To evaluate risk factors for dislocation after primary total hip arthroplasty (THA), and its functional outcomes.
Material and methodsA retrospective study was conducted on 22 cases with dislocation and 431 controls without dislocation, but all were performed with lateral access. The data were collected prospectively with a minimum follow-up of 5 years. Patient-related factors, from primary surgery, and position of components on simple radiographs were analyzed. Harris and Merle D’Aubigné hip scores, and short Womac questionnaire were used.
ResultsDemographic, patient-related or surgical technique factors were not risk predictors of dislocation. With regard to position of components, an acetabular abduction >50° (p=0.003) and anteversion lower or higher than 10°–20° (p=0.044) were risk factors. Controls and dislocation treated conservatively had similar outcomes, and in both were better than in those treated with surgical revision (p=0.03).
DiscussionFactors relating to the patient and soft tissues status may influence the stability of the arthroplasty, but malposition of the acetabular component seems to be the most important and common risk factor for dislocation.
Evaluar los factores de riesgo de luxación tras artroplastia total de cadera (ATC) primaria y su resultado funcional.
Material y métodosEstudio retrospectivo de 22 luxaciones comparadas a 431 ATC no luxadas, todas por vía lateral, cuyos datos habían sido recogidos prospectivamente con seguimiento mínimo de 5 años. Se evaluaron factores relacionados con el paciente, de la cirugía primaria y posición de componentes sobre radiografías simples. Se utilizaron las escalas de Harris y Merle D’Aubigné y el cuestionario Womac corto.
ResultadosNo fueron predictores de luxación los factores demográficos, estado del paciente o técnica quirúrgica. Respecto a la posición de componentes fueron factores de riesgo una abducción acetabular >50° (p=0,003) y anteversión fuera del rango de 10°-20° (p=0,044). Funcionalmente, los resultados fueron similares entre los controles y las luxaciones tratadas conservadoramente, y en ambos fueron superiores a las tratadas mediante revisión quirúrgica (p=0,03).
DiscusiónAun cuando los factores relacionados con el paciente y estado de las partes blandas pueden influir en la estabilidad de la ATC, la malposición del componente acetabular parece ser el más importante y frecuente factor de riesgo para la luxación.
Dislocation is a relatively frequent complication after total hip arthroplasty, with 2–5% of patients suffering a significant impact on morbidity and costs deriving from treatment.1 Around 45% of cases take place in the first 2 weeks following the intervention.2 Numerous risk factors have been reported,3,4 including demographic, related to the health status and general condition of patients, the approach route, implant design, size of the prosthetic head and position of the components. The latter is considered as a crucial factor, and although several measurements have been published as ideal position of the components, as well as safety ranges to avoid dislocation,5 these are difficult to achieve even by experienced surgeons.1 Moreover, the posterior route approach is considered to increase the risk of dislocation compared to the lateral route,6 although the risk associated with the posterior route can be reduced through adequate repair of the soft tissues.7,8 The intrinsic factors of each patient are difficult to assess in many cases.
One objective of this study was to identify potential risk factors for dislocation following uncemented primary total hip prosthesis implanted through the lateral route. The second objective was to compare the functional outcome following dislocation versus non-dislocated hips.
Materials and methodsThe study was approved by the Clinical Research Ethics Committee of our center. We identified 986 consecutive, uncemented, primary, total hip arthroplasties (THA) in 804 patients, performed between 2001 and 2007 by the 2 leading authors of the study and with a minimum follow-up period of 5 years. Of these, 22 THA had suffered dislocation and were the subjects of the study.
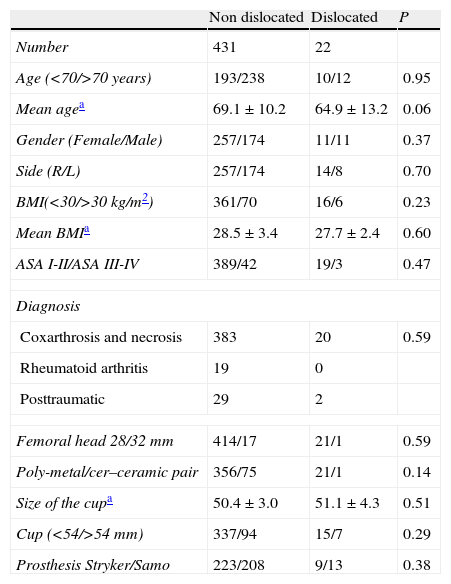
In terms of comparison, we selected consecutive THA implanted in the last 3 years of the studied range (2005–2007) applying the exclusion criteria of age under 20 years, diagnosis of sequelae of developmental dysplasia, need for surgical revision and not completing a minimum follow-up of 5 years. We excluded 21 patients, thus being left with a valid cohort of 431 THA without dislocation. No cases were excluded due to a lack of clinical or radiographic data in the database. The clinical and perioperative characteristics of both cohorts are presented in Table 1, which shows that there were no significant differences regarding demographic data or the prosthetic components employed.
Characteristics of both cohorts.
| Non dislocated | Dislocated | P | |
| Number | 431 | 22 | |
| Age (<70/>70 years) | 193/238 | 10/12 | 0.95 |
| Mean agea | 69.1±10.2 | 64.9±13.2 | 0.06 |
| Gender (Female/Male) | 257/174 | 11/11 | 0.37 |
| Side (R/L) | 257/174 | 14/8 | 0.70 |
| BMI(<30/>30kg/m2) | 361/70 | 16/6 | 0.23 |
| Mean BMIa | 28.5±3.4 | 27.7±2.4 | 0.60 |
| ASA I-II/ASA III-IV | 389/42 | 19/3 | 0.47 |
| Diagnosis | |||
| Coxarthrosis and necrosis | 383 | 20 | 0.59 |
| Rheumatoid arthritis | 19 | 0 | |
| Posttraumatic | 29 | 2 | |
| Femoral head 28/32mm | 414/17 | 21/1 | 0.59 |
| Poly-metal/cer–ceramic pair | 356/75 | 21/1 | 0.14 |
| Size of the cupa | 50.4±3.0 | 51.1±4.3 | 0.51 |
| Cup (<54/>54mm) | 337/94 | 15/7 | 0.29 |
| Prosthesis Stryker/Samo | 223/208 | 9/13 | 0.38 |
ASA: American Society of Anesthesiologists health score; BMI: body mass index; L: left; R: right.
All the surgical interventions were carried out in a laminar flow room and applying spinal anesthesia. The Hardinge lateral approach was used in all cases.9 The anterior capsule was sectioned and not repaired. During the closure we performed suture and reinsertion of the tendon of the gluteus medius muscle to the greater trochanter and closure of the fascia lata. We implanted 2 systems of uncemented THA according to their availability at the center. One was the Meridian stem system with Vitalock or Trident cup (Stryker, Mahwah, USA) in 232 cases (51.2%), and the other was the Duofit stem and cup system (Samo, Bologna, Italy) in 221 cases (48.8%). Both systems had similar geometries. The stems were straight and collarless, composed of a titanium alloy with a circumferential, porous, plasma-spray cover in the proximal third and pressure fit implantation following drilling of the femoral canal. All the cups were semispherical, made of a titanium alloy with porous, plasma-spray, cover and pressure fit implantation following drilling, and had orifices for additional stability with screws. In 93.3% of cases we used 2 divergent screws. The inserts were made of high molecular weight polyethylene sterilized with gamma radiation in air with an elevation of 12° in 377 cases (83.2%), and ceramic in 76 cases (16.8%). The diameter of the femoral head employed was of 28mm in 435 cases (96.0%) and of 32mm in 18 cases (4.0%). Metallic heads were used with polyethylene inserts and ceramic heads were used with ceramic inserts. All the patients received perioperative antibiotic prophylaxis with first generation cephalosporin for 24h, and thromboprophylaxis with low molecular weight heparin for 1 month after the intervention. The postoperative regime was similar in all cases, with rest after 24h and allowing partial load with walking frames after 48h if pain allowed it. No routine measures were used to restrict the mobility of the operated hip.
AssessmentsThe arthroplasty registry at our department contains clinical and radiographic data from all the patients treated with arthroplasty collected in a prospective manner, although used only retrospectively in this study. The assessments were standardized preoperatively and with postoperative follow-up at 3 and 6 months, 1 year and annually thereafter for a minimum of 5 years. The comorbidity was assessed using the scale of the American Society of Anesthesiology.10 The clinical assessment used the Harris11 and Merle D’Aubigné and Postel12 hip scales, and quality of life was assessed using the short Womac questionnaire validated for Spanish.13 The radiographs were obtained in standard AP projections of the pelvis and both hips when standing with 15° internal and axial rotation of the affected hip. We also obtained a CT scan following the closed reduction in all cases of dislocation.
We studied multiple potential risk factors for dislocation described in the literature,1 such as demographic, related to the patient3 including a score ≥3 in the American Society of Anesthesiology scale and BMI ≥30, surgical technique and radiographic position of the components.
The position of the components in non-dislocated cases was assessed following the methods for simple radiographs described by Pradhan14 and Widmer15 for the cup and Visser and Konnings16 for the stem. In all cases of dislocation they were measured on the CT scan obtained after the closed reduction.
Based on the literature4,5,17,18 and the experience of the surgeons, the position of the acetabular component was considered adequate at an abduction of 40°±10° and anteversion of 15°±5°, whilst values of abduction >50° and anteversion outside of the range 10°–20° were considered as a risk factor for dislocation. The stem should be in a neutral position and anteversion of 5°–10°, as uncemented stems with metaphyseal pressure fit did not allow greater anteversion. Given this constraint, we considered as the range of safety of combined anteversion, the sum of the acetabular and femoral anteversions, values outside of the range 15°-30°. We considered as inadequate an offset <10% with respect to the preoperative (insufficient reconstruction) and a positive Voss effect.
Statistical analysisThe statistical analysis was carried out using the software package SPSS v. 15.0 (SPSS Inc., Chicago, USA). We considered as statistically significant values of P≤.05. In order to determine the normal distribution we used the Kolmogorov–Smirnov test. First, we carried out univariate analysis, comparing each variable in both groups, using the categorical variables of the Chi squared test or the exact, non-parametric Fisher test and for continuous variables the Student's t or the Mann–Whitney test. When comparing more than 2 samples, we used the analysis of variance. Those variables which showed certain association in univariate tests were used as independent covariates in the logistic regression analysis for the presence of dislocation. The quantification of risk factors was assessed through the odds ratio with a 95% confidence interval. We used the Kaplan–Meier survival analysis to calculate cumulative risk of suffering at least 1 dislocation, comparing the survival curves of both cohorts through the log-rank analysis. The Cox multivariate analysis was used to assess the risk of dislocation over time, adjusting it to multiple variables, quantified through the hazard ratio with a 95% confidence interval.
ResultsThe mean follow-up time of patients with dislocation was 8.2 years (range: 5–11 years), whilst for controls it was 6.7 years (range: 5–8 years). The gross rate of incidence for at least 1 episode of dislocation, no bilateral patients, was of 2.2%. Chronologically, the first episode took place within the first 3 months after the intervention in 20 cases, and belatedly in the remaining 2 (22 and 46 months after the intervention). Using Kaplan–Meier analysis, the cumulative risk of suffering dislocation was of 4.2% at 3 months, 4.4% at 1 year and 4.9% at 5 years.
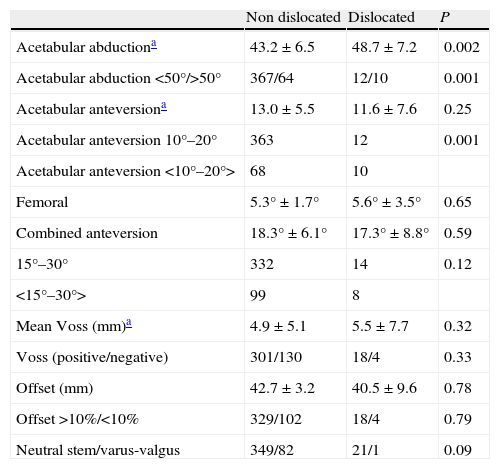
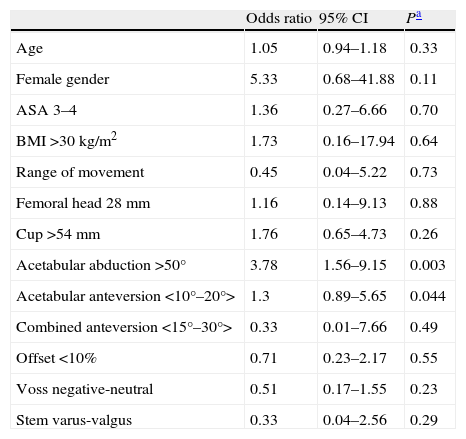
Risk factorsAs shown in Table 1, when the clinical, technical or THA model variables were analyzed individually, none of them was a potential predictor of dislocation (P>.05). Table 2 shows the radiographic position of the components in both cohorts, where only acetabular abduction >50° and acetabular anteversion outside of the range 10°–20° were potential predictors of dislocation in the univariate analysis (P=.001). When the influence of the variables was assessed jointly through multiple regression analysis (Table 3), both variables were also predictors of dislocation (P=.003 and P=.044, respectively).
Radiographic position of the components.
| Non dislocated | Dislocated | P | |
| Acetabular abductiona | 43.2±6.5 | 48.7±7.2 | 0.002 |
| Acetabular abduction <50°/>50° | 367/64 | 12/10 | 0.001 |
| Acetabular anteversiona | 13.0±5.5 | 11.6±7.6 | 0.25 |
| Acetabular anteversion 10°–20° | 363 | 12 | 0.001 |
| Acetabular anteversion <10°–20°> | 68 | 10 | |
| Femoral | 5.3°±1.7° | 5.6°±3.5° | 0.65 |
| Combined anteversion | 18.3°±6.1° | 17.3°±8.8° | 0.59 |
| 15°–30° | 332 | 14 | 0.12 |
| <15°–30°> | 99 | 8 | |
| Mean Voss (mm)a | 4.9±5.1 | 5.5±7.7 | 0.32 |
| Voss (positive/negative) | 301/130 | 18/4 | 0.33 |
| Offset (mm) | 42.7±3.2 | 40.5±9.6 | 0.78 |
| Offset >10%/<10% | 329/102 | 18/4 | 0.79 |
| Neutral stem/varus-valgus | 349/82 | 21/1 | 0.09 |
<>: outside of the range.
Factors predicting dislocation.
| Odds ratio | 95% CI | Pa | |
| Age | 1.05 | 0.94–1.18 | 0.33 |
| Female gender | 5.33 | 0.68–41.88 | 0.11 |
| ASA 3–4 | 1.36 | 0.27–6.66 | 0.70 |
| BMI >30kg/m2 | 1.73 | 0.16–17.94 | 0.64 |
| Range of movement | 0.45 | 0.04–5.22 | 0.73 |
| Femoral head 28mm | 1.16 | 0.14–9.13 | 0.88 |
| Cup >54mm | 1.76 | 0.65–4.73 | 0.26 |
| Acetabular abduction >50° | 3.78 | 1.56–9.15 | 0.003 |
| Acetabular anteversion <10°–20°> | 1.3 | 0.89–5.65 | 0.044 |
| Combined anteversion <15°–30°> | 0.33 | 0.01–7.66 | 0.49 |
| Offset <10% | 0.71 | 0.23–2.17 | 0.55 |
| Voss negative-neutral | 0.51 | 0.17–1.55 | 0.23 |
| Stem varus-valgus | 0.33 | 0.04–2.56 | 0.29 |
ASA: American Society of Anesthesiologists health score; BMI: body mass index.
<>: outside of the range.
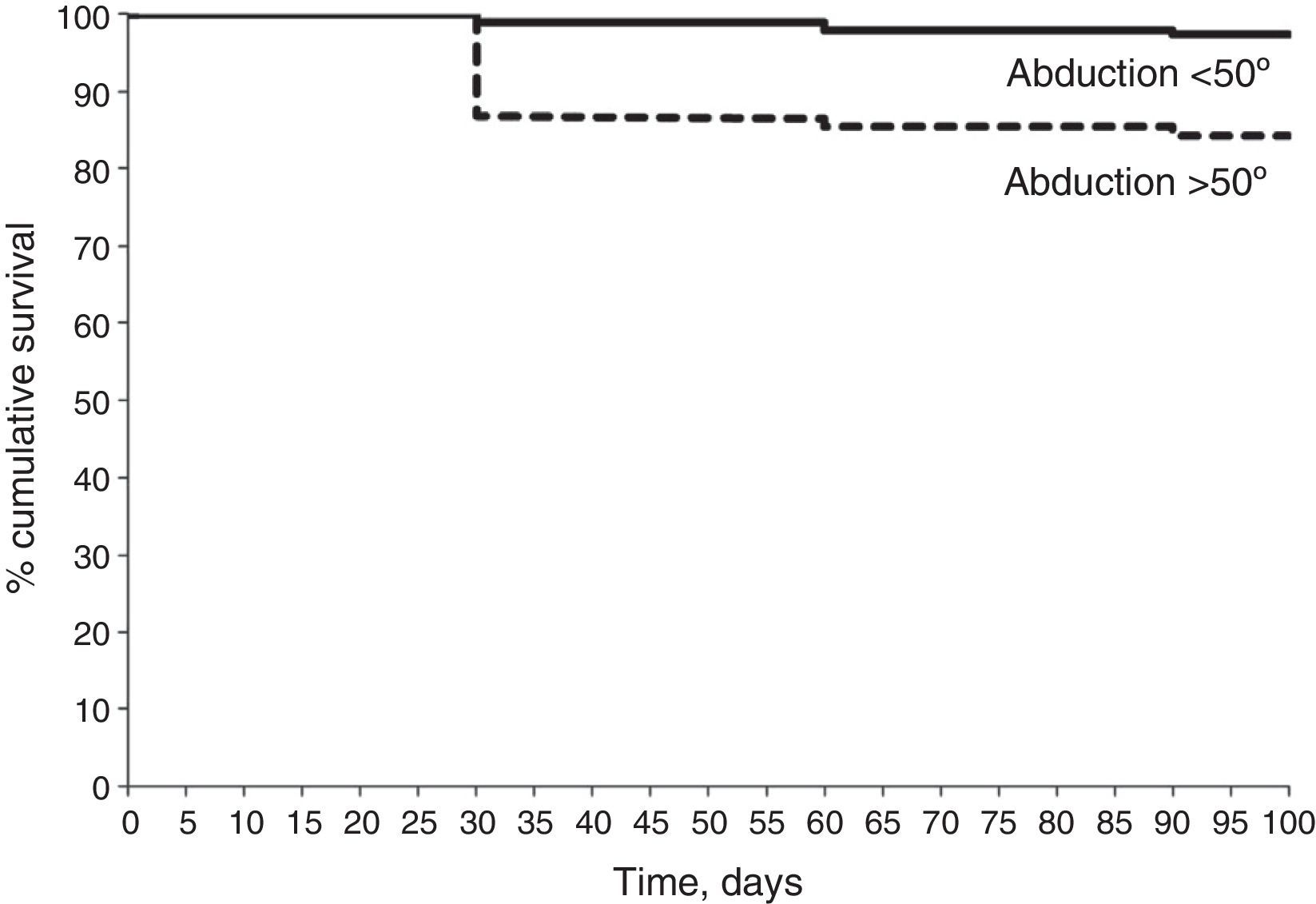
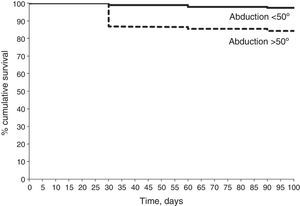
According to the Kaplan–Meier analysis (Fig. 1), cumulative survival at 3 months, considering dislocation as the final point, was 84.2% (95% CI: 76.7–92.1) in THA with acetabular abduction >50° and 97.3% (95% CI: 96.3–99.8) with abduction <50°. The log-rank analysis showed significant differences between both curves (P=.001). The Cox regression analysis revealed that, in the group of patients with dislocation, acetabular abduction >50° was an independent predictor of dislocation (P=.004), with a hazard ratio of 3.2 (95% CI: 1.9–8.4).
Functional resultsInitially, all the dislocated hips underwent emergency closed reduction under general anesthesia. Subsequently, the treatment for dislocation was determined according to the intraoperative stability of the prosthesis after reduction and to the position of the components. The criteria for intraoperative stability consisted of maneuvers of hip flexion over 90°, maximum extension with external rotation and adduction with external rotation.
One case presented displacement of the fracture of the greater trochanter, which went unnoticed initially, with no loosening of the components, treated by internal fixation and resulting stable and without complications until the end of the follow-up period. Another 12 cases were initially treated conservatively, with apparent stability after the closed reduction, with the acetabulum presenting a mean abduction value of 46.3° (range: 32°–52°) and anteversion of 18° (range: 16°–23°). Of these, 6 were stable until the end of the follow-up period and the other 6 suffered a second dislocation after a mean period of 30 days (range: 18–52 days), leading to replacement of the acetabulum, and resulting stable thereafter.
Another 4 cases presented intraoperative instability and evident malposition of some component. One case suffered collapse of the stem in dislocation, which was stable after replacement. Another case presented an acetabulum with 45° abduction and 20° anteversion and stem with 10° anteversion. The latter was changed to neutral anteversion and resulted stable. In the remaining 2 cases, with acetabulum abduction 58° and 66°, the components were replaced and resulted stable.
The remaining 5 cases presented instability after the initial closed reduction, but without evident component malposition. In 2 of them, both with polyethylene–metal pairs, stability was achieved after replacement of the insert with reorientation of the rim. In the remaining 3 cases, we considered soft part failure, but they did not present neuromuscular disease. In these 3 cases we carried out revisions of the acetabulum to another with a retentive insert and a 28mm head (Duofit IPR, Samo, Italy) and retensing of soft parts. Two of them suffered redislocations which were treated by replacement of the retentive cup. One of them resulted stable and the other suffered a third dislocation without dissociation of the retention ring, which was revised to a 48mm megahead on the original stem and replacement of the cup to a metal–metal pair (M2 Magnum, Biomet, USA), resulting stable.
In short, 6 patients with dislocation (27.3%) were treated successfully with conservative measures and the remaining 16 patients (72.7%) required surgical revision. The revision consisted in a replacement of the acetabulum in 11 patients, of the insert in 2 patients, the stem in 2 patients, and synthesis of the fracture of the greater trochanter in 1 patient.
In the cohort suffering dislocations there were no immediate complications in the cases which were not surgically revised, but 1 patient presented polyethylene usury and loosening of the acetabulum after 7 years of follow-up, requiring surgical revision. Among the revised cases there was 1 patient with paralysis of the external popliteal sciatic nerve, who recovered after 4 months. Another patient presented superficial infection which was resolved by surgical cleaning and antibiotic therapy. Another patient presented aseptic loosening of the stem 3 years after its replacement, and rejected a new surgical revision. Another 2 patients presented chronic infections after 1 and 3 years of replacing the acetabulum, requiring a new revision. The complications and survival of non-dislocated THA were not analyzed, as they were not part of the study.
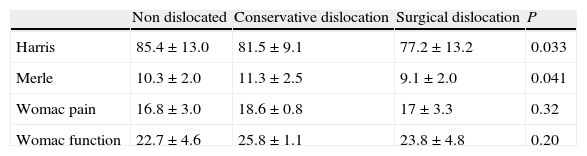
We compared both cohorts to assess whether the dislocation affected medium-term functional results. Likewise, in the cohort with dislocation we compared patients treated conservatively and those who required surgical revision. Table 4 contains the functional results of the last assessment conducted, showing that there were no significant differences between non-dislocated and dislocated cases which were treated conservatively regarding Harris (P=.06) and Merle (P=.07) scores, although both were significantly higher (P=.03) than in dislocated cases treated by surgical revision. No differences regarding quality of life were observed between the 3 groups.
Functional results.
| Non dislocated | Conservative dislocation | Surgical dislocation | P | |
| Harris | 85.4±13.0 | 81.5±9.1 | 77.2±13.2 | 0.033 |
| Merle | 10.3±2.0 | 11.3±2.5 | 9.1±2.0 | 0.041 |
| Womac pain | 16.8±3.0 | 18.6±0.8 | 17±3.3 | 0.32 |
| Womac function | 22.7±4.6 | 25.8±1.1 | 23.8±4.8 | 0.20 |
Womac: Western Ontario and McMaster Universities Osteoarthritis Index.
Data presented as mean±standard deviation.
The strength of the study lied in the implantation of THA by 2 experienced surgeons using the same surgical techniques. The main limitation of this study was the fact that the measurement of acetabular and femoral anteversion was conducted two-dimensionally on simple radiographs in non-dislocated cases, rather than through a CT study. Radiographs in any rotation of the pelvis in its longitudinal or transverse axis would determine an oblique projection which would affect the measurement and reading of anteversion, but the cost of CT discouraged establishing it as a routine procedure in all THA. Nevertheless, several studies14,15 have confirmed that, despite not being precise, the possible error in measurement was within acceptable limits.
Several risk factors for dislocation have been reported in the literature. Among those relating to patients19 are advanced age, female gender, dementia, alcoholism and neuromuscular diseases. Coinciding with our study, Jolles et al20 did not find them to be a risk factor, except for an ASA score over 3. Recent studies21,22 have reported an incidence 6 times higher with the posterior or posterolateral access route compared to the anterior or anterolateral, whilst others23,24 have found a reduction in risk with the posterior or posterolateral route carrying out a meticulous repair of the soft tissues. In our study, the lateral route, which we used in all cases, presented an incidence of dislocation of 2.2%, similar to the 2.4% reported with the anterolateral route.17 In the lateral route, the fascia lata is approached longitudinally and the gluteus medius tendon is separated subperiosteally, thus facilitating the repair of both structures, preserving their dynamic mechanism to maintain the head inside the acetabulum. The size of the femoral head has been reported to be a risk factor,21,25 decreasing in heads with a size of 32mm or larger compared to those with a size of 28mm. In our study it was not found to be a risk factor, but 32mm heads only accounted for 4% of the total.
Factors related to the position of the components seem to be more frequent.19,26 It has been reported that the safety ranges regarding dislocation5 are an acetabular abduction of 40°±10°, acetabular anteversion of 15°±5° and anteversion of the femoral stem of 5°±5°, but the ideal position is difficult to obtain even for experienced surgeons.1 The literature still contains considerable discrepancies in results, despite using methods to measure anteversion by CT which were more reliable than ours.
The combined anteversion of the acetabulum and femur has been described as a significant risk factor,4 considering that it should be between 20° and 15°, respectively. In our study, were considered adequate a range of combined anteversion of 15°–30°, since the stems used did not allow a femoral anteversion greater than 10°. Jolles et al20 found that the main risk factor was a combined anteversion of <40° or >60°, whilst other studies21 reported that an acetabular anteversion >17° was a risk factor for anterior dislocation and <11° for posterior dislocation. Masaoka et al26 found no difference in the mean value of acetabular abduction between dislocation patients and controls, regardless of the direction of the dislocation, whereas anteversion was significantly less than in posterior dislocations (4.5°) and more than in anterior cases (42°) compared to controls (15°). Femoral anteversion was similar (25°) in the first 2 groups, but higher (41°) in anterior dislocations.
On the other hand, Biedermann et al17 observed that anteversion did not have an influence, whilst acetabular abduction >48° favored anterior dislocation and <42° favored posterior dislocation. Caeiro et al27 conducted a multicenter study in Spain involving 410 THA with ceramic–ceramic pairs and found 1.7% of dislocations, with the only risk factor being acetabular abduction.
Position of the acetabular component in excessive abduction also appears to have an influence on dislocation when the posterior route is used, whereas the position of the femoral stem does not.23,28
In our study, with the mentioned limitations regarding measurement of anteversion, we have also found excessive abduction (>50°) and retroversion or excessive anteversion (outside the range 10°–20°) of the acetabular component to be risk factors for dislocation, whereas the orientation of the femoral component did not have a significant influence.
Furthermore, we must also consider that some patients do not seem to present risk factors, and dislocation is attributed to a subjective failure of the soft tissues1 or local trauma caused by an extreme movement, especially when carrying out an effort from a sitting position.
Regarding the functional results, the published data show mixed results. Di Schino et al29 studied 19 patients with dislocation treated conservatively and followed during a mean period of 4 years, and found satisfactory functional results in all cases, despite having 4 patients with recurrent dislocation. Kotwal et al30 conducted a study of 99 dislocations followed for a mean period of 4.5 years, of which 50% did not require surgical revision, and found that, compared to controls without dislocation, the functional result and quality of life were lower among patients with dislocation and that this decrease became more notable with increasing episodes of recurrent dislocation. Forsythie et al31 examined 32 patients with dislocation who had been treated conservatively compared to 64 patients without dislocation, and found no significant differences in the functional assessment conducted after 1 year. In our study, dislocations which did not require surgical revision presented similar functional results to those obtained in patients without dislocations, but revision worsened the medium-term results.
With the limitations described, the only risk factors found were an increase in the angle of acetabular abduction greater than 50° and values of acetabular anteversion under or over 10°–20°. We believe that, using the lateral route, the risk of dislocation could be reduced with a meticulous repair technique of the soft tissues and a correct placement of the acetabular component, with the orientation of the stem having no influence, given the scarce margin for orientation in the uncemented model used. Reintervention should be planned meticulously, as it worsens the functional result.
Level of evidenceLevel of evidence III.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sanz-Reig J, Lizaur-Utrilla A, Miralles-Muñoz F. Factores de riesgo de luxación de artroplastia total de cadera primaria y su resultado funcional. Rev Esp Cir Ortop Traumatol. 2015;59:19–25.