To analyze the long-term results and the prognosis of patients who have undergone proximal row carpectomy (PRC) in our hospital.
Material and methodThis is a retrospective study of 14 patients undergoing PRC with a follow-up of 3–16 years. The ability to perform daily activities, mobility and functional capacity after the surgery were assessed using the Patient-Rated Wrist Evaluation questionnaire (PRWE).
ResultsThe range of movement was satisfactory. The mean score on the PRWE scale was 20.9±17.2 for the pain subscale and 39±35.5 for the functional capacity subscale. None of the patients required revision surgery or developed complications. Eighty percent of the patients were satisfied or very satisfied. Ninety percent of the patients would undergo surgery again.
DiscussionThe wrist's range of movement achieved with this technique is similar to that obtained with other mobility preservation techniques. Secondary arthritic changes in the radio-capitate joint do not necessarily produce pain. Some authors have described that the degree of satisfaction after PRC is equivalent to that of other procedures such as arthrodesis in 4 corners with circular plate arthrodesis or middle-carpal arthrodesis.
ConclusionPRC achieved high satisfaction rates among the patients providing pain relief, good mobility and post-operative functionality of the wrist. In addition, it presented few complications.
Conocer los resultados a largo plazo y el pronóstico de los pacientes que han sido intervenidos de resección de la primera fila del carpo (RPFC) en nuestro centro.
Material y métodoRealizamos un estudio retrospectivo de 14 pacientes intervenidos de RPFC con un seguimiento de 3 a 16 años. Se evaluaron la movilidad, la capacidad funcional mediante el cuestionario Patient-Rated Wrist Evaluation (PRWE) y la capacidad para realizar las actividades de la vida diaria tras la intervención.
ResultadosEl balance articular fue satisfactorio. La puntuación media en la escala PRWE fue de 20,9±17,2 para la subescala de dolor y de 39±35,5 para la subescala de funcionalidad. Ningún paciente había precisado reintervención ni han desarrollado complicaciones. El 80% de los pacientes estuvieron satisfechos o muy satisfechos. El 90% de los pacientes volvería a operarse.
DiscusiónEl rango de movimiento de la muñeca es similar con las diferentes técnicas de preservación de la movilidad. Los cambios artrósicos en la articulación radio-hueso grande secundarios a esta intervención no producen necesariamente dolor. Algunos autores han descrito que el grado de satisfacción de la RPFC es comparable con el de otros procedimientos, como la artrodesis en 4 esquinas con placa circular o artrodesis mediocarpiana con agujas.
ConclusiónLa RPFC tiene alta tasa de satisfacción entre los pacientes con alivio del dolor, buena movilidad y funcionalidad postoperatoria de la muñeca. Además, presenta escasas complicaciones.
Proximal row carpectomy (PRC) is a surgical treatment used in advanced osteoarthritis of the wrist that fails to respond to conservative treatment. It seeks to relieve symptoms without limiting mobility.1–3 Advanced osteoarthritis of the wrist is often due to nonunion of the scaphoid,4–6 advanced Kienböck's disease,4,7 dislocation of the perilunate or calcium pyrophosphate deposits.4 PRC is proposed as an alternative to four corner fusion, fusion of the capitate and perilunate, or to total arthrodesis of the wrist.8 It is indicated if the aspect of the radius facing the perilunate and the cartilage of the proximal surface of the capitate bone are in good condition,9–14 although there are no studies that specify the degree of joint wear that is acceptable to use this technique.5 Furthermore, there are reports in the literature that radius-capitate osteoarthritis that occurs secondary to surgery does not necessarily cause pain.1,3,5,13,15,16
The mid- and long-term results reported in the literature confirm that it is a procedure by means of which adequate mobility of the radio-carpal joint is maintained, with good functional outcomes, and a high degree of patient satisfaction.1,3,7,10,11,13–15,17–21 In spite of the good results, a reconversion to radio-carpal arthrodesis rate of between 4.9 and 15% of the cases has been reported.11,12,14
The objective of this work is to review the cases of PRC at our centre to ascertain prognosis and long-term outcomes.
Material and methodWe conducted a retrospective study of 14 patients who underwent PRC between the years 2002 and 2015. The mean of age of our series was 60.9±11.2 years. Ten subjects were male and 4, female. All cases were right-handed. Twenty-nine percent (29%) of the patients had surgery on the left (non-dominant) wrist; 57% on the right (dominant side) wrist, and 14% were underwent surgery on both wrists at 2 different times.
The PRC was performed to treat advanced osteoarthritis of the wrist due to scaphoid necrosis, Kienböck's disease, scaphoperilunate dissociation, or idiopathic radio-carpal osteoarthritis in 4, 3, 6, and 3 cases, respectively. Denervation of the posterior interosseous nerve (PIN) was associated in all cases as coadjuvant treatment for postoperative pain, given that it is a straightforward procedure with no additional morbidity for the patient. All the surgeries were performed by the same surgeon, using a posterior approach and the same surgical and postoperative technique reported by Escribano et al.18
The patients were seen at check up to evaluate mobility, symptomatology, radiological status of the joint, and to fill in the Patient-Rated Wrist Evaluation (PRWE) questionnaire.22 In addition, an evaluation questionnaire was conducted to assess their capacity to perform the activities of daily living following the operation. The minimum follow up was 3 years and the maximum was 16 years.
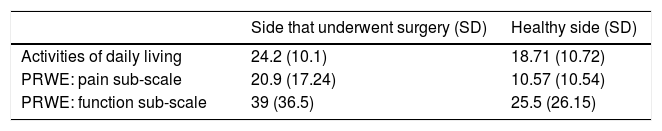
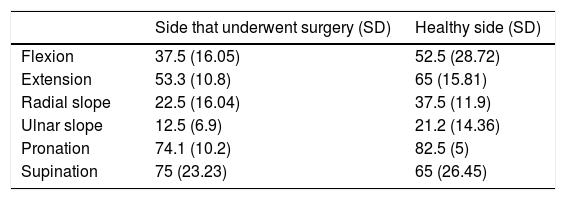
ResultsFollow-up was completed in 9 of the 14 patients who underwent PRC. Of them, none had required reintervention. The mean score on the PRWE scale was 20.9±17.2 for the pain sub-scale and 39±35.5 for the functionality sub-scale (Table 1). Moreover, the evaluation of the ability to carry out their activities of daily living yielded a score of 24.2±10 (Table 1). Joint balance resulted in mean flexion of 37.5±16°, mean extension of 53±10.2°, mean ulnar deviation of 12.5±6.9°, mean radial deviation of 22.5±16°, mean pronation of 74.2±10.2°, and mean supination of 75±23.2° (Table 2).
Mean in degrees of mobility of the side that underwent surgery following the intervention and the contralateral side.
| Side that underwent surgery (SD) | Healthy side (SD) | |
|---|---|---|
| Flexion | 37.5 (16.05) | 52.5 (28.72) |
| Extension | 53.3 (10.8) | 65 (15.81) |
| Radial slope | 22.5 (16.04) | 37.5 (11.9) |
| Ulnar slope | 12.5 (6.9) | 21.2 (14.36) |
| Pronation | 74.1 (10.2) | 82.5 (5) |
| Supination | 75 (23.23) | 65 (26.45) |
SD: standard deviation.
Eighty percent (80%) of the subjects were satisfied or very satisfied with both the functional and aesthetic result, scoring it as very good or excellent, and only 20% of the individuals were unhappy because it did not meet their expectations and they expected more from the intervention. Ninety percent (90%) of the patients would undergo surgery again. None of the patients who underwent PRC developed complications.
DiscussionRahgozar et al. reported that PRC is a procedure that is largely indicated for older patients, reserving arthrodesis for younger individuals12; although there are studies that report cases in younger patients with a mean age of 43 years and some of even 24 years.1,16 In our series, the mean age was 60.9±11.2 years.
Many authors have published good functional results with arcs-of-mobility in flexion-extension in excess of 70° and radial-cubital deviation of more than 40°.1,3,4,16,16–20 Although wrist mobility is less than the anatomical norm, it is better in comparison with preoperative mobility.21 There appear to be no major differences as regards range of movement with other mobility-preserving techniques and mobility is better in than in those techniques that entail some form of arthrodesis.23,24 Jebson et al. and Liu et al. achieved a range of mobility of 63% and greater than 75%, respectively, with respect to the contralateral wrist.1,20 Wall et al. reported 66% more flexion and 50% more extension versus the contralateral wrist.15 Prousa et al. studied 12 patients and attained 92% good results and a 56.7° range of movement in flexo-extension (range, 90°–35°) and 32.9° (range, 36°–23°) cubital-radial deviation.17 In our study, postoperative mobility is similar to the mobility reported in the literature, 75% in flexo-extension, 100% in prono-suppination, and 59% in cubital-radial deviation in comparison with the contralateral wrist. Our older patients also display involvement of mobility in the contralateral wrist.
Despite the fact that we did not patients’ measure grip strength in this study, the literature reports grip strength in excess of 70% of the healthy limb.4,20,21 Furthermore, no differences have been reported in the literature insofar as grip strength is concerned when comparing PRC and 4-corner arthrodesis.15,23,25
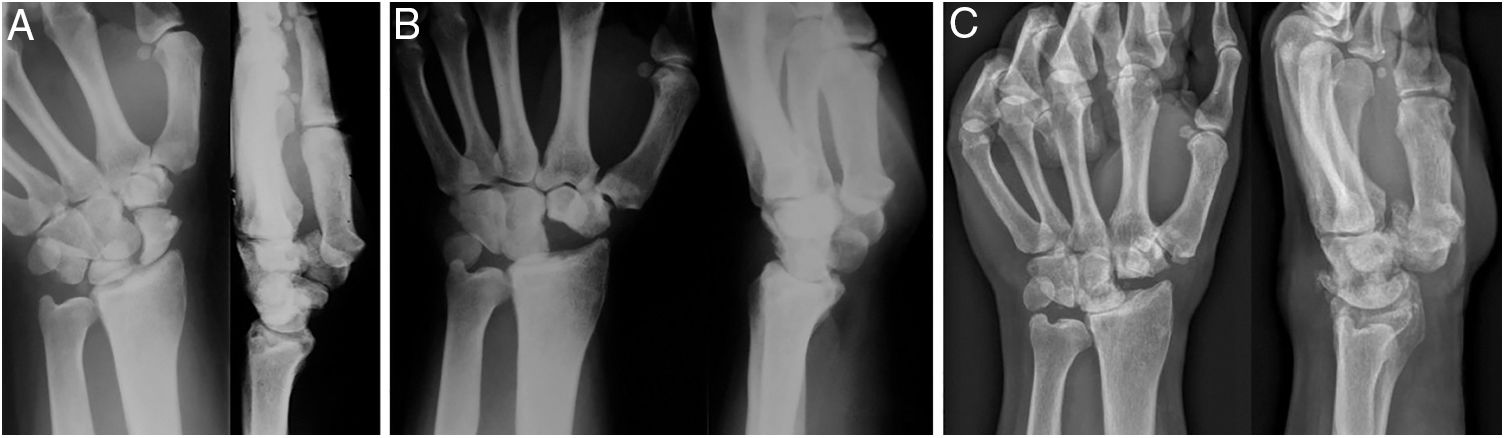
A cadaver study revealed an 86% decrease in the surface contact area of the radio-carpal joint following PRC.26 This accounts for the increase in pressure on the lunate fossa by 37% after PRC.27 The degree of congruency of the new joint between the lunate fossa and the capitate bone appears to correlate with mobility, and a higher degree of congruency appears to correlate with better postoperative ranges of movement.10 The radius-capitate arthritic changes reported in the literature as being secondary to this surgery do not necessary provoke pain.1,3,5,13,15,16,28 Over the long-term, patients who underwent PRC presented more arthritic changes than those who underwent a four corner fusion and the latter group have 10% more complications due to non-union of the arthrodesis, dorsal compression, and complications related to the material of osteosynthesis.23,29 The PRC is described as a procedure that yields good outcomes1,3,7,13,14,16,18–21 with a rate of reconversion to radio-carpal arthrodesis ranging from 4.9 to 15%,11,12,14 and a lower risk of reconversion to arthrodesis than when a partial arthrodesis of the wrist is performed.12 Other authors state that there are no differences in the reconversion rate compared to other techniques, reporting rates of reconversion to radio-carpal arthrodesis of 2.9% after a four corner fusion and 3.9% following PRC.12,23 None of the cases in our series required reconversion to arthrodesis, despite developing degenerative changes over time (Fig. 1).
Forty-seven year old male diagnosed with necrosis of the scaphoid bone in the left wrist that underwent resection of the first carpal row. (A) Pre-operative AP-L X-ray of the wrist. (B) Control at 6 weeks following surgery. (C) Control after 16 years of follow up that displays degenerative changes in the radio-capitate joint that cause no clinical symptoms or loss of strength.
The degree of patient satisfaction with PRC in the literature is good.3,17 The degree of subjective satisfaction obtained was very good or excellent in 80% of our cases. Only 2 patients reported that they were unsatisfied with the result of the operation. The satisfaction rates with PRC reported in the literature are comparable to those of other procedures, such as the four corner fusion with a circular plate23,25 or mid-carpal pin fixation.16 Our patients presented PRWE scores on a par with those found in the literature.15
Denervation of the PIN is used as coadjuvant treatment for postoperative pain and did not alter results,30 given that it is a partial denervation after which spontaneous reinnervation can take place. Moreover, the isolated denervation has a 25% failure rate during the first year following surgery.31,32 Therefore, although the results during the first 2 years may be due to the effect of both procedures, we believe that the mid- and long-term outcomes are due to the PRC. In 13 patients, Palazzi performed an isolated denervation of the PIN associated with other procedures and concluded that the denervation of the PIN leaves no clinically measurable sequelae and that changes in wrist mobility cannot be attributed to the neurectomy.30
We agree in that PRC should be contemplated as another procedure in the treatment arsenal for degenerative, painful osteoarthritis of the wrist and as a good palliative procedure.18,19 PRC yields predictable results and a high degree of satisfaction with few complications and recurrences when performed with a proper indication and technique.1
This study presents certain limitations. The patients in our series are older than those described in other series, with an age of 60.9±11.2 years. This might condition the fact that they had more advanced osteoarthritis with greater preoperative limitation. In addition, the functional demands in these patients are not as high and this conditions postoperative expectations. We do not have data regarding grip strength, given that since it was a retrospective study, it was not possible for patients to come for evaluation of their grip strength. Finally, because of its retrospective nature, there is a certain bias owing to the loss of certain data that could not be recorded. Furthermore, the preoperative questionnaires were filled in after surgery, which could incur a memory bias.
In summary, the PRC has a high rate of satisfaction among patients, displaying good pain relief, and good postoperative mobility and functionality of the wrist. Moreover, it is a technique with few complications when performed with the proper indication.
Level of evidenceLevel of evidence III.
FundingNone.
Conflict of interestsNone.
To Dr. Pons, for his help in drafting the patient questionnaires.
Please cite this article as: Montiel V, Payo-Ollero J, Amillo S. Resección de la primera fila del carpo en pacientes mayores de 50 años: 3 a 16 años de seguimiento. Rev Esp Cir Ortop Traumatol. 2019;63:295–299.