The indications for radial head arthroplasty are essentially complex fractures with ligament damage (medial, lateral or Essex-Lopresti), and/or associated with bone damage (coronoids or olecranon). The aim of this study is to review our experience with the use of a radial head prosthesis in the context of a trauma.
Material and methodAn observational, descriptive and retrospective study, with a follow-up of 1–11 years, was performed on a study group of 82 patients with a mean age of 41.6 (±9.2) years.
The inclusion criteria were: patients of working age (25–64 years) with complex radial head fractures (Mason II, III, IV), with soft tissue and bone injuries that caused instability, non-reconstructable by osteosynthesis and treated using arthroplasty.
The primary variables analysed were social demographics, Mason classification, or surgical aspects such as delay, surgical time, type of prosthesis (where the bipolar prosthesis was most used, 88.6%), need of fixation or further surgery. Rehabilitation time, causes of prosthesis failure, radiological findings (according to Van-Riet), areas of loosening (according to Popovic), as well as the Mayo Elbow Performance Score (MEPS) and the Cassebaum scale.
Various associated injuries were observed, such as injuries in the lateral collateral ligament of the elbow in 39% of cases, coronoid fractures in 25.6%, and an olecranon fracture in 15.9% of the series. There was one case of an Essex-Lopresti injury.
The tests used for the statistical analysis were Chi squared and Fisher test for categorical variables and contingency tables. The Mann Whitney U or Kruskal Wallis tests were used for the numerical variables. Evidence level: IV.
ResultsThe mean surgical time was 100 (±56.8)min. The prosthesis was fixed in 53.8% of cases. The mean score on the MEPS scale was 80.4 (±19.3) points, being good–excellent in 71.6%. The elbow was stable in 93.7% of cases. There was moderate instability, with 10° or more in varus or valgus, and in 1.3% in the rest of the series. The rehabilitation time was lower in the fixed cases (P=0.03), and there was greater rigidity (P=0.03) and more sequelae (limitations in mobility, residual pain), (P<0.05) in the cases where the LCL had to be repaired (given that there were other serious injuries in these cases). When the surgical delay was less than one week, better results were obtained on the Cassebaum scale (P=0.02), as well as more excellent results on the MEPS scale MEPS (P=0.02). The prosthesis was removed in 11 cases (13.4%), with the main cause for removal being pain in pronosupination in 5 cases, and capitellar injuries in 4 cases, one dislocation, and one infection. The most frequent complication was rigidity (30.5%). There were 3 infections (3.7%). Popovic areas 1 and 7 had greater osteolysis.
ConclusionsThe presence of concomitant bone and ligament injuries determined a longer surgical time and more sequelae. Early surgery would achieve better clinical results.
Las indicaciones de artroplastia de cúpula radial son esencialmente fracturas complejas con daño ligamentoso (medial, lateral o Essex-Lopresti), y/o asoaciadas a daños óseos (coronoides u olécranon). Nuestro objetivo es revisar nuestra experiencia con la utilización de prótesis de cabeza del radio en un contexto traumático.
Material y métodoEstudio observacional, descriptivo y retrospectivo, con seguimiento de 1–11 años. El grupo de estudio tuvo un tamaño muestral de 82 pacientes, con una edad media de 41,6 años (±9,2).
Los criterios de inclusión fueron: pacientes en edad laboral (25–64 años) con fracturas de cúpula radial complejas (II, III, IV de Mason), con lesiones de partes blandas u óseas, que conllevarán inestabilidad, no reconstruibles mediante osteosíntesis y tratadas mediante artroplastia.
Las principales variables analizadas fueron datos de filiación, clasificación de Mason o aspectos quirúrgicos, como demora, tiempo quirúrgico, tipo protésico (donde la prótesis bipolar fue la más utilizada, 88,6%), necesidad de cementación o reintervenciones. También se analizó el tiempo rehabilitador, las causas de fracaso protésico, complicaciones, hallazgos radiológicos (según Van-Riet), zonas de aflojamiento (según Popovic), así como las escalas MEPS y de Cassebaum.
Se apreciaron diversas lesiones asociadas, como el daño en el ligamento colateral lateral cubital en el 39% de los casos, la fractura de coronoides, en el 25,6% y la fractura de olécranon, en el 15,9% de la serie. Hubo un caso de lesión de Essex Lopresti.
Los test estadísticos utilizados fueron: para variables categóricas, las tablas de contingencia, Chi Cuadrado y test de Fisher. Para las variables numéricas, la U de Mann Whitney o el test de Kruskall Wallis. Nivel de evidencia IV.
ResultadosEl tiempo quirúrgico fue de 100 minutos (±56,8). Se cementaron el 53,8% de las prótesis. El resultado de la escala MEPS: 80,4 puntos (±19,3), siendo excelentes-buenos en el 71,6%. El codo era estable en el 93,7% de los casos, presentaba una moderada inestabilidad, inferior a 10° en varo-valgo, en el 4,9% de los casos y una franca inestabilidad, con 10° o más de inestabilidad en varo o en valgo, en el 1,3% restante de la serie. El tiempo de rehabilitación fue menor en las cementadas (p=0,03), hubo mayor rigidez (p=0,03) y más secuelas (limitaciones de movilidad, dolor residual), (p<0,05) en los casos en los que hubo que reparar el ligamento colateral lateral cubital (dada la coexistencia de otras lesiones graves en estos casos). Se obtuvieron mejores resultados en la escala de Cassebaum (p=0,02) y más resultados excelentes en la escala MEPS (p=0,02), cuando la cirugía fue antes de una semana. Se retiró la prótesis en 11 casos (13,4%), donde la principal causa de retirada fue el dolor en la pronosupinación en 5 casos, las lesiones capitelares en 4 casos, una luxación y una infección. La complicación más frecuente fue la rigidez (30,5%). Hubo 3 infecciones (3,7%). Las zonas 1 y 7 (Popovic) fueron las de mayor osteólisis.
ConclusionesLa presencia de lesiones óseas y ligamentosas concomitantes determinaba más tiempo quirúrgico y secuelas. La cirugía precoz conseguiría mejores resultados clínicos.
Radial head fractures constitute 1.7–5.4% of all adult fractures. Approximately 33% of the elbow fractures can be associated with radial head fractures and up to 85% of these occur in young people and active patients.1
Biomechanically, the radial head is the main posterolateral stabiliser, when the coronoid is fractured or the lateral ulnar collateral ligament (LUCL) is injured and it is the secondary in valgus, when the medial collateral ligament is incompetent. The radial head is the main stabiliser of the elbow if the coronoid is fractured, the medial collateral ligament is incompetent or the LUCL is injured.
The Mason classification recognises type III fractures as comminuted and displaced factures that affect the entire radial head. Because the vascular of the epiphysis proximal to the radial is limited to small intra-articular vessels, open reduction and osteosynthesis could cause associated osteonecrosis, lack of consolidation or secondary displacements.2 In cases with associated elbow instability, the most appropriate treatment is replacing the prosthesis. In the rare situation in which the osteosynthesis is stable and lacking elbow instability, osteosynthesis could be performed.3
Removal without arthroplasty can change elbow biomechanics and stability, which is why associated arthroplasty offers better results than isolated resection in cases without associated instability.4–7 Radial head removal would be contraindicated in patients with incompetent medial collateral ligament, interosseous membrane lesion or elbow dislocation and it has been related with pain, instability, proximal translation of the radius, osteoarthritis, loss of strength and cubitus valgus,8 mainly when there was some type of underlying instability.
Radial head arthroplasty would be indicated in non-reconstructable displaced and comminuted fractures that affect more than 25–30% of the radial head surface6 and allow reconstructing radiocapitellar contact and acting as a spacer while lesions associated with the medial collateral ligament, lateral collateral ligament, interosseous membrane7 or the joint capsule8,9 heal, re-establishing joint biomechanics. Better results have recently been obtained with arthroplasty as compared with osteosynthesis in Mason type III radial head fractures.10
Our objective was to assess whether our experience with radial head arthroplasty in complex fractures with ligament damage, concomitant lesions or surgery timing might have on the final functional result and any possible complications.
Material and methodsThis was a retrospective, descriptive, observational study, with a study group sample size of 82 patients, operated on in our centre between 2000 and 2011. Mean age was 41.6 years (±9.2). Level of evidence: IV. Follow-up time was 1–11 years, with a median of 18 months, a minimum of 12 and a maximum of 125 months. There were no losses to follow-up. In addition to the fact that the patients were treated by many members of our service, there is a specific shoulder and elbow unit, which participated actively in the interventions and follow-up of all the patients.
We used the Mason classification,11 modified by Johnston,12 considering 4 types: type I (non-displaced, up to 2mm of depression), type II (more than 2mm of displacement), type III (comminuted) and type IV (with dislocation).
Criteria of inclusion: work age patients (25–64 years old) with complex radial head fractures (Mason II, III and IV), with associated soft tissue or bone structure lesions, which involved instability, non-reconstructable by osteosynthesis and that underwent radial head arthroplasty.
The associated lesions were LUCL damage (39%), coronoid fracture (25.6%) and olecranon (15.9%). There was 1 case Essex-Lopresti injury, 1 case of associated Monteggia fracture and 2 cases of terrible triads. The incidence of LUCL lesions has probably been underdiagnosed in this series, given that it is more frequent than the mere 39% of cases registered.
The injury mechanism was indirect trauma (indirect mechanism) in 98.8% of the cases. The patients’ job positions were considered to be of high functional demand (with great strength requirements) in 78% of the series. The right elbow was affected in 45.1%. The dominant arm was the arm affected in 50% of the series.
According to the Mason classification the distribution of the fractures was as follows: type II fractures represented 2.5%; type III, 27.2% and type IV (associated to dislocation), 70.3% of the series.
Time of surgical delay before the intervention was less than 1 week (acute) in 42.7%, between 1 and 4 weeks (subacute) in 32.9% and over 4 weeks (chronic) in the remaining 24.4%. Intervention time was 100.5±56.8min.
The approach used was the one described by Kocher, between the extensor carpi ulnaris and the anconeus muscles. If the coronoid could be synthesised by this approach, if there was a fracture at this level, the medial approach would be avoided. In the case of fracture of the olecranon, the posterior approach would be used to synthesise the radial head. The medial approach of Kasparyan and Hotchkiss13 was also used in 2 cases, where it was impossible to reconstruct the coronoid laterally.
The treatment algorithm used in the face of a radial head fracture was orthopaedic with early rehabilitation in type I fractures. In type II fractures, following evacuation arthrocentesis and local intraarticular anaesthesia, if there was no pronation/supination block, the treatment was early rehabilitation after 1 week of immobilisation. If there was blockage, osteosynthesis, partial extirpation (if less than 25% affected) or total extirpation, as long as there was no varus instability as well. In type III, the computed tomography scan study (which we attempted to perform fundamentally from type II fractures on) made it possible to clarify treatment using osteosynthesis or prosthesis. Where there were also ligament lesions, the lateral ligament complex was repaired. We did not repair the medial collateral ligament. In the case of Essex-Lopresti lesion, osteosynthesis or arthroplasty was performed and the distal radioulnar joint was stabilised with a Kirschner needle in supination for 3 weeks. If there was an associated coronoid fracture, the coronoid fracture was treated first according to the Regan-Morrey classification14 (from the lateral approach if it were possible from having removed the radial head, or from the medial if the head was conserved) and then osteosynthesis or arthroplasty of the radial head was performed. That is, if the coronoid fracture was type I, it was not synthesised and, if the fracture was type II or III, reinsertion or osteosynthesis was performed, with needles or Mayo Clinic plate (Acumed®). In this series, of the 21 cases (25.6%) with coronoid fracture, we stabilised the fracture in 15 cases (18.2%), all type II, using 2 threaded 1.5-mm Kirschner needles; in 4 cases (4.8%) the fractures (also type II) were stabilised with transosseous suture and in 2 cases (2.4%), both type III, the fractures were reconstructed with radial head grafting and screws. In the case of associated fracture of the olecranon, osteosynthesis or arthroplasty of the radial head and osteosynthesis of the olecranon, with cerclage or plate, were performed, with repair of the lateral ligament complex; a provisional external fixator could even be placed if there was residual instability.
Type of intervention: The lateral ligament complex (LLC) was reinserted in 32 cases (39%). In this procedure, the ligament was directly sutured in 37.5% of the cases and transosseous suture was used in 31.3% of the cases, while in the rest we used anchors when there was frank instability upon forcing varus. External fixator was used in 4.9% of the patients and osteosynthesis of the olecranon in 15.9%.
The prosthesis used most often was the modular metallic Tornier®, in a non-cemented short version and a long, cemented one. These prostheses were placed in 88.6% of the patients.
Cement was applied in the prosthesis implantation in 53.8% (cases corresponding to the years in which the Tornier® prostheses were only cemented and in those that had a long shaft), with short shafts in 50 cases (61%) and long shafts in 32 (39%). The modular metallic anatomic prosthesis (Anatomic Radial Head System, ACUMED®, Hillsboro, Oregon, USA) was placed in 7.3%. The Mopyc® prosthesis was used in 4.1%. Despite having several prosthesis models available from various commercial firms, as mentioned earlier (Tornier®, Acumed® or Mopyc®), and considering component versatility and ease of placement, the Tornier® prosthesis was the one most accepted by the members of our service.
We placed 52 short-shaft prostheses and 30 long-shaft ones. The choice of one or the other depended on the state of the radial neck. If there were few adjustment guarantees from osteoporosis or comminution of the osteotomy area, a prosthesis with cemented diaphyseal anchorage, with a long shaft, would be preferred.
The surgical procedure to measure the implant and avoid overlengthening or “overstuffing” obeyed the considerations that follow. The gap in the lateral ulnohumeral joint visible in surgery would be the most reproducible indicator of head overlengthening, after prosthesis implantation, considering that when the gap begins to be detected, the head overlengthening is already ≥2mm.15 The appearance of a hiatus in the ulnohumeral section is a reliable index of prosthetic “overlengthening”.15,16 In this manner,17 the distance between the osteotomy level and the proximal border of the lesser sigmoid cavity should be equal to the thickness of the radial head.18 In this study we fundamentally used the measurement of the hiatus in the lateral ulnohumeral joint and attempted as much as possible for the distance between the osteotomy level and proximal border of the lesser sigmoid cavity to be the same as the thickness of the radial head.
The patients were immobilised with a splint for 3 weeks if there was ligament injury or associated lesions such as coronoid fracture. Rehabilitation commenced after that. When great instability was maintained stable with Orthofix® or Stryker® external fixation, it was kept for 3–6 weeks, although elbow mobilisation began immediately at 24–48h, in a protected manner. If there were no other injuries, mobilisation began postoperatively (24–48h post-intervention).
Complications were considered to be all the adverse situations that arose following prosthesis implantation that lengthened or worsened the process of the original pathology (fracture of the radial head) and that were not related to it. The Mayo Elbow Performance Score (MEPS)19,20 and the Cassebaum21,22 scales were used (scales that mainly took into account pain, movement and stability); rigidity was considered according to the description by Morrey23,24: very severe rigidity when the total arc was 30° or less, severe when it was between 31° and 61°, moderate in the 61°–90° range and minimal when it was greater than 90°.
Elbow osteoarthritis was considered according to the Rettig classification,25 in which Class I was characterised by initial osteoarthritic changes in the ulnohumeral joint, with a normal radiocapitellar joint. Class II referred to marginal osteoarthritic changes in the ulnohumeral joint in addition to osteoarthritic changes in the radiocapitellar. Finally, Class III was characterised by marginal ulnohumeral and radiocapitellar changes, with a radiocapitellar subluxation as well. The higher the class, the greater the joint narrowing was. Loose bodies appeared in Classes II and III.
Prosthesis mobilisation was considered to be the radiological phenomenon by which prosthesis displacement from the original insertion spot would be produced. Radial head subluxation was also considered in radiological monitoring, which could be anterior, posterior, static or dynamic. Heterotopic ossifications, osteolysis and so forth were assessed as well.
The variables analysed were affiliation details, Mason classification, surgical factors (delay, surgical time, type of prosthesis, cementation, reinterventions), rehabilitation period, causes of prosthesis failure, complications, radiological findings (loosening, overlengthening, radial head subluxation and component dissociation, according to Van-Riet26), prosthesis osteolysis area (zones 1–7, in the prosthesis anchor to the radius, Popovic27), and the MEPS scale (pain, movement, stability and daily life functionality19,20) and the Cassebaum rating scale,21,22 according to flexion/extension degree from very good (flexion exceeding 130°), good, moderate, to poor (flexion less than 110°).
To find statistically significant differences, the data obtained were analysed using the statistical package SPSS v. 15.0. To analyse categorical variables we used contingency tables and analysis by the Chi squared and Fisher's exact test. For the analysis of numerical variables, a normal distribution study was first carried out, using the Shapiro–Wilk test, finding that the variables to analyse presented non-parametric distribution. For that reason, for these variables, the Mann–Whitney U test was used when there were 2 independent samples, while that of Kruskal–Wallis was used for 3 independent samples. The interval necessary to establish reliable statistical conclusions was set to a 95% interval of confidence, considering that the differences were statistically significant when P<0.05.
All the patients signed the proper informed consent and the study was approved by the Ethics Committee at our centre.
ResultsFinal flexion was 127.3° (±18.3), extension was 18.5° (±11.8), pronation was 78.7° (±18.8) and supination was 77° (±19.4). On physical examination, 93.8% of the series had a stable elbow, 4.9% had moderate elbow instability (less than 10° in varus or in valgus), and only 1 case (1.2%) showed instability greater than 10° in varus or valgus.
According to the Cassebaum scale the results were very good in 50%; good, 30.5%; moderate, 4.9% and poor in 14.6% (with ranges of elbow motion less than 100° in flexion/extension).
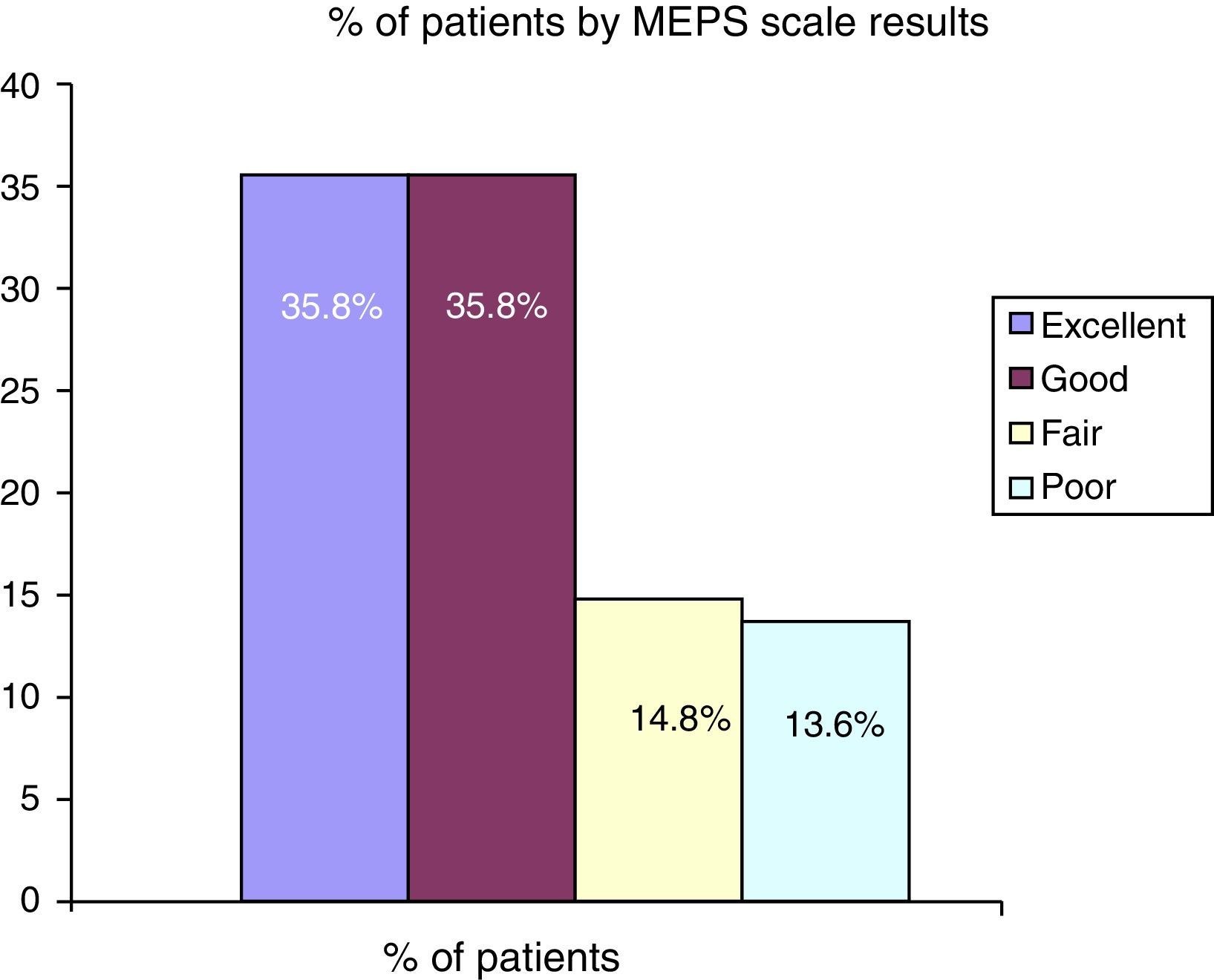
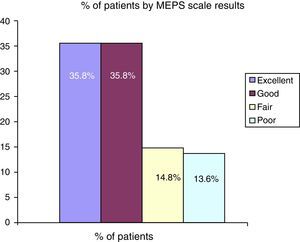
The final MEPS result was 80.4 points (±19.3). The distribution of the results is shown in Fig. 1. Poor results were considered to be those where less than 60 points were obtained in this scale.
Of the total patients, 75.6% returned to their usual demanding jobs.
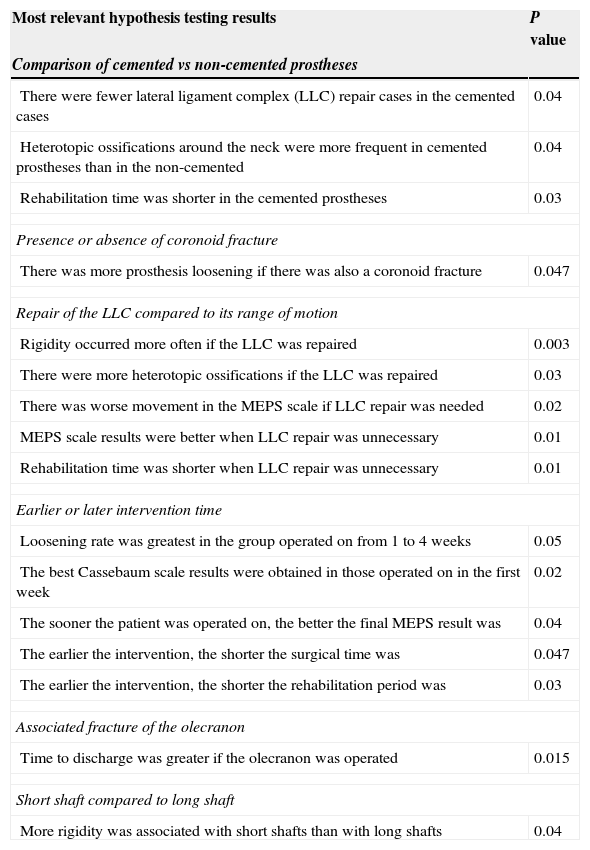
Statistical hypothesis testing resultsWe describe the main hypothesis testing results, showing all the statistically significant results, in Table 1. It can be seen that ossification around the neck was more frequent (P=0.046) in the cemented prostheses than in the non-cemented. Other interventions were associated more frequently in the cases of concomitant coronoid fractures (P=0.05), and the greater the coronoid comminution, the worse the MEPS scale results were.
Comparative hypothesis testing study, with the main statistical differences found.
| Most relevant hypothesis testing results | P value |
|---|---|
| Comparison of cemented vs non-cemented prostheses | |
| There were fewer lateral ligament complex (LLC) repair cases in the cemented cases | 0.04 |
| Heterotopic ossifications around the neck were more frequent in cemented prostheses than in the non-cemented | 0.04 |
| Rehabilitation time was shorter in the cemented prostheses | 0.03 |
| Presence or absence of coronoid fracture | |
| There was more prosthesis loosening if there was also a coronoid fracture | 0.047 |
| Repair of the LLC compared to its range of motion | |
| Rigidity occurred more often if the LLC was repaired | 0.003 |
| There were more heterotopic ossifications if the LLC was repaired | 0.03 |
| There was worse movement in the MEPS scale if LLC repair was needed | 0.02 |
| MEPS scale results were better when LLC repair was unnecessary | 0.01 |
| Rehabilitation time was shorter when LLC repair was unnecessary | 0.01 |
| Earlier or later intervention time | |
| Loosening rate was greatest in the group operated on from 1 to 4 weeks | 0.05 |
| The best Cassebaum scale results were obtained in those operated on in the first week | 0.02 |
| The sooner the patient was operated on, the better the final MEPS result was | 0.04 |
| The earlier the intervention, the shorter the surgical time was | 0.047 |
| The earlier the intervention, the shorter the rehabilitation period was | 0.03 |
| Associated fracture of the olecranon | |
| Time to discharge was greater if the olecranon was operated | 0.015 |
| Short shaft compared to long shaft | |
| More rigidity was associated with short shafts than with long shafts | 0.04 |
Analysis of LUCL repair results yielded the following results: there was more rigidity (normal range of motion limited to less than 50% of the normal range of motion) observed in the patients where the LUCL was repaired. More sequelae (limitations in mobility, residual pain, etc.) also appeared when it was necessary to repair it (P<0.05), and there were better MEPS results when the LUCL was not repaired (P=0.01).
Time of surgical delay was an important variable. The best results according to the Cassebaum rating scale were obtained when the patient was operated in the first week (P=0.02). With respect to the MEPS the best results (more excellent results) were reached when the surgery was performed before the first week (P=0.02) and the rehabilitation period was shorter if the operation took place earlier (P=0.03). Patient distribution in these 3 groups were characterised by presenting different concomitant injuries of the elbow. Likewise, soft tissue involvement or other associated traumas caused changes in the intervention date. We believe that these data could affect the results.
For example, the group in which the prosthesis was implanted later than 4 weeks (20 cases, 24.4% of the patients) was characterised by presenting other associated lesions, such as coronoid fracture in 15% of this group, instability with need for LUCL repair in 20%, need for external fixator in 10%, fracture of the olecranon in 20%, or need for cementation in 68.4%.
Reintervention was necessary for 25% of the patients, removing the prosthesis in 3 cases, performing arthrolysis in 1 case, cleaning due to superinfection in another case and anchor removal in 2 cases, as well as drainage of a Morel-Lavallée lesion in an affected member. Almost all of these patients had consulted later than after 2 weeks’ evolution, so the surgery was delayed until late, with longer than 3 weeks’ evolution. This group presented 42.1% complications. The reason for reintervention in these patients was pain in 40% of the patients, rigidity in another 40% and instability in 15% of these patients. These circumstances led to worse results in this group of reoperated patients, given that rehabilitation time was a mean of 4 (±1.5 months), 5 (±1.6 months) and 6.4 months (±3.7 months), depending on whether the group was reoperated in the first week, between 1 and 4 weeks, and more than 4 weeks later, respectively. Likewise, the MEPS results were 86.3 (±13.5 points), 80.8 (±16.2 points) and 68.9 points (±26.8), respectively.
Finally, osteosynthesis of the olecranon also modified the results obtained. Time until discharge was longer if there was also olecranon operation (P=0.015).
The short shaft prostheses did not show statistically significant differences from those of long shafts. Neither were there statistically significant differences in the final MEPS results (78.4±19.6 points, against the 83.4±19.6 points for the long shaft), rehabilitation time (5.02±2.6 points, against 4.6±2.2 months) or reintervention rates (46.7% reinterventions for short shaft prostheses, against 37.5% in the long shaft prostheses). There were only significant differences in final rigidity (which was 38.8% in the cases with short shaft prostheses, compared to 16.7% rigidity with long shaft prostheses (P=0.04)).
Overall rehabilitation time was 4.9 months (±2.4 months).
Some type of complications appeared in 40% of the cases. On the one hand, we can classify the complications based on their origin in those of the radial head fracture and its prosthetic treatment: 1 case of periprosthetic fracture, 1 case of dislocation, 3 cases of infection, 1 case of capitellar erosion from prosthesis overload, 1 case of chronic posterolateral instability, 2 cases of calcifications in the area of the prosthesis neck, and 1 case of lack of consolidation following associated coronoid osteosynthesis. Other more frequent and more important clinical complications were as follows: severe rigidity (range of motion of 31°–60°), which appeared in 14.3% (5 cases); 2 cases of chronic synovitis; 4 cases (11.4%) of reflex dystrophy and transient sensitive ulnar neuropathy in 3 cases. One case of Morel-Lavallée, 1 case of adhesive capsulitis of the shoulder, 2 cases with transient paresis of the posterior interosseous membrane and 2 cases of heterotopic ossification in the medial collateral ligament (with Grade II Rettig osteoarthritis) also appeared.25 (In this last case, with a probable residual instability associated to lesion of the medial collateral ligament and assessed in 2 patients [2.4%], with follow-up of 9 years.)
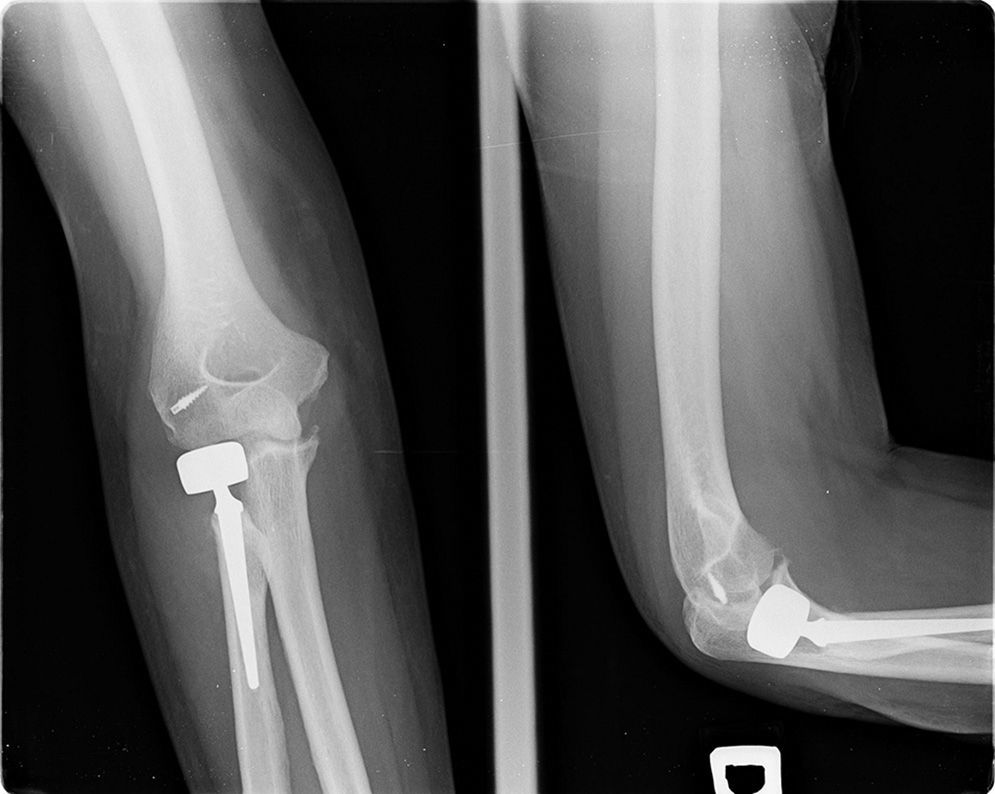
The main complications arose in 10 (47.6%) of the 22 fractures Mason III and in 20 (35.7%) of the 57 Mason type IV fractures. The most notable of these complications were as follows: heterotopic ossification (Fig. 2) was found in 41.5%. These ossifications were related to the seriousness of the initial lesion and treatment type. The more extensive the approaches were, and the greater the soft tissue manipulation, the more ossifications there were. The most frequent places for these heterotopic calcifications were the anterior capsule (35.7%), the entire neck (28.6%) and the medial and lateral region concomitantly (21.4%). The patients with heterotopic ossifications presented greater rigidity (appearing in 50% of the cases, compared with 16.7% in the group without heterotopic ossification) and worse final MEPS result, with 75 points (±23) for the group with ossifications, against 84.3 points (±15.2) for the groups without calcifications, although without statistically significant differences (P=0.51). For the cases with ossification, the medical treatment consisted of indomethacin, at 75mg/day for some 6 weeks. This treatment was preventative, from the postoperative period, and not once these ossifications had been established. When there was soft tissue involvement or coexistence of other lesions, visible before prosthesis placement, this treatment was begun, although this also depended on each surgeon. Indomethacin was used in 14.6% of the patients. Only a quarter of these cases developed some type of minimal heterotopic ossification. The greatest incidence arose in the patients who were not administered indomethacin and had great soft tissue involvement.
Example of heterotopic ossification. The joint surface was involved, with loss of flexion/extension and pronation/supination (Foruria Grade IIC) following type II fracture of the radial head and coronoid. Observe the calcifications in the anterior capsule and coronoid, as well as in the area of triceps insertion. Open arthrolysis was necessary.
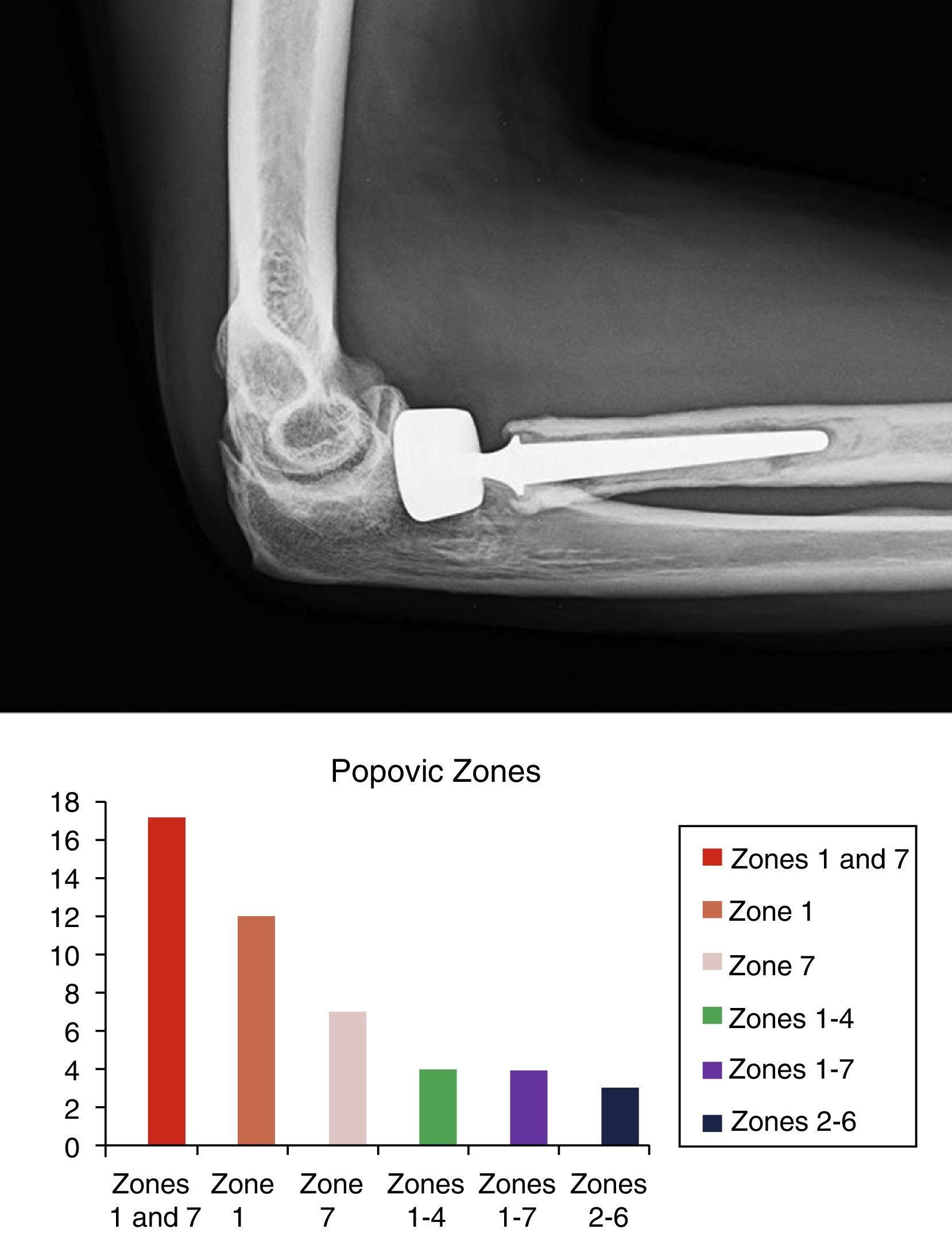
We observed prosthetic mobilisation in 8.5%. In our cases, there was normally associated peri-implant osteolysis.
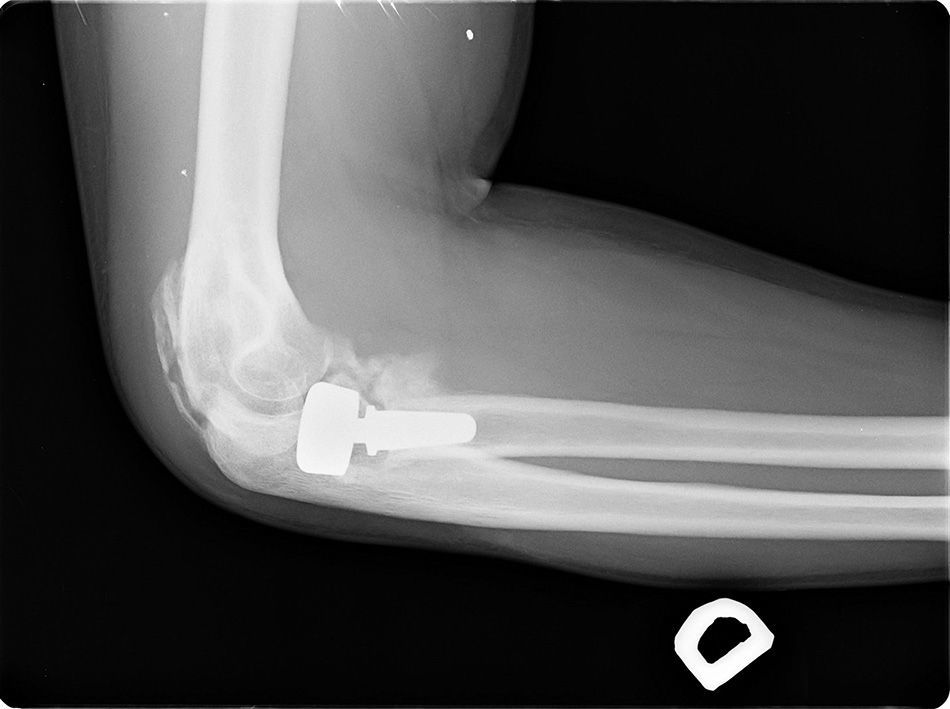
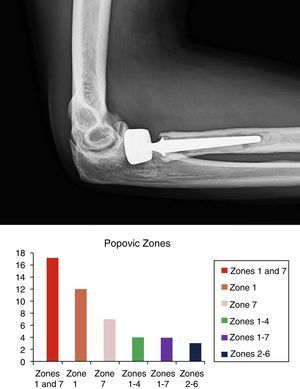
Periprosthetic osteolysis (Fig. 3) was found in 57.3% (47 cases), overlengthening of the head (Fig. 4) in 15.9% (13 cases), undersizing of the head in 2.4% (2 cases), and anterior and dynamic subluxation of the radial head in 3.7% (2 cases).
Upper image: example of periprosthetic osteolysis in Popovic zones 1–7. Cemented bipolar prosthesis 3 years after implantation. Lower image: distribution of periprosthetic osteolysis in our series according to the different Popovic zones. Zones 1 and 7 were the most strongly affected.
The zones of prosthetic loosening according to Popovic27 are described in Fig. 3.
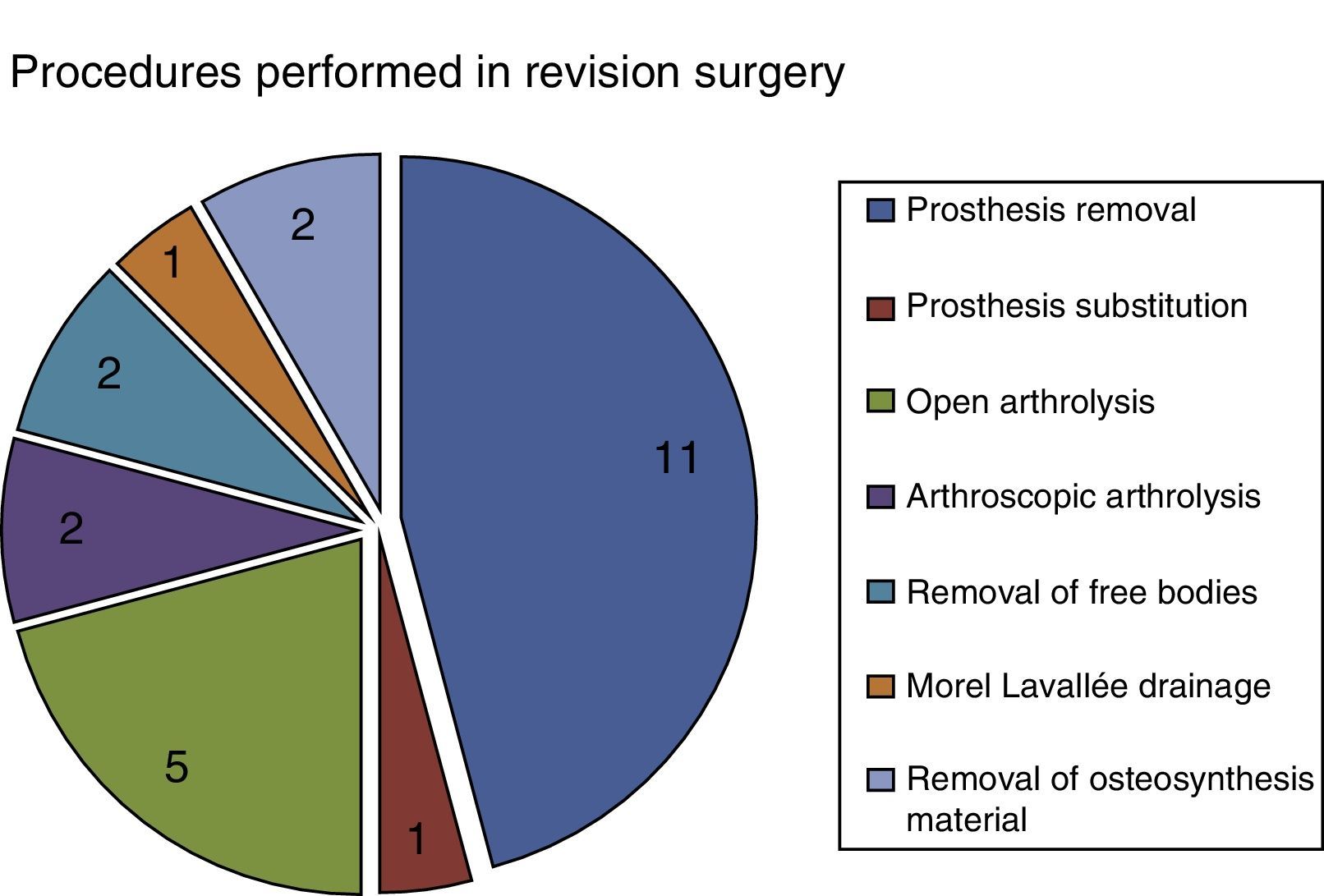
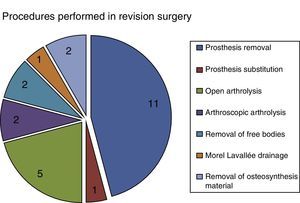
Twenty-four patients (30%) were reoperated; prosthesis removal was necessary in 11 patients (13.4%), where the main cause of removal was pronation/supination pain in 5 cases, capitellar lesions in 4 cases, 1 dislocation and 1 infection. There was 1 case of prosthesis substitution (1.2%). In the remaining 10, no new arthroplasty was placed after removal of the prostheses. The other 12 reinterventions were open arthrolysis in 5 patients (6.1%), or arthroscopic in 2 patients (2.4%). Arthroscopy was also used to remove free bodies in 2 cases (residual elements from the fracture) and to treat 1 case with Morel-Lavallée leak. Osteosynthesis material was also removed in another 2 cases (2.4%) (Fig. 5).
DiscussionRadial head prostheses have improved functional results in patients with complex radial head fractures. There are essentially 2 designs: unipolar or bipolar. The design and material for elbow arthroplasties is controversial.3,28,29
Currently, the results of monopolar metallic prostheses are better than those of silicone4 or carbon pyrolytic prostheses.8 Bipolar implants (whose shafts rotate with a metal-covered, semi-constricted polyethylene head) have also provided favourable results. Holmenschlager,30 after reviewing 16 bipolar prostheses, found 2 excellent results and 12 good (MEPS). Burkhart,31 in 19 patients with bipolar Judet-type implants,32 described 6 with excellent results (MEPS), with 124° of flexion, 21° of extension, 64° of pronation and 64° of supination. In our series, on 82 patients, similar results were achieved, with final flexion of 127.3° (±18.3), extension of 18.5° (±11.8), pronation of 78.7° (±18.8) and supination of 77° (±19.4). Harrington33 carried out a follow-up of 12.1 years after metallic radial head arthroplasty in complex fractures (basically type III), with 20 patients, considering 12 results excellent (60%). Popovic27 reviewed 51 patients (follow-up of 8.4 years), with comminuted fractures, almost all type III, with bipolar prostheses, finding 14 cases of excellent results (27.4%) with Judet prostheses (MEPS). In our study there were 29 cases (35.8% in our series) with excellent results, according to the MEPS. These results differ from those gathered by some authors in the References. Assessment in the MEPS gave these values thanks to early rehabilitation treatment and to the fact that the lower the Mason subtype treated, the better the prognosis was.
The moment of the intervention had an influence, given that the patients operated on the earliest presented better results in the Cassebaum or MEPS scales (P=0.02 or P=0.04, respectively). Likewise, there was a shorter rehabilitation time (P=0.03) in these patients. There is no evidence that supports early surgery.
Studies comparing both types of prostheses in cadavers yielded better results in primary stability for monopolar prostheses, and worse results for the bipolar ones with different dislocation rates or clinical instability.34 That is, when the soft tissues were not sutured the results were superior using monopolar prostheses, but when these tissues were repaired, both prostheses were similar in results. Soft tissue involvement would impact stability more in bipolar implants; for that reason, in cases of extensive soft tissue damage, the monopolar implant would provide greater stability than the bipolar and would be the prosthesis indicated in the opinion of Chantalit.34 In our experience, cases in which the lateral ligament complex was repaired yielded greater rigidity (P=0.03) and more sequelae (P<0.05). In fact, there was associated rigidity in 40.6% and sequelae in 37.5%, with a final MEPS of 78.1 points (±21.9), compared with the cases in which it was not repaired, which yielded 24% rigidity and 20% sequelae, with a final MEPS of 81.9 points (±17.4). However, it is equally true that in the cases in which the lateral ligament complex was damaged and had to be repaired, the greater complexity of the lesions when they affected the ligament was probably what entailed the greatest sequelae. It is difficult to determine why there was greater incidence of rigidity in the cases with associated ligament repair, although perhaps the greater seriousness of the initial injury might influence the results.
In our study we have not been able to detect differences in the mobility results comparing the 3 types of arthroplasty that we used. Other important factors probably exist that determine the final result, such as commencement of postoperative mobilisation,35 severity of the initial injury, associated lesions, surgical duration and so forth.
There is controversy on the influence of the design (bipolar or monopolar) in the clinical and biomechanical results. For Chantalit36 the resistance to posterior subluxation of the anatomical prosthesis (monopolar) is more similar to that of the native head, even though joint contact would be better after bipolar prostheses.37 No prosthesis would remedy the joint surface angle,38 although monopolar prostheses would present lower subluxation indexes in cadavers.39 Bipolar prostheses seem to be better in secondary surgery, even though their bipolarity could cause trochlea damage.37
We found 41.4% of complications, sequelae in 27.1% and instability in 2.9%, using the bipolar design, against an absence of sequelae or instability in the monopolar. For all these reasons, monopolar prostheses are currently used more often, for acute treatment, in our service.37
Fair or poor results in the Mayo Clinic scale (MEPS) were shown in 28.4% of our patients. These worse results were due to the existence of complications.
At this point we should explain that the best results occurred when the LUCL was not repaired, given that the cases in which the LUCL was repaired were high-energy dislocation fractures or associated lesions and these points were factors that worsened the MEPS scale results more than the suture itself.
The main complications of the radial head prostheses found in our series, and in the references, were dislocation or subluxation (clinical instability), radiolucency and osteolysis (signs of loosening), degeneration of the capitellum and insufficient osteotomy.
We observed overlengthening40 of the head in 13 cases (15.8%) in our series. From those, 5 cases were reoperated. Of those, the prosthesis was removed in 4 and an arthrolysis was performed as well in 3 cases, due to the associated functional limitation. Chien4 indicated 23% in the series with overlengthening. The cutting level is important for prosthetic placement, as lengthening the superior radials to 2.5mm causes reduction of pronation/supination, deficit in extension, posterolateral subluxation, capitellar hyperpressure and early osteoarthritis. However, shortening the radius more than 2.5mm provokes valgus hypermobility and proximal migration of the radius. For Athwal16 and Frank,15 medial ulnohumeral joint incongruity apparently occurs only when the size of the proximal radial osteotomy is more than or equal to 6mm of what would be correct. In the opinion of Van Riet17 the distance between the osteotomy level and the proximal border proximal of the lesser sigmoid cavity should be the same as the thickness of the radial head.18 For Athwal16 the implant has to be 1mm less than the sigmoid cavity and, because the head cartilage measures 0.9mm, intraoperative measurements are required, especially of the ulnohumeral joint.40 Anatomical reproduction of the radial head is complicated, and most authors recommend different measurements and techniques for achieving the best surgical result.
The intraoperative X-ray measurements indicate sensitivity of 98%, a positive predictive value of 99.5% and prosthetic subluxation would begin with more than 8mm of overlengthening, which would lead to overestimating implant size; consequently, the decision to revise the implant should depend more on the clinical symptoms (pain and rigidity) than on the X-rays themselves.40
In our experience, the area where prosthetic radiolucencies were most frequent turned out to be the shared involvement of zones 1 and 7 (36.2%). Osteolysis affecting the entire implant surroundings occurred in only 8.5% of the cases. In our series, we observed radiolucencies in 57.3% (47 cases), in follow-up X-rays, although the prosthesis was removed in only 8.5% (7 cases) for loosening and clinical symptoms. Some authors associate early loosening with poor implantation technique and delayed loosening with associated mechanical factors.27 For O’Driscoll41 pain following radial head arthroplasty indicates symptomatic mechanical loosening. Loosening rates have been greater in smooth shaft bipolar designs. Popovic27 found 31 cases of radiolucencies in their series of 51 patients with Judet prostheses, although the presence of radiolucencies did not necessarily involve removal of the implant. Harrington33 described 20 cases of monoblock prosthesis, with 100% radiolucencies, and implant substitution in 20%. Chien,4 in a series of 13 cases (all modular) found no necessity to remove the prostheses. Shore8 indicated up to 31 of their 32 cases with radiolucencies, without requiring prosthesis removal. Zunkiewitz42 gathered 30 cases, all with radiolucencies, with 6.6% of replacement. Popovic,27 in a series of 55 prosthesis, found 27 (53%) with radiolucencies, and the prostheses were removed in only 3 (5.4%) cases. The authors only removed the implants if clinical symptoms were associated.27 Prosthesis loosening was the main cause26 of prosthesis removal. Of their series of 44 patients who underwent prosthesis removal, 31 presented painful loosening. In our experience, 7 cases of prosthesis loosening were found. Of these 7 cases with osteolysis (7.5%) 6 implants were removed and 1 was replaced. According to Van Riet26 the causes of prosthesis failure can be distributed into several groups, with the proportion being, in our experience, the following: pain in 36.6%, rigidity in 30.5%, instability in 6.1% and infection in 3.7%.
Another complication is the risk of lesion to the posterior interosseous nerve, given its proximity to the radial head, 1.2mm (±1.9mm). Holmenschlager30 in a series of 16 bipolar prostheses, found 1 case of nerve palsy and 1 case of reflex sympathetic dystrophy. In our experience there were 2 cases of posterior interosseous lesion, with slow but complete recovery.
We found 41.5% of heterotopic ossifications in our series. This group of patients had 51.5% complications, sequelae in 41.2%, 50% cases with rigidity, and a final MEPS of 75 points (±23). The group without ossifications had complications in 31.9%, sequelae in 16.7%, 16.7% of cases with rigidity and a final MEPS of 84.3 (±15.2 points). In the group with heterotopic ossification, 32% were reoperated, principally for pain and rigidity. Foruria,43 in a review of 142 fractures of the proximal radioulnar, concluded that 37% of these surgically treated elbows developed heterotopic ossification. Foruria proposed a classification system based on joint damage and severity of clinical-radiological involvement, with various subtypes, from IA to IIC.
Other complications were reflex sympathetic dystrophy,30 ulnar neuropathy (in 3 cases in our experience), proximal radioulnar synostosis, persistent pain in the mobilisation, and capitellar erosion (more frequent when the implant was placed after 6 weeks following the trauma26 and with risk of producing osteopenia in the capitellar area in 14 of 32 cases, according to Shore8).
As study limitations we can point out the fact that it was retrospective study; the limited number of patients included, despite the lengthy time to gather the cases (11 years); and the fact that in all this time prosthetic procedures and types have been modified and some were different from those currently available. Another limitation is the fact that the study covers different associated lesions and this might have affected the results. There were no follow-up losses in this study. However, various surgeons participated, having different levels of experience, which might constitute another limitation in the results obtained. There was also interobserver variability in data interpretation of the clinical cases, which could have led to classifying fewer cases of terrible triads, when a coronoid fracture coexisted. As study advantages, we consider that the number of cases and their heterogeneity is representative of a unit or team that habitually handles this type of trauma.
ConclusionsIn our series we found 70% good and excellent clinical results in patients with unstable radial head fractures. A less important initial lesion and early surgery seem to be factors that improve prognosis, without the use of a specific arthroplasty type being definitive. Fair or poor clinical results were obtained in approximately 30% of the patients and the complication rate was high.
Monopolar prostheses seem to provide greater stability in primary surgery.
Special attention should be given to the size of the head intraoperatively and it should be monitored afterwards radiographically.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of persons and animalsThe authors declare that the procedures followed comply with the ethical regulations of the appropriate committee on human experimentation and are in agreement with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects mentioned in this article. This document is held by the corresponding author.
Conflict of interestThe authors have not received any economic funding for this study. Neither have they signed any agreement by which they are to receive benefits or fees from any commercial entity; nor has any commercial entity paid, or will pay, foundations, educational institutions or other non-profit organisations to which the authors are affiliated.
Please cite this article as: Contreras-Joya M, Jiménez-Martín A, Santos-Yubero FJ, Navarro-Martínez S, Najarro-Cid FJ, Sánchez-Sotelo J, et al. Artroplastia de cúpula radial, experiencia de 11 años. Estudio sobre 82 pacientes. Rev Esp Cir Ortop Traumatol. 2015;59:307–317.