To describe the incidence, etiological factors, functional impairment and therapeutic management of scapular fractures after reverse shoulder arthroplasty (RSA) in rotator cuff arthropathy.
Material and methodA retrospective study was conducted on 126 RSA between 2009 and 2011, in which four fractures were identified that were compared with a control group of 40 patients. An analysis was performed on the variables related to the surgical technique, functional results, and quality of life (Constant scale, EQ-5D).
ResultsThe fracture incidence was 3.28% with a mean age of 74.7 years. The mean time until diagnosis was 11.9 months.
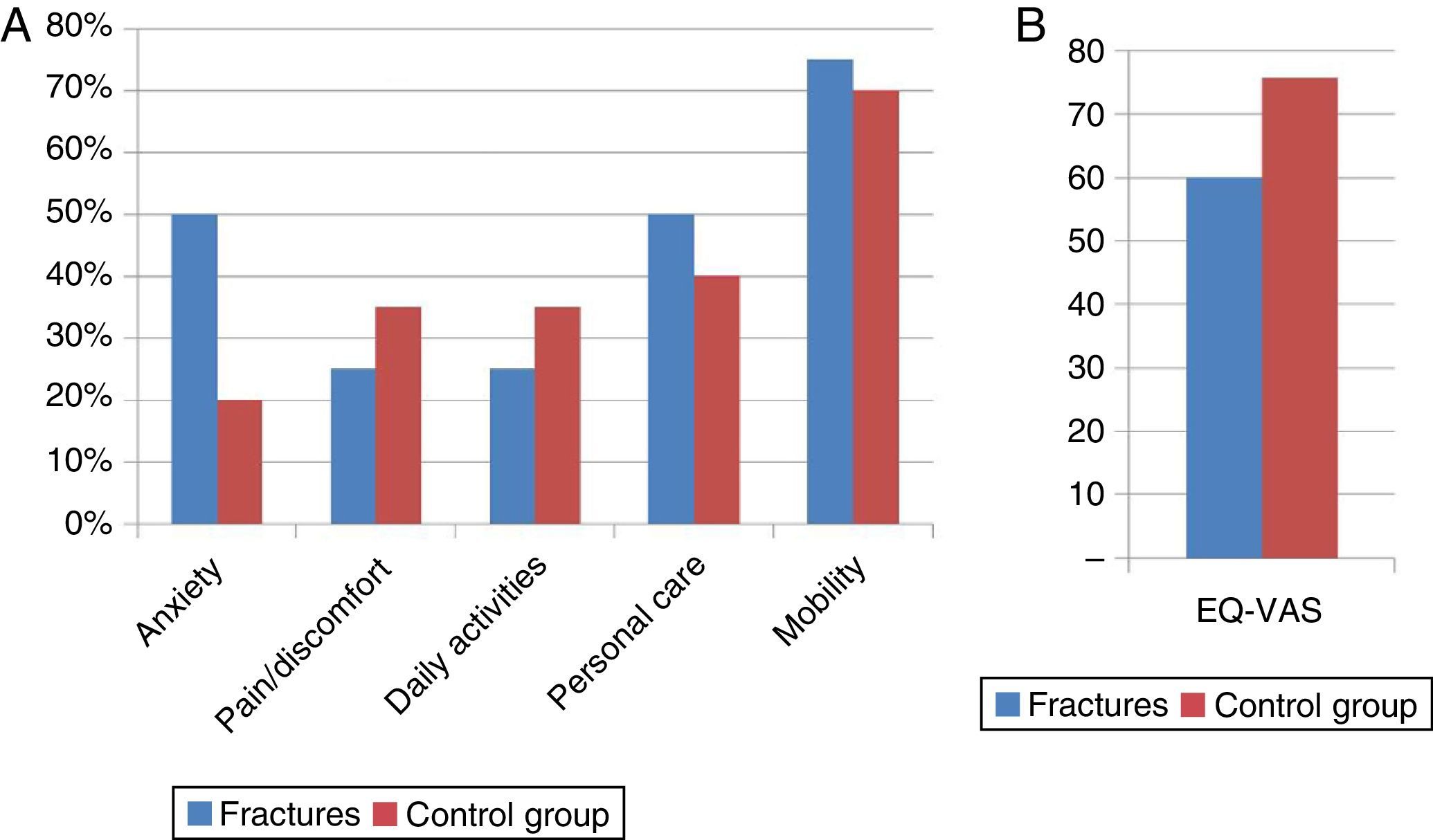
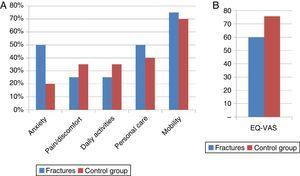
The preoperative Constant score in the control group was 37.3%, and 34.7% in the fracture group (P>.05); postoperative Constant score: 81.2 and 66.5%, respectively (P>.001). Forward elevation and abduction in fracture patients decreased by 39° (P=.02), and 34° (P=.057) respectively. The perceived quality of life (EQ-VAS) was lower in the fracture group (60 vs. 76) (P=.002).
There were no instability cases, and no revision surgery was required. The union rate was 50% after a mean follow-up 39.6 months.
ConclusionsScapular fracture after RSA is a rare complication. Despite its presence, the functional outcomes and quality of life of these patients are higher than preoperatively; however, they are lower than that obtained in patients with RSA without this complication. More prospective studies are needed to define guidelines for therapeutic action against this complication.
Describir la incidencia, factores etiológicos, repercusión funcional y actitud terapéutica de las fracturas de acromion y espina de la escápula tras artroplastia invertida por artropatía de manguito rotador.
Material y métodoAnálisis retrospectivo de 126 artroplastias inversas entre los años 2009–2011. Se identificaron 4 fracturas que se compararon con un grupo control de 40 pacientes. Se analizan variables relacionadas con el proceso quirúrgico, funcionales y de calidad de vida (escala Constant, EQ-5D).
ResultadosLa incidencia de la fractura fue 3,28% (4 pacientes), edad media 74,7 años y tiempo medio hasta el diagnóstico 11,9 meses.
El Constant preoperatorio del grupo control fue de 37,3% y de los pacientes con fractura 34,7% (p>0,05); el postoperatorio 81,2% y 66,5%, respectivamente (p<0,001). La anteversión y abducción en los pacientes con fractura descendieron en 39° (p=0,02) y 34° (p=0,057) respectivamente con respecto al grupo control. La calidad de vida percibida (EQ-VAS) es inferior en el grupo de fractura (60 vs 76) (p=0,002).
En ninguno de los casos de fractura se observó inestabilidad, no precisando cirugías de revisión. La tasa de consolidación fue de un 50% tras un seguimiento medio de 39,6 meses.
ConclusionesLa fractura de escápula tras artroplastia invertida es una complicación poco frecuente. A pesar de su aparición los resultados funcionales y de calidad de vida de estos pacientes son superiores a los presentes preoperatoriamente, sin embargo, resultan inferiores a los de los pacientes intervenidos en los que no se encuentra dicha complicación. Son necesarios más estudios prospectivos que nos ayuden a definir las pautas de actuación terapéutica ante esta complicación.
Scapular stress fractures after reverse prosthesis implantation are a relatively rare complication, with its incidence ranging between 0.8% and 7.2% in the different series.1–14 However, an increase in these fractures is to be expected with the growing use of this type of arthroplasty and the ever-expanding knowledge of its existence that surgeons that perform this implantation have. These facts lead to clinical suspicion even when the diagnosis is often not so apparent with simple radiography. Its aetiology and treatment have not been completely clarified. Various studies reveal that the functional result remains unchanged after its occurrence, while others disagree as to surgical treatment vs. conservative.5,8
The objective of this study was to determine the incidence, aetiological factors, functional repercussion and therapeutic technique of acromial fractures found in a series of reverse arthroplasties implanted using rotator cuff arthropathy.
Material and methodThis was a retrospective analysis of a series of 126 reverse arthroplasties consecutively implanted using rotator cuff arthropathy between 2009 and 2011 in our centre. We excluded four cases from the study due to loss during follow-up.
Criteria for inclusion were all the patients in which a reverse arthroplasty had been performed in rotator cuff arthroplasty and that presented a fracture of the anterior acromial process or of the scapular spine, with a minimum follow-up of 2 years from its onset.
The presence of fracture of the acromion was established using simple radiography and computed axial tomography CAT scan following clinical suspicion (sudden pain in the posterior face of the shoulder and/or poor progress in joint mobility improvement). A total of 4 fractures (3 fractures of the acromial process and 1 of the acromial base) were identified in 4 patients. In all the cases conservative treatment was initially given, consisting of sling immobilisation for 6 weeks (allowing pendulum exercises from the first) and then assisted and active exercises for rehabilitation based on tolerance.
The data gather included the following: age, sex, degree of arthroplasty,15 antecedents prior to surgery in the shoulder involved, approach type used and time from prosthetic implantation to appearance of the fracture.
Once the cases of fracture had been identified, we determined the number of patients without fractures required as a control group for a study strength of 80%, which would permit detecting differences of 35° in joint mobility in abduction and anteversion, and of 15 points in the Constant scale. The control group consequently consisted of 40 patients extracted from the remaining series (118 patients), divided into 4 groups of 10 patients (if there were more than 10 patients, the selection was made randomly) with similar demographic characteristics (age, sex, degree of arthroplasty) and follow-up from implantation in the patients with fractures (10:1). This was done to attempt to determine if the functional results after fracture appearance were poorer or not than the functional results after fracture absence, as well as the repercussion on the quality of life that the patients perceived.
Surgical techniqueAfter pleural block and using general anaesthesia, the patient is placed in a semi-sitting (beach chair) position. The patient is intervened by one of the three surgeons specialised in shoulder surgery (generally at least 2 of these 3 surgeons are always present, so decision-taking in the operating theatre is always joint). The mean surgery length was 54min (43–72). Mean hospital stay after surgery was 5 days (2–7).
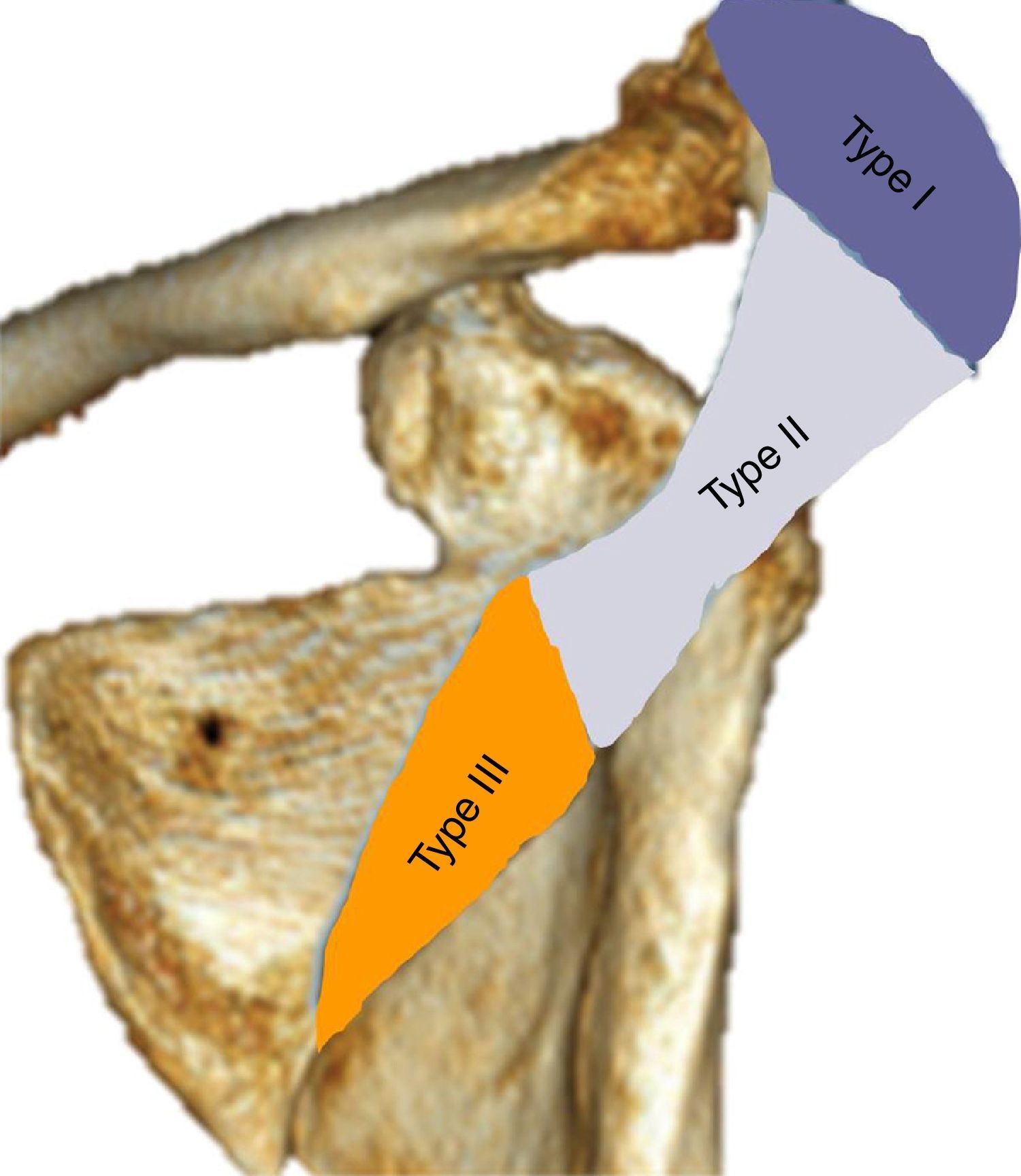
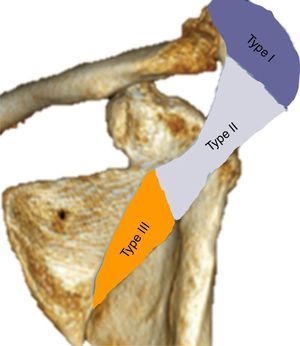
To classify the fractures the system proposed by Levy et al.16 was used: Type I affects a portion of the middle and anterior deltoid, Type ii affects the entire origin of the middle deltoid and Type III affects the entire middle and posterior deltoid origin (Fig. 1).
Classification of fractures of the acromion according to Levy et al.16.
Functional results were evaluated before and after surgery, and after a minimum of 2 years from fracture appearance, using the Constant scale adjusted for age and sex17 and measurement of joint mobility. To assess quality of life, we used the EuroQol 5 dimension questionnaire (EQ-5D) score.18,19
Statistical analysisWe used the Fisher exact test to compare categorical variables between the 2 groups and the Wilcoxon test to compare continuous variables. The Mann–Whitney U test was used to determine if the patients with acromial fracture presented a clinical result and quality of life lower than the control patients withtrol, while Student's t-test was used to determine if the patients with acromial fracture presented range of movement lower than the control group (statistical significance P<.05).
ResultsEpidemiological resultsThe incidence in our series of fractures of the acromion and/or of the scapular spine was 3.28%.
Mean age for the complete series (122 cases) at the time of operation was 81.6 years (70–92) and the surgical indication was in all cases Grade 3 or higher (Hamada classification) rotator cuff arthroplasty. Mean follow-up for the entire series up to the time of revision was 47.6 months (range 29–72 months). In 76% of the cases, the patient was female, while the dominant arm was operated in 75%. We found three cases of bilaterality. The superolateral approach was used for implantation in 73% of the arthroplasties and the remaining 27% by deltopectoral approach.
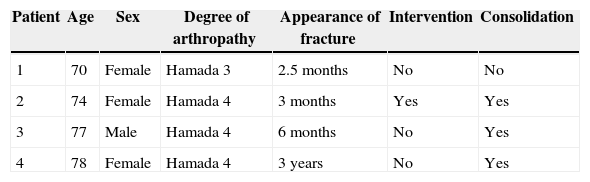
Four patients with acromial fracture were identified. Mean age for this group was 74.7 years. In 3 cases there was a Hamada classification Grade IV arthroplasty and in 1, a Grade III. Mean time to fracture diagnosis was 11.9 months. Females represented 75% of the cases. The epidemiological results are summarised in Table 1. Among the predisposing factors we identified osteopenia in 3 cases, female sex in 3 cases and Hamada classification Grade 3 or superior arthroplasty in 4 patients. None of the 4 patients did sports activities or had physically demanding jobs, with their activity being limited to basic tasks of daily life. As for the approach used, in 3 cases a superolateral approach was used and in 1, a deltopectoral. The sizes of the glenospheres implanted were as follows: in 3 patients, 38mm, and in 1 patient, 42mm. None of the 4 patients with fractures had other factors such as deformities of the proximal humerus, performance of untimely manipulations (either during the surgical intervention or during rehabilitation), rheumatoid arthritis or previous subacromial decompression. All of the patients lacked any traumatic antecedents.
Demographic characteristics of the patients with fracture of the scapula.
| Patient | Age | Sex | Degree of arthropathy | Appearance of fracture | Intervention | Consolidation |
|---|---|---|---|---|---|---|
| 1 | 70 | Female | Hamada 3 | 2.5 months | No | No |
| 2 | 74 | Female | Hamada 4 | 3 months | Yes | Yes |
| 3 | 77 | Male | Hamada 4 | 6 months | No | Yes |
| 4 | 78 | Female | Hamada 4 | 3 years | No | Yes |
The control group was composed of 40 patients (10 for each case) extracted from the remaining series without acromial fracture (118 patients), with demographic characteristics similar to each of the 4 fractures: mean age of 76.5 years, 30 women and 10 men with arthroplasty greater than or equal to Hamada classification Grade 3 and mean follow-up of 44 months. All the control group patients had a superolateral approach, except for the group of 10 patients paired with 1 of the fracture cases with deltopectoral approach. From this group of 10 patients, 3 presented a deltopectoral approach and 6, a superolateral, given that 10 control cases with deltopectoral approach and the same demographic characteristics were not found.
We did not find any statistically significant differences between the demographic characteristics of the 2 groups (P>.05), so they were considered comparable.
We found no statistically significant relationships between the main surgeon and length of surgical intervention, although the sample was very small (4 patients) to be able to detect them.
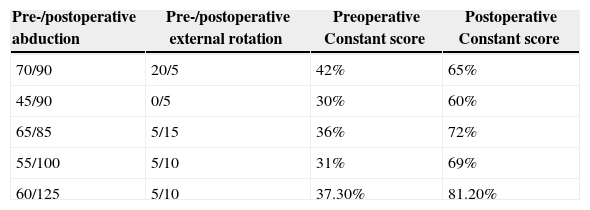
Clinical resultsThe preoperative mean Constant score normalised for age and sex of the entire series (122 patients) was 36.4%, that of the patients with fracture was 34.7% and that of the control group, 37.3% (P>.05). Consequently, there were no statistically significant differences in the preoperative functional condition between the 2 groups under study. The mean preoperative Constant score for the control group, at a follow-up similar to that of the patient with which each group was paired, was 81.2%; this mean value for the patients with fracture was 66.5% (P<.001). Table 2 summarises the results of the 4 patients with acromial fracture at 2 years after its appearance. Although the Constant score of the 4 patients was lower than the preoperative Constant value for the control group, all patients presented a post-fracture Constant score higher than the one they had preoperatively (P<.001).
Joint mobility and postoperative Constant score.
| Pre-/postoperative abduction | Pre-/postoperative external rotation | Preoperative Constant score | Postoperative Constant score |
|---|---|---|---|
| 70/90 | 20/5 | 42% | 65% |
| 45/90 | 0/5 | 30% | 60% |
| 65/85 | 5/15 | 36% | 72% |
| 55/100 | 5/10 | 31% | 69% |
| 60/125 | 5/10 | 37.30% | 81.20% |
The postoperative Constant score was evaluated after a minimum of 2 years’ fracture development and in each of the 4 control groups; this is a mean follow-up similar to that of the patient paired with the group.
As for joint mobility in flexion, abduction and external rotation, Table 2 presents the figures for the fracture cases, as well as the mean values for the control group. The patients with fracture showed a mean decrease of 39° in anteversion with respect to the control group (P=.02), while the mean decrease in abduction was 34° (P=.057). No statistically significant differences (P>.05) were found for external rotation. The patient with scapular spine fracture (Patient 2) presented a greater reduction in joint mobility than the patients with Type I fracture (anterior section of the acromion).
The percentage of problems reported for both groups (fracture and control group) in each of the items that the EQ-5D assesses can be seen in Fig. 2A. The results are similar for both the fracture and control group (P>.05); however, the quality of life perceived as per the EQ visual analogue scale (EQ-VAS) is lower in the patients that had some type of fracture (60 vs. 76) (P=.002) (Fig. 2B).
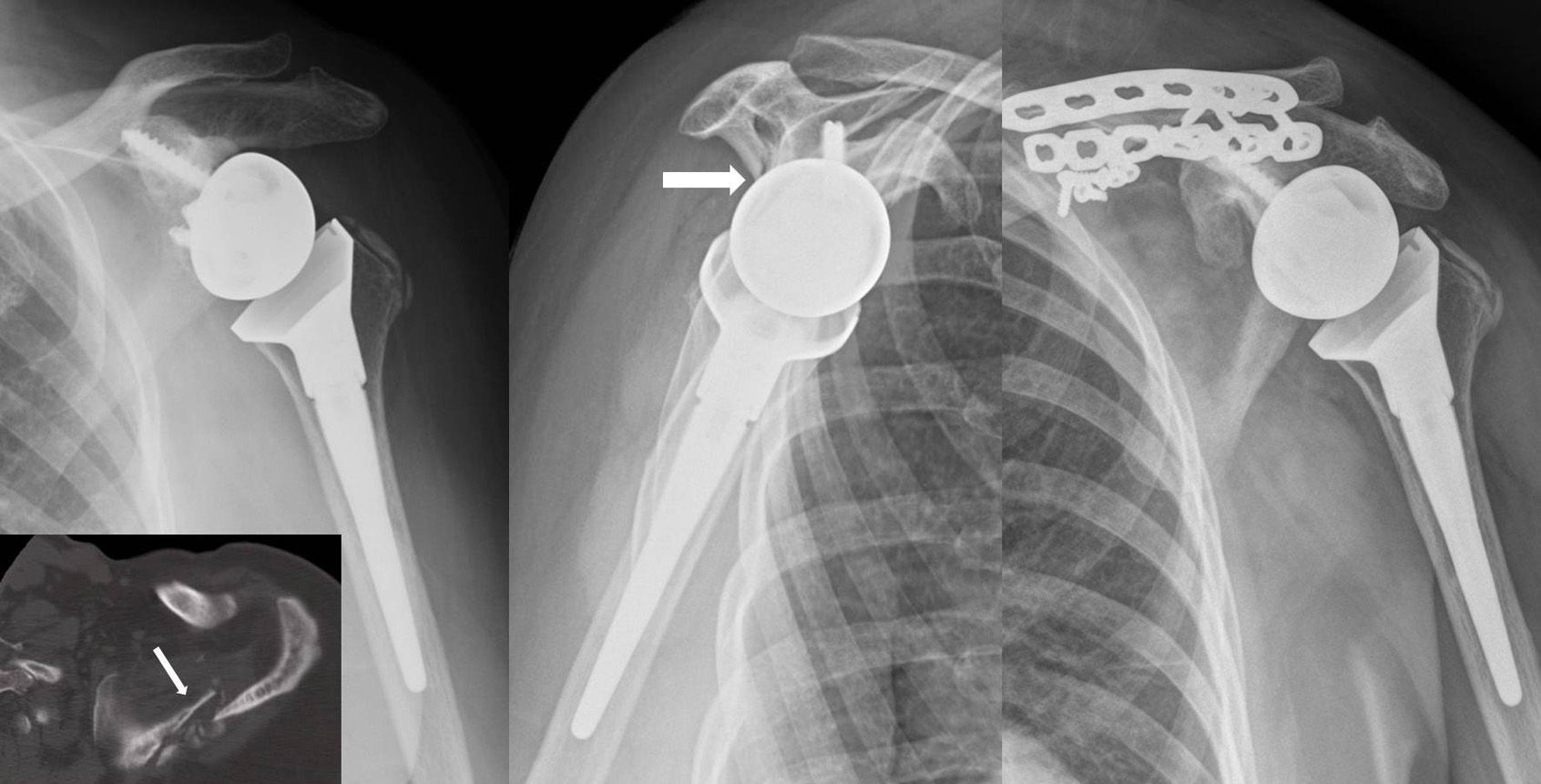
None of the 4 cases required revision surgery for the prosthesis, nor were any cases of instability associated to fracture presence found. Only the scapular spine fracture required surgical treatment through open reduction and plate osteosynthesis for persistence of pain.
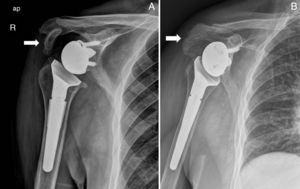
Radiographic resultsAfter analysing our series results, we found 3 fractures that affected the anterior section of the acromion (Type I in the Levy classification) and 1 that affected the base of the acromion or scapular spine (Type III in the Levy classification).
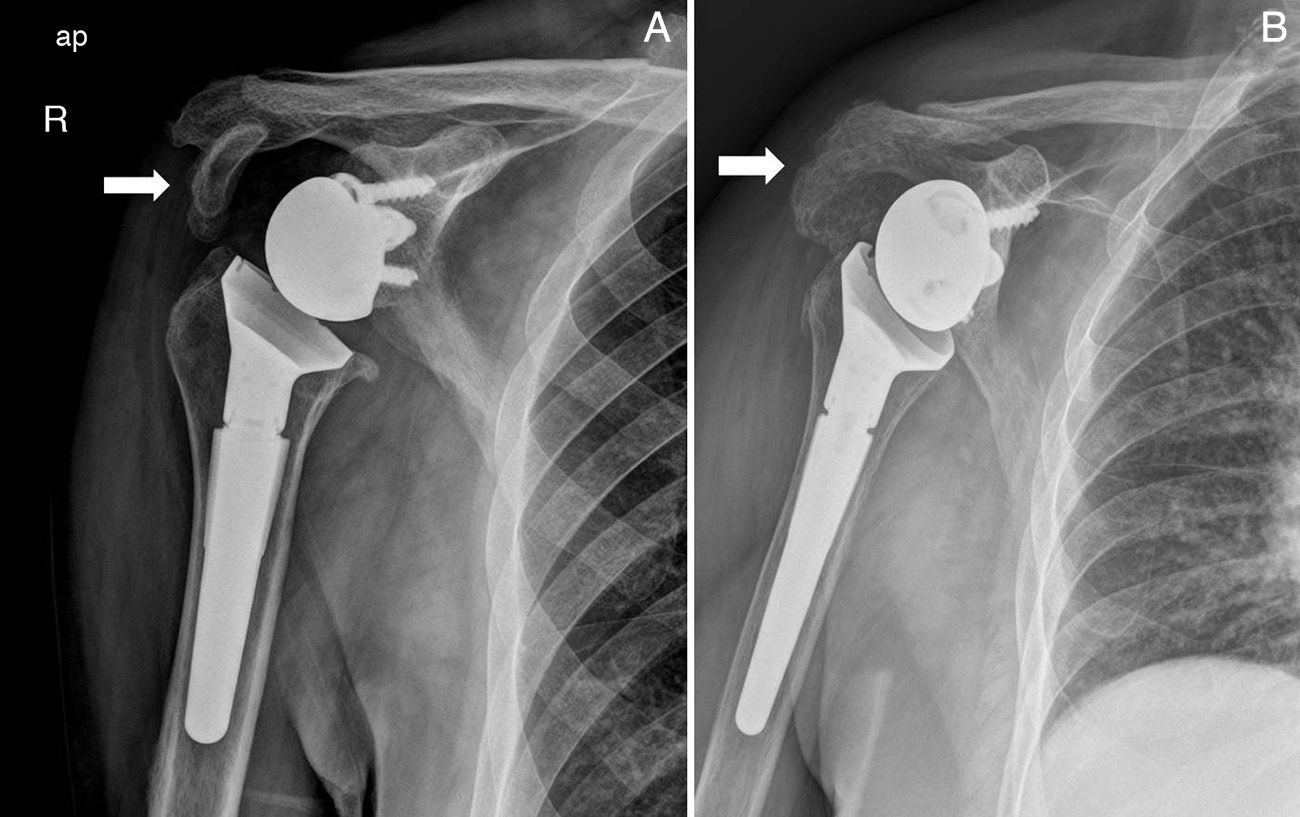
After a mean follow-up of 39.6 months, we found 2 cases of consolidation. These were, firstly, 2 fractures that affected the anterior section of the acromion (Fig. 3A), and then 1 case of painless pseudoarthrosis corresponding to the third case of fracture of the anterior acromial process anterior (which did not affect the stability of the prosthetic component and was consequently not treated (Fig. 3B). Finally, there was 1 case of painful pseudoarthrosis in the scapular spine fracture that required surgical reintervention and osteosynthesis with 2 plates (Fig. 4). The consolidation rate was consequently 50%.
Fracture of the scapula after reverse implantation of a prosthesis is a complication that is perfectly defined, but rarely understood.
The incidence in our series was approximately 4%, in agreement with the data from previous publications.1–14 It is a rare complication, although it is probably underdiagnosed due to how difficult it is to detect. Simple radiology is often insufficient and it should be the clinical suspicion (sudden pain following an appropriately evolving arthroplasty) that leads us to confirm it using additional diagnostic tests such as the CAT scan.
Its etiopathogenesis is unclear. Several factors are involved. Among preoperative factors, acromion weakness secondary to acetabulisation and thinning in advanced states of rotator cuff arthropathy undoubtedly play an important role. If the subscapular muscle is intact in these cases, erosion is more posterior, which affects the scapular spine or the base of the acromion, more than its anterior section. The aetiology would be easy to establish, with a humeral head indenting on a weakened bone. However, we find cases of fractures of the acromion or of the scapular spine in the face of rotator cuff tear that are unaccompanied by head ascension as such. Coiradas et al.20 explained their existence by a scapular kinematic alteration secondary to the rotator cuff injury (which increases the activity of the muscles with origin and insertion in the scapular spine or base of acromion while elevating the arm), combined with the presence of reduced mineral-density bone and micro-architectural changes (such as those occurring in osteoporosis). A weakened osteopenic bone is generally the rule in patients with this type of disease, in which there is also a clear female dominance. Our series had a mean age of 81 years and 76% were females.
Among intraoperative factors, the intraoperative fracture – although barely present in the literature – should also be kept in mind. The deltopectoral approach has been linked to a greater incidence of these fractures.21 However, other authors did not find differences based of the approach used (deltopectoral or superolateral).22 Of the 4 cases of acromial fracture that we found, 3 occurred after a superolateral approach, while 1 took place after using a deltopectoral approach. In our series, the limited number of patients with acromial fracture and its greater prevalence in the use of the superolateral approach with respect to the deltopectoral (73% vs. 27%) makes it possible for us to detect differences in the incidence of these fractures in relation to the approach used. The position of the metaglene screws has also been proposed as being involved. The screws placed in the posterior-superior quadrant of the glene are directed precisely at the base of the acromion. This might cause additional stress in that area and facilitate fracture development.3 Of the 4 fracture cases that we present, we did not find any screws placed near or in the base of the acromion in the CAT scan taken after their appearance.
Other intraoperative factors, such as over-sizing the head to avoid scapular notching, or untimely manipulations to carry out the reduction, were not found in this series.
Finally, postoperative factors related to the design of the implant itself also appear to be involved. Some authors have indicated that the stress generated in the deltoid by placing the glenosphere is one of the main causes.1 After reverse prosthesis implantation, the arm become approximately 2.5cm longer. This increases the tension over the deltoid; this, together with the increase in the lever arm that causes medialization of the centre of rotation, make the loads on the acromion rise in turn.
As for functional results, just as in other studies,7,8,23 in our series the patients with scapula fractures have worse functional results than those that do not present this fracture. However, the final result is always better than the preoperative state.
We agree with Teusink et al.23 in that this type of fracture could occur at any point in the follow-up. They indicated that they had found fracture occurrence dating from 4 weeks up to 8 years, and our 4 cases were found from 2.5 months to 36 months. These authors indicated that the location of the fracture (scapular spine or acromion) did not affect functional results. Our patient sample is limited and we cannot infer this directly from our results. However, based on our experience with stress fractures of the scapular spine (without prosthetic implantation)20 and on the existing bibliography,8,22 we consider that fractures of the scapular spine constitute a different problem from fractures of the anterior process of the acromion. In these fractures, the entire middle and poster deltoid origin is affected and the stress, after a reverse arthroplasty, is essential for a stable and functional shoulder; this fact could justify the greater reduction in mobility that the patient in our series with scapular spine fracture experienced in comparison with the others. When the acromial fracture occurs more laterally, the scapulothoracic movement remains unaltered. This would explain that fact that patients with a significant displacement had a range of movement similar to those that did not have it,24,25 as was demonstrated by the similarity in functional results obtained among the patients presenting fracture of the anterior acromial process, independently of the consolidation position.
The acromion was not found to be fragmented in any of our cases preoperatively (prior CT control) and simple radiographic study in the immediate postoperative period showed no evidence of any fractures. We found a pseudoarthrosis rate of 50%, in line with what the literature describes. Teusink et al.23 presented a consolidation rate of 57% for the fractures of the anterior acromial process (8 out of 14) and of 50% for the fractures involving the scapular spine (2 of 4). Rouleau et al., in their review of the literature, identified 30 cases of fracture of the base of the acromion and of the scapular spine,26 21 of which were treated conservatively with a sling, 7 were treated by open reduction plus internal fixation, and 1 by revision of the prosthesis. Among those treated conservatively, 14 did not consolidate, 4 did so in poor position and in 2 cases it was not clear whether consolidation was achieved. Among the patients that were treated using fracture fixation, 1 did not consolidate, 2 cases required repetition of the fixation, and 1 patient needed to have the osteosynthesis material removed. The patient that required revision surgery of the reverse arthroplasty presented consolidation in a poor position of the fracture.
The fact that the series published on this matter contain such a limited number of cases makes it difficult to establish formal treatment guidelines. Wermer13 questioned internal fixation. Walch et al.22 as well felt it was inadvisable after fixation failure in 1 of the 4 cases in their series, recommending a splint in abduction to prevent displacement or inferior inclination of the acromion. Rittmeister and Kerschbaume12 also described failures in osteosynthesis in almost half of their cases.
Our study does not allow us to answer the question as to which is the best treatment for this type of fracture. However, analysing the previously mentioned pathogenesis, it seems reasonable to recommend fixation for fractures that affect the insertion of the majority of the deltoid (fractures of the scapular spine or base of the acromion) because of the repercussion that it involves in implant stability and in function obtained.
Study limitationsStudy limitations are its retrospective character and the limited number of patients with this type of complication.
Level of evidenceLevel of evidence III.
ConclusionsWith the same follow-up, patients with postoperative scapular fracture present worse clinical results than patients with a reverse arthroplasty that do not present this complication.
This complication requires no previous trauma at all for its appearance.
This is a rare complication that should be suspected when rehabilitation progresses slowly, is painful or there is a sudden deterioration of functional results, and it can appear at any time during follow-up.
Further prospective studies are needed that make it possible to define therapeutic guidelines for this complication.
Ethical responsibilitiesProtection of personas and animalsThe authors declare that no experiments were performed on human beings or animals in this research.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Lópiz Y, Rodríguez-González A, García-Fernández C, Marco F. Fracturas de estrés de la escápula tras artroplastia invertida en artropatía de manguito: ¿cuál es su repercusión funcional?. Rev Esp Cir Ortop Traumatol. 2015;59:318–325.