Classically acute syndesmosis injuries have been treated using screws. A few years ago more flexible implants appeared evolving to current TighRope® Knotless. The primary aim of this study is to compare clinical and radiographic outcome of both implants.
Material and methodsFrom April 2019 to September 2020 68 patients diagnosed with acute syndesmosis injury were randomised to use screws or TighRope® Knotless. Syndesmosis reduction was assessed using bilateral CT potsoperatively. Outcomes were clinically and radiologically assessed at three, six, and twelve months after surgery.
ResultsNo significant differences were identified in the AOFAS Scale between groups at three months (83.1 vs. 81.80; P=1.03), nor at six (88.27 vs. 88; P=.26) or at twelve (93.03 vs. 92.10; P=.93). There were also no differences in Olerud–Molander scale at three (65 vs. 61.50; P=3.5), six (82.33 vs. 80.67; P=1.67) and twelve months (92.67 vs. 90; P=2.67). Likewise, there were no differences in rate of postoperative malreduction (no cases in both groups), loss of reduction (three cases in screw group vs. four in TighRope® Knotless group, P=.54) or complications (P=1).
ConclusionsTreatment of acute syndesmosis injuries with screws or the TighRope® Knotless implant is similar in both clinical and radiological results.
Clásicamente el tratamiento de las lesiones agudas de la sindesmosis se ha realizado mediante tornillos. Hace unos años aparecieron implantes más flexibles que han evolucionado hasta el moderno TighRope® Knotless. El objetivo del presente estudio es comparar los resultados de ambos implantes.
Material y métodosDesde abril de 2019 hasta septiembre de 2020 reclutamos 68 pacientes diagnosticados de lesión aguda de la sindesmosis que fueron aleatorizados para tratamiento quirúrgico con tornillo o con TighRope® Knotless. Realizamos control posquirúrgico con tomografía axial computarizada, y a los 3, 6 y 12 meses se recogieron datos del rango articular, valores de escalas funcionales y se realizaron estudios de radiología simple.
ResultadosLos pacientes tratados con tornillos no presentaban diferencias estadísticamente significativas en la escala AOFAS frente al grupo tratado con TighRope® Knotless a los 3 meses (83,1 vs. 81,80; p=1,03), ni a los 6 meses (88,27 vs. 88; p=0,26), ni a los 12 meses (93,03 vs. 92,10; p=0,93). Igualmente recogimos resultados similares en la escala de Olerud-Molander a los 3 meses (65 vs. 61,50; p=3,5), 6 meses (82,33 vs. 80,67; p=1,67) y 12 meses (92,67 vs. 90; p=2,67). Tampoco hubo diferencias en la tasa de malreducción posquirúrgica (ningún caso en ambos grupos), pérdida de reducción (3 en el grupo tratado con tornillo frente a 4 del grupo del TighRope® Knotless, p=0,54) o complicaciones (p=1).
ConclusionesEl tratamiento de las lesiones agudas de la sindesmosis con tornillos o con TighRope® Knotless es similar tanto en resultados clínicos como radiológicos.
According to published studies, between 10% and 20% of ankle fractures involve a tibiofibular syndesmosis injury.1–4 Damage to this joint is usually caused by trauma to the ankle in pronation and external rotation.4–6 Misdiagnosis or undertreatment of these injuries often leads to significant joint sequelae, resulting in chronic pain, joint limitation, or early osteoarthritis.5,7–10
Until recently, the gold standard to treat acute syndesmosis injuries was the use of trans- or suprasyndesmotic screws.1,3,10 However, these implants lead to rigid fixation of the joint, which increases the risk of loosening and breakage of the implant, with consequent loss of joint reduction.11,12 To avoid these complications, screw removal has often been a routine procedure in the postoperative protocol. However, this removal of material involves a second surgical procedure with its associated risks, including the risk of postoperative loss of joint reduction.2,5,13
Knotless TightRope® dynamic implants were developed to address the potential problems of using screws to treat syndesmosis.14,15 These implants enable treatment of the injury with more physiological joint dynamics, reducing the risk of loss of reduction due to loosening or breakage of the implant, and the need to remove the implant in a second operation, as they do not limit the joint function of the syndesmosis. However, they are not complication-free, including complications related to the suture knot, which often require removal of the implant.15,16 The Knotless TightRope® is the latest generation of dynamic implants designed to reduce these complications, which has a self-locking suture mechanism and therefore no need to tie a knot.
We have found only two clinical trials to date that compare the use of screws and TightRope® systems in syndesmosis injuries.8,17 We designed a prospective randomised clinical trial to compare screws versus the Knotless TightRope® implant in the treatment of acute syndesmosis injuries.
Material and methodsTo meet our objective of comparing the results of the use of screws versus the TightRope® system in the treatment of acute syndesmosis injuries, we designed a prospective randomised clinical trial registered in the International Clinical Trials Registry Platform (ICTRP) with code: ISRCTN71276902. This study was approved by our centre's ethics committee and that of the Hospital Universitario de La Paz (HULP code: 5242).
As of April 2019, all skeletally mature patients assessed in our centre's emergency department, diagnosed with acute syndesmosis injury with or without associated bone injury, were invited to participate in the present study. All those who agreed signed a specific informed consent form and became part of the study sample.
To estimate the sample size, we relied on previous publications comparing similar syndesmosis fixation systems and using the same functional scales as those used in our study.2,3,5,8 Assuming an adequate mean score (± standard deviation [SD]) on the American Foot and Ankle Society (AOFAS) scale at 1 year after joint fixation with screws of 93.1±9.313,2 a minimum of 40 patients (20 per study group) were required to demonstrate the non-inferiority of the TightRope® system with a non-inferiority cut-off of 10%, power of 80%, confidence level of 97.5%, and estimating a loss rate of 15%.
From this estimate, and based on the only 2 previous studies that used the same specific implants that we used in our study8,17 (screws and Knotless TightRope®), our target number was at least 60 patients (30 in each treatment group) for our clinical trial.
We excluded from the study patients with open growth plates, patients with previous injuries to the affected ankle or with rheumatic and/or neuromuscular diseases that could interfere with the recorded results, as well as patients who were unable to follow the postoperative instructions and protocols detailed below.
Surgical techniquesThe operations were performed by members of the centre's trauma service, from the foot and ankle unit and from the other the units. The anaesthesiologist chose the type of anaesthesia, and all surgeries were performed under ischaemia with a cuff placed on the thigh.
First, the patients underwent fracture fixation: in the case of peroneal malleolus fractures, this was done using a plate and interfragmentary screws, while tibial malleolus and posterior malleolus fractures were synthesised with 3.5mm cannulated screws.
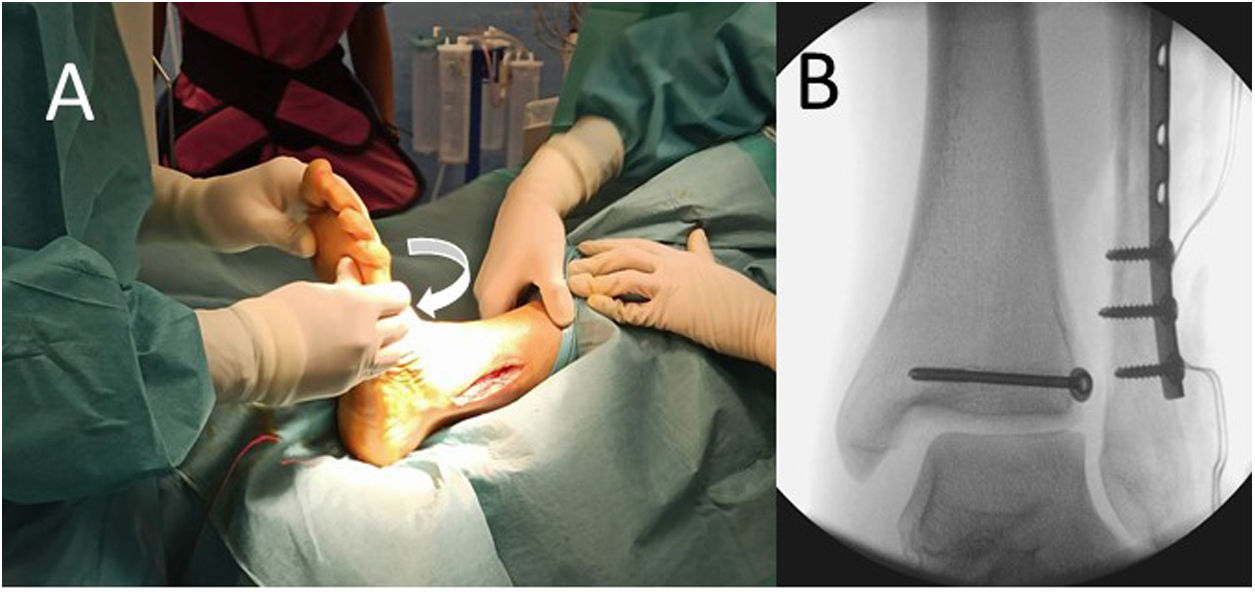
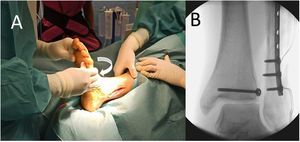
We then checked the syndesmosis injury using an external rotation stress test under fluoroscopic control (Fig. 1). If this joint was found to be affected, it was fixed using one of the implants in the study: a 3.5mm fully threaded four-axis trans-syndesmotic screw or the Knotless TightRope®. To select the implant, at the start of the trial, the statistics team at our centre provided us with a randomisation list created using computer software from which numbered opaque envelopes were made, into which a card was inserted with the implant to be used in each case according to the order of the patient in the recruitment process. Thus, once the syndesmosis injury had been verified intraoperatively, the circulating nurse opened the relevant envelope and we proceeded to use the fixation system that appeared on the card taken from it. We used a single implant in each case except in the Maisonneuve injuries, where we placed two implants in different planes to achieve fixation with better rotational control over the joint.
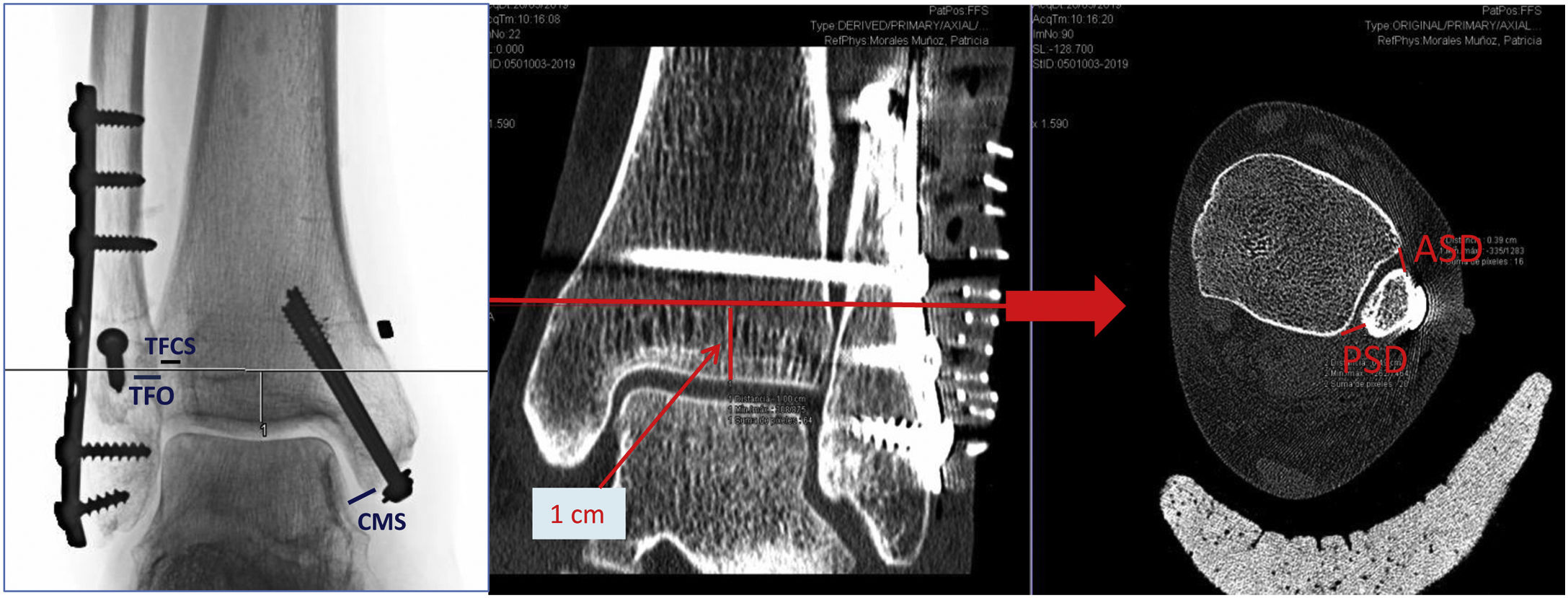
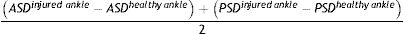
Protocol and postoperative follow-upThe day after the operation, we took a plain X-ray and computed axial tomography (CT) of both ankles to check for adequate joint reduction and correct positioning of the implant. As criteria for correct reduction on plain X-ray, we considered the following: clear medial space (CMS) less than 4mm, tibiofibular clear space (TFCS) less than 6mm, and tibiofibular overlap (TFO) greater than 1mm on the mortise projection and 1cm from the joint line.7,10,11,18 In the case of the CT study we used the criteria published in the article by Mukhopadhyay et al.18 who use anterior syndesmosis distance (ASD) and posterior syndesmosis distance (PSD) measurements; considering a value of less than 2mm correct joint reduction in the equation (Fig. 2):
All these values were measured in axial CT projections at 1cm from the articular surface by one surgeon from the foot and ankle unit.
The postoperative protocol for all patients was the same. Immobilisation with a posterior foot splint for 2 weeks and then weight-bearing mobilisation of the ankle joint was allowed with referral to the rehabilitation service to begin treatment there. At 6 weeks after surgery, all patients began gradual partial weight bearing until full weight bearing about 2 months after surgery. Impact sports or high intensity physical activities were resumed 6 months after surgery.
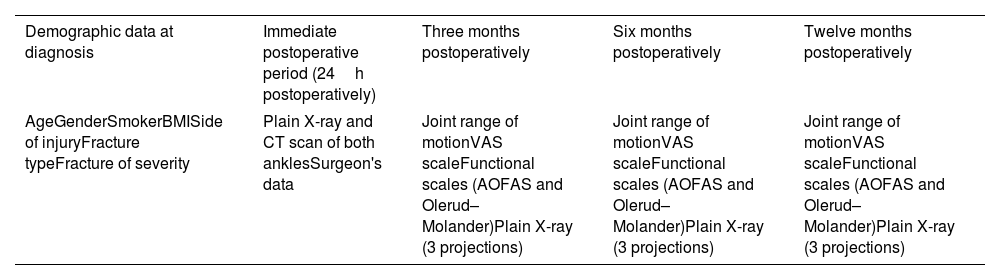
Clinical check-ups at 3, 6, and 12 months after the surgery were performed by 2 members of the foot and ankle unit. In these check-ups, the arc of joint motion of the operated ankle was measured, using a manual goniometer, the visual analogue scale (VAS) to rate pain, and the AOFAS and the Olerud–Molander score (OM) forms were completed. A plain X-ray was also taken at these check-ups in 3 projections (anteroposterior, lateral, and mortise projection) to confirm correct progression of the fractures, maintenance of the articular reduction of the syndesmosis, and to rule out complications with the implants used (Table 1). All data were collected by 2 specialists from the foot and ankle unit.
Timeline for data collection and imaging studies.
| Demographic data at diagnosis | Immediate postoperative period (24h postoperatively) | Three months postoperatively | Six months postoperatively | Twelve months postoperatively |
|---|---|---|---|---|
| AgeGenderSmokerBMISide of injuryFracture typeFracture of severity | Plain X-ray and CT scan of both anklesSurgeon's data | Joint range of motionVAS scaleFunctional scales (AOFAS and Olerud–Molander)Plain X-ray (3 projections) | Joint range of motionVAS scaleFunctional scales (AOFAS and Olerud–Molander)Plain X-ray (3 projections) | Joint range of motionVAS scaleFunctional scales (AOFAS and Olerud–Molander)Plain X-ray (3 projections) |
AOFAS: American Orthopaedic Foot & Ankle Society score; BMI: body mass index; CT: computed axial tomography scan; VAS: visual analogue scale.
Routine removal of the syndesmotic screw was not performed throughout the study.
Statistical analysisFirst, we performed a descriptive analysis of the variables using absolute (n) and relative (%) frequencies for qualitative variables. In the case of quantitative variables, we initially evaluated their parametric behaviour using the Kolmogorov–Smirnov test. Based on this data, we used the mean and SD if they followed a normal distribution, or the median (interquartile range [IQR]) if not.
Secondly, we compared the two fixation systems studied. To do so, we used the Chi-square test (χ2) for qualitative variables and for quantitative variables, we used the Student's t-test or the Mann–Whitney U test according to the results obtained from the normality test, i.e., according to whether the variables were normally or non-normally distributed, respectively. In all cases we considered a p-value of less than .05 statistically significant.
IBM SPSS® version 25.0 programme (IBM Corp; USA) will be used for the data analysis.
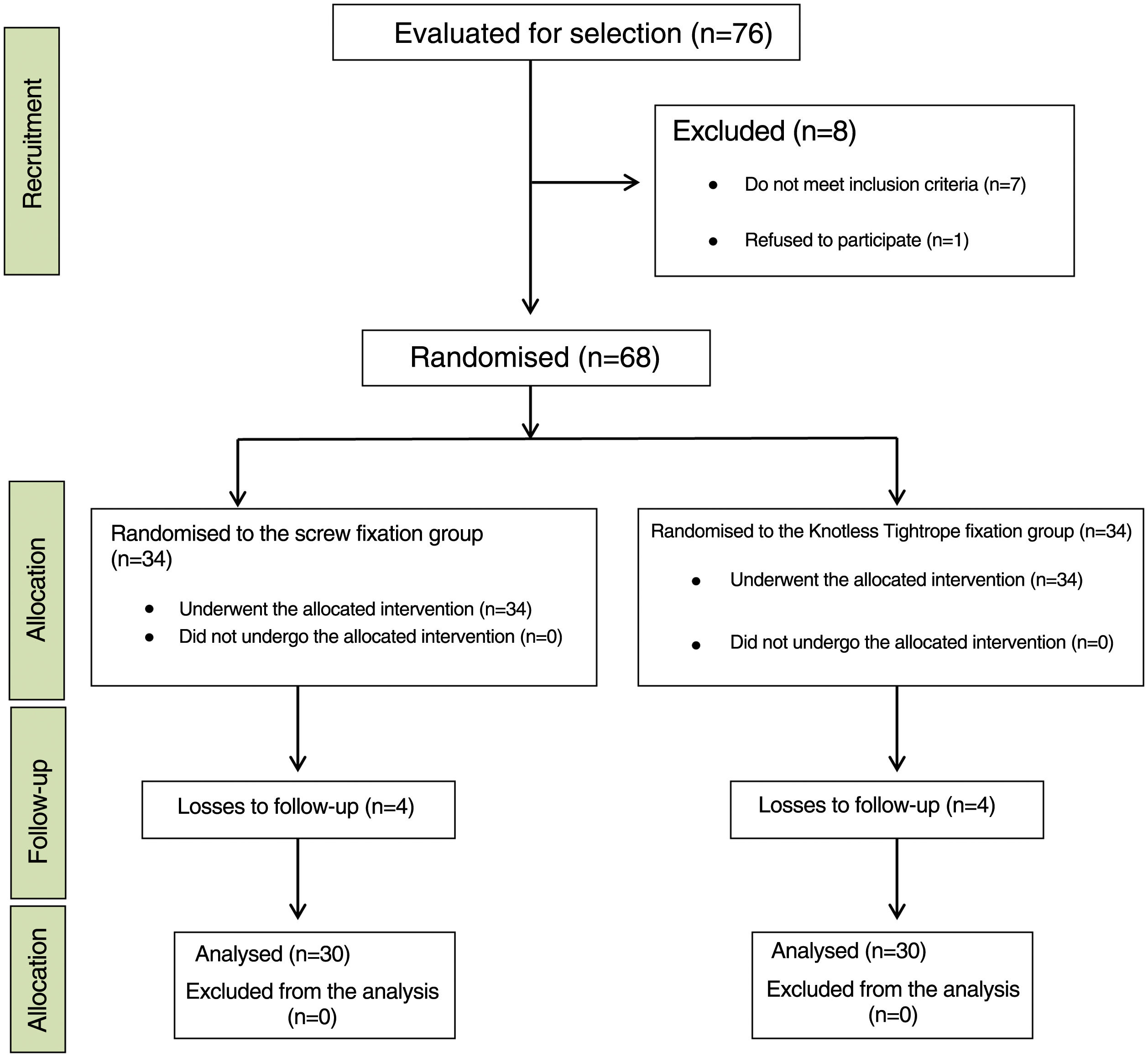
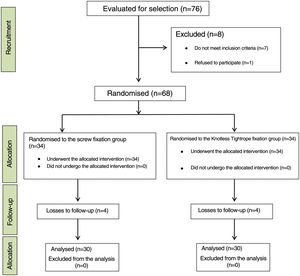
ResultsFrom April 2019 to September 2020 a total of 76 patients attended our emergency department with acute syndesmosis injury associated or not with ankle fracture. Of these, one patient decided not to participate in the study and 7 others did not meet the inclusion criteria. Therefore, a total of 68 patients were randomised: 34 underwent surgery with quadricortical transsyndesmotic screw implantation and 34 were treated with the Knotless TightRope® system. Eight patients were lost to follow-up (4 from each group). Three of them were not from Spain and returned to their country before completing the follow-up, 2 patients (one from each group) had pseudoarthrosis: one in the peroneal malleolus and one in the tibial malleolus, requiring reoperation 6 months after the initial surgery. One patient did not follow the postoperative instructions correctly and another 2 patients treated with screws wished to have the screws removed and leave the study during follow-up, and therefore are not included in the analysis of results. Finally, a total of 60 patients (30 in each treatment group) completed the one-year follow-up and constituted the study sample (Fig. 3).
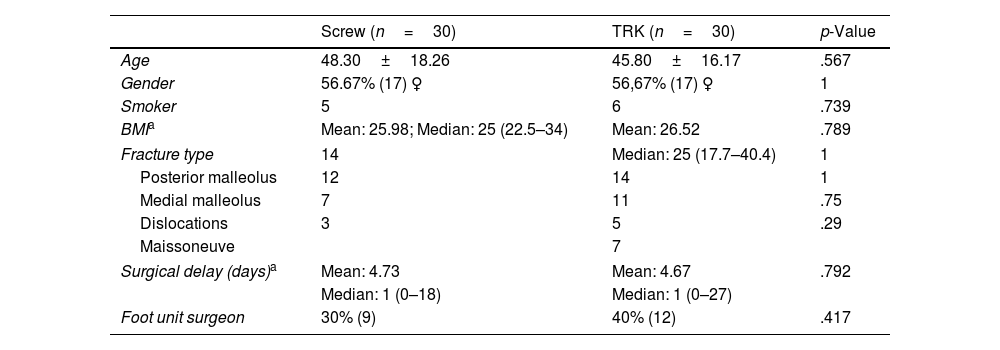
First, we performed an analysis of the demographic variables of each group: age, gender, body mass index (BMI) and smoking habits of the participants in each group. The same was done with respect to the fracture severity data; for which in each case we analysed involvement of the posterior and/or medial malleolus, the existence of joint dislocation during the initial assessment in the emergency department or a diagnosis of Maisonneuve's injury. Other factors analysed were the time from diagnosis to intervention and the type of surgeon performing the intervention, for the latter aspect we differentiated between surgeons with more than 5 years of experience in the foot and ankle unit and the other specialists in the department. Statistically significant differences were not found between the 2 groups in any of these variables (Table 2).
Data from each study group.
| Screw (n=30) | TRK (n=30) | p-Value | |
|---|---|---|---|
| Age | 48.30±18.26 | 45.80±16.17 | .567 |
| Gender | 56.67% (17) ♀ | 56,67% (17) ♀ | 1 |
| Smoker | 5 | 6 | .739 |
| BMIa | Mean: 25.98; Median: 25 (22.5–34) | Mean: 26.52 | .789 |
| Fracture type | 14 | Median: 25 (17.7–40.4) | 1 |
| Posterior malleolus | 12 | 14 | 1 |
| Medial malleolus | 7 | 11 | .75 |
| Dislocations | 3 | 5 | .29 |
| Maissoneuve | 7 | ||
| Surgical delay (days)a | Mean: 4.73 | Mean: 4.67 | .792 |
| Median: 1 (0–18) | Median: 1 (0–27) | ||
| Foot unit surgeon | 30% (9) | 40% (12) | .417 |
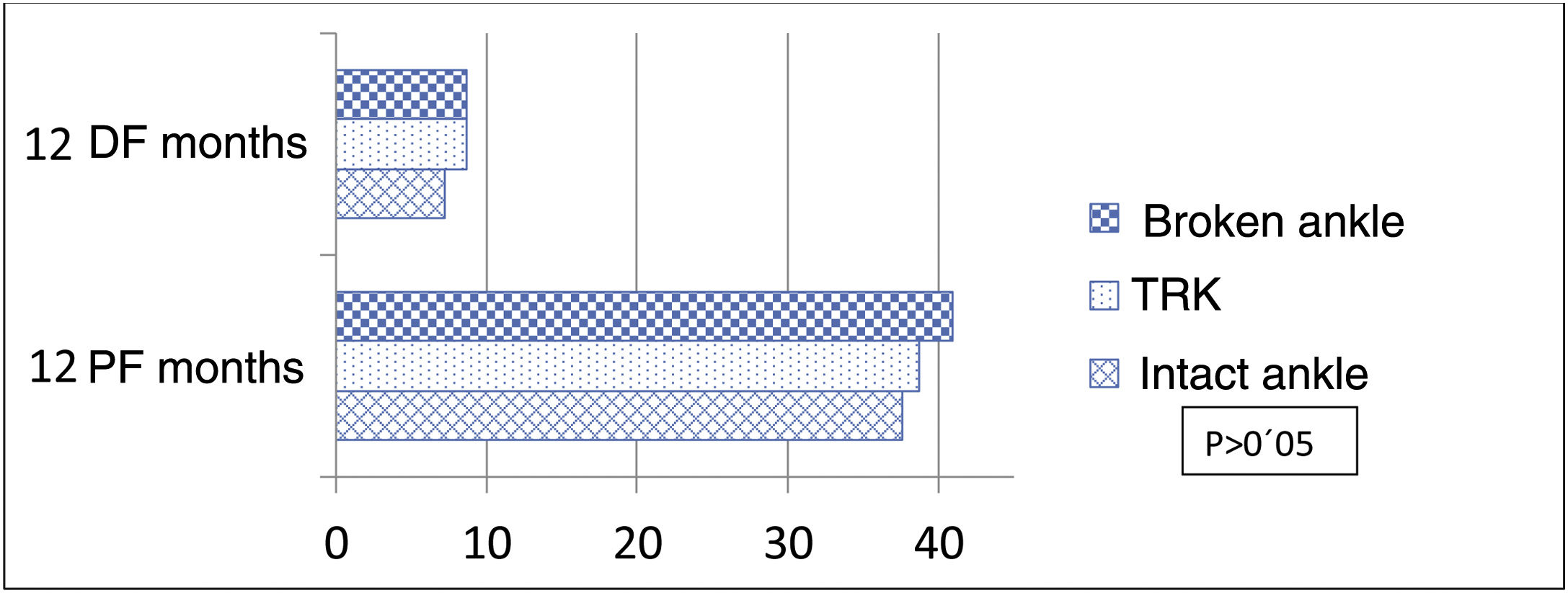
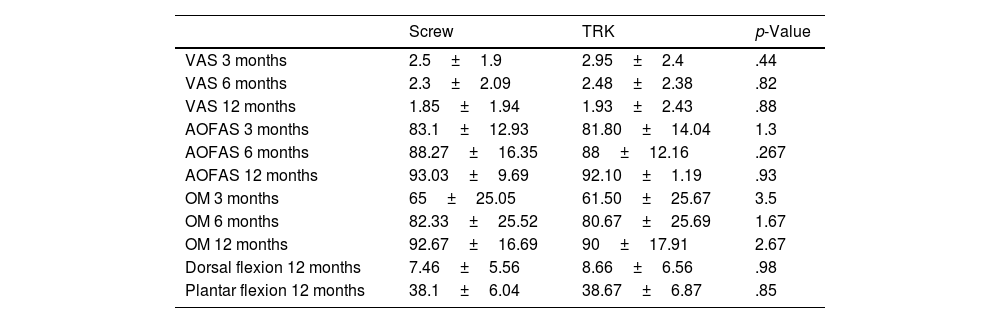
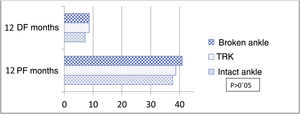
With regard to the analysis of the VAS and AOFAS and OM scores, at 3, 6 and 12 months, no statistically significant differences were found in the scores of the two groups. However, with respect to joint range of motion, patients treated with the Knotless TightRope® implant had greater joint range of motion at the end of follow-up, especially for dorsal flexion. These differences in motion were not statistically significant (Table 3). In view of these scores, we performed a stratified analysis dividing the patients into 3 groups: treated with the Knotless TightRope® (n=30), treated with a screw that broke during follow-up (n=12), and treated with a screw that remained intact during the 12 months of the study (n=19). Patients with screw breakage had higher motion scores 12 months after surgery than those with intact screws: mean dorsal flexion of 8.6 (6.74) vs. 7.1 (±5.39) and mean plantar flexion of 40.91 (4.9) vs. 37.7 (±6.44), respectively. These motion scores in the group with transsyndesmotic screw breakage were close to those recorded for the Knotless TightRope® implant (8.6±6.3/38.67±6.69) (Fig. 4). However, there were still no statistically significant differences in the VAS, AOFAS and OM scores between the 3 study groups.
Table of results.
| Screw | TRK | p-Value | |
|---|---|---|---|
| VAS 3 months | 2.5±1.9 | 2.95±2.4 | .44 |
| VAS 6 months | 2.3±2.09 | 2.48±2.38 | .82 |
| VAS 12 months | 1.85±1.94 | 1.93±2.43 | .88 |
| AOFAS 3 months | 83.1±12.93 | 81.80±14.04 | 1.3 |
| AOFAS 6 months | 88.27±16.35 | 88±12.16 | .267 |
| AOFAS 12 months | 93.03±9.69 | 92.10±1.19 | .93 |
| OM 3 months | 65±25.05 | 61.50±25.67 | 3.5 |
| OM 6 months | 82.33±25.52 | 80.67±25.69 | 1.67 |
| OM 12 months | 92.67±16.69 | 90±17.91 | 2.67 |
| Dorsal flexion 12 months | 7.46±5.56 | 8.66±6.56 | .98 |
| Plantar flexion 12 months | 38.1±6.04 | 38.67±6.87 | .85 |
AOFAS: American Orthopaedic Foot & Ankle Society score; OM: Olerud–Molander scale; VAS: visual analogue scale.
In the CT studies performed in the first 24h after surgery comparing the joint situation of the syndesmosis injury with the healthy ankle, we found that all the patients in the study, those treated with screws and those treated with the Knotless TightRope® had adequate joint reduction values after surgery.
During follow-up, from the plain X-ray study, there was loss of joint reduction of the syndesmosis in 3 patients in the screw-treated group and 4 in the Knotless TightRope® group (p=.54).
Finally, analysing the complications, 4 patients had a complication in each group. Among those treated with a screw, one patient suffered complex regional pain syndrome (CRPS) and all the osteosynthesis material was removed. The other 3 patients required screw removal due to high stiffness and pain that their surgeon related to the implant. In the group treated with the Knotless TightRope®, one patient had a superficial infection, one patient had a superficial surgical wound dehiscence, and the other 2 patients underwent implant removal due to implant intolerance. These data showed no statistically significant differences between the two groups (p=1).
DiscussionThere are currently 2 options to treat acute syndesmosis lesions: rigid implants (screws) or flexible implants (TightRope®).
There are several clinical trials comparing these treatment systems: screws vs. TightRope® systems.2,3,5,6,8,17 In most of these studies, patients treated with dynamic implants presented better scores on the functional scales,2,5,6,8,17 however, the results of these scales did not show statistically significant differences between either group, except in one.3
Despite the extensive published literature on this condition, we found only 2 clinical trials comparing screws and the Knotless TightRope® in the treatment of syndesmosis injuries.8,17 The study by Colcuc et al.8 analysed the results of a total of 54 patients: 26 treated with TightRope® and 28 with screws. In all patients in the screw fixation group, screw removal was performed in a second operation before weightbearing was allowed. However, in the multicentre study by Sanders et al.17 30% of patients treated with screws also underwent a second scheduled screw removal procedure. Similar postoperative screw removal protocols have been followed in other studies analysing the classic TightRope®, the largest sample size was that published by Andersen et al.3 Because the patients underwent reoperation during follow-up, the postoperative course of each group is not uniform, which could influence the results and the reported complication rate. The retrospective study published by Schepers et al.19 analysed 76 cases of patients who underwent syndesmotic screw removal as scheduled reoperation and found a total of 22.4% complications, including 9% infectious conditions, and 6.6% loss of joint reduction.
For all these reasons, and in an attempt to standardise the postoperative protocol of the patients in each group as much as possible, in our trial we did not schedule removal of fixation material in any patient, and only performed this surgery in cases that presented some type of complication. Thus, we attempted to ensure that the results achieved can be attributed to the type of implant used.
When we assessed the functional results with both implants, we found no significant differences between the two groups in our study. Very similar results were achieved in the study by Colcuc et al.8 with AOFAS and OM scores very like ours at the end of follow-up: 91±8 and 91±9 on the AOFAS scale and 90±12 and 93±12 on the OM scale for screws and the Knotless TightRope®, respectively. Grassi et al. published one of the most recent meta-analyses evaluating the 2 types of syndesmosis fixation systems: screws vs. TightRope® type implants.1 A total of 7 clinical trials were analysed (6 using the classic TightRope® implant and one using the Knotless Tightrope® system), and there was a tendency to achieve better functional results with flexible implants. However, statistically significant results were only obtained on the AOFAS scale and not the OM or VAS scales. Of the seven clinical trials, two did not use a screw as a fixed implant but a cerclage system in one and a fixation plate specifically designed for the syndesmosis in the other. Shimozono et al.12 published another meta-analysis of only the 5 trials comparing classic screws with the TightRope® systems (only one of these studies analysed the Knotless Tightrope® implant). In their results, they did find significant differences in AOFAS and OM scores. Analysing the postoperative protocol of the trials, in 23,8 the implant was routinely removed during the follow-up period. It is possible that the patient undergoing a second operation, together with the risks involved, may have affected the recovery process, and delayed the recovery process and this would be reflected in the functional scale scores. In addition, there is currently no clear support in the literature that this intervention is of real benefit to the patient. In this regard, Dingemans et al.20 published a systematic review to assess the need for screw removal as a routine procedure after treatment of syndesmosis injuries. In their conclusions, with the available literature, they are unable to reach a strong recommendation in this regard given the low quality of the publications. However, the tendency they find is that there seems to be no justification to subject patients to this further intervention from the results of these publications. Along these lines, it would be interesting to design new studies with a larger number of patients and a longer follow-up, analysing the effect of removing the material on the patients’ recovery process.
When assessing joint range of motion in our study, we found better scores in the patients treated with the Knotless Tightrope® implant. However, the differences between the groups are not significant and we were not able to correlate this with the functional results of the patients. There are few studies that analyse this variable, but those that do have achieved results similar to ours.2,6,21
In terms of complication rates, we found similar results in both groups to the meta-analysis by Onggo et al., 22 based on 5 clinical trials (only one analysing the Knotless Tightrope® implant), and those by Fan et al.23 and Gan et al.,24 which analyse cohort studies in addition to clinical trials, all based on the classic TightRope® systems. Considering that malreduction of the syndesmosis is the most important predictor of long-term outcomes for patients with acute injuries of this joint,21,25 in our study we found no differences between the 2 groups, in either the initial malreduction rates after surgery, or in the rate of loss of reduction during follow-up. In this aspect, most studies report similar results.2,3,15 The clinical trial by Andersen et al.3 found no differences in initial malreduction. However, the loss of reduction rate was higher in the screw-treated group; in fact, their results showed a 2.5-fold higher risk of loss of joint reduction in the screw-treated group. This could be related to their routine removal of the screws, given that in 5 of the 7 cases in which loss of reduction occurred, this was after the implant removal surgery. In fact, Laflemme et al.,2 who only remove the screw in cases of complication and not as a postoperative protocol, cite 4 cases of loss of reduction among patients treated with screws, 3 of which required reoperation to remove the fixation material. Once again, and in view of these data, it could be that surgery to remove the material, as a routine procedure, could contribute to increased complication rates, affecting the long-term results of the patients, as we mentioned previously.
Among the limitations of our study, we consider that, although the number of patients studied is similar to that of previous publications, it is still a very limited number. Likewise, the follow-up period in our case is 12 months and, given that the onset of degenerative joint sequelae is usually seen between 2 and 5 years after the injury, we were not able to analyse this variable in our trial. We believe that studies with longer follow-up are needed to assess this aspect, and its impact on patients’ functional status. Furthermore, the fact that the surgeons were not specifically foot and ankle specialists could have a double effect: less experience with the use of newer implants such as the Knotless Tightrope® of surgeons who do not deal specifically with this condition could lead to a higher rate of complications and worse outcomes. However, because these lesions are often treated as emergency surgeries and are not always performed by surgeons belonging to a specific unit, the results we obtained are more generalisable and would be closer to standard clinical practice.
Finally, with a view to future studies, we believe it would be interesting to design cost studies to determine the differences between both types of implants in this respect. It is possible that considering a treatment with screws without routinely requiring a second intervention to remove them could lead to significant cost savings compared to the use of dynamic implants.
ConclusionsFrom the present study, we conclude that treating acute syndesmosis injuries with screws or with the Knotless Tightrope® implant produces similar functional and radiological results, and complication rates. However, studies with larger numbers of participants and longer follow-ups are needed to increase the consistency of these data.
Level of evidenceLevel of evidence iii.
FundingThis study was funded by the SECOT Foundation's Research Initiation Project Grant.
Conflict of interestsThe authors have no conflict of interests to declare.