Clinical, radiological and functional results of the first Spanish series of patients undergoing total hip arthroplasty assisted by Mako® (Stryker) robotic arm at the Hospital Clínico San Carlos (HCSC) in Madrid.
Material and methodsProspective and descriptive study analyzing the first 25 patients who underwent robotic-assisted THA at the HCSC, with a minimum follow-up of 4 months. Demographics, imaging studies (Mako® processing, Rx and CT), clinical parameters, functionality (modified Harris) and associated complications were evaluated.
ResultsAverage age was 67.2 years (min 47, max 88), being 56% male population sample. 88% involves primary coxarthrosis, 4% post-traumatic coxarthrosis, 4% secondary avascular necrosis and 4% secondary femoroacetabular impingement.
Average surgery time was 116.9min (min 92, max 150). The average time of the first five surgeries was 122.6min, and, regarding the last five interventions, it was 108.2min. Found medical intraoperative complications were four intraoperative markers loss.
Average admission time was 4.4days (min 3, max 7), with an average postoperative haemoglobin decrease of 3.08±1.08g/dl, requiring a transfusion in 12% of the cases. Three medical complications have been registered in the meantime of the admission, with a relevant case of a confusional syndrome and a fall, which resulted in a non-displaced AG1 periprosthetic fracture.
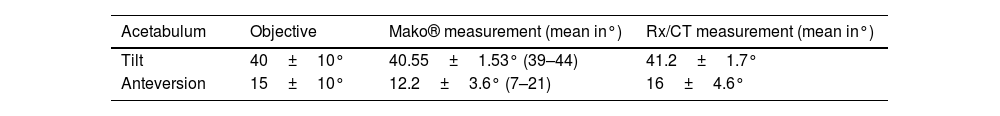
The analysis of the positioning of registered implants with Mako® system shows 40.55±1.53 acetabular inclination degrees and 12.2±3.6 acetabular anteversion degrees. The postoperative image study carried out on patients, are consistent with Mako® results, as it shows an acetabular inclination of 41.2±1.7 in Rx, as well as acetabular anteversion of 16±4.6 in CT.
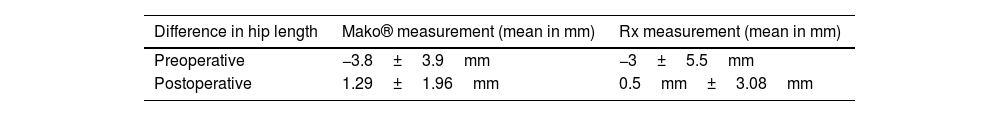
Hip length variance ranges depending on preoperative values of 3.91mm (SD: 3.9; min −12, max 3) to 1.29mm (SD: 1.96) after surgery registered with Mako®, with an increase of an average hip length of 5.64mm (SD: 3.35). Rx simple study results show a postoperative difference between both hips of 0.5±3.08mm, which is consistent with Mako® results.
Native femoral offset was stable after surgery with a showing difference both pre and post operative of the intervened hip of 0.1mm (SD: 3.7), registered with Mako®.
Preoperatory modified Harris punctuation was 41.6±13.3, improving to postoperative values of 74.6±9.7 after four months since the surgery. No complications were registered in immediate postoperative (4 months).
ConclusionsTotal hip arthroplasty robot-assisted achieves an adequate precision and repeatability of the implant positioning and the postoperative hip dysmetry without showing an increase of associated complications to the technique applied. Surgery time, complications and functional results in a short-time period are similar to conventional techniques applied to great series previously published.
Resultados clínicos, radiológicos y funcionales de la primera serie española de pacientes intervenidos de artroplastia total de cadera (ATC) asistida mediante brazo robótico Mako® (Stryker) del Hospital Clínico San Carlos (HCSC) de Madrid.
Material y métodosEstudio descriptivo prospectivo que analiza los primeros 25 pacientes intervenidos de ATC asistida por robot (ATCaR) en el HCSC, con un seguimiento mínimo de 4meses. Se evaluaron la demografía, los estudios de imagen (procesamiento Mako®, Rx y TAC), los parámetros clínicos, la funcionalidad (Harris modificada) y las complicaciones asociadas.
ResultadosLa edad media fue de 67,2años (min 47, máx 88), siendo el 56% varones. El 88% corresponden a coxartrosis primaria, el 4% postraumática, el 4% secundaria a necrosis avascular (NAV) y el 4% secundaria a choque femoroacetabular.
El tiempo medio de cirugía fue de 116,9min (min 92, máx 150). La media de las 5 primeras intervenciones fue de 122,6min, y la de las 5 últimas, de 108,2min. Como complicaciones intraoperatorias se cuantificaron 4 pérdidas de marcadores intraoperatorios.
El tiempo de ingreso medio fue de 4,4días (min 3, máx 7), con una disminución de hemoglobina posquirúrgica media de 3,08±1,08g/dl, requiriendo transfusión en el 12% de los casos. Se registran 3 complicaciones médicas durante el ingreso, destacando un síndrome confusional con caída y fractura periprotésica AG1 no desplazada.
El análisis del posicionamiento de los implantes registrados con sistema Mako® fueron 40,55±1,53 grados de inclinación y 12,2±3,6 grados de anteversión acetabular. El estudio de imagen posquirúrgico realizado a los pacientes, en concordancia con Mako®, muestra valores de inclinación acetabular de 41,2±1,7 en Rx y versión acetabular de 16±4,6 en la TAC.
La discrepancia de longitud de cadera varía de valores preoperatorios de −3,91mm (DE: 3,9; min −12, máx 3) a 1,29mm (DE: 1,96) tras la cirugía registrados con Mako®, con un aumento de longitud de cadera medio de 5,64mm (DE: 3,35). El estudio de Rx simple demuestra una diferencia posquirúrgica en concordancia con Mako® entre ambas caderas de 0,5±3,08mm.
El offset femoral nativo se mantuvo tras la cirugía con una diferencia pre y posquirúrgica de la cadera intervenida de 0,1mm (DE: 3,7), registrado con Mako®.
La puntuación Harris modificada preoperatoria fue de 41,6±13,3, mejorando hasta valores postoperatorios de 74,6±9,7 a los 4meses.
No se registraron complicaciones en el postoperatorio inmediato (4meses).
ConclusionesLa artroplastia total de cadera asistida por brazo robótico consigue una adecuada exactitud y reproducibilidad en el posicionamiento de los implantes y la dismetría de cadera posquirúrgica, sin aumentar las complicaciones asociadas a la técnica. El tiempo de cirugía, las complicaciones y los resultados funcionales a corto plazo son comparables a la técnica convencional de las grandes series publicadas previamente.
Although total hip arthroplasty (THA) is a successful surgical treatment for symptomatic osteoarthritis of the hip in advanced stages,1,2 there continues to exist a fine line between good clinical outcomes and the development of major complications. When such complications do occur, they compromise the patient's ability to function due to inadequate biomechanics,3 impingement,4 instability,5 accelerated liner wear,6 and lower limb length discrepancy.3 In the future, these circumstances will result in our patients requiring a revision THA surgery.7 Correct component orientation determines the biomechanics of THAs so as to avoid such complications. Orthopaedic surgeons and healthcare systems are investigating methods to increase the accuracy of implant placement with the aim of averting adverse outcomes.8
Recent studies have compared the radiological results of robotic arm-assisted THA (rTHA) and manual THA (mTHA) with respect to orientation and alignment of the prosthetic components within the theoretical ranges of the classical safety zones described by Lewinnek et al.9 and by Callanan et al.10 for THA, demonstrating that the use of rTHA yields superior radiological results compared to mTHA, improving the precision of implant placement, femoral stem alignment, canal filling, and differences in overall offset compared to mTHA.11 Nevertheless, the improvement in radiological outcomes in rTHA has not translated into differences in short-term functional outcomes in the studies published.12
Concerning outcomes, we must include the biomechanical results of THA. Older software did not include preoperative dynamic imaging, and advanced stage osteoarthritis of the hip often presents with abnormal spinal-pelvic alignment and sagittal imbalance along the hip flexion arc. This implies that new patient-specific safety zones must be taken into account if optimal implant positioning is to be achieved, which may fall outside the theoretical safety zones. These new features are of great importance to prevent implant position-related complications and represent one step closer to excellence in THA.13 The analysis of the literature (in terms of long-term follow-up results) is controversial, because no long-term studies of the new rTHA have been published.
Several advances in implant design and materials have been made up to the current THA. There have been few changes in surgical technique until rTHA was developed and included in our daily practice. In the last decade, rTHA has increased its numbers by decreasing surgical errors and improving accuracy and precision compared to mTHA.14
The limitations of rTHA have to do with the additional costs (purchase of the robotic device, software upgrade, and maintenance; training of the surgical team); compatibility with a number of selected implant designs; the learning curve; the need for preoperative CT for surgical planning, and technical issues, such as robotic device malfunction with conversion from rTHA to conventional mTHA in up to 18% of the cases.15
rTHA is now becoming more widely used in hospital hip units in the Americas and in Europe. To date, no experience with rTHA in Spain has been reported.
The aim of this study was to evaluate the short-term results with Mako® rTHA in the first Hip Unit in Spain that has started to use this technology in its routine practice.
As a working hypothesis, we consider that hip prosthesis surgery assisted by the Mako robotic arm provides the surgeon with a high degree of accuracy and precision in the implantation of the components of the replacement compared to the outcomes reported in the literature, without increasing complications associated with this surgery.
Material and methodsThis is a non-randomised, prospective, descriptive study that analyses the first 25 patients who underwent total hip arthroplasty assisted by Mako® (Stryker) robotic arm at our hospital.
The study was approved by the Ethics and Research Committee of our hospital (protocol C.P.-C.I.22/205-O_P), in accordance with the ethical guidelines set out in the Declaration of Helsinki.
The patients included in the study were those assessed in the consultation of the Hip Unit of our hospital centre from June to September 2021 who met all the criteria for participation.
The inclusion criteria for the series were: patients with hip osteoarthritis grades II and III as per the Tönnis radiological scale16; with functional limitation and requiring daily analgesia; who were able to comprehend the information regarding the use of the new robotic arm-assisted system, and who gave their informed consent.
Patients who did not understand the informed consent; who did not want robotic arm-assisted surgery; who were not eligible for prosthetic hip surgery due to associated medical comorbidities, and those who had a prior hip arthroplasty requiring revision surgery were excluded.
The epidemiological analysis consisted of assessing patients’ age, sex, laterality, and clinical-radiological diagnosis.
The radiographic study carried out consisted of preoperative plain AP pelvis and axial Rx of both hips, preoperative and postoperative hip CT, serial plain hip Rx (at 24h, 4 weeks, and 2 and 4 months following the intervention), as well as a tele-Rx of the lower limbs during postoperative weight-bearing.
The preoperative study involved the measurement of the AP pelvis and axial hip X-ray following calibration with a radiographic reference, classification of the degree of osteoarthritis according to the Tönnis radiological scale, assessment of the possible dysmetry between the two hips (by comparative analysis of the distance between the ischial crests and the most medial aspect of the lesser trochanter), and calculation of the offset of the two hips. These measurements were repeated in the simple Rx study 4 months following the procedure.
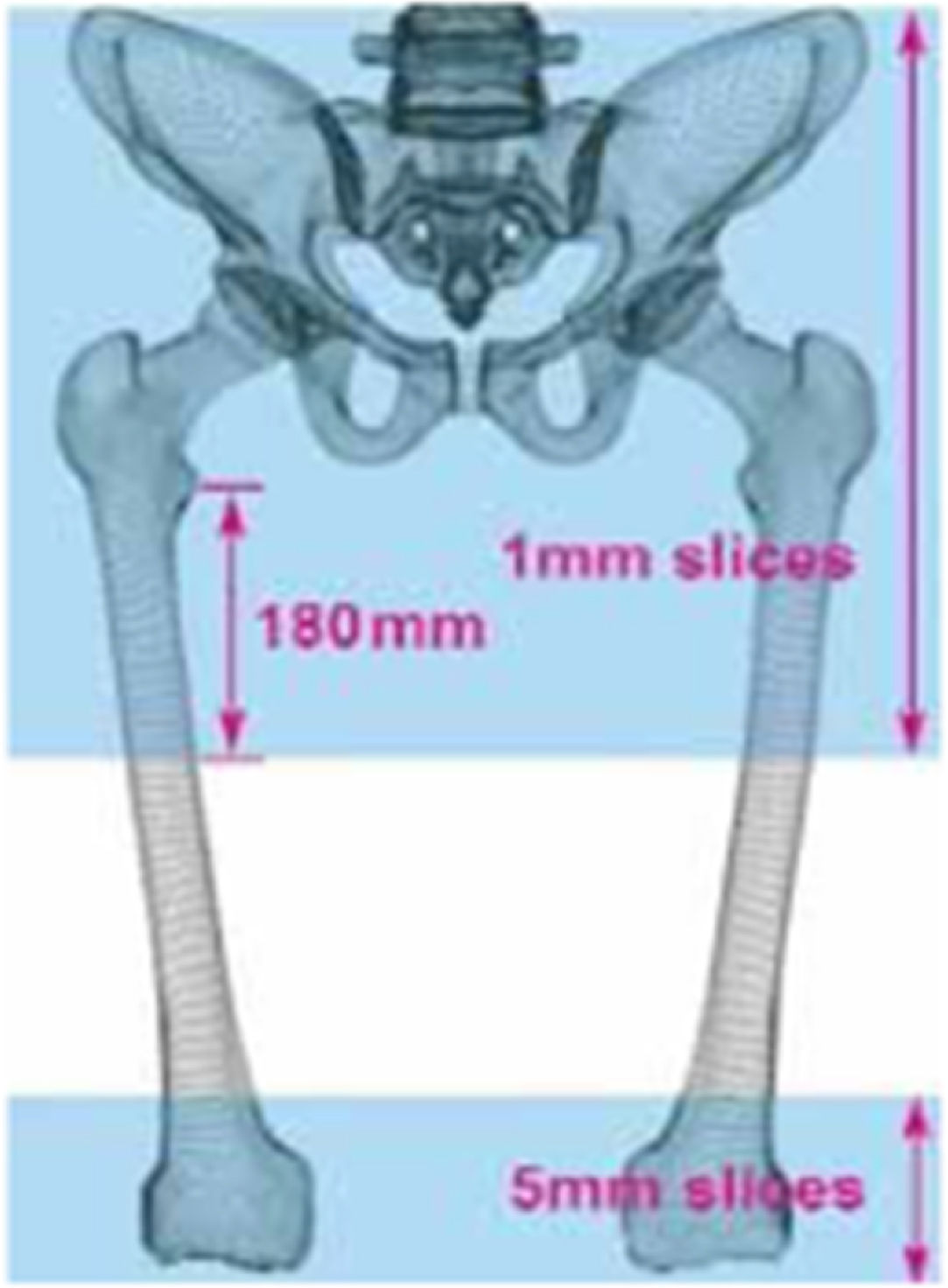
The preoperative CT scan serves as the basis for the Mako® 3.0 (Stryker) software for the design of the surgical plan, which calculates the dysmetry of both hips, the preoperative femoral offset, and femoral version. For this purpose, a continuous CT scan of two regions is performed: (1) the entire pelvis, including 180mm of the proximal femur distal to the lesser trochanters, and (2) the distal femur, including the epicondyles, which is necessary to calculate the femoral version (Fig. 1).
In addition to the evaluation of the dysmetry between both hips (previously described), the total impact of the intervention on the length of the lower limbs was studied, taking into account not only hip dysmetry, but also the possibility of dysmetries at other levels of the lower limbs (LL) which are not recorded solely on hip X-ray evaluation. Therefore, we used postoperative LL tele-XR, on which we quantified the height of the iliac crests to compare the residual complete clinical lower limb dysmetry after the operation.
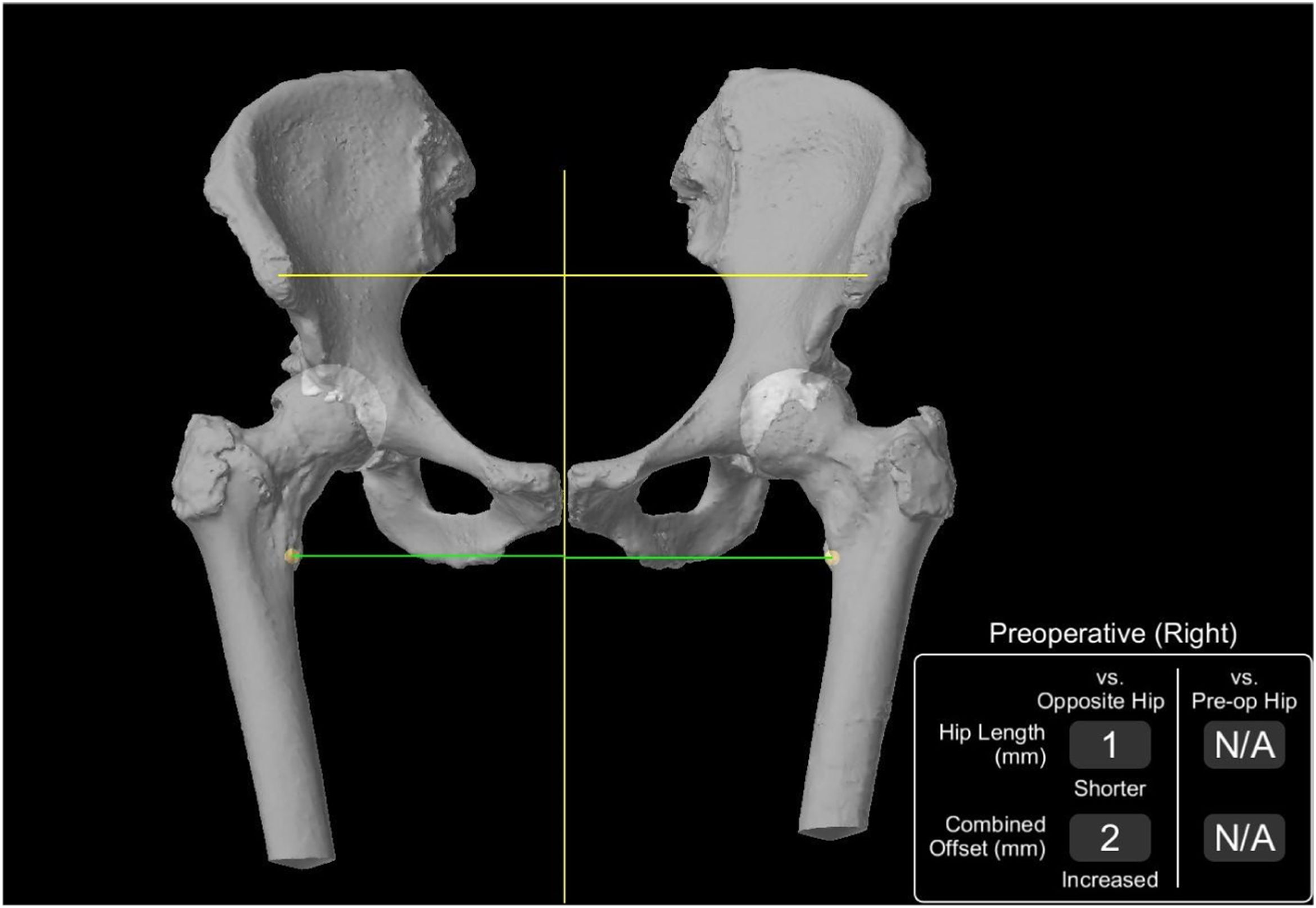
The Mako® system (Stryker) uses this CT data to create patient-specific preoperative planning that facilitates appropriate component size selection and precise intraoperative positioning of the stem and cup. Furthermore, 3D models of the patient's pelvis and knees provide information on the native anatomy, including pelvic tilt, hip joint length, and combined hip offset. The Mako® (Stryker) system enables us to compare this data before and after surgery, as well as with the contralateral hip (Fig. 2).
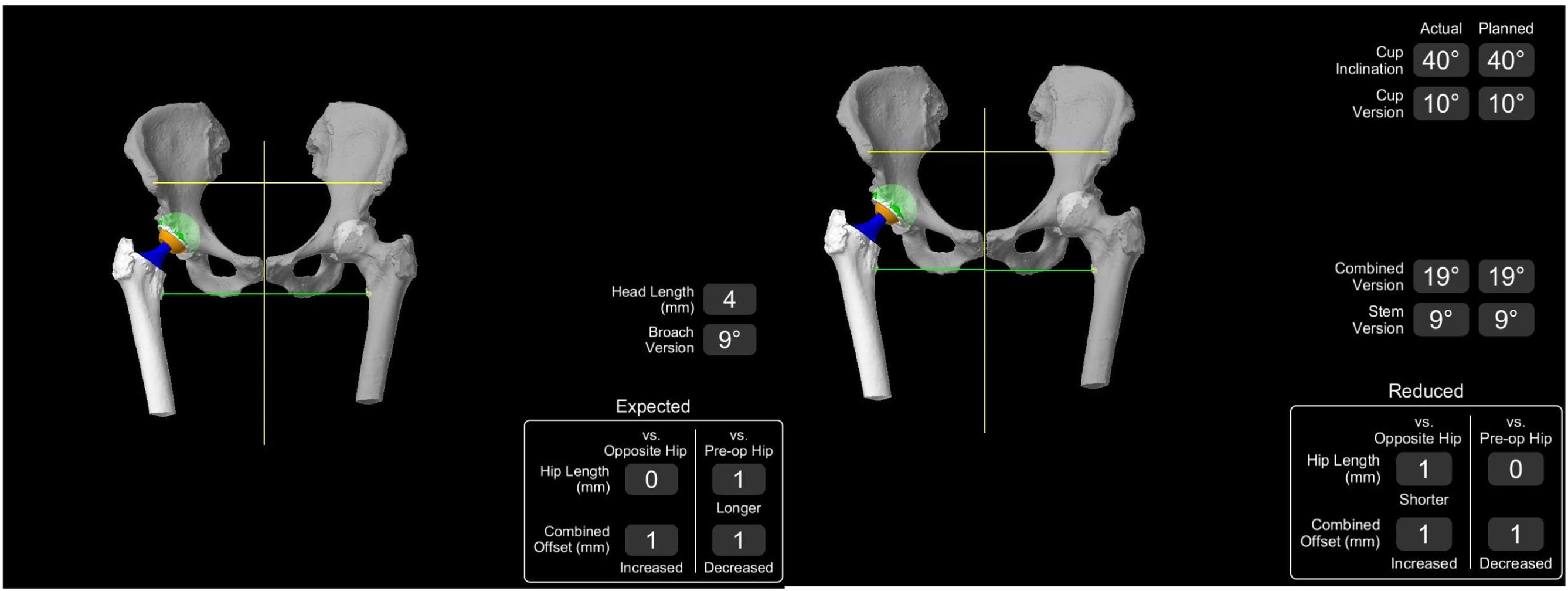
Once the implants have been individually selected in the surgical plan, data are obtained regarding the femoral version of the implant, tilt angles and acetabular anteversion, dysmetry between the two hips, and post-surgical offset, which will later be verified following implantation during surgery (Fig. 3).
The postoperative CT scan is assessed by a radiologist from the radio diagnostic service of our hospital specialised in musculoskeletal imaging and the tilt angle and acetabular anteversion are analysed, in addition to the proper implantation of the femoral stem.
The subject's level of functionality was recorded by means of the modified Harris Hip Score (mHHS) adapted to Spanish,17 in the preoperative consultation and 4 months postoperatively, as well as the patient's degree of satisfaction with the operation, rated as very satisfied, satisfied, not very satisfied, or very dissatisfied.
As for the perioperative clinical data, we quantified the days of hospital stay, the patients’ discharge destination, haemoglobin loss by comparing the preoperative values with those of the first postoperative analysis, possible transfusions required, and the values of the drains in those patients who required them. Complications during admission and in the first 4 months of follow-up were recorded.
Patients were assessed in the consultation room 4 weeks after surgery, 2 months and 4 months after surgery, which is the follow-up according to the usual protocol in our centre.
Surgical techniqueThe preoperative plan is made subsequent to the analysis of the preoperative scan using the Mako® 3.0 software. A second confirmatory surgical planning is elaborated on the basis of calibrated plain radiography using the usual classical technique, as described by Della Valle et al.18 Safety ranges of 40±10° acetabular tilt and 15±10° acetabular anteversion were deemed as implantation criteria, consistent with the theoretical ranges of the classical safety zones outlined by Lewinnek et al.9 to avoid prosthetic dislocation and based on the surgeons’ expertise. A final combined version based on the one proposed by Dorr et al.19 is sought from 35° (range, 20–50), adjusting for male patients from 25° to 35° and female patients from 30° to 50° according to the Mako® 3.0 software.
The surgery is performed by a single surgeon experienced in hip arthroplasty with the same assistant surgeon, in lateral decubitus, under spinal anaesthesia, and controlled hypotension. The lateral Hardinge approach is used. Two Mako markers are implanted following the technique described by the Mako® system. The first marker, the pelvic one, is placed using three pins in the iliac wing. The second marker, the femoral marker, in the lateral trochanteric region, after analysing the amount of space between the shoulder of the implant and the lateral cortex of the trochanter, adapting the direction and location of the marker without influencing the rest of the instrumentation, especially the manual preparation of the femoral canal. The usual surgical technique of the hospital for the implantation of a total hip prosthesis has not been changed, except for the addition of robotic arm assistance. The surgical technique used for the Mako®-assisted surgical technique in all cases was the advanced or enhanced workflow.
Intraoperative analysis of the femoral version of the implant, acetabulum tilt and anteversion, overall offset, combined anteversion and length difference between the two hips is carried out intraoperatively using the Mako® system.
The cases of intraoperative replanning performed by the Mako® assistant when the two surgeons do not consider the preoperative plan to be suitable are recorded. Intraoperative times and complications are analysed, as well as their solutions.
Statistical analysisStatistical analysis was performed with IBM SPSS software (version 26; IBM, Armonk, NY, USA). Qualitative variables are presented with their frequency distribution and percentages and were examined using Fisher's exact test. Mean, standard deviations, and ranges are presented for continuous variables, which were analysed using Student's t-test. Continuous variable data that did not display normal distribution are expressed with the median and interquartile ranges (IQR), and with the Mann–Whitney U test for the analysis of statistical significance of these variables. We considered values of p<0.05 as significant.
ResultsThe non-randomised, prospective, descriptive study consisted of 25 patients who underwent surgery in our hospital between June and September 2021 and with follow-up of 4 months; no losses were recorded during this period.
Epidemiological resultsThe mean age was 67.2 years, with a minimum of 47 and a maximum of 88 years; 56% were male. The mean age of the male group was 63.9±10.2, while the mean age of the female group was 72.9±10.6 years. Laterality was very similar in the sample, with 52% of the hips treated being on the right.
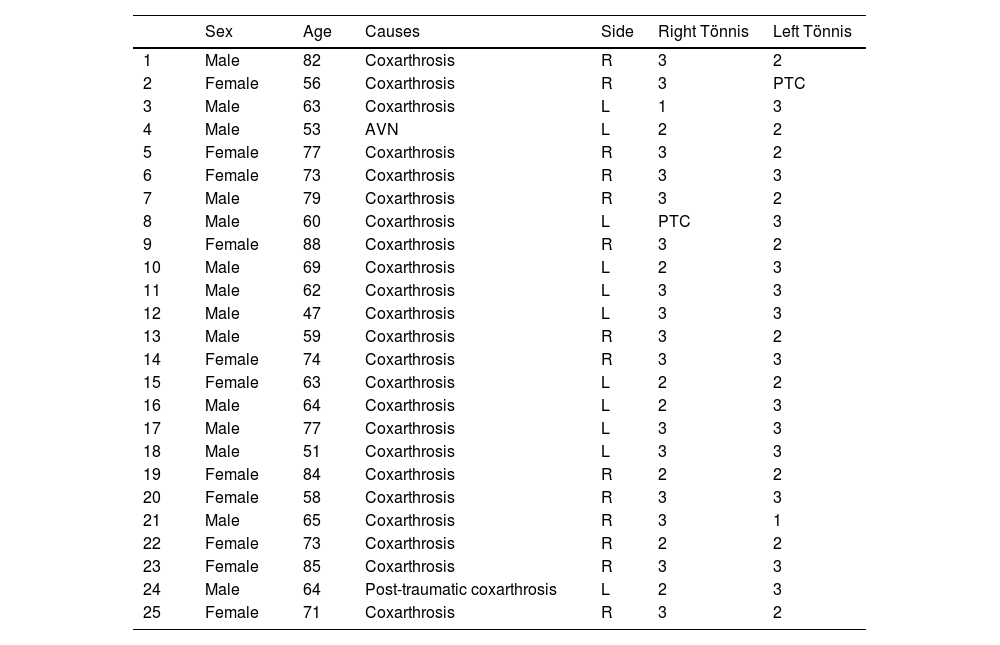
As for the preoperative diagnosis, 88% (22 cases) correspond to primary coxarthrosis, 4% to post-traumatic coxarthrosis, 4% to secondary to AVN and 4% secondary to femoral-acetabular impingement. The series displayed a predominance of Grade 3 coxarthrosis as per the Tönnis radiographic scale, present in 88% of the cases, and 12% of the sample exhibited grade 2 (Table 1).
Demographic data of the patients under study.
| Sex | Age | Causes | Side | Right Tönnis | Left Tönnis | |
|---|---|---|---|---|---|---|
| 1 | Male | 82 | Coxarthrosis | R | 3 | 2 |
| 2 | Female | 56 | Coxarthrosis | R | 3 | PTC |
| 3 | Male | 63 | Coxarthrosis | L | 1 | 3 |
| 4 | Male | 53 | AVN | L | 2 | 2 |
| 5 | Female | 77 | Coxarthrosis | R | 3 | 2 |
| 6 | Female | 73 | Coxarthrosis | R | 3 | 3 |
| 7 | Male | 79 | Coxarthrosis | R | 3 | 2 |
| 8 | Male | 60 | Coxarthrosis | L | PTC | 3 |
| 9 | Female | 88 | Coxarthrosis | R | 3 | 2 |
| 10 | Male | 69 | Coxarthrosis | L | 2 | 3 |
| 11 | Male | 62 | Coxarthrosis | L | 3 | 3 |
| 12 | Male | 47 | Coxarthrosis | L | 3 | 3 |
| 13 | Male | 59 | Coxarthrosis | R | 3 | 2 |
| 14 | Female | 74 | Coxarthrosis | R | 3 | 3 |
| 15 | Female | 63 | Coxarthrosis | L | 2 | 2 |
| 16 | Male | 64 | Coxarthrosis | L | 2 | 3 |
| 17 | Male | 77 | Coxarthrosis | L | 3 | 3 |
| 18 | Male | 51 | Coxarthrosis | L | 3 | 3 |
| 19 | Female | 84 | Coxarthrosis | R | 2 | 2 |
| 20 | Female | 58 | Coxarthrosis | R | 3 | 3 |
| 21 | Male | 65 | Coxarthrosis | R | 3 | 1 |
| 22 | Female | 73 | Coxarthrosis | R | 2 | 2 |
| 23 | Female | 85 | Coxarthrosis | R | 3 | 3 |
| 24 | Male | 64 | Post-traumatic coxarthrosis | L | 2 | 3 |
| 25 | Female | 71 | Coxarthrosis | R | 3 | 2 |
All surgeries were performed by the same surgical team, always with the same main surgeon, with the same first assistant. The advanced or enhanced Mako® assisted surgical workflow technique in all cases.
Mean surgery time was 116.9min (min 92, max 150). The mean time for the first five operations was 122.6min, as opposed to 108.2min for the last five operations, with a decrease of 14.4min, albeit lacking statistical significance (p=0.38).
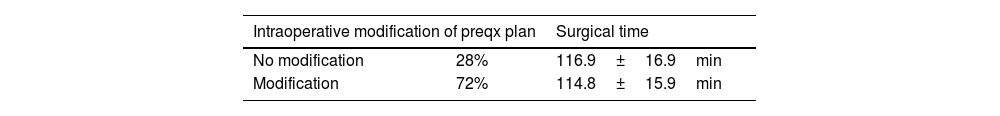
The preoperative plan carried out by the Mako® 3.0 software was supervised at all times by the two surgeons. In our series, preoperative planning was maintained during the procedure in only 28% of cases. In the remaining 72% of the cases, it was modified intraoperatively under the supervision of both surgeons. The acetabular component matched the exact size in 96% (24 out of 25) of the cases and +1 size in the remaining 4%. For the femoral component, the planned size was implanted in 60% (15 of 25). The size varied only ±1 size from the original size in the remaining cases. Fifty-six percent (14 of 25) of patients had an exact correlation between the femoral neck length chosen during planning and the one implanted at surgery.
All these new intraoperative planning procedures were performed by the Mako® assistant under the supervision of both surgeons, without increasing the preoperative time. In those surgeries in which the initial plan was modified, the mean time was 116.9±16.9, while in those in which it was not modified, it was 114.8±15.9 (p=0.99) (Table 2).
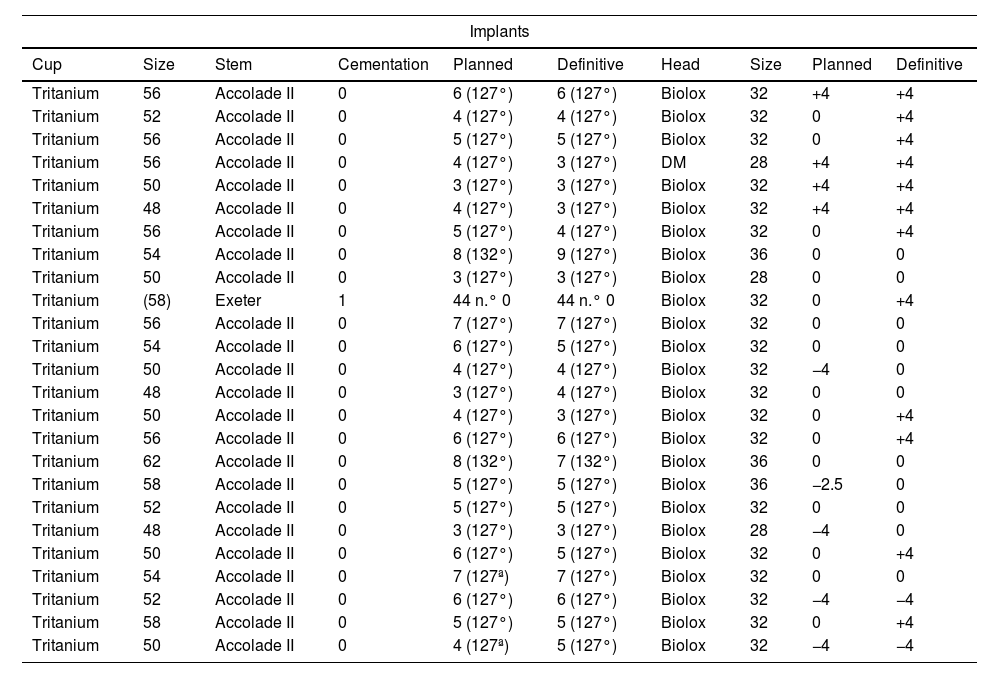
All the implanted acetabular components were the cementless Tritanium (Stryker) model cups secured with two posterosuperior screws. All the implanted femoral stems were the cementless Accolade II model (Stryker) except for one case, in which a cemented Exeter model (Stryker) stem was used due to the patient's anatomy, this being the most suitable implant for its proper implantation. The most commonly used acetabular component sizes were 50mm (24%) and 56mm (24%), while the most frequently used stem sizes were 5mm (28%) and 3mm (24%), with a cervical-diaphyseal angle of 127° in 95.7% of the cases. In all cases, the insert used was PET with an antiluxation brow (following the usual component implantation protocol in our unit), and the head component was Biolox ceramic. It is worth noting that 32mm heads were used in 69.6% of the patients. The femoral neck length was +4mm in 48% (12 cases), 0mm in 44% (11 cases), and −4mm in cases 2 (Table 3).
Planned implants and definitive implants.
| Implants | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cup | Size | Stem | Cementation | Planned | Definitive | Head | Size | Planned | Definitive |
| Tritanium | 56 | Accolade II | 0 | 6 (127°) | 6 (127°) | Biolox | 32 | +4 | +4 |
| Tritanium | 52 | Accolade II | 0 | 4 (127°) | 4 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 56 | Accolade II | 0 | 5 (127°) | 5 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 56 | Accolade II | 0 | 4 (127°) | 3 (127°) | DM | 28 | +4 | +4 |
| Tritanium | 50 | Accolade II | 0 | 3 (127°) | 3 (127°) | Biolox | 32 | +4 | +4 |
| Tritanium | 48 | Accolade II | 0 | 4 (127°) | 3 (127°) | Biolox | 32 | +4 | +4 |
| Tritanium | 56 | Accolade II | 0 | 5 (127°) | 4 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 54 | Accolade II | 0 | 8 (132°) | 9 (127°) | Biolox | 36 | 0 | 0 |
| Tritanium | 50 | Accolade II | 0 | 3 (127°) | 3 (127°) | Biolox | 28 | 0 | 0 |
| Tritanium | (58) | Exeter | 1 | 44 n.° 0 | 44 n.° 0 | Biolox | 32 | 0 | +4 |
| Tritanium | 56 | Accolade II | 0 | 7 (127°) | 7 (127°) | Biolox | 32 | 0 | 0 |
| Tritanium | 54 | Accolade II | 0 | 6 (127°) | 5 (127°) | Biolox | 32 | 0 | 0 |
| Tritanium | 50 | Accolade II | 0 | 4 (127°) | 4 (127°) | Biolox | 32 | −4 | 0 |
| Tritanium | 48 | Accolade II | 0 | 3 (127°) | 4 (127°) | Biolox | 32 | 0 | 0 |
| Tritanium | 50 | Accolade II | 0 | 4 (127°) | 3 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 56 | Accolade II | 0 | 6 (127°) | 6 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 62 | Accolade II | 0 | 8 (132°) | 7 (132°) | Biolox | 36 | 0 | 0 |
| Tritanium | 58 | Accolade II | 0 | 5 (127°) | 5 (127°) | Biolox | 36 | −2.5 | 0 |
| Tritanium | 52 | Accolade II | 0 | 5 (127°) | 5 (127°) | Biolox | 32 | 0 | 0 |
| Tritanium | 48 | Accolade II | 0 | 3 (127°) | 3 (127°) | Biolox | 28 | −4 | 0 |
| Tritanium | 50 | Accolade II | 0 | 6 (127°) | 5 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 54 | Accolade II | 0 | 7 (127ª) | 7 (127°) | Biolox | 32 | 0 | 0 |
| Tritanium | 52 | Accolade II | 0 | 6 (127°) | 6 (127°) | Biolox | 32 | −4 | −4 |
| Tritanium | 58 | Accolade II | 0 | 5 (127°) | 5 (127°) | Biolox | 32 | 0 | +4 |
| Tritanium | 50 | Accolade II | 0 | 4 (127ª) | 5 (127°) | Biolox | 32 | −4 | −4 |
Concerning intraoperative complications, four intraoperative markers were lost (16% of cases). Of them, three were femoral markers and one was an acetabular marker. The markers were lost because of possible placement errors, in connection with the surgeons’ learning curve, as well as in the technical handling to incorporate them into the surgical technique, with 2 cases of loss due to improper manipulation by the surgeons. It should be mentioned that these four marker losses took place in the first 10 patients, with no record of loss in the 15 subsequent cases.
One intraoperative fracture was also recorded, corresponding to a case of loss of femoral marker, incomplete AG1, without affecting the stability of the implant, which required reinforcement suturing with Ethibond.5
Hospital follow-up outcomesThe mean stay on the hospital ward was 4.4 days (min. 3 and max. 7), with a discharge destination to home for all subjects except for one individual who required a short-term stay facility because of lack of social support.
A mean post-surgical haemoglobin decrease of 3.08±1.08g/dl was recorded, requiring transfusion in 12% of the cases and a single transfusion of two units of RBC concentrates was necessary in all cases. The mean patient age of those who required transfusion of packed red blood cells was 74.5±6.6 years, while those who did not need transfusion had a mean age of 66.6±11.5 years (p=0.20). Transfused patients had preoperative haemoglobin levels of 13.5±1.3g/dl versus 14.0±1.2g/dl in non-transfused patients (p=0.04), underscoring the importance of good preoperative medical planning.
Postoperative intra-articular drainage was necessary in three cases (12% of the patients); one, owing to anticoagulated AF, which contraindicated the use of tranexamic acid, whereas in the other two cases, it was indicated by the surgeons on the basis of intraoperative criteria. Drainage was maintained for a maximum of 48h, with a mean drainage output of 210cc.
Three medical complications arose during hospitalisation, most notably a confusional syndrome with a fall and a non-displaced AG1 periprosthetic fracture. The other two involved a hydroelectrolyte imbalance and one case of post-surgical paralytic ileus, which were successfully resolved with the collaboration of the internal medicine department of our centre.
Functional outcomes at follow-up appointmentThe minimum follow-up was 4 months at check-ups, with consultations at 4 weeks following hospital discharge and again at 2 and 4 months postoperatively, with clinical, radiological, and functional monitoring.
No postoperative complications were detected in the first 4 months following surgery, except for the non-displaced AG1 periprosthetic fracture that occurred during in-patient stay in the context of a confusional syndrome that included a fall, without requiring further treatment.
The preoperative modified Harris score was 41.6±13.3, improving to postoperative values of 74.6±9.7at 4 months. The patient-reported satisfaction index regarding the surgical intervention (rated as very satisfied, satisfied, not very satisfied, or very dissatisfied with the operation) was high (satisfied) in 100% of the patients, with 28% reporting a very high satisfaction index with the procedure.
Imaging study resultsThe preoperative CT radiographic study analysed with the Mako® system reveals a median native femoral anteversion of 3° (range −36°/17°). The preoperative difference in the length of both hips as recorded by the Mako® system was 3.8±3.9mm, with a maximum of 12mm. The difference between the offset of the operated hip and the contralateral hip was 2±7.6mm, with a maximum of 20mm. The preoperative simple AP radiograph of the pelvis and axial projection of the hip on X-ray revealed hip dysmetry values (by comparative analysis of the distance between the ischial crests and the most medial aspect of the lesser trochanter) of 3±5.5mm and a maximum of 11mm, with no differences between the Mako® and simple X-ray measurements (p=0.53).
These values allow individualised preoperative planning for each case, with the possible intraoperative modifications previously described depending on the technical criteria observed by the surgeons. The target for implant positioning are the safety ranges of 40±10° acetabular inclination and 15±10° acetabular anteversion, in accordance with the theoretical ranges of the safety zones described by Lewinnek et al. and a combined anteversion proposed by Dorr et al. of 37.67° (range, 19–50). The aim is to maintain the native offset to avoid modifying the muscular lever arm. The aim is also to eliminate residual hip dysmetry as much as possible, except in cases of significant contralateral degenerative involvement, where a post-surgical dysmetry of around 2–4mm superior in the operated hip is sought, in order to lower the contralateral hip in its subsequent replacement surgery and achieve a balance between the two.
Analysis of acetabular positioning recorded with the Mako® system showed 40.55±1.53 degrees of inclination (range 39°–44°) and 12.2±3.6 degrees of acetabular anteversion (range 7°–21°). The postoperative imaging study performed on the patients shows radiographic acetabular inclination values of 41.2°±1.7° and CT acetabular version values of 16±4.6. No significant differences were found between the acetabular value recordings (p=0.59) between the Mako® system and the post-surgical imaging study (p=0.59 abduction and p=0.09 anteversion) (Table 4). The final combined version in our series falls in the lower limits of the range described by Dorr et al. with a mean of 22.5±5.8 (min 19°, max 36°).
Hip length discrepancy varied from preoperative values of −3.91mm±3.9mm (range −12/+3mm) to 1.29mm±1.96mm following the procedure as recorded by Mako®. The variation in length of the operated hip to achieve symmetry was a mean hip length increase of 5.64±3.35mm. The single Rx study demonstrates a postoperative difference between both hips of 0.5±3.08mm, with no statistically significant difference being noted between radiographic and Mako® recordings (p=0.53) (Table 5).
When comparing the target hip length discrepancy between preoperative planning and the result on postoperative control X-ray (measuring this radiographic variation as the distance between the line of union of the ischial ridges and the most medial aspect of the lesser trochanter), we observed that in 64% of cases (16 of 25 patients) there was less than 2mm concordance with respect to the planned result; seven patients exhibited a difference of between 2mm and 5mm compared to the initial plan, and in only two cases did the difference exceed 5mm (specifically, 5 and 8mm). Thus, in our series, the accuracy of inter-hip dysmetry was 96%, assuming a difference of 5mm from the preoperative plan, or 64%, assuming a difference of 2mm from the plan.
At the postoperative follow-up visit, the height of the iliac crests was quantified by means of an AP tele-X-ray of the lower limbs to compare the overall clinical dysmetry of the residual lower limbs after the operation. A mean lower extremity dysmetry of 3.36±5.04mm was found, with a minimum value of −9mm, corresponding to two cases of intraoperative marker loss.
The native femoral offset was maintained after surgery with a pre- and post-surgical difference of the operated hip of 3.2±3.8mm, recorded with Mako® (range −4/+10mm). The pre-surgical and post-surgical offset difference measured on plain radiography was 2±7.6mm.
DiscussionThe Mako® robotic arm-assisted THA allows for greater precision and accuracy in component placement without increasing the rate of early complications. This calls for preoperative planning with CT to restore the hip centre of rotation, offset, final leg length, and proper implant placement, maximising muscle balance, stability, and implant survival.20 Preoperative planning in mTHA offers limited possibilities compared to robotic surgery. Some series report promising 5-year survival results, with higher scores on functional rating scales and an 89% lower risk of acetabular implant placement in Lewinnek's unsafe zone and a 79% lower risk of implantation in Callanan's zone compared to conventional CTA surgery.21
After studying this series, the HCSC Hip Unit implemented the Mako® 4.0 software, which incorporates an individualised analysis of the patient's spinopelvic balance. This enables us to integrate an analysis of the final joint balance based on the dynamic changes in the orientation of the acetabulum according to the patient's individual spinopelvic index into the planning.
This correlation of intraoperative versus postoperative accuracy in implants has already been proven in several studies.14,22 Kanawade et al.22 have reported a postoperative CT accuracy of 88% for tilt, 84% for anteversion, and 81.5% for the centre of rotation of the cup compared to the planned and intraoperatively observed values in subjects who underwent surgery with robotic instrumentation.
The analysis of acetabular positioning recorded in our series with the Mako® system was 40.55±1.53 degrees of inclination and 12.2±3.6 degrees of acetabular anteversion, achieving the objective of implant positioning within the safety ranges described by Lewinnek et al.9 in all patients, and a combined anteversion in our series located in the lower limits of the range described by Dorr et al.,19 with a mean of 22.5±5.8 (min 19°, max 36°). In the analysis of planned acetabular positioning, within the theoretical safety model of Lewinek and Dorr, we found that all our patients (25/25) had implants within the range, demonstrating the maximal accuracy of the technique. We did not find a single case outside the planned range with a margin of ±4°, thereby ensuring that the reproducibility of the result was also optimal and, therefore, maximally accurate.
Our series presents a mean lengthening of 5.64±3.35mm with the aim of achieving minimal postoperative dysmetry, with mean postoperative hip dysmetry values of 1.29±1.96mm recorded by the Mako® system. It should be noted that in cases of contralateral degenerative involvement, the authors of the current study preferred to aim for a postoperative dysmetry of approximately 2–4mm higher in the operated hip, in order to lower the contralateral hip in its subsequent replacement surgery and to achieve good balance between the two.
When comparing the target hip length discrepancy between preoperative planning and the result on postoperative control X-ray (measuring this radiographic variation as the distance between the line of union of the ischial crests and the most medial aspect of the lesser trochanter), we have observed that in 64% of the cases (16 of 25 patients), there was a concordance of less than 2mm with respect to the planned result, with 7 patients displaying a difference of between 2 and 5mm with respect to the initial plan, and only 2 cases, of more than 5mm (namely 5 and 8mm). This indicates a 64% accuracy of the technique for hip dysmetry with respect to plan, with an error of 2mm and 95% accuracy if we consider a margin of error of 5mm in the final result compared to plan.
In 2019, Kayani et al.23 compared postoperative implant accuracy between patients undergoing manual and robotic-assisted surgery. Accuracy was statistically significantly greater (p=0.001) in the robotics group for tilt, anteversion, and centre of rotation, as well as for placement within Lewinnek's (p=0.02) and Callanan's (p=0.01) safety zones compared to the manual group. Work and reviews of robotic THA have corroborated the accuracy of intraoperative planning with postoperative implant measurements, placing it above the traditional technique,11,14,22 in which up to 50% of implants may fall outside the Lewinnek safety zones.10,24,25
In our series, the native femoral offset was maintained after surgery with a pre- and post-surgical difference of 3.2±3.8mm for the operated hip, recorded with Mako® (range −4/+10mm). The benefits of restoring femoral offset during total hip arthroplasty should be to reduce wear of weight-bearing surfaces, as well as implant loosening and dislocation rates; therefore, we have sought to modify the native offset as little as possible in our series.26 Some studies have highlighted the importance of both centre of rotation and offset on postoperative outcomes. Differences of >5mm in the centre of rotation with respect to its anatomical position are associated with increased rates of polyethylene loosening and wear.27 Offset impacts gait and stability, and decreasing it is associated with impaired mobility and limping.28 Mahmood et al.29 published a review of 222 total hip replacement patients in 2016; in the group of patients with an offset reduction of >5mm, statistically significantly worse functional, gait, and hip abduction mechanism outcomes were observed. Rösler and Perka30 also reported gait disturbances when the centre of rotation was mobilised cranially, while walking was seen to be unaffected with horizontal changes in the centre of rotation or limb length discrepancy of less than 1cm. Our series presents a mean offset variation of 3.2mm, within the safe range according to earlier publications.
In their series, Li et al.31 assessed the improvement of rTHA in relation to restoring lower limb length. There was no significant difference in postoperative leg length discrepancy between the conventional and robotic groups (p=0.445), although 23% of the cases in the conventional group had a leg length discrepancy in excess of 5mm, compared to 9.7% in the robotic surgery group, thus concluding that there is a benefit in lower limb length restoration by robotic-assisted surgery. Similarly, Emara et al.,11 in their meta-analysis comparing robotic and conventional arthroplasty, indicated a smaller difference in both offset and postoperative length discrepancy with the planned and contralateral native hip in favour of the robotic group.
In 72% of our cohort, the advantage of Mako® intraoperative re-planning enabled us to improve the accuracy of implant placement and the final result when patient characteristics precluded the preoperative plan from being executed. These intraoperative modifications were made with the aim of achieving the values proposed in the preoperative plan in cases in which the surgery did not progress in such a way as to enable the surgeons to redesign the preoperative plan intraoperatively without incurring additional surgical time. In all the cases included in our series, the variation was ±1 size with respect to the planned size when a change was introduced during surgery. One of the advantages of the Mako® system is the capacity for intraoperative replanning of the final values of positioning, offset, and dysmetry, by modifying the implant sizes.
In our series, the surgeries were all performed by the same surgical team, always with the same main surgeon and the same first assistant, with a 14-min reduction in surgical time from the first five patients relative to the last five cases. The mean operative time in our series was 116.9min (min 92, max 150). The mean surgical time to perform a conventional hip arthroplasty is between 50 and 120min in most series32,33 and is longer when the anterior approach is used.34,35 The mean time for the first five procedures was 122.6min, as opposed to 108.2min for the last five procedures. Published works of robotic hip arthroplasty reveal decreased operative time as a function of the learning curve after the first 12–14 cases,11,23,36,37 with the mean surgical time dropping from 123min to a mean of between 50 and 90min in the last patients operated on in these series. It should be noted that the advanced or enhanced workflow was used in all cases in our series. This modality of work makes it possible to improve the measurements of the femoral version, the height of the cervical cut, and the final length in a more accurate way, with a slight increase in surgical time. It is important to keep the surgical time within this range, as longer surgeries have been shown to increase postoperative complications.38
Regarding complications during surgery, we highlight four intraoperative marker losses, similar to the series by Kong et al.,36 in which they report technical errors during the learning curve: loss of registries, repetitive reaming, and difficult cup implantation. As in the Kong et al.36 series, our initial technical errors account for the outliers in operative time, which were not recorded after the first ten cases, with a consequent improvement in surgical times.36
The occurrence of an intraoperative femoral AG1 fracture is in line with previous published series. In the series by Perets et al.,39 1.9% fractures of the greater trochanter and 1.9% fractures of the calcar were recorded. All fractures were diagnosed and treated intraoperatively using standard procedures. Semi-active systems (such as Mako®) have the ultimate control of the surgeon, so complication rates related to intraoperative fractures and soft tissue injury are low, as reflected in the systematic review and meta-analysis by Ahmed K. Emara et al.11 on robotic arm-assisted hip arthroplasty versus manual surgery in 2021. Other large published series, such as that of Schwartz et al.,40 which included 1318 patients who underwent conventional total hip arthroplasty, recorded 39 intraoperative fractures (3%), 17 of which were proximal (12 incomplete), as was the case in our series. Our fracture involved the position of a trochanteric screw marker in a small, osteoporotic femur.
Among other advantages, advances made in robotic-assisted surgery in hip arthroplasty and the new fast-track protocols have made it possible to shorten the length of hospital stay. The 2019 study by Molko et al.41 reports a mean hospital stay in 141 Spanish hospitals of 5.7 days, 1.5 times lower than that published by the NHS (7.2 days) four years earlier. The mean length of stay in our series was 4.4 days.14,37 Despite improving on what has been published in the latest Spanish registries, this result is due to the mean age of the series, 67.2 years (min 47, max 88), with longer hospitalizations for older patients. Specifically, the mean age of the three longest-stay patients was 76.6 years, with a maximum stay in the 88-year-old patient, who required blood transfusions due to anaemia. The recent implementation of a home hospitalisation service and the decrease in the mean age of patients bring us closer to the data provided by Sawhney et al.42 in their study on the impact of navigated surgery on length of hospital stay in Canada. Their results are statistically significant in the reduction of hospital stays in patients undergoing navigated total hip arthroplasty (2.7 days/2020) compared to those undergoing non-navigated surgery (4.8 days/2017–2018).
Transfusion of blood products predisposes to a greater risk of cardiopulmonary events, transfusion reactions, increased risk of infection (allogeneic transfusions), and costs, while being one of the main limiting factors in hospital stay. In our series, all but one of the subjects (anticoagulated AF) received tranexamic acid intraoperatively. A postoperative haemoglobin decrease of 3.08±1.08g/dl was recorded, with a mean of 11.68g/dl at 24h following surgery. Our results are consistent with those previously published by Yong-Cheol Lee et al.,43 who put blood loss after tranexamic acid use in total hip arthroplasty at 24h at 10.9g/dl Hb. Three patients in our series required blood transfusion (12% of the total) within the first 48h following surgery, data that are very much in line with the series reported by Vijay et al.,44 16%, by Malhotra et al.,45 24%, and by Niskanen et al.,46 17% and 26%, respectively.
In the immediate postoperative period, a non-displaced AG1 periprosthetic fracture has been reported in the context of a confusional syndrome involving a fall during admission that did not require surgical treatment.
Functional assessment was performed 4 months after surgery using the modified Harris scale adapted to Spanish.17 Kızkapan et al.,47 in their work on the correlation between the HHS, mHHS, and Oxford Hip Score (OHS), conclude that there is a very strong correlation (p=0.0000) between the HHS and mHHS, which can be used interchangeably in the various studies, with the advantage that the mHHS only examines the patient's functionality and not the deformity and range of motion. In our series, the preoperative mHHS score was 41.6±13.3, improving to postoperative values of 74.6±9.7 at 4 months and exhibiting a mean improvement in the series of 33 points. Previous large published series, such as the Dutch series by Philip J. van der Wees et al.,48 enrolling 2089 patients undergoing manual THA, with a mean age similar to ours (61.4 years), the modified Harris scale score at 4 months was 78.3±14.5, in keeping with our postoperative record of 74.6±9.7.
Nathan Ng et al.11 compared functional outcomes using a meta-analysis of rTHA versus mTHA. Overall, there was a 41.3–44.1 point improvement on the HHS in the robotic-assisted group, while the improvement was 37.4–47.6 points on the HHS in the manual group. The meta-analysis of the functional outcome data showed that rTHA yielded a significantly better HHS score than mTHA in the short and medium term (difference 3.05 [95% CI: 0.46–5.64]; p=0.02). Nonetheless, other authors, such as Kong et al.36, using a retrospective cohort study comparing the experience of a single surgeon in manual total hip arthroplasty versus rTHA, found no statistically significant difference in HHS score in the immediate post-op period across the different groups studied. The new series of cases of rTHA being published Xiangpeng Kong in 202036 published HHS scores at 3–4 months of 82.64 [72–91] and 83.35 [64–93] in the different groups studied.
Our clinical and functional results at 4 months for the first 25 cases of rTHA are comparable to those of other series with similar characteristics, for both rTHA and mTHA. Given the follow-up time of our series, as in most published studies, the intention is not to assess medium- and long-term clinical outcome, implant survival, or the occurrence of late complications. There is a limitation in the assessment of the results published in the literature due to the heterogeneity of the patient samples with regard to the different robotic surgery systems used. The Mako® 3.0 version was used for this study. This software allows static measurement and planning for the position of prosthetic components. The software version 4.0, which includes dynamic measurements, has now been introduced in our hospital and makes it possible to assess the actual kinematics of the hip, taking into account spinal-pelvic mobility. This enables us to calculate the safety areas of each hip individually, theoretically improving the safety of the procedure. We are therefore limited in these first 25 patients in our series. Robotic software is evolving rapidly and is being incorporated into practice with new surgical features in a very short time, making it even more difficult to compare series of patients, even from the same hospital.
Study limitationsThis is a series of 25 patients with a follow-up time of 4 months. The first cases from our Hip Unit after implementation of the Mako® system are analysed. The study may underestimate the results due to the learning curve necessary for the use and integration of the system, but, at the same time, the prospective descriptive nature of the study enables us to analyse this curve after the incorporation of robotic-assisted surgery. The follow-up time is limited because this is a study of preliminary results, continuing over time after the publication of these data. Following the study of this series, the HCSC Hip Unit implemented the Mako® 4.0 software, which adds an individualised analysis of the patient's spinopelvic balance. This makes it possible for us to add an analysis of the final joint balance based on the dynamic changes in the orientation of the acetabulum according to the patient's individual spinopelvic index to the planning. A longer-term comparative study with the manual technique is recommended, taking into account the difficulty of inter-surgeon bias.
ConclusionsrTHA delivers great accuracy and a high degree of reproducibility in implant positioning and postoperative hip dysmetry, without increasing the complications associated with the technique. Surgical time, complications, and short-term functional outcomes are comparable to those of the conventional technique published in earlier large series. Longer follow-up studies are needed to properly evaluate the new robotic-assisted surgical systems and their impact on implant survival.
Level of evidenceLevel of evidence IV.
Conflict of interestsOne or more of the authors of this work have declared possible conflicts of interests which may include receiving direct or indirect payment, institutional support or support related with an institution pertaining to the biomedical field.