To determine outcomes after hip arthroscopy (HA) for femoroacetabular impingement (FAI) at a minimun 10-year follow up and identified risk factors for revision surgery.
MethodsRetrospective study of a prospective database of patients undergoing HA between January 2010 and December 2011. Rim chondral injuries were evaluated using the acetabular labral articular disruptions system (ALAD). Clinical and radiological data was obtained. Cumulative survival was estimated by Kaplan–Meier and a multivariate Cox proportional hazards model.
ResultsSeventy-four patients were included in the study. Mean follow-up was 132 months. There was statistically significant improvement from preoperative PROs at latest follow-up. Seventeen patients (23.9%) underwent revision surgery. Odds ratio for revision surgery was 8.08 in a patient above 40 years old, 7.57 in a patient Tönnis greater than 1, and 4.25 in a patient ALAD 2–3. Cumulative survivorship rate at 10 years was 77.8%, with a 45.4% for patients with Tönnis grade greater than 1 in front of 85.2% for patients with Tönnis grade of 1 or less (p<.001). Risk factor for revision surgery was preoperative degree of osteoarthrosis (p=.02).
ConclusionCumulative survivorship rate at 10 years was 45.4% for patients with Tönnis grade greater than 1 in front of 85.2% for patients with Tönnis grade of 1 or less (p<.001). Age, chondral injuries, and degree of osteoarthrosis would increase the risk for revision surgery.
Valorar los resultados de la artroscopia de cadera (CAC) como tratamiento del choque femoroacetabular (CFA) con un seguimiento mínimo de 10 años, y determinar las variables predictoras de reintervención quirúrgica.
Material y métodosEstudio retrospectivo de una base de datos prospectiva de pacientes intervenidos mediante CAC entre enero de 2010 y diciembre de 2011. Las lesiones del reborde acetabular se evaluaron según la clasificación acetabularlabral articular disruptions (ALAD). Se realizó una valoración clínica y radiológica. La supervivencia de la técnica quirúrgica se calculó con la prueba de Kaplan-Meier y la prueba de regresión de Cox.
ResultadosSe incluyeron en el estudio 74 pacientes con un seguimiento medio de 132 meses. La puntuación media en las escalas de valoración mejoró significativamente al final del seguimiento. Fueron reintervenidos 17 de ellos (23,9%). El odds ratio de reintervención en un sujeto mayor de 40 años fue de 8,08; en un paciente con escala Tönnis grado 2-3 fue de 7,57; y en uno con lesión cartilaginosa ALAD 2-3 fue de 4,25. La supervivencia de la CAC en el CFA a 10 años fue de 77,8%, con 45,4% en los pacientes con grado de Tönnis mayor a 1 vs. 85,2% en aquellos con grado 1 o menor (p<0,001). La variable predictora asociada a la necesidad de reintervención quirúrgica fue la degeneración articular radiológica preoperatoria (p=0,02).
ConclusionesLa supervivencia de la CAC en el tratamiento del CFA a 10 años fue de 45,4% en los pacientes con grado de Tönnis mayor a 1 vs. 85,2% en aquellos con grado 1 o menor. La edad, la lesión cartilaginosa y la degeneración articular incrementarían el riesgo de reintervención quirúrgica.
Hip arthroscopy (HA) has experienced exponential growth in the last decade as a hip-preserving surgery in Spain. Novoa-Parra et al. performed a retrospective review of the minimum data set from 1998 to 2018, with a population incidence that increased from .14 per 100,000 inhabitants in 1998 to 4.09 per 100,000 inhabitants in 2018. And with a projected increase of 156% for 2030.1
Femoroacetabular impingement (FAI) is a disease that is increasingly recognised as a cause of inguinal pain and progression towards hip osteoarthritis.2 Systematic reviews and meta-analyses of FAI treatment report that HA is the surgical technique mostly indicated for its treatment, and conclude that satisfactory results are achieved in a high percentage of patients in the short and medium term.3–5. Kyin et al., in a systematic review of 13 articles, reported satisfactory results of HA with a minimum follow-up of 5 years.6 However, in only 4 articles the minimum follow-up was 10 years.6–10 In addition to obtaining a satisfactory result, the fundamental objective of HA should be the preservation of the native hip and delaying the need for a total hip arthroscopy replacement (THA), especially in young patients. Sohatee et al.11 published a systematic review of 64 articles that included 59,430 HAs with a 9.47% conversion rate to THA. The average follow-up of the articles reviewed was 46.1 months, and in only 2 articles was it longer than 120 months.9,12 Age >40 years, sex, joint space <2mm and moderate or severe degree of joint degeneration were indicated as factors associated with a poor outcome or conversion to THA.6,12,13
The objective of this study was to evaluate the results of our first cases of FAI treated by HA with a minimum follow-up of 10 years and to determine the predictor variables of the need for surgical reintervention. The working hypothesis established that age and the degree of joint degeneration would increase the risk of surgical reintervention.
Material and methodA retrospective study of a prospective database of patients who underwent HA between January 2010 and December 2011 with a diagnosis of FAI, demographic variables, intraoperative findings, clinical and radiological assessment and minimum follow-up of 10 years. The study was approved by the Ethics Committee with Registration Code PI 05/2022. Informed consent was obtained from all patients. The diagnosis of FAI was based on the clinical history, physical examination, and additional tests requested.14 Patients with centre-edge angle less than de 25° or greater than 40°, previous hip surgery, and aged under 18 years were excluded.
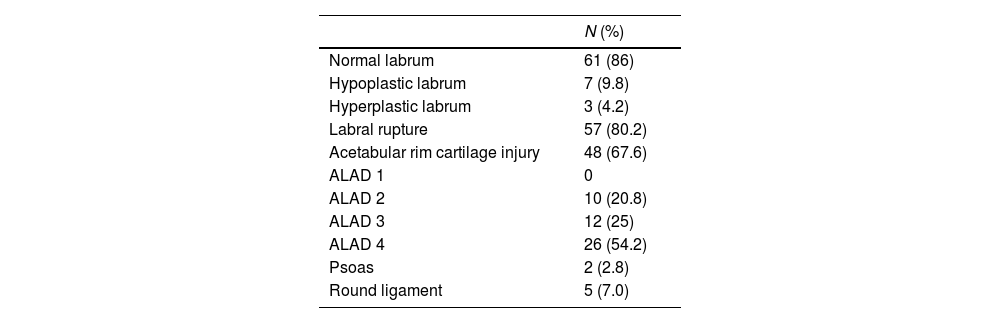
Surgical techniqueHA was performed in the supine position on a traction table with perineal protection and protection of both feet, and with spinal anaesthesia. The anterolateral, medioanterior, and distal anterolateral portals were used. The acetabular rim injuries were evaluated according to the ALAD15 classification, which distinguishes 4 stages: ALAD 1 (softening of the cartilage adjacent to the labral lesion), ALAD 2 (delamination of the adjacent cartilage without loss of continuity), ALAD 3 (extensive delamination of the adjacent cartilage with loss of continuity), ALAD 4 (complete cartilage loss with bone exposure). The size of the labrum was recorded to determine the presence of hypoplastic and hyperplastic labrum,16 as well as the presence of injury to the round ligament17 and the psoas.18 Capsular closure was not performed. Surgical time, traction time, and intraoperative complications were noted. All HAs were performed by the same surgical team.
Postoperative managementPostoperative management was similar in all patients. Discharge was indicated at 24h. Hip mobility and crutch-assisted ambulation were allowed for 4 weeks. The rehabilitation protocol was similar in all patients.19
Radiological assessmentAnteroposterior radiology of the pelvis in standing position and axial Dunn 45° was requested in all patients preoperatively and at the end of follow-up. Pincer type morphology was determined by the presence of the crossing sign and the ischial spine sign, and cam type morphology by an alpha angle greater than 60°.20 The degree of joint degeneration was recorded according to the Tönnis21 classification. Joint height was measured by recording the minimum value present in the joint space, the centre-edge angle, and the Tönnis angle on the anteroposterior radiograph of the pelvis. In the axial radiograph the alpha20 angle was measured. All measurements were performed digitally by 2 orthopaedic surgeons who had not participated in the surgeries or clinical assessments of the patients.
In all cases, preoperative non-contrast NMR was requested to detect avascular necrosis, labral lesion, or cartilage lesion.
Clinical assessmentClinical assessment was performed with the recently validated modified Harris scale (mHHS),22 the Hip Outcome Score (HOS) questionnaire with subscales for activities of daily living (HOS-ADL) and sports activities (HOS-SS),23 translated and validated24; and the International Hip Outcome Tool (iHOT-12) questionnaire.25 The patients also responded to 2 questions: how would they evaluate their function in activities of daily living and sports activities, giving a score between 0 and 100, with 100 being their level of function prior to the appearance of their hip problem and 0 being the impossibility to carry out these activities? Question number 2 was: do you consider your activity level to be normal, close to normal, abnormal, or severely abnormal? Assessments were performed at 6 months, 12 months, and annually until the end of follow-up.
Clinical significance at the end of follow-up was analysed with minimal clinically important difference (MCID), patient acceptable symptom status (PASS), and substantial clinical benefit (SCB) for mHHS, HOS-ADL, HOS-SS. and iHOT-12. Previous studies have defined MCID, SCB and PASS at 5 and 10 years of follow-up.26,27
The level of preoperative sports activity was determined according to the Tegner scale.28
Surgical reintervention by revision arthroscopy or conversion to total hip replacement was recorded. The indication for surgical reintervention was established by the presence of pain, functional limitation and progressive decrease in scores on the assessment questionnaires used.
Statistical analysisSPSS® version 20.0 (SPSS Inc., Chicago, USA) was used. P values equal to or less than .05 were considered significant. The normality of the quantitative variables was determined using the Kolmogorov–Smirnov test. For the comparison of pre- and postoperative continuous variables, the Student's t test for related samples was used; and for the comparison of qualitative variables the Chi-square test. Based on daily clinical practice and as other previous studies have reported6,12,13 the variable degree of joint degeneration and joint height was re-coded into 2 groups: Tönnis 0–1 and Tönnis 2–3, to differentiate between patients without osteoarthritis or with minimal degenerative changes and patients with moderate or severe degenerative changes. The joint height variable was also recoded into 2 groups: greater than 2mm and less than 2mm.
A univariate analysis of demographic, radiological and intraoperative variables was performed with the need for surgical reintervention. The effect size of the difference between the means with statistical significance was performed with Cohen's d test. A d value of less than .2 would indicate a small effect size, .5 an effect of medium magnitude, and greater than .8 a high magnitude effect. Odds ratios were calculated for dichotomous variables with statistical significance. Survival of the surgical technique with the need for surgical reintervention as the end point was calculated with the Kaplan–Meier and log-rank tests to compare survival between groups. Variables with clinical significance in the univariate analysis were analysed as predictor variables for the need for surgical reintervention with Cox regression.
ResultsDuring the study period 74 patients were selected. Of these, 3 patients were excluded: one due to death from heart disease and 2 due to loss to follow-up. The final study sample comprised 71 patients. The mean age of the patients was 42 years (SD: 10.7). In 57.8% (41 patients) the age was over 40 years and in 42.2% (30 patients) under 40 years. The mean BMI of the patients had a value of 25.2kg/m2 (SD: 2.9). By sex, there was a predominance of men in 84.5% (60 patients) compared to women in 15.5% (11 patients).
Intraoperative findingsThe intraoperative findings are indicated in Table 1. Labral tear was detected in 57 patients (80.2%), treated by suturing with 3-implants. Acetabular rim injury occurred in 48 patients (67.6%). Of these, in 26 patients (54.2%) there was acetabular bone exposure. In cartilage lesions, debridement was performed in ALAD grades 2–3 and microfractures in ALAD grade 4. In case of presence of round ligament injury, debridement was performed, and tenotomy was performed in the psoas tendon.
The mean surgical time was 96.5min (SD: 6.9) and the mean traction time was 57.3min (SD: 5.4).
No intraoperative complications were recorded.
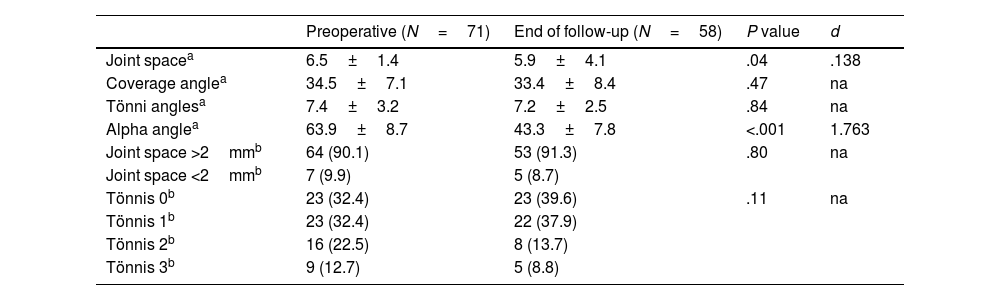
Radiological resultsCam-type morphology was present in the preoperative radiograph in 95.8% (68 patients) and Pincer-type morphology in 4.2% (3 patients). The type of FAI was Cam type in 64.7% (46 patients), Mixed type in 30.9% (22 patients) and Pincer type in 4.4% (3 patients). The mean alpha angle correction was 17.1° (SD: 1.8). At the end of follow-up, joint height decreased significantly, and in 5 patients (8.7%) it progressed to a value less than 2mm. Progression of joint degeneration was detected in 6 patients (10.3%) (Table 2). The correlation coefficient for radiological measurements was .92.
Radiological results.
| Preoperative (N=71) | End of follow-up (N=58) | P value | d | |
|---|---|---|---|---|
| Joint spacea | 6.5±1.4 | 5.9±4.1 | .04 | .138 |
| Coverage anglea | 34.5±7.1 | 33.4±8.4 | .47 | na |
| Tönni anglesa | 7.4±3.2 | 7.2±2.5 | .84 | na |
| Alpha anglea | 63.9±8.7 | 43.3±7.8 | <.001 | 1.763 |
| Joint space >2mmb | 64 (90.1) | 53 (91.3) | .80 | na |
| Joint space <2mmb | 7 (9.9) | 5 (8.7) | ||
| Tönnis 0b | 23 (32.4) | 23 (39.6) | .11 | na |
| Tönnis 1b | 23 (32.4) | 22 (37.9) | ||
| Tönnis 2b | 16 (22.5) | 8 (13.7) | ||
| Tönnis 3b | 9 (12.7) | 5 (8.8) |
d: d of Cohen; na: not applicable.
The mean preoperative sports activity level was 5.7 according to the Tegner scale (SD: 1.7).
The mean follow-up of the patients was 132±9.7 months (minimum 120, maximum 144).
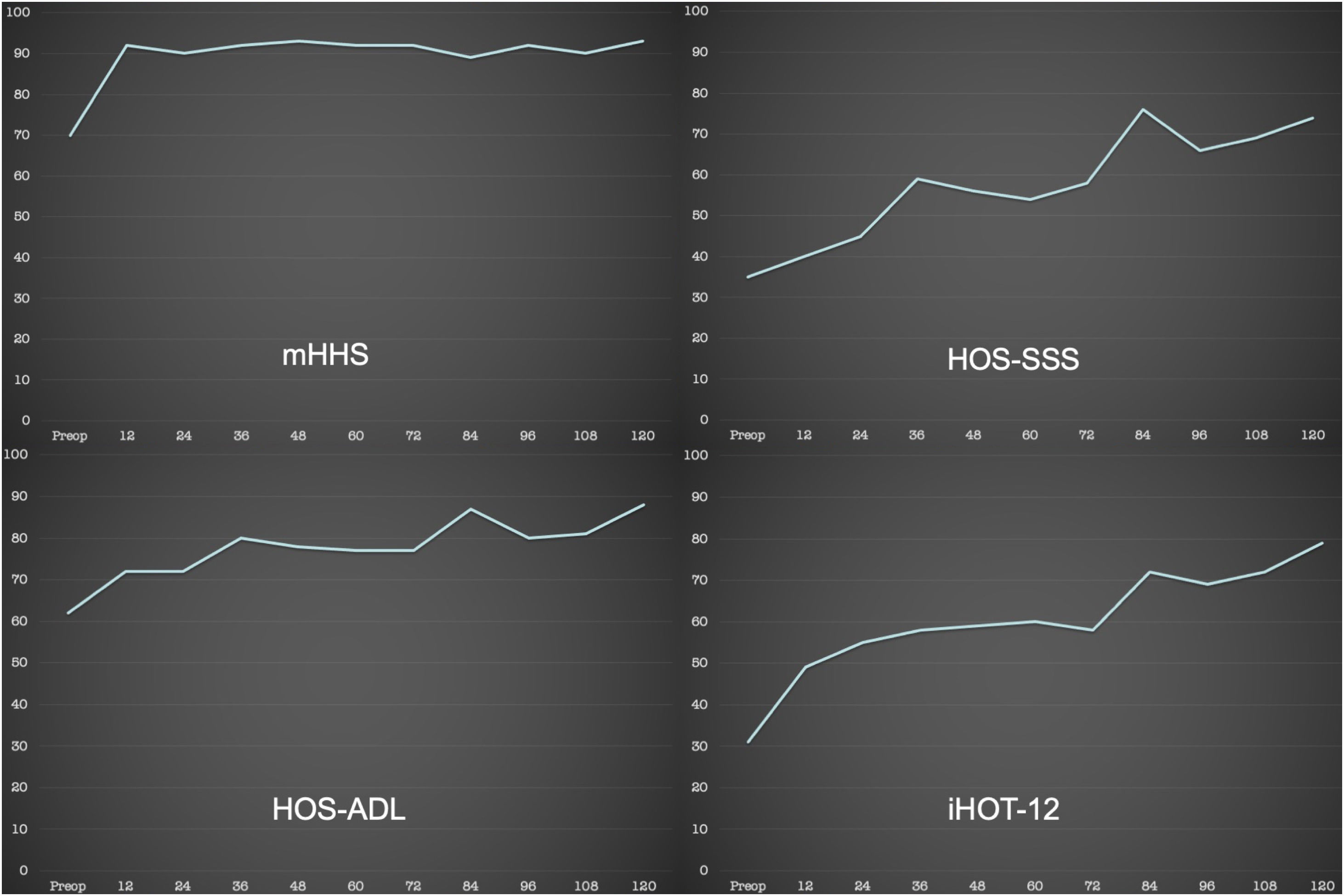
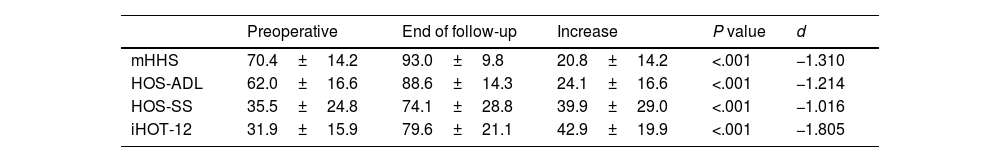
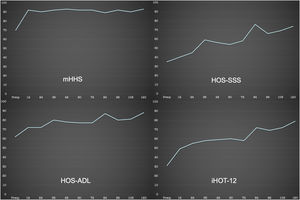
The mean score on the rating scales improved significantly at the end of follow-up (Table 3 and Fig. 1).
Functional results.
| Preoperative | End of follow-up | Increase | P value | d | |
|---|---|---|---|---|---|
| mHHS | 70.4±14.2 | 93.0±9.8 | 20.8±14.2 | <.001 | −1.310 |
| HOS-ADL | 62.0±16.6 | 88.6±14.3 | 24.1±16.6 | <.001 | −1.214 |
| HOS-SS | 35.5±24.8 | 74.1±28.8 | 39.9±29.0 | <.001 | −1.016 |
| iHOT-12 | 31.9±15.9 | 79.6±21.1 | 42.9±19.9 | <.001 | −1.805 |
d: d of Cohen; HOS-ADL: Hip Outcome Score questionnaire for activities of daily life; HOS-SS: Hip Outcome Score questionnaire for sports activities; iHOT-12: International Hip Outcome Tool questionnaire; mHHS: modified Harris score.
Mean±standard deviation.
Evolution of the assessment scales during follow-up. X-axis: tracking. Y-axis: score. HOS-ADL: Hip Outcome Score questionnaire for activities of daily living; HOS-SS: Hip Outcome Score questionnaire for sports activities; iHOT-12: International Hip Outcome Tool questionnaire; mHHS: modified Harris scale.
The patients’ evaluation of hip function on a scale of 0–100 increased in activities of daily living from 46.6 (SD: 18.6) to 89 (SD: 16.4) and in sports activities from 23.3 (SD: 15.6) to 72.7 (SD: 32.1), the differences being significant (p<.001 and p=.02, respectively).
Preoperatively, 80% of patients considered their activity level as abnormal or severely abnormal, compared to 21.9% at the end of follow-up.
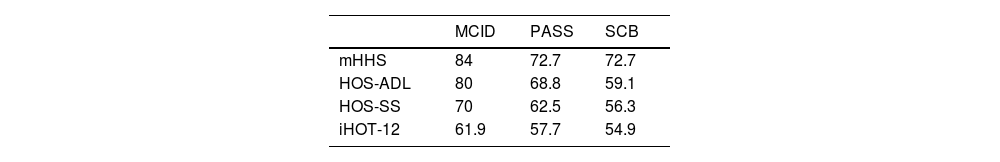
The percentage of patients who reached clinical significance for the assessment questionnaires at the end of follow-up is shown in Table 4.
Percentage of patients who met with clinical significance at the end of follow-up.
| MCID | PASS | SCB | |
|---|---|---|---|
| mHHS | 84 | 72.7 | 72.7 |
| HOS-ADL | 80 | 68.8 | 59.1 |
| HOS-SS | 70 | 62.5 | 56.3 |
| iHOT-12 | 61.9 | 57.7 | 54.9 |
HOS-ADL: Hip Outcome Score questionnaire for activities of daily life; HOS-SS: Hip Outcome Score questionnaire for sports activities; iHOT-12: International Hip Outcome Tool questionnaire; MCID: minimum clinically important difference; mHHS: modified Harris hip score; PASS: patient acceptable symptom status; SCB: substantial clinical benefit.
During the follow-up period, 17 patients (23.9%) required surgical reintervention.
Thirteen patients (18.3%) underwent reoperation by conversion to PTC with a mean time to reintervention of 63 months. The average age of the patients was 49.6 years. In preoperative radiology the average joint height was 2.8mm, in 4 of them less than 2mm; one Tönnis 1 patient, 6 Tönnis 2 patients and 6 Tönnis 3 patients.
Four patients (5.6%) underwent reoperation with revision HA with a mean time to reoperation of 39 months. The average age of the patients was 42.2 years. In preoperative radiology, the mean joint height was 4.7mm, in no patient less than 2mm; 2 Tönnis 0 patients and 2 Tönnis 1 patients. Insufficient femoral osteoplasty was detected in the revision HA. No patient required conversion to THA during follow-up.
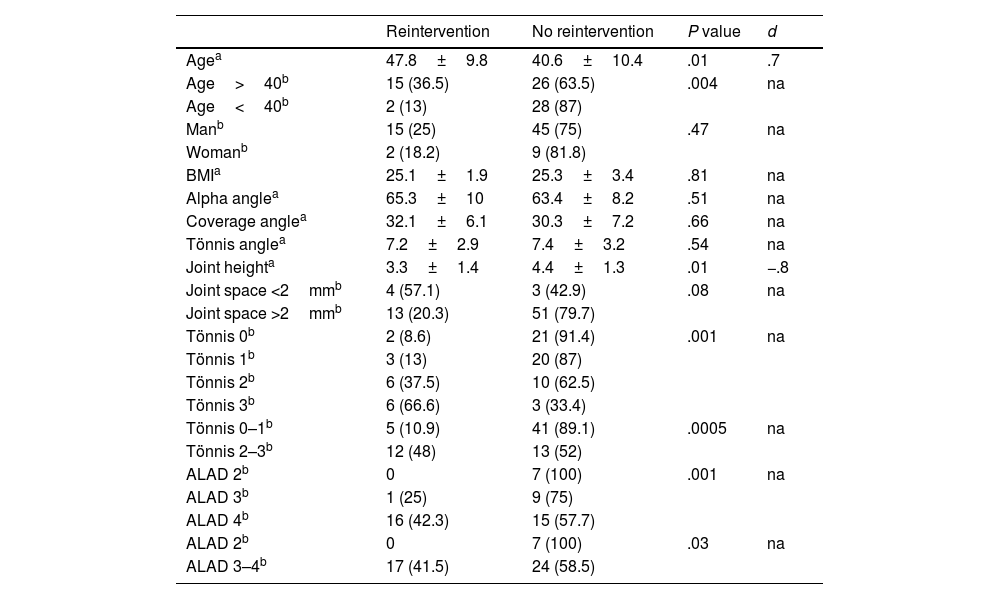
Statistically significant differences were detected between reoperated and non-reoperated patients in age, radiological degree of joint degeneration, and degree of cartilage lesion (Table 5). The odds ratio for reintervention in a patient over 40 years of age was 8.08 (95% CI: 1.68–38.79); in one patient Tönnis 2–3 of 7.57 (95% CI: 2.24–25.53); and in a patient with cartilage lesion ALAD 2–3 of 4.25 (95% CI: 0.47–38.6).
Univariate analysis between preoperative and intraoperative variables and surgical reintervention.
| Reintervention | No reintervention | P value | d | |
|---|---|---|---|---|
| Agea | 47.8±9.8 | 40.6±10.4 | .01 | .7 |
| Age>40b | 15 (36.5) | 26 (63.5) | .004 | na |
| Age<40b | 2 (13) | 28 (87) | ||
| Manb | 15 (25) | 45 (75) | .47 | na |
| Womanb | 2 (18.2) | 9 (81.8) | ||
| BMIa | 25.1±1.9 | 25.3±3.4 | .81 | na |
| Alpha anglea | 65.3±10 | 63.4±8.2 | .51 | na |
| Coverage anglea | 32.1±6.1 | 30.3±7.2 | .66 | na |
| Tönnis anglea | 7.2±2.9 | 7.4±3.2 | .54 | na |
| Joint heighta | 3.3±1.4 | 4.4±1.3 | .01 | −.8 |
| Joint space <2mmb | 4 (57.1) | 3 (42.9) | .08 | na |
| Joint space >2mmb | 13 (20.3) | 51 (79.7) | ||
| Tönnis 0b | 2 (8.6) | 21 (91.4) | .001 | na |
| Tönnis 1b | 3 (13) | 20 (87) | ||
| Tönnis 2b | 6 (37.5) | 10 (62.5) | ||
| Tönnis 3b | 6 (66.6) | 3 (33.4) | ||
| Tönnis 0–1b | 5 (10.9) | 41 (89.1) | .0005 | na |
| Tönnis 2–3b | 12 (48) | 13 (52) | ||
| ALAD 2b | 0 | 7 (100) | .001 | na |
| ALAD 3b | 1 (25) | 9 (75) | ||
| ALAD 4b | 16 (42.3) | 15 (57.7) | ||
| ALAD 2b | 0 | 7 (100) | .03 | na |
| ALAD 3–4b | 17 (41.5) | 24 (58.5) |
BMI: body mass index; d: d of Cohen; na: not applicable.
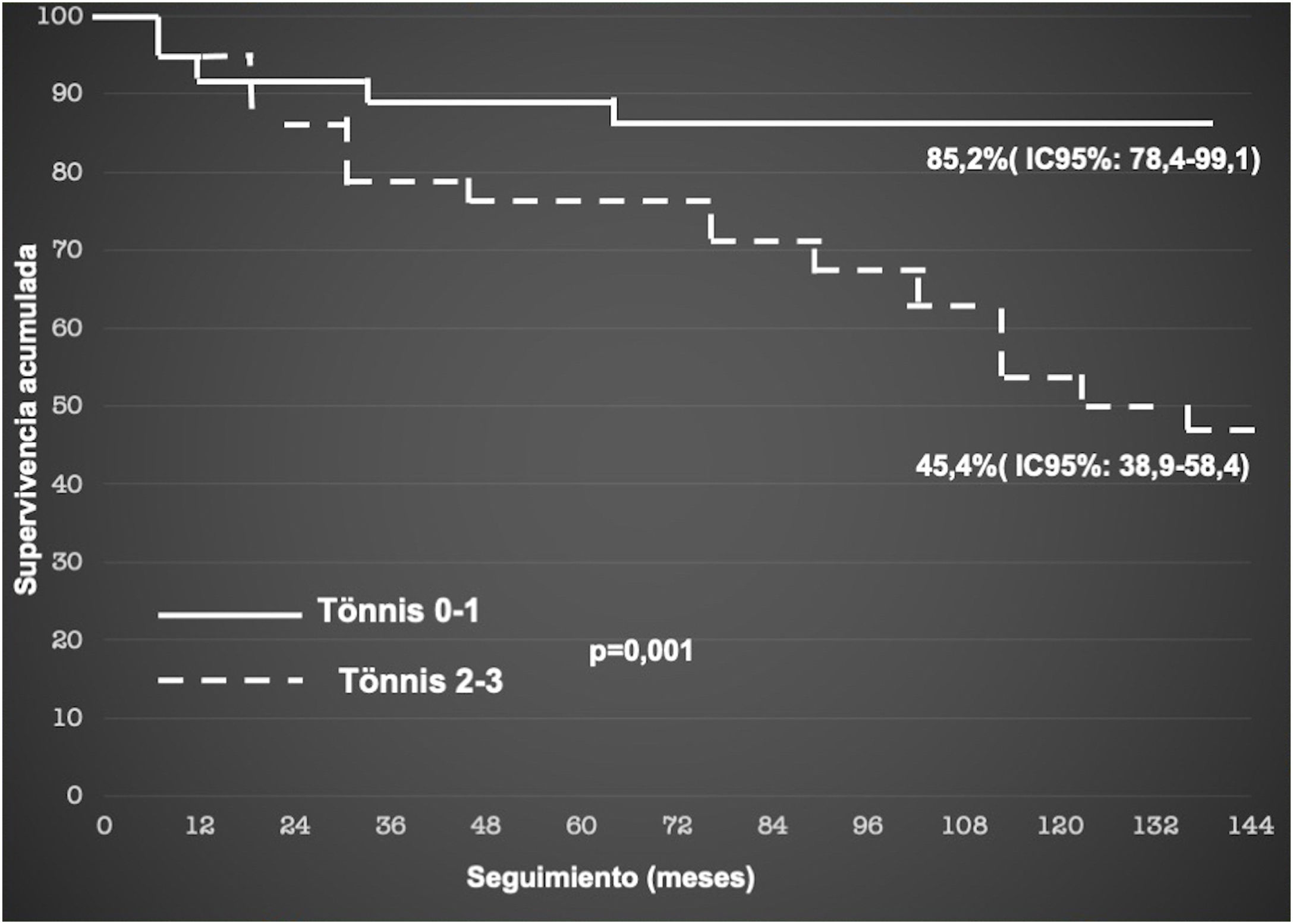
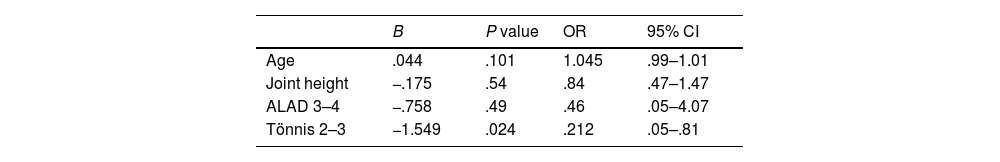
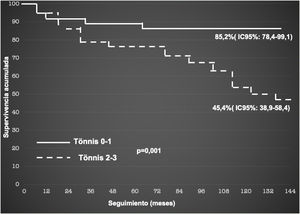
The 10-year survival of HA in FAI was 77.8% (95% CI: 61.3–94.1). The Cox regression model detected a statistically significant relationship between the preoperative radiological degree of joint degeneration according to Tönnis as an independent variable and surgical reintervention. During follow-up, Tönnis 0–1 patients presented a 78.8% reduction in the risk of surgical reintervention, compared to Tönnis 2–3 patients (Table 6). HA survival according to the degree of preoperative joint degeneration was 45.4% in Tönnis 2–3 patients versus 85.2% in Tönnis 0–1 patients (Fig. 2), the differences being significant (p=.001).
Cox regression model between variables with statistical significance in the univariate analysis.
| B | P value | OR | 95% CI | |
|---|---|---|---|---|
| Age | .044 | .101 | 1.045 | .99–1.01 |
| Joint height | −.175 | .54 | .84 | .47–1.47 |
| ALAD 3–4 | −.758 | .49 | .46 | .05–4.07 |
| Tönnis 2–3 | −1.549 | .024 | .212 | .05–.81 |
95% CI: 95% confidence interval; OR: odds ratio.
The most important finding of our study was that the presence of radiological degenerative changes negatively influences the results of HA in FAI at a minimum follow-up of 10 years. When considering surgical reintervention as the end point, HA survival was 85.2% in Tönnis 0–1 patients. However, in patients Tönnis 2–3 decreased to 45.4%.
Our results are similar to previous studies published with follow-up of more than 10 years. Zimmerer et al. report a survival of 86.3% in Tönnis 0–1 patients, compared to 46.4% in Tönnis 2–3 patients, in their series of 112 hips with 11 years of follow-up.13 Grammatopoulos et al. indicate a survival of 91% in Tönnis 0 patients, 89% in Tönnis 1 and 68.4% in Tönnis 2 in their series of 393 hips, of which 238 were operated on with HA, at 10 years of follow-up.29
Age has been another factor related to long-term HA survival. McCarthy et al., in their series of 111 hips with a 10-year follow-up, report an odds ratio of 3.6 for conversion to THA in patients over 40 years of age.12 Zimmerer et al. published that advanced age increases the risk of conversion to THA by 24%, with statistical significance in the Cox regression model.1 In our study, the odds ratio for reintervention in a patient over 40 years of age was 8.08. However, as in McCarthy's study, age as a predictor variable did not reach statistical significance in the Cox regression model.
Studies on the influence of sex on long-term HA outcome are contradictory. Zimmerer et al. report an odds ratio of 1.97 for women obtaining worse results.13 However, in the study by McCarthy et al.,12 and in ours, sex did not influence the results at the end of follow-up.
In our study, we performed labral suture in 80.2% of HAs, with an overall survival of 77.8% at 10 years of minimum follow-up. Labral debridement has been associated with poor results and the need for surgical reintervention.3,30 Zimmerer et al. performed labral debridement in all patients in their series, with an overall survival of 64.3% at 11 years of follow-up.13 Menge et al. published a comparative study between 75 hips treated by labral suture, and 75 hips treated by labral debridement, with a 10-year follow-up; without statistically significant differences in the Cox regression model between both groups with respect to surgical reintervention and clinical outcome. However, both groups presented statistically significant differences with respect to sex, type of FAI, and microfracture treatment.7
The need to perform microfractures due to the presence of a severe cartilage lesion of the acetabular rim has also been indicated as a predictor variable for surgical reintervention, if also associated with labral debridement.7,13 Consequently, chondral therapy associated with labral repair should be an objective to reduce the need for surgical reintervention and increase HA survival. Recently, Maldonado et al. report in their case-control study of patients with irreparable labral injury and severe cartilage damage, a relative risk of 4.0 of conversion to THA in patients treated with microfractures and labral debridement compared to patients treated with microfractures and reconstruction of the labrum.31 In our study, we performed microfractures in 54.2% of the hips with cartilage damage, with labral repair association in all of them.
We did not perform capsular closure in the hips of the series, similarly to that reported by Zimmerer et al.13 Owens et al. recently published a systematic review of 10 studies comparing the results between capsular closure and non-closure. In 8 of them the results were significantly better in patients with capsular closure, and in 2 no statistically significant differences were found; all studies with an average follow-up of less than 5 years. Recently, Tahoun et al. performed a comparative study between 42 patients without capsular repair and 44 patients with capsular repair with a minimum follow-up of 5 years. Functional results were better in patients with capsular repair, although there were no differences in clinical significance or in the rate of surgical reintervention.32 Given that no study without capsular closure has demonstrated superior results, the current recommendation in HA is to perform capsular closure.33
The assessment questionnaires used showed a statistically significant improvement at the end of follow-up in the patients who did not require surgical reintervention in our study, with a high magnitude effect of the mean difference. These results are comparable to previous studies published with similar follow-ups,7,8,13,29 and seem to indicate that HA in the treatment of FAI facilitates the obtaining and maintaining of satisfactory long-term results.
The percentages of surgical reintervention through revision HA are between 2% and 20.9% at 10 years of follow-up, with a mean time for performing HA between 8 and 42 months. And conversion to THA between 2.4% and 2.5%, with an average completion time between 46 and 96 months.6 The predictor variables for surgical reintervention reported in the literature have been advanced age, joint height, severe cartilage injury, and advanced joint degeneration.7,9,10,12,13,29 In our study, the percentage of revision HA was 5.6% and conversion to THA was 18.3%. Our conversion rate to THA was higher than that reported in the literature,11 possibly due to a higher percentage of patients with joint degeneration undergoing surgery. At the end of follow-up, 48% of Tönnis 2–3 patients had required conversion to THA, compared to 0% of Tönnis 0–1 patients. Although Rosinky et al. published in a systematic review that the short-term functional results in patients with HA prior to THA are similar to patients who had not previously undergone surgery, a trend is observed towards a higher incidence of complications, mainly dislocation and infection.34
Our study has the following limitations. This is a retrospective study without a control group. However, data collection has been carried out prospectively. It is a unique series with a small sample size, which may limit the generalisation of the results obtained. The questions used in the clinical assessment are not validated at the current time.
ConclusionsThe 10-year survival of HA in the treatment of FAI was 45.4% in patients with Tönnis grade greater than 1 versus 85.2% in patients with Tönnis grade 1 or less. Age, cartilage damage and joint degeneration would increase the risk of surgical reintervention.
Level of evidenceLevel of evidence IV.
FundingThe authors declare that they have received no funding for the conduct of the present research, the preparation of the article, or its publication.
Conflict of interestsThe authors have no conflict of interests to declare.
Ethics Committee approvalRegistration Code (PI 05/2022).