesions. The aim of our study was to determine serum vitamin D levels in patients diagnosed with JOCD.
MethodsSerum 25(OH)D levels of 31 patients (22 males) presenting 40 lesions (29 JOCD of the knee, and 11 of the ankle) were evaluated. The average age was 11.9 ± 2.9 years. Hypovitaminosis D was defined as a value less than 30 ng/ml and was divided into vitamin D insufficiency (20–30 ng/ml) and vitamin D deficiency (<20 ng/ml).
ResultsHypovitaminosis D was present in 45.2% of the evaluated patients (32.2% insufficiency and 13% deficiency). No significant differences were found in the mean values and incidence of hypovitaminosis between those patients in which the sample was taken in warm or cold season (P = .267 and P = .875, respectively). Patients who required surgery had a higher incidence of hypovitaminosis than those treated conservatively (60% versus 31%, P = .054). There was no correlation in the incidence of hypovitaminosis with sex, location, stability of the lesion, or if the lesion was uni or bilateral.
ConclusionIn our series, almost half of the patients diagnosed with JOCD presented abnormal serum levels of vitamin D. A two-fold incidence of hypovitaminosis was observed in patients requiring surgical treatment compared to patients managed conservatively. The association found in this study does not imply causation, but it should be considered within the set of actions for the treatment of these injuries.
La osteocondritis disecante juvenil (OCDJ) es una patología adquirida de etiología desconocida que afecta a pacientes esqueléticamente inmaduros y predispone al desarrollo de artrosis. Estudios recientes han reportado una alta prevalencia de deficiencia de vitamina D en pacientes con lesiones osteocondrales. El objetivo de nuestro estudio fue determinar los niveles séricos de vitamina D en pacientes diagnosticados con OCDJ.
MétodosSe evaluaron los niveles séricos de 25 hidroxivitamina D de 31 pacientes (22 masculinos) que presentaban 40 lesiones (29 OCDJ de rodilla y 11 de tobillo). La edad promedio fue de 11.9 ± 2.9 años. La hipovitaminosis D se definió como un valor inferior a 30 ng/mL y se dividió en insuficiencia de vitamina D (20 a 30 ng/mL) y deficiencia de vitamina D (<20 ng/mL).
ResultadosEl 45.2% de los pacientes evaluados presentaron hipovitaminosis D (32.2% insuficiencia y 13% deficiencia). No se encontraron diferencias significativas en los valores promedio e incidencia de hipovitaminosis entre aquellos pacientes en que la muestra se tomó en meses cálidos o fríos (P = .267 y P = .875, respectivamente). Los pacientes que requirieron cirugía tuvieron una mayor incidencia de hipovitaminosis que aquellos tratados de manera conservadora (60% versus 31%, P = .054). No encontramos correlación en la incidencia de hipovitaminosis con el sexo, la ubicación, la estabilidad de la lesión, o si la lesión fue uni o bilateral.
ConclusiónEn nuestra serie, casi la mitad de los pacientes evaluados con OCDJ presentaron niveles séricos anormales de vitamina D. Los pacientes que requirieron tratamiento quirúrgico presentaron una incidencia dos veces mayor de hipovitaminosis que aquellos que respondieron al tratamiento conservador. La asociación encontrada en este estudio no implica causalidad, pero debería ser considerada dentro del conjunto de medidas para el tratamiento de estas lesiones.
Juvenile osteochondritis dissecans (JOCD) is described by the ROCK group as an “idiopathic focal change of the subchondral bone with risk of instability and interruption of the adjacent joint cartilage that may lead to premature osteoarthritis”.1 JOCD mainly affects the knee, ankle and elbow.2 The aetiology of this pathology is unknown and many theories have been proposed, including hereditary, vascular and mechanical factors.3–6
In recent years, it has been suggested that existing endocrine factors also contribute to the development of these lesions. Hussain et al.7 consider that the lack of the growth hormone could lead to atypical ossification of nuclei and the posterior development of JOCD type lesions. Recent studies have reported a high prevalence of vitamin D deficiencies in patients with osteochondral lesions.8–10 Vitamin D is a liposoluble vitamin which plays a major role in the absorption and use of calcium. Its plasmatic levels may vary between the different population groups, depending on latitude, pollution, exposure to the sun, gender and dietary habits.11,12 Vitamin D is essential for bone growth and development. It has been demonstrated that abnormal levels of vitamin D may have negative effects on bone health in older children and teenagers.13 There are many factors involved in hypovitaminosis in children. The main reasons for it include insufficient ingestion of foodstuffs containing vitamin D and low exposure to sunlight,14 particularly during the winter months.14–16 In recent years it has been confirmed that there are musculoskeletal conditions associated with deficient serum levels of vitamin D, such as idiopathic scoliosis17 and dysplasia of hip development.18 The aetiology of Juvenile osteochondritis dissecans is unknown, although origin would appear to be multifactorial2 where mechanical factors (excessive mechanical contact) and biological factors combine in a vascular vulnerable area in a genetically susceptible individual.19,20 Among these factors, changes to bone metabolism appears to play a role.
For the last 4 years, in the department of childhood orthopaedics, we have analysed vitamin D levels as part of the general evaluation of patients with JOCD. The aim of this study was to report the serum levels of vitamin D in these patients. Our hypothesis is that a high percentage would present lower than normal levels.
Material and methodsStudy design and populationA cross-sectional study. Approval was requested from the ethics committee of our hospital prior to beginning the study. The demographic data were analysed retrospectively, together with familial pathology, serum levels of 25 hydroxyvitiamin D (25(OH)D) in a group of patients with JOCD. All patients presented with a diagnosis of JOCD confirmed by radiography and magnetic resonance. Patients with a diagnosis of celiac disease, rickets, chronic renal failure, liver failure and recurrent fractures that could affect serum levels of vitamin D were excluded.
Patient assessmentOsteochondral lesions are classified in accordance with location (knee/ankle) and where they present signs of instability in the magnetic resonance (MR) (stable/unstable). In the MR the 4 criteria established by Kijowski et al.21 were reviewed: a high T2 signal intensity rim which had the same signal intensity as the adjacent joint fluid; a secondary outer rim of low T2 signal intensity; multiple breaks in the subchondral bone plate, and the existence of multiple cysts or only one cyst above 5 mm in diameter (Fig. 1A) If none of the Kijowski criteria were met but bone oedema was observed in the MR, the lesions were considered stable (Fig. 1B). In cases which required surgery the characteristics of the lesion were confirmed or modified in keeping with intraoperative findings.
A) Magnetic resonance in coronal and saggital slices where an unstable lesion was observed in the medial femoral condyle in keeping with the criteria of Kijowski et al.21: a high T2 signal intensity rim which had the same signal intensity as the adjacent joint fluid; a secondary outer rim of low T2 signal intensity; multiple breaks in the subchondral bone plate, and the existence of multiple cysts or only one cyst above 5 mm in diameter. In addition to this, in this case, disruption of the joint cartilage was observed. B) Magnetic resonance in coronal and sagggital slices where we observed a stable lesion with osseous subchondral oedema in the medial femoral condyle but with none of the previously described features.
To determine serum levels of 25(OH)D a blood sample was taken from a peripheral vein and collected in vacultainer vacuum tubes with 5 mL of separator gel and without any contact with light for transportation to the laboratory. The sample was centrifuged for 10 min at 4.000 rpm to separate the serum from the cellular components and using the electrochemical-luminescence method (ECL) on a modular analytical cobas® 8000 (mod. 602) platform, dosing of 25(OH)D proceeded. Hypovitaminosis D was defined as a level of 25(OH)D in serum below 30 ng/mL and was divided into vitamin D insufficiency (20–30 ng/mL) and vitamin D deficiency (< 20 ng/mL).22 The phototype of patients was assessed using the Fitzpatrick23,24 scale which separates skin tone into 6 types.
Statistical analysisDescriptive statistics were calculated with regards to demography. The Shapiro-Wilk test was used to analyse data normality. Categorical variables were described as absolute frequencies and continuous variables as mean and standard deviation (DE). Paired t tests were used to examine the differences of serum levels according to sex, type of lesion, laterality, treatment and season in which the sample was taken. Due to the number of participants, patients were grouped according to warm months (spring-summer) and cold months (autumn-winter). One-way ANOVA was also used with a post hoc Tukey (HSD) test to analyse 25(OH)D differences between skin types according to Fitzpatrick. The alpha value was established at 0.05. All statistical analysis was performed using SPSS v. 19.0 (IBM Corp., Armonk, NY, U.S.A.).
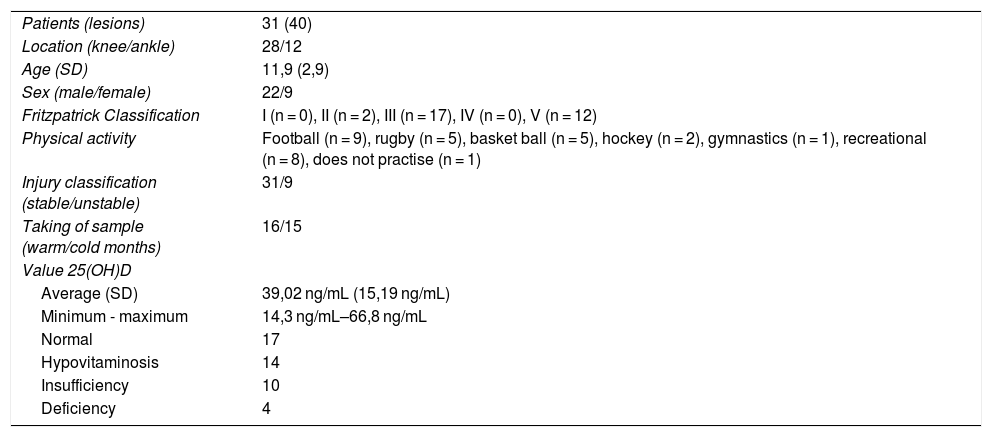
ResultsThe demographic characteristics of the sample are contained in Table 1. Average serum levels of 25 (OH)D were 39.02 ± 15.19 ng/mL. 45.2% of the patients assessed presented with hypovitaminosis D (32.2% insufficiency and 13% deficiency).
Demographic data of the sample.
| Patients (lesions) | 31 (40) |
| Location (knee/ankle) | 28/12 |
| Age (SD) | 11,9 (2,9) |
| Sex (male/female) | 22/9 |
| Fritzpatrick Classification | I (n = 0), II (n = 2), III (n = 17), IV (n = 0), V (n = 12) |
| Physical activity | Football (n = 9), rugby (n = 5), basket ball (n = 5), hockey (n = 2), gymnastics (n = 1), recreational (n = 8), does not practise (n = 1) |
| Injury classification (stable/unstable) | 31/9 |
| Taking of sample (warm/cold months) | 16/15 |
| Value 25(OH)D | |
| Average (SD) | 39,02 ng/mL (15,19 ng/mL) |
| Minimum - maximum | 14,3 ng/mL–66,8 ng/mL |
| Normal | 17 |
| Hypovitaminosis | 14 |
| Insufficiency | 10 |
| Deficiency | 4 |
SD: Standard deviation.
No significant differences were found in the average levels or in the incidence of hypovitaminosis between patients in whom the sample was taken in warm or cold months (41.7 ± 15.9 ng/mL versus 30.2 ± 9.4 ng/mL, P = .267, and 44% versus 47%, P = .875, respectively). In patients who required surgery, the incidence of hypovitaminosis was higher than in those who received conservative treatment (60% versus 31%, P = .054). We did not find any correlation in the incidence of hypovitaminosis with sex, location, lesion stability or whether the lesion was unilateral or bilateral (Table 2).
Variable comparisons.
| Demographic Variable | Specific Comparative | n (%) | Levels of 25(OH)D | P | |||
|---|---|---|---|---|---|---|---|
| Normal | Hypovitaminosis | Insufficient | Deficient | ||||
| Sex | Male | 22 (71%) | 12 (56%) | 10 (45%) | 8 (36%) | 2 (9%) | .947a |
| Female | 9 (29%) | 5 (56%) | 4 (44%) | 2 (22%) | 2 (22%) | ||
| Lesion | Stable | 31 (77.5%) | 16 (52%) | 15 (48%) | 9 (29%) | 6 (19%) | .437a |
| Unstable | 9 (22.5%) | 6 (67%) | 3 (33%) | 3 (33%) | 0 (0%) | ||
| Side | Unilateral | 23 (74.2%) | 12 (52%) | 11 (48%) | 9 (39%) | 2 (9%) | .627a |
| Bilateral | 8 (25.8%) | 5 (62%) | 3 (38%) | 1 (13%) | 2 (26%) | ||
| Treatment | Conservative | 16 (52%) | 11 (69%) | 5 (31%) | 4 (25%) | 1 (6%) | .54a |
| Surgical | 15 (48%) | 6 (40%) | 9 (60%) | 6 (40%) | 3 (20%) | ||
| Time | Warm | 16 (51.6%) | 9 (56%) | 7 (44%) | 4 (25%) | 3 (19%) | .268a |
| Cold | 15 (48.4%) | 8 (53%) | 7 (47%) | 6 (40%) | 1 (7%) | ||
| Fritzpatrick | I | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | .252b |
| II | 2 (6.5%) | 0 (0%) | 2 (100%) | 2 (100%) | 0 (0%) | ||
| III | 17 (54.8%) | 10 (59%) | 7 (41%) | 6 (35%) | 1 (6%) | ||
| IV | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| V | 12 (38.7%) | 8 (67%) | 4 (33%) | 2 (17%) | 2 (17%) | ||
| VI | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
Numbers represented in wholes and percentages.
The main finding of our study was that a high percentage of patients with JOCD presented with hypovitaminosis D, and this was even more marked in those who required surgery. In this patient subgroup with a less favourable evolution and who required surgery for the treatment of their lesion, incidence of hypovitaminosis was twice as high, incidence of deficiency of 25(OH)D was three times as high and there was a 15% higher incidence of insufficiency.
Recent studies have demonstrated a relationship between the genetic polymorphisms of vitamin D receptors and osteoporosis.25,26 Both osteoporosis and vitamin D deficiency have recently been associated with juvenile osteochondritis dissecans.27 Quan et al.28 reported on the association between rickets and bilateral JOCD of the knee and argued that the reduction of associated ossification with rickets led to an abnormally low bone density and the possible development of JOCF type lesions. Following this line of investigation, Bruns et al.8 reported the serum levels of vitamin D in 23 patients (12 male and 11 female) who presented with osteochondritis dissecans: in 15 patients the lesion was located in the talus bone, in 7 in the femoral condyles and in one in the capitellum humeral. Eighteen of their 23 patients presented with vitamin D deficiency and 3 with insufficiency. Maier et al.9 found a very high prevalence of vitamin D deficiency in young JOCD patients compared with a control group. In their study, where a total of 80 patients were assessed (51 male and 29 female) 97.5% of them presented with levels of hypovitaminosis and 37% showed levels of severe vitamin D insufficiency (<10 ng/mL). Telleria et al.10 assessed 46 patients with osteochondral lesions in the talus bone. The average levels of 25(OH)D were similar to those of our series (31.2 [12,6] ng/mL, with 54% of hypovitaminosis). Fraissler et al.29 determined serum levels of 25(OH)D in 65 patients with osteochondral lesions of the ankle (OCD and traumatic). 75.4% of the patients had low levels of vitamin D, with an average general level of 25(OH)D of 24.2 ng/mL. 35.4% presented with deficiency, 40% with insufficiency and only 24.6% of patients presented with sufficient levels of vitamin D. The levels of hypovitaminosis found in the Bruns et al.8 and Maier et al.9 studies are higher than those in our study. These findings were able to be justified by the place where they were performed (Germany) and for the average age of the first study (31.3 years). Geographical location and age are major risk factors. The synthesis of vitamin D on the skin has an inversely proportional relationship with increase in latitude and with being older.30 Several authors consider that phototype also has an impact, since less pigmented skins (type I or II) would have a greater ability to synthesisz vitamin D.31 In our study we did not find any statistically significant relationship with phototype.
The aetiology of osteochondritis dissecans is unknown but it is believed to be multifactorial, as a combination of stress of excessive mechanical contact in a vascular vulnerable osteochondral area in a genetically susceptible individual.2 Recent studies maintain that epiphyseal vascular affront at a very early age could trigger off an alteration of ossification in the epiphysis.19,20 These precursory lesions called osteochrondrosis have also been observed in animal species. Some of these precursory lesions evolve into spontaneous healing, whilst other progress towards OCD.32 Although the biomechanics is probably the main factor of progression of these lesions, it is not the only element to participate in this complex interaction. Here is where vitamin D could play a role as the potential predisposing factor.
The results of this pilot study should be interpreted within the context of its limitations. The principal limitation is its methodological design with the absence of a control group. Lack of updated information on a population in Argentina makes it difficult to compare our findings. Although data have been reported in other countries, such as Germany and the United States, they would not be analogous because of the geographical differences (climate/annual hours of sunlight), the racial distribution and the dietary characteristics of the population. Due to sample size the seasons were assessed as cold and warm seasons. Although we found there was no correlation with levels of 25(OH)D, ideally these should be assessed individually. Another limitation relating to the retrospective design is that we did not have exact data on body mass index, time of exposure to sunlight and type of diet. The following step in this study would be to increase the number of patients with JOCD and add a control group paired in age and sex to find any other relationship and to confirm the existing ones.
In our series, almost half of the patients diagnosed with JOCD presented abnormal serum levels of vitamin D. A two-fold incidence of hypovitaminosis was observed in patients requiring surgical treatment compared with those managed conservatively. The association found in this study does not imply causation but should be considered within the set of actions for the treatment of these injuries. Due to the complexity of the metabolism of vitamin D, further studies are required to confirm or refute this relationship.
Level of evidenceLevel of evidence III.
Conflicts of interestEach author certifies that there is no commercial assertion which could raise any conflicts of interest in relation to the paper submitted.
AuthorsVirginia Oberti: Data collection preparation of the manuscript.
Milca Sánchez Ortiz: Data collection, preparation of the manuscript.
Victoria Allende: Study design, critical review of the manuscript.
Javier Masquijo: Study design, statistical analysis, preparation of the manuscript.
Please cite this article as: Oberti V, Sanchez Ortiz M, Allende V, Masquijo J. Prevalencia de hipovitaminosis D en pacientes con osteocondritis disecante juvenil. Rev Esp Cir Ortop Traumatol. 2021;65:132–137.