There is no generalised consensus regarding perioperative prophylaxis of venous thromboembolism (VTE), either on using or timing it in patients undergoing spine surgery. VTE is a current concern because, even though being an uncommon event, it can cause serious complications. The aim of the present study is to propose guidelines for the prevention of thrombotic events in posterior spinal surgery, either as deep vein thrombosis or pulmonary thromboembolism. If the number of patients getting prophylaxis drugs is reduced a subsequent reduction of the incidence of epidural haematoma can be expected.
Materials and methodsA number of 235 patients who had undergone posterior spinal arthrodesis in the previous five years were studied. Mechanical thromboprophylaxis measures consisting of compression stockings were applied in all of them. Anticoagulant drugs were also applied whenever risk factors for thrombosis were observed. Early weight-bearing was resumed immediately after surgery. Demographic, clinical, and surgical variables were collected, as well as complications appearing during the follow-up period, that was scheduled at one, two, four, six and twelve months after the surgery. Thrombotic events, if present, were diagnosed by clinical and imaging tests such as ultrasound and CT angiography.
ResultsFrom the total 235 patients of this series, one hundred and fifty-three cases met the study inclusion criteria. A total of four thrombotic events appeared, one in the form of deep vein thrombosis and other three in the form of pulmonary thromboembolism. These last patients suffering an embolism died because of it. None of the variables studied had statistical significance for the occurrence of a thrombotic event. All four patients who suffered thrombotic events were receiving anticoagulant drugs, in addition to mechanical compression stockings, because of the presence of risk factors for thrombosis.
ConclusionsBy applying the fore mentioned protocol, adequate prevention of thromboembolic events was achieved in this study population of patients undergoing posterior spinal surgery.
En la actualidad, la tromboprofilaxis en cirugía de columna es motivo de estudio ya que a pesar de ser un evento poco frecuente, puede causar complicaciones graves. El objetivo del presente estudio es proponer un protocolo de prevención de eventos trombóticos en cirugía de columna por vía posterior que reduzca la aparición de estos eventos, ya sea en forma de trombosis venosa profunda o tromboembolismo pulmonar, limitando el número de pacientes en los que se emplea profilaxis farmacológica para intentar evitar la aparición de hematoma epidural.
Material y métodoSe estudió de manera retrospectiva a los 235 pacientes del centro a los que se les había practicado una cirugía de artrodesis de columna por vía posterior en los cinco años previos, encontrándose el protocolo en vigencia. En todos ellos se aplicaron medidas mecánicas de tromboprofilaxis, consistentes en medias de compresión y, en aquellos con factores de riesgo de trombosis se aplicaron también medidas farmacológicas. En todos se inició la deambulación precoz tras la cirugía. Se recogieron variables demográficas, clínicas, quirúrgicas, así como las complicaciones aparecidas a lo largo del seguimiento que se realizaba al mes uno, dos, cuatro, seis y 12 tras la cirugía. Los eventos trombóticos, en caso de aparecer, se diagnosticaban mediante la clínica y pruebas de imagen, como la ecografía Doppler y el angio-TAC.
ResultadosDe los 235 pacientes, 153 cumplieron con los criterios de inclusión del estudio. Aparecieron un total de cuatro eventos trombóticos, uno en forma de trombosis venosa profunda y tres en forma de tromboembolismo pulmonar, acabando estos últimos en éxitus. Ninguna de las variables estudiadas tuvo significación estadística para la aparición de evento trombótico. Estos pacientes estaban recibiendo medidas farmacológicas adicionales a las mecánicas por presentar factores de riesgo de trombosis.
ConclusionesMediante la aplicación de dichas medidas se consigue realizar una adecuada prevención de eventos tromboembólicos en la población estudiada de pacientes intervenidos de cirugía de columna por vía posterior.
Thrombotic events in spine surgery, either in the form of deep vein thrombosis or pulmonary thromboembolism, are a rare event but can have serious consequences. This varies according to authors, ranging from 0% to 26.5% for deep vein thrombosis, and from 0% to 18% for pulmonary thromboembolism, according to the series.1 However, excessive bleeding can lead to adverse events such as the onset of epidural haematoma, the frequency of which is between 0% and 3%.2 This is why spine surgeons sometimes reject pharmacological prophylaxis.
Early ambulation and intermittent pneumatic compression stockings are the measures widely accepted in spine surgery.3 Drugs such as acetylsalicylic acid, low molecular weight heparin, or warfarin,4 can be combined with these measures, according to the risk of thrombotic event. The risk factors to be taken into account include the aggressiveness of the surgery, both in terms of duration and number of arthrodesis levels, post-operative immobilisation, or previous thrombotic events or disease.5 Although it is true that, of the different spinal surgery routes, the posterior approach seems to be associated with a lower rate of thrombosis, it is important to select well the patients to be given pharmacological prophylaxis to determine in whom its benefit will outweigh the risk of onset of epidural haematoma.
The aim of this study is to evaluate the incidence of thrombotic events in posterior spinal surgery with a new thromboprophylaxis protocol. The working hypothesis is that by applying these measures, based on the use of mechanical measures in all patients and pharmacological measures only in those with risk factors, thromboembolic events can be adequately prevented.
Material and methodA retrospective review was made of all the patients in our centre who had undergone primary posterior lumbar arthrodesis between 2019 and 2021. All patients over 18 years of age who had undergone a primary lumbar arthrodesis using a posterior approach were included. Patients with a diagnosis of vertebral fracture, infection, or oncology were excluded, as well as those who had been reoperated. The hospital and primary care clinical histories of all the patients were reviewed to collect demographic, surgical, and post-operative progression variables. The study was performed in accordance with the ethical standards recognised by the Declaration of Helsinki and resolution 008430 of 1993 and was approved by the Institution's Ethics Committee.
The following variables were recorded: age, sex, underlying pathology of the patient, BMI, smoking, length of hospital stay, pathology for which the intervention was performed, associated processes, arthrodesis levels, intraoperative antibiotherapy administered, use of graft, placement of drains, need for transfusion, and use of pharmacological or mechanical prophylaxis. Dural sac rupture, infection, seroma, changes in the surgical implants, such as material breakage or implant malposition, and occurrence of thrombotic events were recorded as complications.
Clinical and analytical criteria such as elevated D-dimer were used to diagnose a thrombotic event, either deep vein thrombosis or pulmonary thromboembolism. Suspected deep vein thrombosis was confirmed with imaging tests, such as Doppler ultrasound of the lower or upper limbs. However higher resolution imaging tests, such as pulmonary CT angiography, were required for suspected pulmonary embolism.6
All patients followed the recovery protocol for postoperative spine pathology patients in force in our centre. This protocol begins on admission with fitting intermittent pneumatic compression stockings that are activated in the immediate postoperative period, even in the operating theatre. Intraoperatively, before closure, drains are placed in all patients and local haemostatic agents can be used in the event of excessive bleeding.
On the first postoperative day, the patient begins to ambulate, and the drains and compression stockings are removed. Low molecular weight heparin (LMWH) is prescribed in patients with risk factors for thrombosis, such as known thrombophilia, previous thrombotic events, patients already anticoagulated, or those not starting immediate ambulation (e.g., those with dural sac rupture). Pharmacological prophylaxis is maintained for 30 days.
Outpatient follow-up is performed four weeks after surgery, where the patient is clinically and radiographically assessed. The following controls are performed at two, six, and 12 months after surgery.
Variables were collected using an Excel database (Microsoft, Washington, USA) and all statistical analyses were performed using the free software R Commander 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria).
Prior to the analytical study, the normality of the data was assessed using the Shapiro–Wilk test and with the Lilliefors test (Kolmogorov–Smirnov), the result was not significant in either case (p>.05), and therefore it was considered an adequate normal distribution of the sample, using parametric tests.
Quantitative parameters were studied using the t-Student test and qualitative parameters using χ2. The differences in the statistical results were considered significant for values of p<.05.
ResultsOf the total 235 patients who underwent posterior lumbar arthrodesis surgery, a total of 153 who met the inclusion criteria were included in the study.
In the demographic data we found a mean age of 60±13.27 years, with a predominance of males (60.8%). Some 39.9% of the patients were smokers and the mean BMI was 29±3.5. The mean hospital stay was 3.5 days.
The diagnosis for which surgery was most frequently indicated was spinal stenosis (41.2%), followed by discopathy (26.1%), spondylolisthesis (15.7%), disc herniation (9.8%), and nonspecific low back pain (2%).
Hypertension was the most frequent concomitant pathology among the patients (49.6%). Some 8.5% of the patients had a history of thrombosis and 3.9% of the patients had autoimmune pathology and, therefore, a higher risk of thrombotic events. Diabetes mellitus was present in 16.3% of patients and 6.2% of patients had cardiovascular disease which involved chronic anticoagulant drugs.
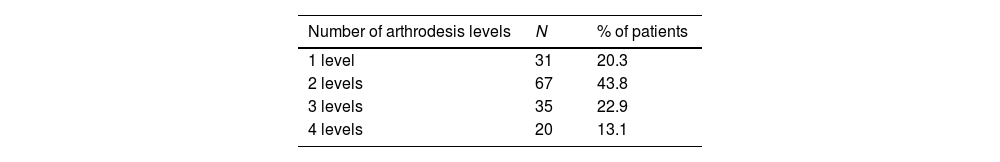
As for the surgical data, the average number of arthrodesis levels was 2.28. Table 1 shows a breakdown of the number of arthrodesis levels in Table 1. The surgical approach was posterior arthrodesis in 83% of patients and circumferential (360°) in the remainder.
As for the surgical technique, autologous graft was used in 83.7% of patients. The most commonly used antibiotic was intraoperative single-dose cefazolin in 54.4% of the patients, repeating the dose in 43% of them. A different antibiotic was used in only 2.7% of patients.
The thromboprophylactic measures used were intermittent pneumatic compression stockings only in 127 patients and in 14 patients pharmacological prophylaxis measures were also used, consisting of LMWH (enoxaparin) at a weight-adjusted dose.
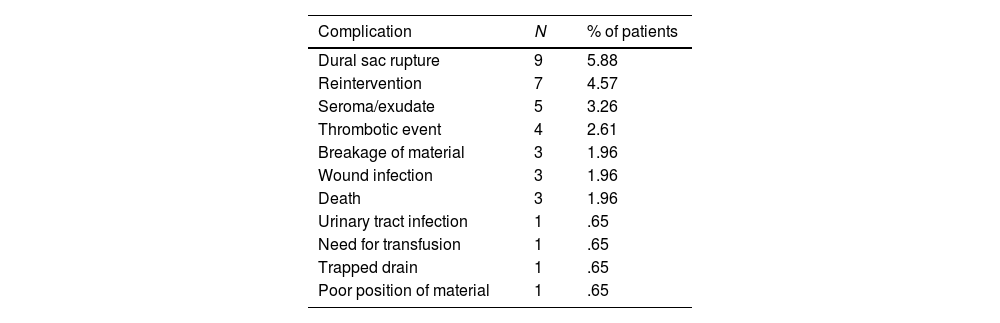
The most frequent complication was dural sac rupture, which occurred on nine occasions, unrelated to the thrombotic events that occurred. Only four patients had a thrombotic event (2.61%). Symptomatic epidural haematoma did not occur in any patient. The complications are shown in Table 2.
Complications recorded in the patient cohort.
| Complication | N | % of patients |
|---|---|---|
| Dural sac rupture | 9 | 5.88 |
| Reintervention | 7 | 4.57 |
| Seroma/exudate | 5 | 3.26 |
| Thrombotic event | 4 | 2.61 |
| Breakage of material | 3 | 1.96 |
| Wound infection | 3 | 1.96 |
| Death | 3 | 1.96 |
| Urinary tract infection | 1 | .65 |
| Need for transfusion | 1 | .65 |
| Trapped drain | 1 | .65 |
| Poor position of material | 1 | .65 |
Among the patients who suffered a symptomatic thrombotic event, several characteristics can be highlighted. Most were male (3/4), one had hypertension, and half were smokers (2/4). The mean BMI in these patients was 28.7, but there was no association with diabetes mellitus. All patients had mechanical thrombotic prophylaxis with compression stockings, and three of them were also given pharmacological thrombotic prophylaxis because they had risk factors for thrombosis: previous anticoagulation due to underlying pathology, previous thrombotic event, and autoimmune pathology such as thrombophilia, which predisposed to a higher risk of thrombosis. Dural sac rupture did not appear as a complication in any case. Of the four patients who suffered a thrombotic event, in one of them it appeared in the form of deep vein thrombosis diagnosed by ultrasound, while in the remaining three it appeared in the form of pulmonary embolism diagnosed by CT angiography. Two of these patients died; however, COVID pneumonia could not be ruled out as the cause of death in one of them because it happened at the beginning of the pandemic and PCR for coronavirus detection was not available.
DiscussionThis study shows an incidence of symptomatic thrombotic event of 2.64% and an incidence of symptomatic epidural haematoma of 0%. In the literature, the rates of symptomatic thrombotic events vary greatly, ranging from 0% to 26.5% for deep vein thrombosis, and from 0% to 18% for pulmonary thromboembolism according to the series.1 On the other hand, the incidence of symptomatic epidural haematoma ranges between 0% and 3%. Therefore, the incidence in the study population of thrombotic event rates is in line with that described in the literature, and therefore the thrombotic prophylaxis protocol could be effective.
Unfortunately, in the literature there is no clear protocol for thrombotic prophylaxis in lumbar arthrodesis surgery. There is evidence that early ambulation from the first day after surgery, which is among the prophylactic measures proposed in the study, reduces the onset of thrombotic events.7 Therefore, it would be logical to consider pharmacological prophylaxis in patients who cannot start immediate ambulation, such as those in whom dural sac rupture occurs during surgery making it impossible to start ambulation the first postoperative day. Several authors have proposed the use of pneumatic compression systems as an effective measure to reduce thrombotic events.8,9 However, physical measures may not be sufficient, and pharmacological prophylaxis should be considered in certain patients with factors that increase thrombotic risk.
Different variables have been described in the literature as risk factors for thrombosis, such as the presence of coagulopathy, cardiovascular risk factors, obesity, diabetes, difficulty in ambulation, dural sac rupture, greater number of arthrodesis levels, or longer surgical duration.10,11 Moreover, smoking, the use of anticoagulants, the presence of coagulopathy, or a greater number of arthrodesis levels have been proposed as risk factors for epidural haematoma.12,13 Nevertheless, no correlation with these factors was seen in the sample studied. This could be due to the low statistical power at the time of the detailed study of these groups of patients.
It is important to individualise the use of drugs for thrombotic prophylaxis to achieve an adequate balance between the benefit of preventing thrombotic events and the risk of haematoma.14 In this series, none of the variables was statistically significant for onset of a thrombotic event; however, most of the patients had previous thrombotic events in common, and therefore almost all of them were given pharmacological prophylaxis.
The study by Eskildsen et al.15 proposes a therapeutic algorithm based on three key points to assess the benefit-risk of thromboembolic prophylaxis: the characteristics of the patient, the risk of thrombosis due to the surgery itself, and the neurological risk in the event of haematoma. Each of these items is assigned a risk level with a corresponding score to guide the optimal method of thromboprophylaxis.
Several attempts have been made to reach a consensus on thromboprophylaxis in spine surgery, the most recent being in 2022,16 or that conducted by the ICM-VTE Spine Delegates.7 There seems to be consensus on the selection of patients according to the type of surgery and individual risk factors, such as body mass index, smoking, or history. There is consensus on the use of mechanical measures and early ambulation, combined or not with LMWH; however, this has not been possible to implement as a protocol, but rather as a guide for recommendations.
The only authors that propose a protocol for the prevention of thrombotic events in lumbar spine surgery do so for surgery using the anterior approach, due to the greater risk of thrombotic events in this approach, in which in addition to mechanical measures, pharmacological prophylaxis is generally recommended in all these patients, without increasing the incidence of haematoma.17
In the last year, the Spanish Society of Orthopaedic Surgery and Traumatology proposed thromboprophylaxis guidelines making a series of recommendations that coincide with the above. In addition, they establish LMWH as the drug of choice and recommend its administration 24–36h after surgery. The duration of pharmacological prophylaxis will vary according to the patient's specific clinical situation.16
The main limitation of the study is the small number of patients in the sample with a thrombotic event, as this is a rare adverse event. In addition, the lack of a control group with which to compare whether the protocol really reduces the occurrence of thrombotic events with respect to patients in whom it is not applied is noteworthy. All the patients in whom a thrombotic event occurred were receiving mechanical prophylaxis and, in addition, three of them were receiving pharmacological prophylaxis because they had risk factors for thrombosis, which is why appropriate measures were taken to prevent its onset. However, no symptomatic thrombotic event occurred in the rest of the patients in whom only mechanical measures were used. As advantages, this is a protocol that is easy to apply and not very invasive for patients, since it attempts to reduce the use of pharmacological measures unless necessary and appears to be effective in the population in which it has been used.
ConclusionsBy applying the proposed measures based on the use of mechanical measures in all patients, and pharmacological measures only in those with risk factors, adequate prevention of thromboembolic events was achieved in the studied population of patients who underwent posterior spinal arthrodesis surgery. We obtained a rate of symptomatic thrombotic events similar to that described in the literature and did not observe any symptomatic epidural haematoma.
Level of evidenceLevel of evidence iv.
Ethical considerationsThe present study did not act directly on patients and all data were properly anonymised, and therefore there are no ethical considerations.
FundingNo specific support from public sector agencies, commercial sector, or not-for-profit organisations was received for this research.
Conflict of interestsThe authors have no conflict of interests to declare.