Tibial plateau fractures are injuries prone to postoperative infection, with its reported incidence being higher than that of other fractures, between 5% and 12%. The primary objectives of this study were to quantify the postoperative infection rate of internal fixation of tibial plateau fractures (TPFs) and to identify the risk factors for this.
Material and methodsRetrospective cohort study including patients who underwent TPF osteosynthesis between 2015 and 2020, in the same center. The study population was divided into two groups, according to the presence or absence of postoperative infection. Demographic variables related to the fracture, surgical parameters, as well as the need for reoperation were collected. Finally, in the case of debridement, the number of positive cultures and the pathogen responsible for the infection were collected, as well as the treatment applied.
ResultsOne hundred and twenty-four patients were included, with a total of 14 infections (global infection rate of 11.3%). Risk factors for developing infection were open fractures (p=.002), Schatzker V and VI type fractures (p=.002) and the use of external fixation (p<.001). Regarding the surgical variables, only the longest ischemia time (p=.032) was identified as a risk factor. Staphylococcus aureus was the most frequently identified microorganism (43%), followed by Enterobacter cloacae (35.7%).
ConclusionThe overall infection rate after osteosynthesis of tibial plateau fractures was 11.3%. Different factors are associated with a higher risk of infection, including diabetes mellitus, open fractures, the use of external fixation, a higher grade in the Schatzker classification or a longer intraoperative ischemia time.
Las fracturas de meseta tibial (FMT) son lesiones propensas a infecciones postoperatorias, siendo la incidencia descrita superior a la del resto de fracturas, entre un 5 y un 12%. Los objetivos primarios de este estudio fueron cuantificar la tasa de infección postoperatoria de osteosíntesis de las FMT e identificar los factores de riesgo de esta.
Material y métodosEstudio de cohorte retrospectiva incluyendo a pacientes intervenidos de osteosíntesis de FMT entre los años 2015 y 2020, en un mismo centro. La población del estudio se dividió en 2 grupos, según la presencia o no de infección postoperatoria. Se recogieron las variables demográficas relacionadas con la fractura, los parámetros quirúrgicos, así como la necesidad de reintervención. Finalmente, en caso de desbridamiento, se recogieron el número de cultivos positivos y patógeno responsable de la infección, así como el tratamiento aplicado.
ResultadosSe incluyeron un total de 124 pacientes, con un total de 14 infecciones (tasa global de infección del 11,3%). Se identificaron como factores de riesgo para desarrollar infección el hecho de tratarse de fracturas abiertas (p=0,002), fracturas tipo Schatzker V y VI (p=0,002) y el uso de fijador externo (p<0,001). En lo que respecta a las variables quirúrgicas solo se identificó el mayor tiempo de isquemia (p=0,032) como factor de riesgo. S. aureus fue el microorganismo más frecuentemente identificado (43%), seguido de E. cloacae (35,7%).
ConclusiónLa tasa global de infección tras osteosíntesis de fractura de meseta tibial fue del 11,3%. Diferentes factores se asocian a más riesgo de infección, entre ellos la diabetes mellitus, las fracturas abiertas, el uso de fijador externo, un mayor grado en la clasificación de Schatzker o un mayor tiempo de isquemia intraoperatoria.
Tibial plateau fractures (TPFs) are one of the most serious injuries in the lower extremity with an incidence of 1% of all fractures. These types of injuries are particularly prone to postoperative infections, with reported infection rates of up to 80% of cases in historical records.1 With the use of minimally invasive techniques and more careful soft tissue management, considerably lower infection rates of between 5% and 12% have recently been reported.2
Despite the decrease in postoperative infection rates, the incidence described in the literature remains considerable, described between 1% and 2% in closed fractures and 30% in open fractures.3 To this end, the fact that they are normally high-energy fractures, with greater involvement of soft tissues and requiring greater dissection and surgical times for treatment, contributes to this. Bachoura et al. identified proximal tibia fractures as an independent risk factor for developing postsurgical infection, with an odds ratio (OR) of 2.3.4
Although different variables have been described that may contribute to the development of a postoperative infection in TPF, such as tobacco, diabetes, open fracture, prolonged surgical time or associated compartment syndrome, the literature remains diverse in terms of defining risk factors for this complication, which is associated with a loss of functionality, unsatisfactory results and an increase in hospital costs.5 Therefore, it is important to identify modifiable variables during the perioperative period that allow reducing infection rates and, thereby, reducing associated morbidity.
The primary objectives of this study were: (1) to quantify the rate of postoperative infection in a large series of TPFs operated on in a single center and (2) to identify the risk factors for postoperative infection in patients undergoing osteosynthesis of tibial plateau fracture.
Material and methodsA retrospective cohort study was designed that included patients undergoing TPF osteosynthesis in a single hospital center, from January 2015 to December 2020. Approval from the ethics committee of our institution was obtained prior to the start of the study and the informed consent to all patients to participate in it.
All fractures were evaluated prior to surgery using anteroposterior and lateral radiographs, as well as computed tomography, to accurately analyze the fracture pattern and were subsequently classified according to the Schatzker classification. In case of soft tissue suffering, associated dislocation or injuries with greater involvement of surrounding tissues, an external fixator was applied prior to osteosynthesis, delaying the definitive synthesis until the patient's condition improved. The definitive osteosynthesis of all fractures was performed by surgeons from the knee unit.
The inclusion criteria for this study were: TPF, aged 18 years or older, and complete postoperative follow-up data. The exclusion criteria were fractures treated conservatively or minimum follow-up of less than 12 months.
The study population was divided into two groups, depending on the development (group 1) or not (group 2) of infection during postoperative follow-up. The presence of infection was defined according to the ‘fracture-related infection’ (FRI) criteria of the European Bone and Joint Infection Society (EBJIS) and the FRI consensus group.6,7
According to these criteria, the presence of infection was clinically confirmed if there was a fistulous tract, if the implant was observed or if there was persistent purulent drainage from the wound or fracture site. Furthermore, in case of debridement, the presence of infection was confirmed if any of the following were true: (1) the presence of any phenotypically indistinguishable pathogen identified by culture of at least two different deep tissue samples; (2) the presence of microorganisms in deep tissue samples after histopathological examination and (3) >5 PMN in the sample of this tissue, confirmed by histopathological examination. Therefore, in all reinterventions, at least five peri-implant tissue samples were taken and sent for microbiological study, one tissue sample was sent for histopathological examination, and sonication was performed on the extracted implants.
Demographic variables such as age, sex, body mass index, active smoker, corticosteroid use and diabetes were collected, as well as variables related to the fracture such as Schatzker classification, open fracture and use of external fixator. Within the surgical parameters, the time from trauma to definitive osteosynthesis, surgical time, ischemia time, use or not of arthroscopy during the procedure, use of graft, and associated procedures were recorded. The need for reintervention during follow-up was also assessed, recording the procedure performed and the time from osteosynthesis to said procedure. Finally, for the assessment of postoperative infection, data related to the wound (dehiscence, purulent drainage and signs of skin infection) were collected and, in case of need for debridement, the number of positive cultures and the pathogen responsible for said infection were collected, as well as the treatment applied.
Statistical analysisThe quantitative variables were described through the median and the first and third quartiles. The qualitative variables were described using a frequency table (number and percentage). The bivariate analyses and for continuous variables, the assumption of normality was tested using the Shapiro–Wilk test. As most of these variables did not comply with the normal distribution, the Mann–Whitney U was used for continuous variables.
In the bivariate analyses for categorical variables, comparisons were evaluated through the Chi-square or Fisher's exact test, as appropriate. Statistical analyses were performed using STATA 15.1 software. The results were considered statistically significant with the value of p<.05.
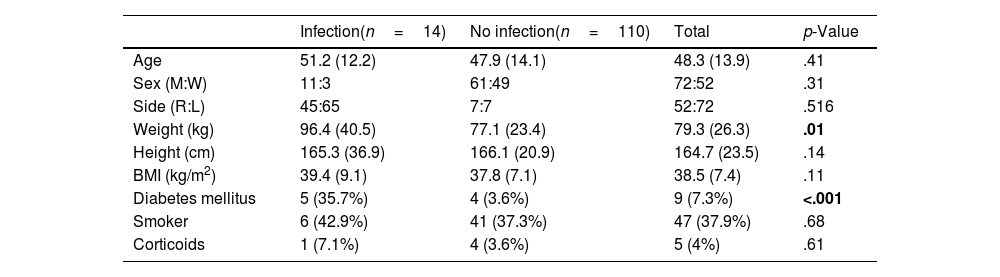
ResultsA total of 124 patients were included, 72 (58.1%) men and 52 (41.9%) women, with a mean age of 48.3 years (SD: 13.93). A total of 14 infections were obtained, corresponding to an overall infection rate of 11.3%. Table 1 shows the comparative analysis of demographic variables between both groups.
Demographic variables and their relationship with the infection rate.
| Infection(n=14) | No infection(n=110) | Total | p-Value | |
|---|---|---|---|---|
| Age | 51.2 (12.2) | 47.9 (14.1) | 48.3 (13.9) | .41 |
| Sex (M:W) | 11:3 | 61:49 | 72:52 | .31 |
| Side (R:L) | 45:65 | 7:7 | 52:72 | .516 |
| Weight (kg) | 96.4 (40.5) | 77.1 (23.4) | 79.3 (26.3) | .01 |
| Height (cm) | 165.3 (36.9) | 166.1 (20.9) | 164.7 (23.5) | .14 |
| BMI (kg/m2) | 39.4 (9.1) | 37.8 (7.1) | 38.5 (7.4) | .11 |
| Diabetes mellitus | 5 (35.7%) | 4 (3.6%) | 9 (7.3%) | <.001 |
| Smoker | 6 (42.9%) | 41 (37.3%) | 47 (37.9%) | .68 |
| Corticoids | 1 (7.1%) | 4 (3.6%) | 5 (4%) | .61 |
R: right; M: man, L: left; BMI: body mass index; W: woman.
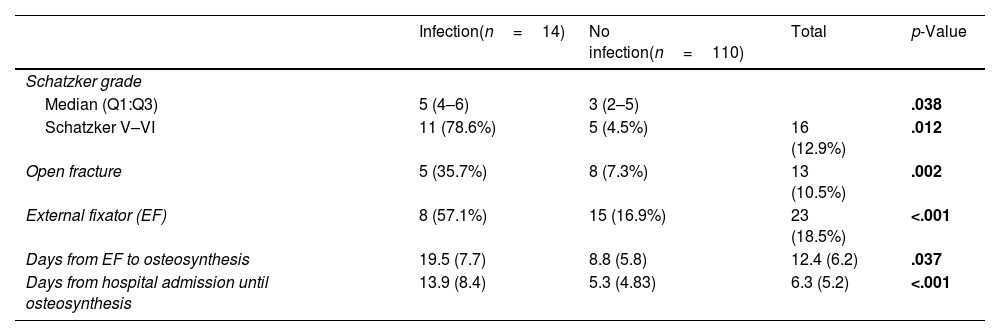
Regarding the type of fracture, it was observed that if it was an open fracture this constituted a risk factor for developing infection since of the 13 (10.5%) open fractures treated, 5 were included in the first group (p=.002). The highest energy fractures, Schatzker V and VI, were also revealed to be associated with a higher risk of developing infection (p=.002). This can also be verified given that the use of external fixator was also associated with a higher risk of developing infection (p<.001). In Table 2 it can be seen that different factors associated with the type of fracture can be associated with a higher risk of infection.
Fractures with a higher Schatzker classification can be observed, open fractures or those that require the use of an external fixator, and are associated with a higher infection rate.
| Infection(n=14) | No infection(n=110) | Total | p-Value | |
|---|---|---|---|---|
| Schatzker grade | ||||
| Median (Q1:Q3) | 5 (4–6) | 3 (2–5) | .038 | |
| Schatzker V–VI | 11 (78.6%) | 5 (4.5%) | 16 (12.9%) | .012 |
| Open fracture | 5 (35.7%) | 8 (7.3%) | 13 (10.5%) | .002 |
| External fixator (EF) | 8 (57.1%) | 15 (16.9%) | 23 (18.5%) | <.001 |
| Days from EF to osteosynthesis | 19.5 (7.7) | 8.8 (5.8) | 12.4 (6.2) | .037 |
| Days from hospital admission until osteosynthesis | 13.9 (8.4) | 5.3 (4.83) | 6.3 (5.2) | <.001 |
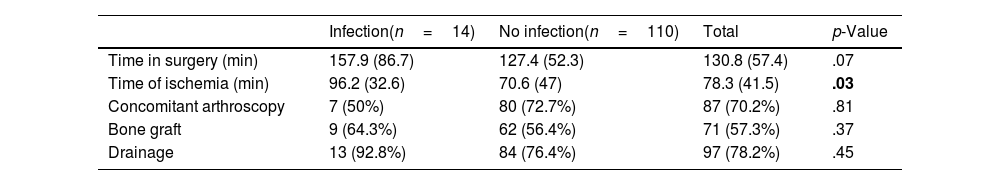
Regarding the surgical variables, it was observed that a longer ischemia time was associated with higher rates of postsurgical infection with a mean of 96min in group 1 versus a mean of 70min in group 2 (p=.032). Regarding the total surgery time, a similar trend was observed of 158 versus 127min, respectively, although without reaching statistical significance (p=.07). In Table 3, it can also be seen that the fact of associating arthroscopy or providing a bone graft does not contribute to higher infection rates.
Comparison of intraoperative variables in both groups.
| Infection(n=14) | No infection(n=110) | Total | p-Value | |
|---|---|---|---|---|
| Time in surgery (min) | 157.9 (86.7) | 127.4 (52.3) | 130.8 (57.4) | .07 |
| Time of ischemia (min) | 96.2 (32.6) | 70.6 (47) | 78.3 (41.5) | .03 |
| Concomitant arthroscopy | 7 (50%) | 80 (72.7%) | 87 (70.2%) | .81 |
| Bone graft | 9 (64.3%) | 62 (56.4%) | 71 (57.3%) | .37 |
| Drainage | 13 (92.8%) | 84 (76.4%) | 97 (78.2%) | .45 |
Finally, in 12 of the 14 infections observed there was clinical confirmation due to the presence of fistula, purulent drainage or exposure of material. In the remaining 2 cases, debridement was performed due to unsatisfactory wound evolution. Among these 14 cases, 2 were caused by polymicrobial infections. The most frequent microorganism was Staphylococcus aureus, in 6 (43%) of the cases, followed by Enterobacter cloacae in 5 (35.7%) cases. For the treatment of this infection, debridement with implant retention was performed in 10 cases and in the remaining 4 cases, material removal with rheosteosynthesis was performed.
DiscussionThe main finding of this study is that the overall infection rate after TPF osteosynthesis is 11.3%, a value comparable to that described in the literature. In a recent meta-analysis, Bullock et al.8 describe an infection rate of 9%, which contrasts with the 12.6% reported in the meta-analysis of the AGA-Society for Arthroscopy and Joint Surgery working group.9 The heterogeneity of reported infection rates is due to different factors. First, the definition of postoperative infection is not standardized, since certain authors differentiate between superficial surgical infection and deep surgical infection. In order to overcome this problem, the EBJIS defined criteria for infection related to fracture, which allow creating a standardized definition of post-osteosynthesis infection and thus more homogeneously compare the different rates of this complication.10 Another cause of this heterogeneity is the different inclusion criteria and type of population of the different studies, which range from exclusively low-grade fractures (Schatzker I–III) to open fractures requiring an external fixator, as well as different types of surgical management that can condition different types of osteosynthesis and soft tissue care.1,11,12
Different variables are identified in this work as risk factors for developing an infection, including weight, diabetes mellitus (DM), a higher grade in the Schatzker classification, open fracture or the use of an external fixator. Intraoperative variables were also analyzed, where it was observed that a longer ischemia time constitutes a risk factor, while neither the use of arthroscopy during osteosynthesis nor the use of bone graft increased the risk of developing infection.
Among the demographic variables identified, weight and DM can be associated in the context of a metabolic syndrome, further increasing the risk of postoperative infection. Although DM is a well-defined risk factor for postsurgical infection not only for urgent procedures but also in scheduled procedures,13 its role as an independent risk factor in TPF remains controversial. Shao et al.14 did not identify DM or sex as a risk factor in the meta-analysis carried out on 2214 cases (with a global infection rate of 9.9%) while Momaya et al.5 did identify DM as a factor. Rodriguez-Buitrago et al.15 attempted to define a threshold value of blood glucose beyond which this risk increased without being able to attribute a defined value either in terms of maximum intraoperative value, fasting blood glucose or glycated hemoglobin (HbA1c). In fact, they end up concluding that, although this value has been defined as a fasting blood glucose greater than 140mg/dl in scheduled procedures, this is not a constant parameter for the risk of infection in TPF.
Open fractures or those that required the use of an external fixator were also identified as a risk factor for developing infection, as well as fractures with greater severity in the Schatzker classification (V–VI). This means that higher energy fractures, with greater soft tissue attrition and more associated injuries are at greater risk of developing infection, as expected. These findings are similar to those described in the literature, which describes that having an open fracture has an OR of 3.2–7.1 for the development of a postoperative infection.11,16 These types of patients also tend to be associated with a longer hospital stay and a greater number of debridements in order to maintain a correct state of healing of the surrounding soft tissues, which in itself entails a greater risk of infection.4 Regarding the use of an external fixator, this is usually applied in open injuries, dislocations or in those injuries with risk of soft tissue compromise in the hours following the trauma. In this study, among the 23 (18.5%) patients in whom an external fixator was applied, 8 developed a postoperative infection, which means that one in 3 patients in whom osteotaxis was initially applied developed this complication. These findings are similar to those previously published, in which the use of an external fixator had an OR of 3.8–5.4 for developing postoperative infection, a value that increased in the case of bicondylar fractures, with an OR of up to 11.2.16,17
Regarding intraoperative variables, a longer ischemia time was also associated with a higher risk of infection in this study. Also observed was that the mean total surgical time in the group that developed infection was higher than the mean time in the group that did not develop it (158 versus 127min, respectively). Colman et al. estimate that, for each additional hour of surgical time, the probability of developing infection increases by 78%.16 Li et al.18 also describe that surgical time is a risk factor for infection, with a mean of 195min in the group with infection versus 147min in the group without infection. It should be added that longer surgical times are usually associated with more complex fractures, with the need for greater soft tissue dissection and greater associated technical difficulty, which together could increase the probability of bacterial colonization and, with it, the development of an infection.
The use of arthroscopy associated with TPF osteosynthesis is an increasingly growing practice. It allows direct observation of the reduction at the intra-articular level, as well as the diagnosis of possible associated joint injuries. Its use in high-grade TPF remains a matter of discussion due to the risk of increased complications, including acute compartment syndrome. Different working groups have reported in recent years that its use is not associated with a greater number of complications, both in low-grade and high-grade fractures.19,20 Specifically, in these studies no case of compartment syndrome has been reported with the use of arthroscopy and the overall infection rate being comparable between groups.21 In our work group, the arthroscopic-assisted reduction strategy was used in the vast majority of both low-grade and high-grade TPF, without an increase in the number of complications. Within the study population, this strategy was used in 70% of cases, without an increase in the associated infection rate.
The most frequently isolated microorganism in the cases that developed infection was S. aureus, in 43% of cases, a rate very similar to the 47% described by Morris et al.11 Despite the different rates reported in the different studies, S. aureus was consistently the most frequent pathogen causing postoperative infections in TPF.5,9,22,23 Thus, taking this finding into account, the antibiotic prophylaxis instituted must pay special attention to this group of pathogens, especially in patients with added risk factors.
This study has limitations that require commenting upon. First, it is a retrospective study which means that, apart from the intrinsic limitations of this type of study, the recording of some variables was carried out through information in the clinical history, with an associated bias. It is also important to mention that the sample size and specifically the number of infections may be insufficient to detect differences in all the variables under study in a multivariate analysis. Furthermore, different variables that may also affect wound healing and, therefore, an increase in infection rates such as nutritional deficiencies or trauma severity scales (such as the Injury Severity Score) have not been collected. Finally, the surgical procedure for these fractures was performed by different surgeons, with different criteria and surgical management, which may also have conditioned a different approach to them, not only in terms of number and length of incisions but also of the osteosynthesis material performed, which can give heterogeneity to the included population.
In conclusion, there is a high infection rate after TPF osteosynthesis. Various risk factors are associated with an increase in this rate, including DM, open fractures, the use of an external fixator, a higher grade in the Schatzker classification or a longer intraoperative ischemia time. The provision of bone graft and the use of arthroscopy during osteosynthesis are not associated with a greater risk of postoperative infection.
Level of evidenceLevel of evidence III.
Ethical approvalThe study was carried out following the guidelines of the Declaration of Helsinki and was previously approved by the ethics committee of our institution.
Authors’ contributionsConception and design: AC, IP-A, RC, JFS-S, RT-C and AA.
Data collection: AC, IP-A and RC.
Data analysis: AC, IP-A and RC.
Redaction: AC and IP-A.
Review and editing: JFS-S, RT-C, AA and JCM.
All authors read and approved the final version of the study.
FundingThis study did not receive any type of funding.
Conflict of interestsThe authors declare that they have no conflict of interest for this study.
Ethics Committee approvalCEIm 2019/8762/I.