Tarsal tunnel syndrome is a compression neuropathy of the posterior tibial nerve and/or its branches in the fibro-osseous tunnel behind the medial malleolus. Clinical symptoms are usually neuropathic pain and loss of sensation that get worse on standing up. Its aetiology includes various pathologies, although tumours are infrequent.
Neurilemmomas or schwannomas are benign tumours that arise from Schwann cells. Usually present as solitary tumours with good prognosis and malignancy is extremely rare.
A case of a 37-year-old man with a neurilemmoma in the posterior tibial nerve of the tarsal tunnel is presented along with the clinical, radiological and treatment features.
El síndrome del túnel del tarso (STT) es una neuropatía por compresión del nervio tibial posterior (NTP) y/o sus ramas en el túnel osteofibroso retromaleolar medial. La clínica es variada siendo los síntomas más frecuentes el dolor neuropático e hipoestesia en la planta del pie, con empeoramiento en bipedestación. Su etiología es variada siendo los tumores poco frecuente, como es nuestro caso.
Los neurilemomas o schwannomas son lesiones nerviosas benignas con origen en las células de Schwann. Habitualmente aparecen como tumores solitarios con comportamiento benigno, siendo excepcional su transformación maligna.
Presentamos un caso clínico de neurilemmoma de nervio tibial posterior a nivel retromaleolar en un varón de 37 años, con clínica de síndrome del túnel del tarso. Destacamos las principales características de esta afección incluyendo presentación clínica, estudio radiológico y tratamiento quirúrgico.
Tarsal tunnel syndrome (TTS) is a neuropathy resulting from entrapment of the posterior tibial nerve (PTN) and/or its branches as it passes beneath the flexor retinaculum in the ankle.1,2 At the postero-inferior aspect of the medial malleolus, the tibial nerve divides into 2 plantar branches (medial and lateral) and 1 sensory calcaneal branch.3 The characteristic symptom of this syndrome is localized pain, with hypaesthesia and/or paraesthesia, radiating to the sole of the foot and exacerbated by standing and walking. Tinel's sign and swelling are often found upon palpation.4
This syndrome is of variable aetiology, including trauma, rheumatoid arthritis, lipoma, giant cell tumour and, rarely, a neurilemmoma.5,6
The diagnosis of TTS is based on symptoms, nerve conduction studies, and imaging studies (ultrasound and/or MRI), if a space-occupying lesion is suspected.4
Treatment of a neurilemmoma that is causing TTS consists of surgical resection under optical magnification, preserving the integrity and continuity of the nerve.7
Clinical caseThe patient was a 37-year-old male who came to the clinic for a painful lump in the internal retromalleolar area of the right lower extremity of 3 years duration. He reported no history of trauma. In recent months, coinciding with a progressive increase in the swelling, he had been experiencing medial plantar hypaesthesia with no other changes. Upon palpation, a movable mass was found, with positive Tinel's sign on percussion. The X-rays taken (lateral and anteroposterior) were normal. Magnetic resonance (MRI) showed an ovoid mass in the distal third of the leg in the medial retromalleolar area (Fig. 1).
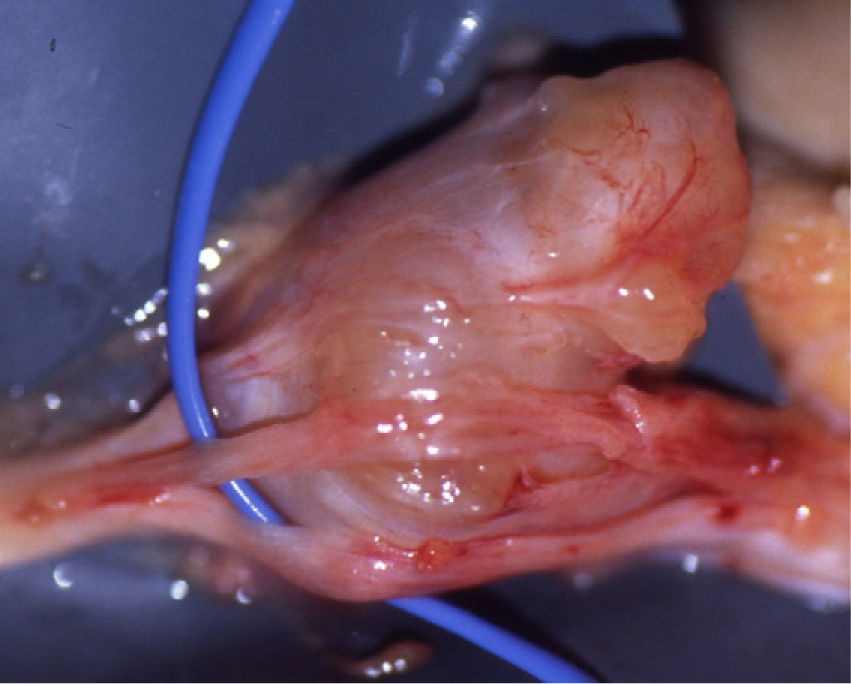
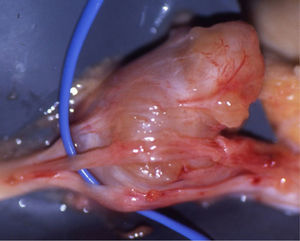
Patient underwent surgical resection with optical magnification (4×); the mass found was greyish-brown in colour (Fig. 2) and spared the continuity of the nerve fascicles adjacent to it (Fig. 3). Histological examination reported the mass to be a neurilemmoma.
There were no complications during the immediate post-operative period. The patient was followed for 8 months, at which time he was asymptomatic.
DiscussionTTS caused by a space-occupying lesion such as a neurilemmoma is rare.
A neurilemmoma is a benign lesion made up of Antoni A and Antoni B cells and Verocay bodies.8 Its most common site is the head and neck, followed by the trunk and upper and lower extremities.
The typical clinical presentation is a single, firm, slow-growing, painful lump with varied neurological symptomatology radiating distally.9
When a tumour is the suspected cause of the TTS, as it was in our case, we do imaging studies—MRI being the study of choice. The diagnosis was confirmed by histological examination of the specimen.
Prior to beginning any treatment, we perform a differential diagnosis to rule out, among others, a lumbar radiculopathy, a neuroma, and plantar fasciitis.
Tumour-caused TTS has been treated surgically under optical magnification, preserving the integrity of the fascicles adjacent to the lesion. Recurrence at the site is rare, and there is very little chance of a solitary neurilemmoma becoming malignant.10
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Please cite this article as: Gago Vidal B, et al. Síndrome del túnel del tarso en paciente con neurilemoma de nervio tibial posterior. A propósito de un caso. Rev esp cir ortop traumatol. 2011;55(6):454–456.