To identify and quantify the risk factors for in-hospital mortality in patients older than 65 years with a hip fracture.
Materials and methodsRetrospective review of prospectively collected data. We studied a cohort of 331 hip fracture patients older than 65 years of age admitted to our hospital from 2011 to 2014. Patients demographics, type of residence, physical function, mobility, prefracture comorbidities data, cognitive status, anti-aggregant and anticoagulant medication, preoperative haemoglobin value, type of fracture, type of treatment, surgical delay, and complications, were recorded.
ResultsThe average age was 83, 73% female, and 57% had sustained a subcapital fracture. In 62.8% pre-fracture baseline co-morbidities were equal or greater than 2. The in-hospital mortality rate was 11.4%. In univariate analysis, age over 90, male gender, haemoglobin ≤10g/dl, no antiplatelet agents, orthopaedic treatment, number of co-morbidities ≥2, Charlson index ≥2, age-adjusted Charlson index ≥6, congestive heart failure, asthma, and rheumatologic disease were associated with in-hospital mortality.
ConclusionsPreoperative patient-related factors have a strong relationship with in-hospital mortality in a hip fracture patients aged older than 65 years. These factors are non-modifiable; we recommend the development of protocols to reduce in-hospital mortality in this group of patients.
Identificar y cuantificar los factores relacionados con la mortalidad intrahospitalaria en pacientes mayores de 65 años con fractura proximal de fémur.
Material y métodosEstudio observacional de cohortes retrospectivo de una base de datos prospectiva de pacientes mayores de 65 años con fractura proximal de fémur entre 2011 y 2014. Se incluyeron en el estudio 331 pacientes. Se registraron variables demográficas, procedencia del paciente, grado de deambulación y dependencia, comorbilidades asociadas, estado mental, toma de medicación anticoagulante o antiagregante, valor de la hemoglobina al ingreso, tipo de fractura, tipo de tratamiento, demora quirúrgica y presencia de complicaciones.
ResultadosLa edad media de los pacientes fue de 83 años. En un 73% eran mujeres. Y el 57% presentaron fractura subcapital de fémur. El número de comorbilidades era igual o mayor de 2 en un 62,8%. La mortalidad intrahospitalaria fue del 11,4%. En el estudio univariante, la edad mayor de 90 años, sexo varón, no antiagregación, el tratamiento ortopédico de la fractura, un valor de la hemoglobina≤10g/dl, un número de comorbilidades≥2, un índice de Charlson≥2, un índice de Charlson ajustado a la edad≥6, la insuficiencia cardíaca, el asma, la enfermedad reumática, fueron variables asociadas a la mortalidad intrahospitalaria.
ConclusionesLos factores preoperatorios relacionados con el paciente influyen directamente en la mortalidad intrahospitalaria del paciente con fractura proximal de fémur mayor de 65 años. Dado que estos factores no son modificables, recomendamos el desarrollo de protocolos de actuación que permitan reducir la mortalidad intrahospitalaria en este grupo de pacientes.
Hip fractures (proximal femur fractures) are both a medical and social problem because the incidence in the elderly is so elevated. In spite of the advances in surgical treatment and regional anaesthesia techniques, the published mortality rates after hip fracture are still very high, ranging between 6% and 9% in the first month after the fracture, between 13% and 19% at 3 months and from 26% to 33% at a year.1–5
In-hospital hip fracture mortality is defined as the number of patients with hip fracture that die during their hospital stay multiplied by 100, divided by the total number of patients with hip fracture. The Spanish National Healthcare System considers it to be an inpatient quality indicator for hospitals.6,7 That is why reducing this indicator as much as possible should be a primary objective for orthopaedic surgery and trauma services.
Giannoulis8 reviewed the last few years of publications on mortality in the first month after surgery and concluded that there was a lack of consensus about patient management protocols, optimum surgical delay time, rehabilitation protocols and length of hospital stay. These disparities make it complicated to compare data and apply similar multidisciplinary approaches.
The factors associated in the literature with 30-day mortality in different studies can be grouped into modifiable and non-modifiable. The first are patient-related, such as age, sex, comorbidities and fracture type; while non-modifiable factors have to do with treatment, such as surgical delay, anaesthesia technique or type of surgery.9–13 There are not many studies on in-hospital mortality in proximal hip fracture, either prospective14–16 or retrospective,3,17,18 that allow us to know the factors having the greatest influence.
Our working hypothesis was that the patient-related factors would have a greater influence on in-hospital mortality in the patient with hip fracture. To verify this, our main objective was to identify and quantify the prognostic factors having to do with in-hospital mortality in patients older than 65 years with hip fracture in our hospital.
Materials and methodThis was a retrospective observational study of cohorts of the patients older than 65 years in our prospective hip fracture database between January 2011 and December 2014. The criteria for exclusion were age less than 65 years, pathological fracture, victims of multiple traumas, bilateral fracture, or history of previous hip fracture.
Patient age, sex and origin were recorded upon admission. The type of hip fracture was classified as subcapital fracture, pertrochanteric fracture and subtrochanteric fracture.
The presence of associated comorbidities was established by the patient history or by review of previous hospital admissions. Comorbidities registered were high blood pressure, auricular fibrillation, heart failure, heart disease, cerebrovascular disease, dementia, epilepsy, Parkinson's Disease, Chronic Obstructive Pulmonary Disease, asthma, diabetes, rheumatic disease, renal failure and peripheral vascular insufficiency.19 We recorded the number of comorbidities, Charlson Comorbidity Index (CCI)20 and age-adjusted CCI.21 Administration of anticoagulant and antiaggregant medication was also registered.
Cognitive state was evaluated with the Mini-Mental State Examination,22 in which the maximum score was 10, with 6 points or less being indicative of dementia.
The patients’ functional status before the fracture was established using the Parker Mobility Score23 for walking and the Katz Index24 for the dependency in 6 activities of daily living. Patients were considered to have limited mobility of they needed the help of another person to walk at home or in the street, and total dependence if they required another person's help to perform 3 or more daily living activities.
Haemoglobin (Hb) levels were recorded on admission. Blood transfusion was indicated if the Hb was less than 8g/dl, and values between 8g/dl and 10g/dl were indicative of anaemia.
Healthcare for the patient with hip fracture was conventional during the study period. The patient was assessed by the emergency physician and the trauma specialist, medication was adjusted and the patient was admitted. On the hospital ward, the trauma specialist evaluated patients on a daily basis, and requested consultation with the Anaesthesiology Service. If needed due to patient stabilisation or review of prior medical treatment, assessment by the Internal Medicine Service was requested. Surgical delay was set by the Anaesthesiology and Resuscitation Service based on the need for preoperative stabilisation of the patient, or on anticoagulant or antiaggregant drugs. Acetylsalicylic acid at 100mg did not cause surgical delay. The surgical technique indicated depended on the type of fracture: osteosynthesis with cannulated screws for non-displaced subcapital fractures; cemented partial bipolar prosthesis for displaced subcapital fractures; and intramedullary nailing for pertrochanteric and subtrochanteric fractures. Spinal anaesthesia was used in all patients receiving surgery. Antibiotic prophylaxis (cefazolin, 2g preoperative and 3 administrations of 1g IV every 8h postoperatively; for allergic patients, vancomycin 1g IV pre- and a single administration of 1g postoperatively) and antithrombotic prophylaxis (enoxaparin 40U sc every 24h for 1 month postoperatively) were identical in all cases. Postoperative laboratory analyses were requested 24h after the surgery. Seated position in an armchair was authorised for the patients at 24–48h, and walking with a walker after that. When the general patient state returned to normal following treatment and was considered apt for continuing with appropriate care at home or in a geriatric residence, the patient was discharged. Surgical and medical complications were registered during hospital admission.
Statistical analysisStatistical analysis was performed using the SPSS computer program, version 18.0 (SPSS Inc., Chicago, USA). To determine if the data fit normal distribution, the Kolmogorov–Smirnov test was used. Quantitative variables were presented with means and standard deviation (SD), and qualitative with percentages. Comorbidities were adjusted as dichotomous variables, with presence or absence of comorbidity. Age was divided into 2 groups: ≤89 years, and ≥90 years. Fracture type was classified as intracapsular (subcapital fracture) or extracapsular (pertrochanteric and subtrochanteric fractures). The number of comorbidities was grouped into ≥2 and <2. The Charlson Comorbidity Index (CCI) was divided into ≥2 and <2, with age-adjusted CCI split into groups ≥6 and <6. Haemoglobin upon admittance was classified as ≤10g/dl and >10g/dl, and surgical delay was divided into groups of >2 days and ≤2 days since hospital admission. Univariate analysis was performed between the variables registered and the in-hospital mortality. For qualitative variables, we used the chi square test with Yates correction depending on whether nonparametric Mantel–Haenszel procedure was applicable or not. For continuous variables, we used independent or paired Student t-test based on whether nonparametric Mann–Whitney or Wilcoxon signs was appropriate. The results were adjusted by age and sex, and the odds ratio was calculated with 95% confidence interval (CI). Significance was set to a value of P equal to or less than 0.05.
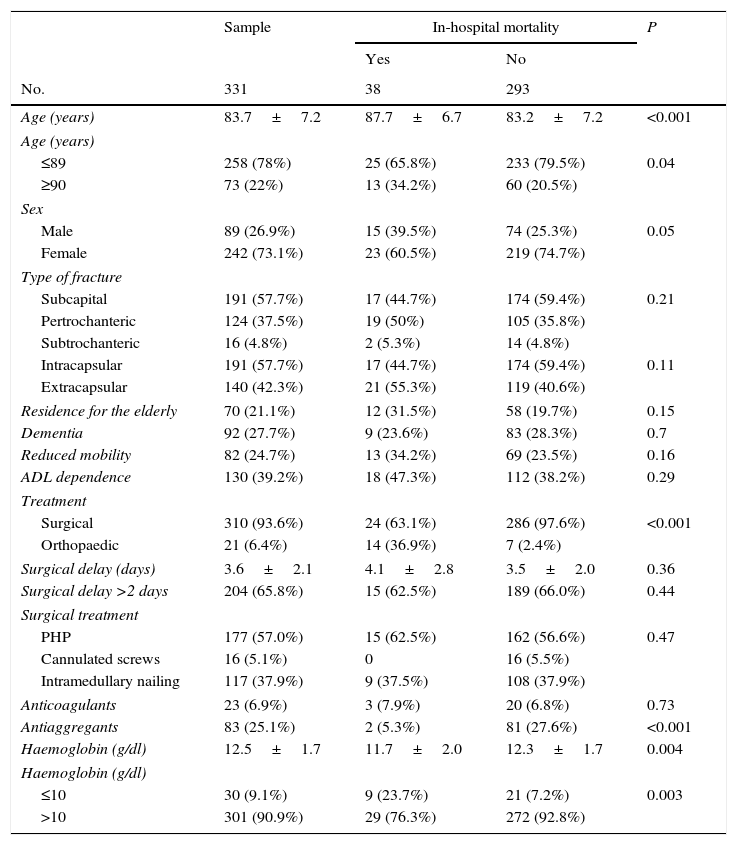
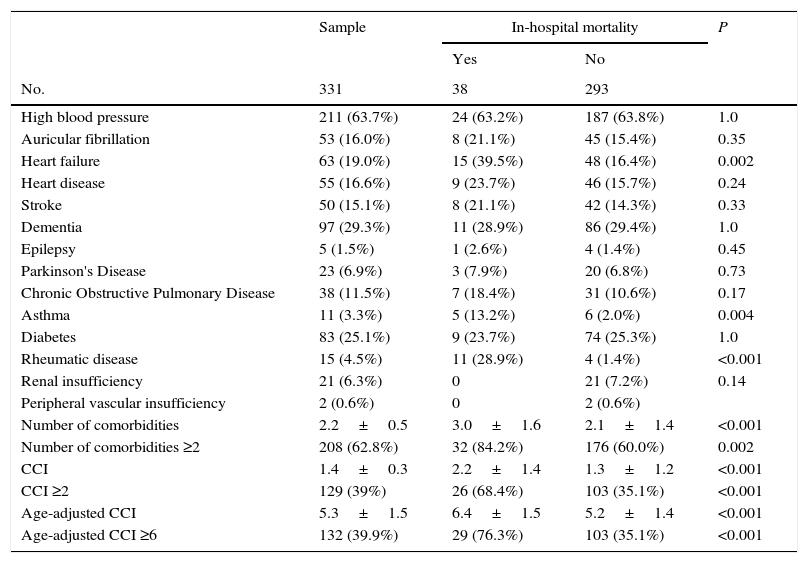
ResultsDuring the study period, 331 patients older than 65 years old with hip fracture, who fulfilled the criteria for inclusion, were admitted to our service. No losses were registered during the study period. Mean age of the patients was 83.7 years, with a higher percentage of patients below 85 years old (51.7%). Divided by sex, there were 242 women (73.1%). The most frequent type of fracture was the subcapital femur fracture, in 191 patients (57.7%). The most frequent comorbidities were high blood pressure, dementia and diabetes. In 208 patients (62.8%), comorbidities were ≥2. Fracture treatment was surgical in 310 patients (93.1%), with a mean delay of 3.6 days. Surgery was performed in the first 48h after hospital admission in 106 patients (34.1%). There was no statistically significant relationship between surgical delay and the fact that comorbidities were ≥2 (P=0.17). During their hospital stay, 79 patients (23.8%) received blood transfusions, with a median of 2 units of packed cells. Analysing the variables haemoglobin at admission and packed cell transfusion revealed that, of the patients having Hb ≤10g/dl at admission, 23.3% required preoperative transfusion, 56.6% required both pre- and postoperative transfusion, and 20.1% postoperative transfusion only (Tables 1 and 2). In 139 patients (41.9%), there were 1 or more complications during hospitalisation: respiratory in 49 patients (14.8%): pneumonia in 32 and bronchitis in 17; renal in 38 (11.4%): urinary infection in 29 and renal insufficiency in 9; cardiac in 26 (7.8%): heart failure in 17, heart arrhythmia in 6 and heart attack in 3; gastrointestinal in 12 (3.8%): paralytic ileus in 7, intestinal ischaemia in 3 and gastric ulcer in 2; deep vein thrombosis in 6 (1.8%); stroke in 5 (1.6%); pulmonary thromboembolism in 4 (1.2%); superficial infection in 3 (0.9%); and deep infection in 1 (0.3%). Surgical delay was longer in the patients that presented complications during hospital admission (P=0.04).
General variables and in-hospital mortality.
| Sample | In-hospital mortality | P | ||
|---|---|---|---|---|
| Yes | No | |||
| No. | 331 | 38 | 293 | |
| Age (years) | 83.7±7.2 | 87.7±6.7 | 83.2±7.2 | <0.001 |
| Age (years) | ||||
| ≤89 | 258 (78%) | 25 (65.8%) | 233 (79.5%) | 0.04 |
| ≥90 | 73 (22%) | 13 (34.2%) | 60 (20.5%) | |
| Sex | ||||
| Male | 89 (26.9%) | 15 (39.5%) | 74 (25.3%) | 0.05 |
| Female | 242 (73.1%) | 23 (60.5%) | 219 (74.7%) | |
| Type of fracture | ||||
| Subcapital | 191 (57.7%) | 17 (44.7%) | 174 (59.4%) | 0.21 |
| Pertrochanteric | 124 (37.5%) | 19 (50%) | 105 (35.8%) | |
| Subtrochanteric | 16 (4.8%) | 2 (5.3%) | 14 (4.8%) | |
| Intracapsular | 191 (57.7%) | 17 (44.7%) | 174 (59.4%) | 0.11 |
| Extracapsular | 140 (42.3%) | 21 (55.3%) | 119 (40.6%) | |
| Residence for the elderly | 70 (21.1%) | 12 (31.5%) | 58 (19.7%) | 0.15 |
| Dementia | 92 (27.7%) | 9 (23.6%) | 83 (28.3%) | 0.7 |
| Reduced mobility | 82 (24.7%) | 13 (34.2%) | 69 (23.5%) | 0.16 |
| ADL dependence | 130 (39.2%) | 18 (47.3%) | 112 (38.2%) | 0.29 |
| Treatment | ||||
| Surgical | 310 (93.6%) | 24 (63.1%) | 286 (97.6%) | <0.001 |
| Orthopaedic | 21 (6.4%) | 14 (36.9%) | 7 (2.4%) | |
| Surgical delay (days) | 3.6±2.1 | 4.1±2.8 | 3.5±2.0 | 0.36 |
| Surgical delay >2 days | 204 (65.8%) | 15 (62.5%) | 189 (66.0%) | 0.44 |
| Surgical treatment | ||||
| PHP | 177 (57.0%) | 15 (62.5%) | 162 (56.6%) | 0.47 |
| Cannulated screws | 16 (5.1%) | 0 | 16 (5.5%) | |
| Intramedullary nailing | 117 (37.9%) | 9 (37.5%) | 108 (37.9%) | |
| Anticoagulants | 23 (6.9%) | 3 (7.9%) | 20 (6.8%) | 0.73 |
| Antiaggregants | 83 (25.1%) | 2 (5.3%) | 81 (27.6%) | <0.001 |
| Haemoglobin (g/dl) | 12.5±1.7 | 11.7±2.0 | 12.3±1.7 | 0.004 |
| Haemoglobin (g/dl) | ||||
| ≤10 | 30 (9.1%) | 9 (23.7%) | 21 (7.2%) | 0.003 |
| >10 | 301 (90.9%) | 29 (76.3%) | 272 (92.8%) | |
Quantitative variables are shown as mean±standard deviation.
ADL: activities of daily living; PHP: partial hip prosthesis.
Comorbidities and in-hospital mortality.
| Sample | In-hospital mortality | P | ||
|---|---|---|---|---|
| Yes | No | |||
| No. | 331 | 38 | 293 | |
| High blood pressure | 211 (63.7%) | 24 (63.2%) | 187 (63.8%) | 1.0 |
| Auricular fibrillation | 53 (16.0%) | 8 (21.1%) | 45 (15.4%) | 0.35 |
| Heart failure | 63 (19.0%) | 15 (39.5%) | 48 (16.4%) | 0.002 |
| Heart disease | 55 (16.6%) | 9 (23.7%) | 46 (15.7%) | 0.24 |
| Stroke | 50 (15.1%) | 8 (21.1%) | 42 (14.3%) | 0.33 |
| Dementia | 97 (29.3%) | 11 (28.9%) | 86 (29.4%) | 1.0 |
| Epilepsy | 5 (1.5%) | 1 (2.6%) | 4 (1.4%) | 0.45 |
| Parkinson's Disease | 23 (6.9%) | 3 (7.9%) | 20 (6.8%) | 0.73 |
| Chronic Obstructive Pulmonary Disease | 38 (11.5%) | 7 (18.4%) | 31 (10.6%) | 0.17 |
| Asthma | 11 (3.3%) | 5 (13.2%) | 6 (2.0%) | 0.004 |
| Diabetes | 83 (25.1%) | 9 (23.7%) | 74 (25.3%) | 1.0 |
| Rheumatic disease | 15 (4.5%) | 11 (28.9%) | 4 (1.4%) | <0.001 |
| Renal insufficiency | 21 (6.3%) | 0 | 21 (7.2%) | 0.14 |
| Peripheral vascular insufficiency | 2 (0.6%) | 0 | 2 (0.6%) | |
| Number of comorbidities | 2.2±0.5 | 3.0±1.6 | 2.1±1.4 | <0.001 |
| Number of comorbidities ≥2 | 208 (62.8%) | 32 (84.2%) | 176 (60.0%) | 0.002 |
| CCI | 1.4±0.3 | 2.2±1.4 | 1.3±1.2 | <0.001 |
| CCI ≥2 | 129 (39%) | 26 (68.4%) | 103 (35.1%) | <0.001 |
| Age-adjusted CCI | 5.3±1.5 | 6.4±1.5 | 5.2±1.4 | <0.001 |
| Age-adjusted CCI ≥6 | 132 (39.9%) | 29 (76.3%) | 103 (35.1%) | <0.001 |
Quantitative variables are shown as mean±standard deviation.
CCI: Charlson Comorbidity Index.
Thirty-eight patients died in the hospital, representing an in-hospital mortality rate of 11.4%. Mean age of the patients that died was 87.7 years; by sex, there were 15 females (60.5%). The most common fracture type was pertrochanteric hip fracture, in 19 patients (50%). The predominant comorbidities were high blood pressure, heart failure, dementia and rheumatic disease. In 32 patients (84.2%), comorbidities were ≥2. Fracture treatment was surgical in 24 patients (63.1%), with a mean delay of 4.1 days. Surgery was performed in the first 48h following hospital admission in 9 patients (37.5%). Blood transfusion was necessary in 22 patients (57.8%), with a median of 4 units of packed cells (Tables 1 and 2). Complications arose in 25 patients (65.7%): pneumonia in 8, pulmonary thromboembolism in 4, stroke in 3, heart attack in 3, intestinal ischaemia in 3, acute renal failure in 2, acute hepatic failure in 1, and septic shock in 1. There was no statistically significant association between presenting a complication and in-hospital mortality (P=0.42). The mode from admission to patient death was 8 days, and the mean value was 12.1 days (range, from 4 to 28).
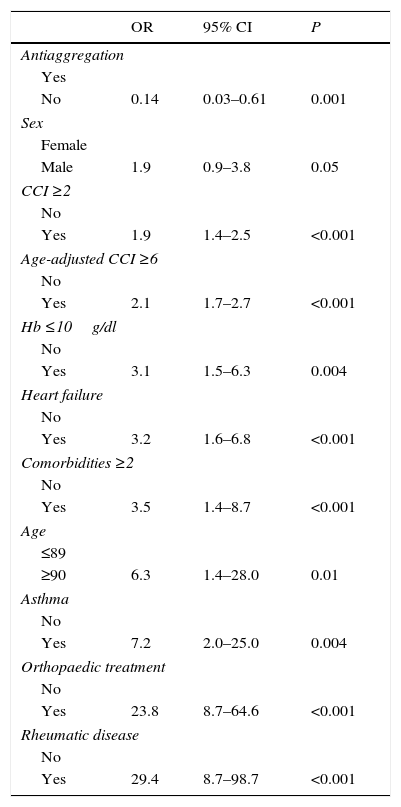
Univariate analysis of both groups revealed significant differences in mean age, age in groups, sex, fracture treatment, mean haemoglobin value, haemoglobin value ≤10g/dl, antiaggregation, the presence of heart failure, asthma and rheumatic disease, the mean number of comorbidities, number of comorbidities ≥2, the Charlson Comorbidity Index (CCI) ≥2, the age-adjusted CCI, and an age-adjusted CCI ≥6 (Tables 1–3).
Relative risk of variables associated with in-hospital mortality.
| OR | 95% CI | P | |
|---|---|---|---|
| Antiaggregation | |||
| Yes | |||
| No | 0.14 | 0.03–0.61 | 0.001 |
| Sex | |||
| Female | |||
| Male | 1.9 | 0.9–3.8 | 0.05 |
| CCI ≥2 | |||
| No | |||
| Yes | 1.9 | 1.4–2.5 | <0.001 |
| Age-adjusted CCI ≥6 | |||
| No | |||
| Yes | 2.1 | 1.7–2.7 | <0.001 |
| Hb ≤10g/dl | |||
| No | |||
| Yes | 3.1 | 1.5–6.3 | 0.004 |
| Heart failure | |||
| No | |||
| Yes | 3.2 | 1.6–6.8 | <0.001 |
| Comorbidities ≥2 | |||
| No | |||
| Yes | 3.5 | 1.4–8.7 | <0.001 |
| Age | |||
| ≤89 | |||
| ≥90 | 6.3 | 1.4–28.0 | 0.01 |
| Asthma | |||
| No | |||
| Yes | 7.2 | 2.0–25.0 | 0.004 |
| Orthopaedic treatment | |||
| No | |||
| Yes | 23.8 | 8.7–64.6 | <0.001 |
| Rheumatic disease | |||
| No | |||
| Yes | 29.4 | 8.7–98.7 | <0.001 |
CCI: Charlson Comorbidity Index; CI: confidence interval; OR: odds ratio.
In-hospital mortality after hip fracture in our hospital was 11.4% in the period from 2011 to 2014. This in-hospital mortality rate is greater than that indicated in studies published in the last 5 years. Belmont14 reported 4.5% in 9286 proximal femur fractures; Frost,15 6% in 1504; Alzahrani,16 5% in 2178; Chatterton,17 6.5% in 4426; Johansen,25 5.2% in 1050; and Tarrant,26 4.6% in 437. In Spain, in-hospital hip fracture mortality is around 5%.27 Sánchez-Hernández28 found 5.1% in 216 hip fractures treated with conventional measures, which fell to 2.8% after the application of a clinical pathway. And Mesa-Lampré29 reported 6.9% in 494 fractures treated in an orthogeriatric unit.
The study findings confirm the hypothesis that the factors related to the patient upon hospital admission (advanced age, male sex, non-administration of antiaggregant drugs and comorbidities) are associated with in-hospital mortality in hip fracture in the patient aged more than 65 years.
Advanced age and male sex are related in the literature to in-hospital mortality. Belmont14 indicated an odds ratio (OR) of 2.3 in the males. Frost15 found an OR of 8.7 in patients aged ≥90 years and of 2.4 in males. Chatterton17 published an OR of 4.1 times [stet] in patients aged ≥91 years and of 2.0 in males. In our series, a patient aged ≥90 years had an odds ratio of 6.3; and a male patient, of 2.6.
With respect to fracture type, Chatterton17 indicated an association between the intracapsular fracture and in-hospital mortality, with an OR of 1.4. In our series, we did not find this relationship upon differentiating fracture type or grouping the fractures into intracapsular and extracapsular, as other studies have reported.16
Mental state did not show any significant relationship with in-hospital mortality in our study. This contrast with the findings of Frost,15 in which 24% cognitive deterioration was found in the patients that died in the hospital, as against 14% in those that did not.
The presence of comorbidities at admission is strongly associated with in-hospital mortality. However, the results of the various studies have been dissimilar as to which comorbidities have the strongest influence. Belmont14 reported that dialysis was the best predictor of in-hospital mortality, with an OR >6. Frost15 indicated that having the number of comorbidities be equal to or greater than 1 was associated with an OR of 2.3 for in-hospital mortality. Chatterton17 reported that the greater the number of comorbidities, the greater the risk of in-hospital mortality. And Neuhaus18 found an association between greater CCI value and age-adjusted CCI value with in-hospital mortality. In our study, heart failure, rheumatic disease, lung tumour, comorbidities ≥2, CCI >2 and age-adjusted CCI >6 were significantly associated with in-hospital mortality.
Alzahrani16 described a greater risk of in-hospital mortality in the patients that lived in residencies for the elderly and with a lower level of independence, with respect to the patients that were totally independent at the time of the fracture. We did not find this in our study.
Published research indicates greater mortality in patients with hip fracture treated orthopaedically.30,31 Gregory32 finds 34% of mortality at 1 month from the fracture in 22 patients with displaced subcapital femur fracture with treatment orthopaedic for anaesthesia contraindication, compared to 4% in the patients treated surgically. In our series, in-hospital mortality in the patients with contraindication for surgical treatment was 66%, against 7.7% in the patients treated surgically.
The association between surgical delay and mortality is disputed. Some studies establish a relationship between a surgical delay of more than 2 days and mortality.13,33–35 However, others do not report this association.3,36,37 With respect to in-hospital mortality, Chatterton17 indicates greater in-hospital mortality in patients with a delay of more than 2 days, although without statistical significance. Belmont14 does not find this association either, although there are more complications in patients with greater surgical delay. In our study, the surgical delay was similar in both groups, but the patients with greater delay showed a greater incidence of complications.
ConclusionPatients that are males, with age more than 90 years, Hb <10g/dl, non-antiaggregants, having heart failure, asthma, rheumatic disease, pulmonary tumour and orthopaedic treatment present greater risk of in-hospital mortality. Given that these factors are not modifiable, we recommend the development of action protocols that would make it possible to reduce in-hospital mortality in this group of patients.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been carried out on human beings or animals for the purpose of this research.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre about the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Sanz-Reig J, Salvador Marín J, Pérez Alba JM, Ferrández Martínez J, Orozco Beltrán D, Martínez López JF. Factores de riesgo de mortalidad intrahospitalaria en la fractura proximal de fémur. Rev Esp Cir Ortop Traumatol. 2017;61:209–215.