Preoperative planning is essential in adolescent idiopathic scoliosis (AIS) surgery to determine the fusion levels and to perform the procedure with greater precision and diligence. However, the protocolized performance of such planning is not as widespread among specialists in training. The aim of this article is to describe in detail the preoperative planning method for AIS used in a specialised paediatric and adolescent spine unit of a referral centre, as well as the logistics and the tactics, supported a free semi-automatic digital measurement and planning software. Three representative cases of different vertebral deformities, treated by posterior spinal fusion after preoperative planning according to the method, are shown. This method is highly suitable for the trainee surgeon as it combines the advantages of traditional and modern methods, and is simple, low-cost, accessible, reproducible and with an educational character.
La planificación preoperatoria resulta fundamental en la cirugía de escoliosis idiopática del adolescente (EIA) para determinar los niveles a fusionar y realizar el procedimiento con mayor precisión y diligencia. Sin embargo, su realización protocolizada no está tan extendida entre los especialistas en formación. El objetivo de este artículo es describir en detalle el método de planificación preoperatoria en la EIA empleado en una unidad especializada de raquis infantil y del adolescente de un centro de referencia, así como la logística y la táctica, apoyado en un software gratuito de medición digital semiautomática y planificación. Se muestran 3 casos representativos de diferentes deformidades vertebrales, intervenidos mediante una artrodesis vertebral posterior tras una planificación preoperatoria según el método descrito. Este método resulta muy adecuado para el cirujano en formación al aunar las ventajas de los métodos tradicionales y los más modernos, y ser sencillo, de bajo coste, accesible, reproducible y con carácter formativo.
Adequate preparation prior to surgery is the basis for optimising results and minimising complications. In spine surgery, and specifically in adolescent idiopathic scoliosis (AIS) surgery, preoperative planning is essential to assess the location and severity of the curve, shoulder asymmetry, coronal and sagittal alignment and balance, and the spinopelvic parameters that guide us in the levels to be instrumented, and in the biomechanical restoration of the spine.
Good planning reduces the risks associated with surgery by forcing the surgeon to study the patient's characteristics, history, and vertebral deformity, and to identify anatomical details and key technical points of the intervention. It also improves surgical efficiency and outcomes,1 allowing the surgery to run more smoothly, avoiding unnecessary prolongation of operative time, and minimising complications. For the specialist starting out in AIS surgery, good preoperative planning of deformity correction is a tool with the potential to manage the deformity prior to surgery, and allows essential time to understand the curve pattern and its complexity, and to consider the levels to be instrumented and the most appropriate reduction method in each case.
Posterior spinal fusion using pedicle screws and rods is currently the most accepted technique for the correction of AIS. It is traditionally planned using measurements on radiographic images. With the advancement of digital medicine, digital measurement programmes have proven faster, more accurate, and less variable than the manual technique.2–5 In recent years their use has become more widespread in routine clinical practice. Other advanced planning technologies incorporating three-dimensional reconstructions are promising tools for the future, although their use in practice is currently limited6 because they are less accessible, time-consuming, costly, technically more demanding, and impractical, and they are primarily used in research.
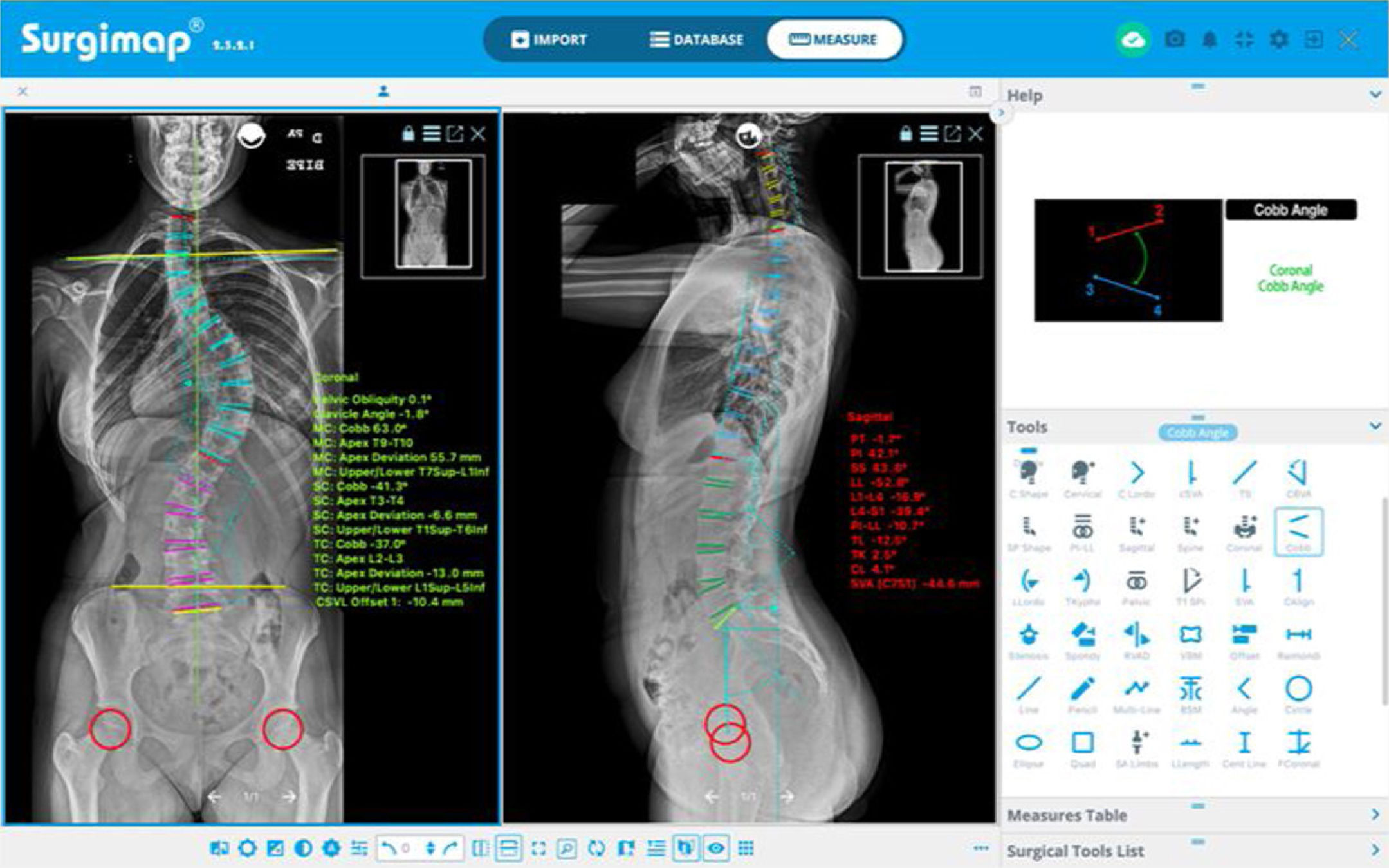
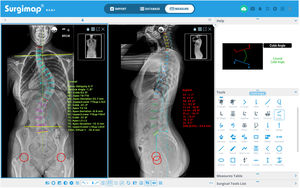
The aim of this paper is to explain in detail the preoperative planning method for AIS used in a specialised paediatric and adolescent spine unit of a referral centre, as well as the logistics and tactics, supported by a free computerised spine measurement and surgical planning software, Surgimap Spine® (Nemaris Inc, New York, USA)8 available at www.surgimap.com. It is a simple, low-cost, accessible, reproducible, relatively fast method that provides good results. All this gives it a training character that makes it ideal for incorporation into the daily practice of specialists in training in spine surgery.
Planning approachPreoperative clinical evaluation in adolescent idiopathic scoliosisWhen surgery is indicated for a patient with AIS, different clinical characteristics such as age, sex, stage of pubertal development according to Tanner stage, the patient's medical history and previous treatments for vertebral deformity are taken into account. A targeted physical examination is also performed, evaluating signs that are fundamental for preoperative classification, such as asymmetry of the shoulders and scapulae, trunk rotation with the Adam's forward bend test quantified with a scoliometer, flexibility of the curves, sagittal and coronal balance with the plumb line, pelvic obliquity, length discrepancy of the lower limbs, and neurological examination that includes cutaneo-abdominal reflexes, among others. Clinical photographs of the patient in different positions (back, profile, and anterior trunk flexion) will be useful in planning.
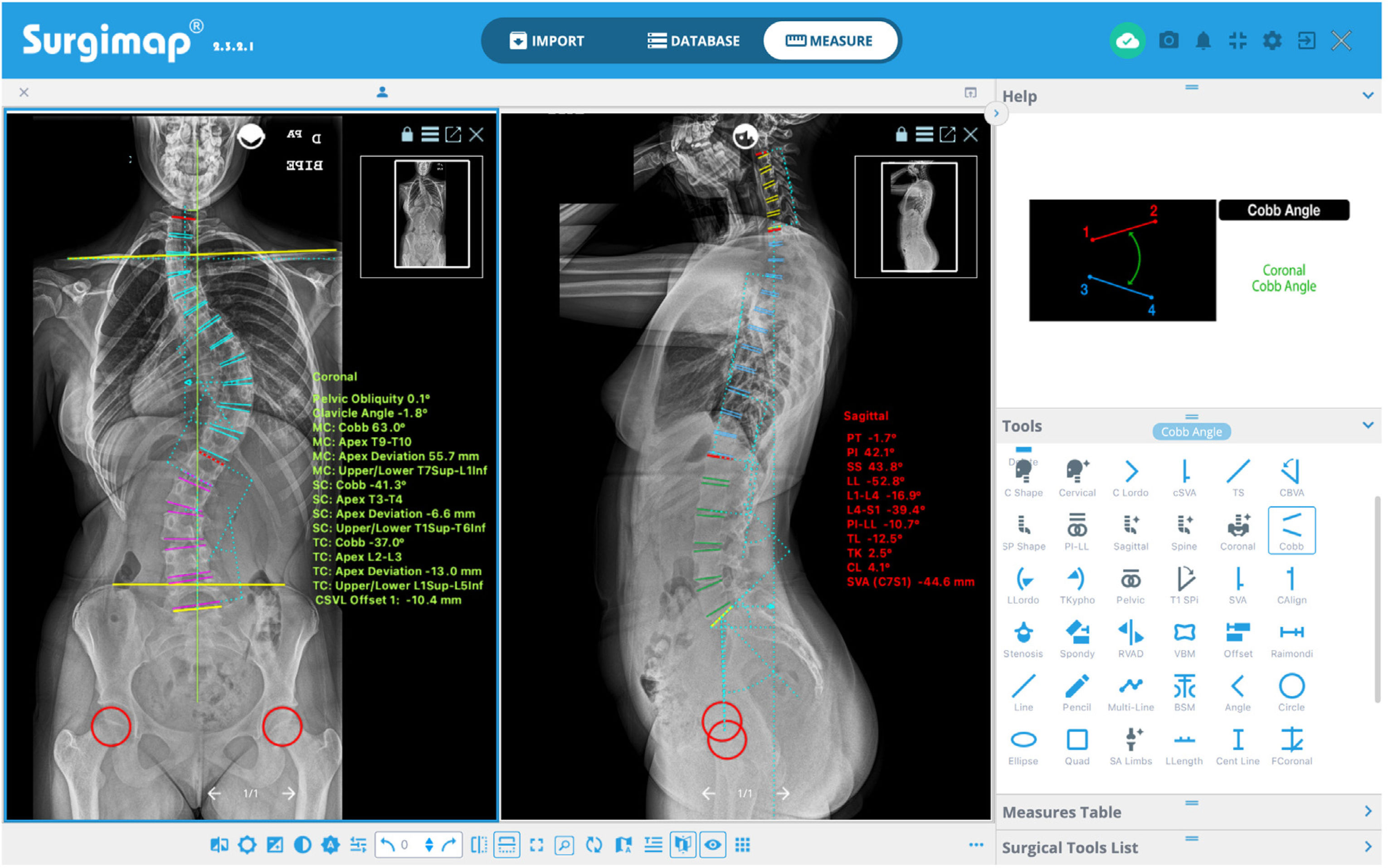
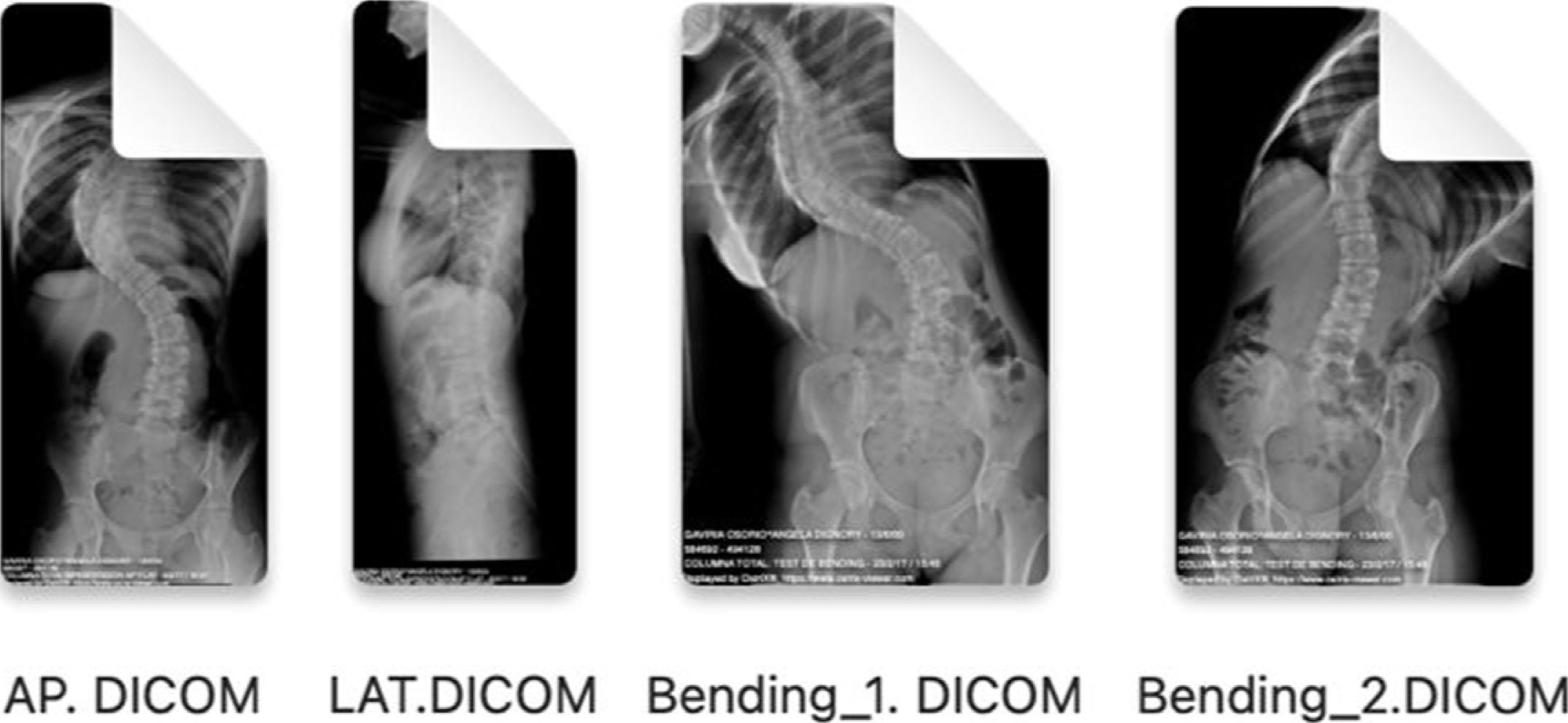
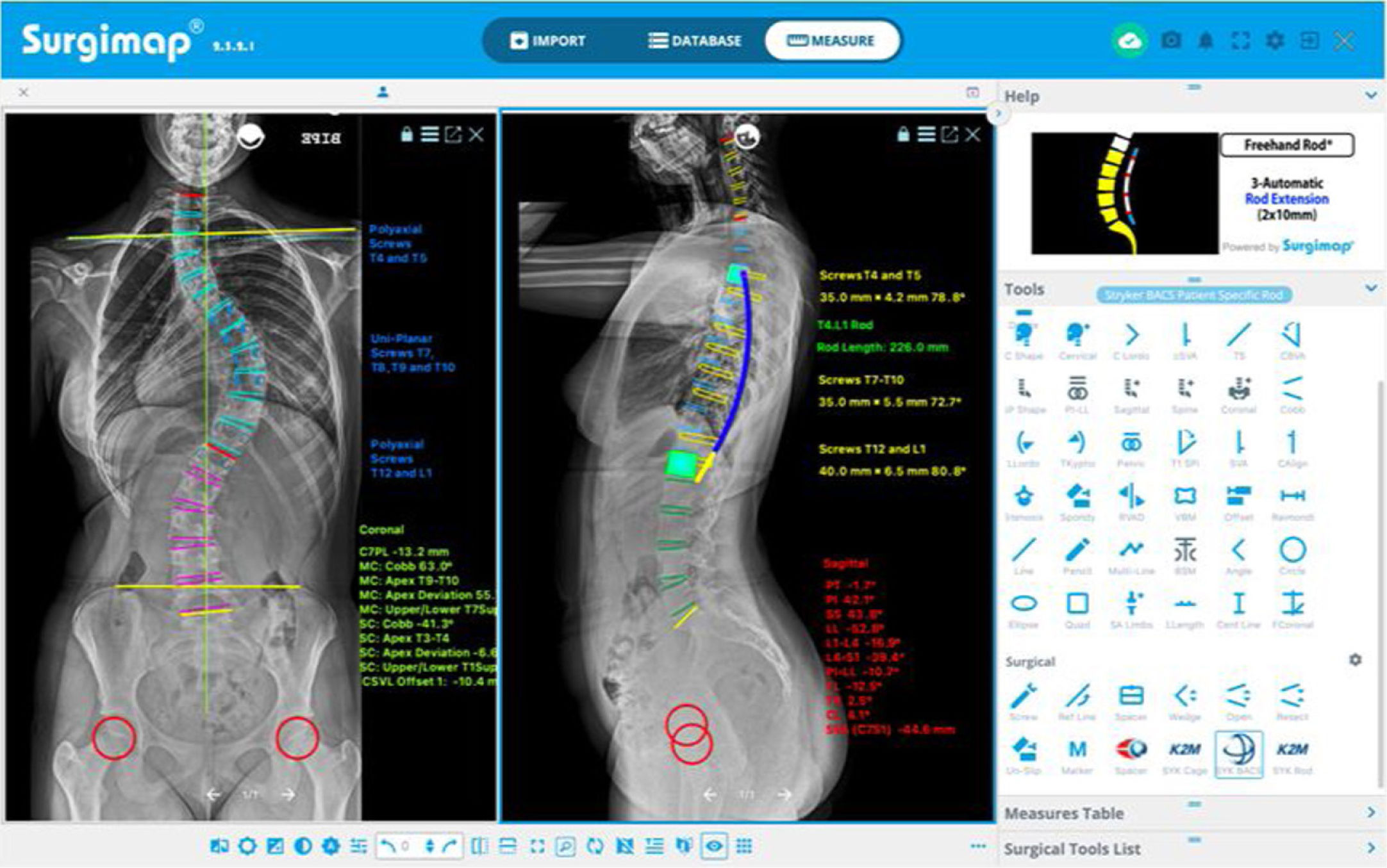
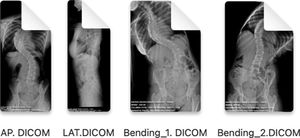
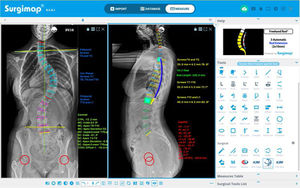
Preoperative radiological measurements in adolescent idiopathic scoliosisThe images of the posteroanterior and lateral teleradiographs and the bending tests obtained from the Picture Archiving and Communication System (PACS) are exported from a digital medical image viewer (e.g., Radiology Information System [RIS] Windows-based PC) in Digital Imaging and Communication on Medicine (DICOM) format and imported via the “import” window of the Surgimap® programme and stored in the “database”.
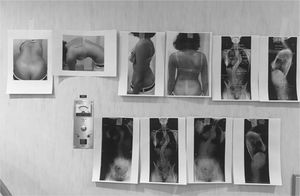
This programme has different semi-automatic digital measurement tools (“Tools”) located on the right side of the screen in the “Measure” window, with which different measurements are performed in each projection, using the coronal (“Coronal”) or sagittal (“Sagittal”) alignment wizard, as shown in Fig. 1. The programme offers a user-friendly interface with instructions and graphical representations in the “Help” box to perform each measurement. This enables the magnitude of the major curve to be determined measured by the Cobb angle defined between the upper end vertebra (UEV) and the lower end vertebra (LEV), as well as its location and direction as defined by the convexity of the curve,9 the apical vertebra (AV) and its degree of rotation according to the Nash-Moe scale and translation, the pelvic obliquity, the angle of the clavicles, the length discrepancy of the lower limbs, the coronal and sagittal balance of the spine, and the spinopelvic parameters: pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT). We also determine the neutral vertebra, the coronal and sagittal stable vertebra, the flexibility of the curves in the bending tests and, finally, the skeletal maturity according to the Risser grade,10 the triradiate cartilage, the greater trochanter physis, and in case of doubt, analysing the X-ray of the hand11 or the ossification of the humeral head12 (Fig. 2). MRI as a preoperative test in AIS is only requested if there are warning signs or atypical curves.
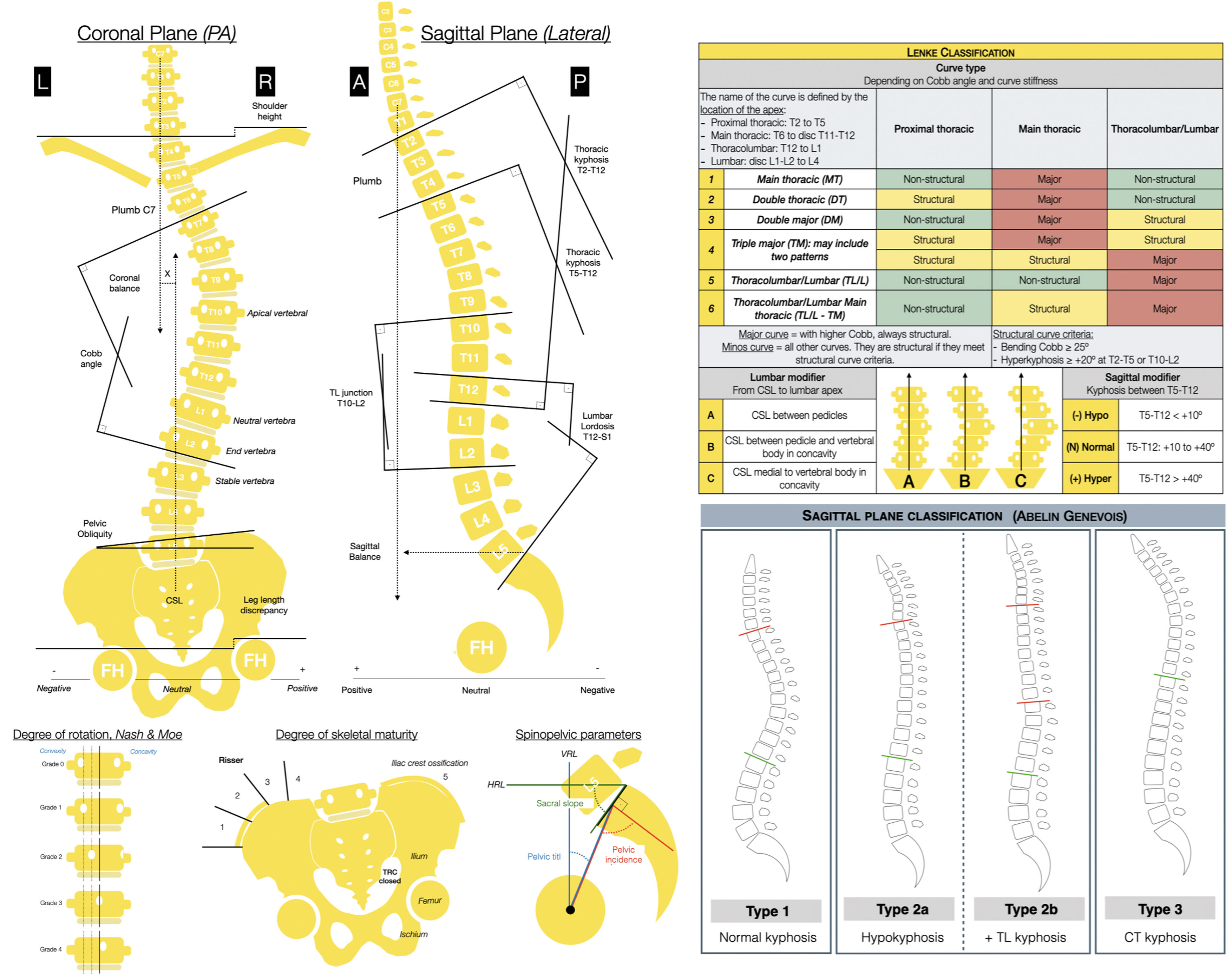
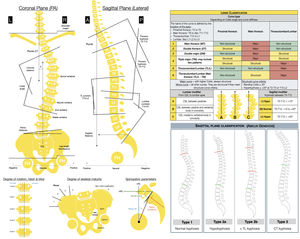
On the left: radiological measurements to be taken on the posteroanterior and lateral radiographs of the total spine in the standing position. Apical vertebra, the one furthest from the CSL and the most rotated. Neutral vertebra, the most proximal under the apex of the greater curve whose pedicles are not rotated, in other words, they are symmetrical. End vertebra, the most proximally and distally inclined at the ends of the major curve. Coronal stable vertebra, the most proximal under the apex of the greater curve which is cut in half by the CSL. A: anterior; FH: femoral head; TRC: triradiate cartilage; R: right; HRL: horizontal reference line; L: left; CSL: central sacral line; LL: lower limbs; P: posterior; PA: posteroanterior; VRL: vertical reference line.
On the right: Lenke's classification and Abelin-Genevois sagittal profile classification.
With the simple radiological assessment, we proceed to classify the curve using Lenke's classification (Fig. 2) as it has a therapeutic approach that allows us to determine the structural curves of a patient with AIS considering the coronal and sagittal planes, which are those that should be included in the fusion.13 We also use the classification by Abelin-Genevois15 according to the type of sagittal profile14 and specific to AIS patients (Fig. 2). The latter has a therapeutic approach to guide surgical correction of the sagittal plane, distinguishing four types according to the location of the sagittal structural curves, independent of the type of curve in the coronal plane, and is therefore considered complementary to Lenke's classification.
Surgical planning for adolescent idiopathic scoliosisThe principles of the surgical treatment of AIS are to fuse as few vertebrae as possible, to arthrodese only structural curves (defined according to Lenke et al. as those that do not correct below 25° on bending tests and/or have a segmental kyphosis of >20° from T2 to T5 or from T10 to L2),13 not to end instrumentation at the apex of a coronal or sagittal curve, and ensure that the central sacral line (CSL) is centred over the last fused vertebra, as well as understanding the interrelationship between the curves in the sagittal plane that allows reconstruction of the sagittal harmony according to the patient's spinopelvic parameters.
Generally speaking, when selecting the levels to be fused, for right thoracic curves the upper instrumented vertebra (UIV) will be T2 if the left shoulder is higher or the proximal thoracic curve is structural, T3 if both shoulders are balanced, and T4 if the right shoulder is higher,22 while for left thoracic curves it will be the other way around. In selective thoracic arthrodesis, the lower instrumented vertebra (LIV) will generally be the stable vertebra,16 defined as the most proximal vertebra below the major curve that is bisected by the CSL, but when the scoliosis has a flexible lumbar curve and is a Lenke lumbar modifier A, instrumentation may be ended at the touched vertebra,17 which is the most cephalad thoracolumbar or lumbar vertebra below the major curve that is “touched” by the CSL on any part of the vertebra. In cases of lumbar selective fusion, the UIV will be the UEV, and the LIV is usually the LEV or one level above it if that vertebra crosses the CSL on the bending test towards convexity and the rotation is less than Nash-Moe 2 on the bending test.18 The sagittal plane should also be considered, so that in cases of thoracic hyperkyphosis or thoracolumbar transverse kyphosis, the stable sagittal vertebra, defined as the most proximal divided by 50% by the posterior central sacral line, should be included in the instrumentation to minimise the risk of kyphosis of the distal junction.19
In severe and inflexible curves, pre- or intraoperative traction or the need for osteotomies at the apex of the deformity can be considered. The latter could also be used in cases of hyper- or hypokyphosis or other abnormalities in the sagittal plane as proposed by Abelin-Genevois et al.15According to these authors’ classification, type 2a may require Ponte-type osteotomies at the thoracic level to restore the kyphosis, type 2b in the thoracolumbar transition to rectify it, and type 3 in the lower thoracic area to lower the cervicothoracic kyphosis. In relation to the degree of correction, the main objective is correct coronal and sagittal balance, although in some cases this may involve under-correcting the curve to compensate for the residual deformity of a non-instrumented lumbar curve, avoiding postoperative distal imbalance or “adding-on”.20
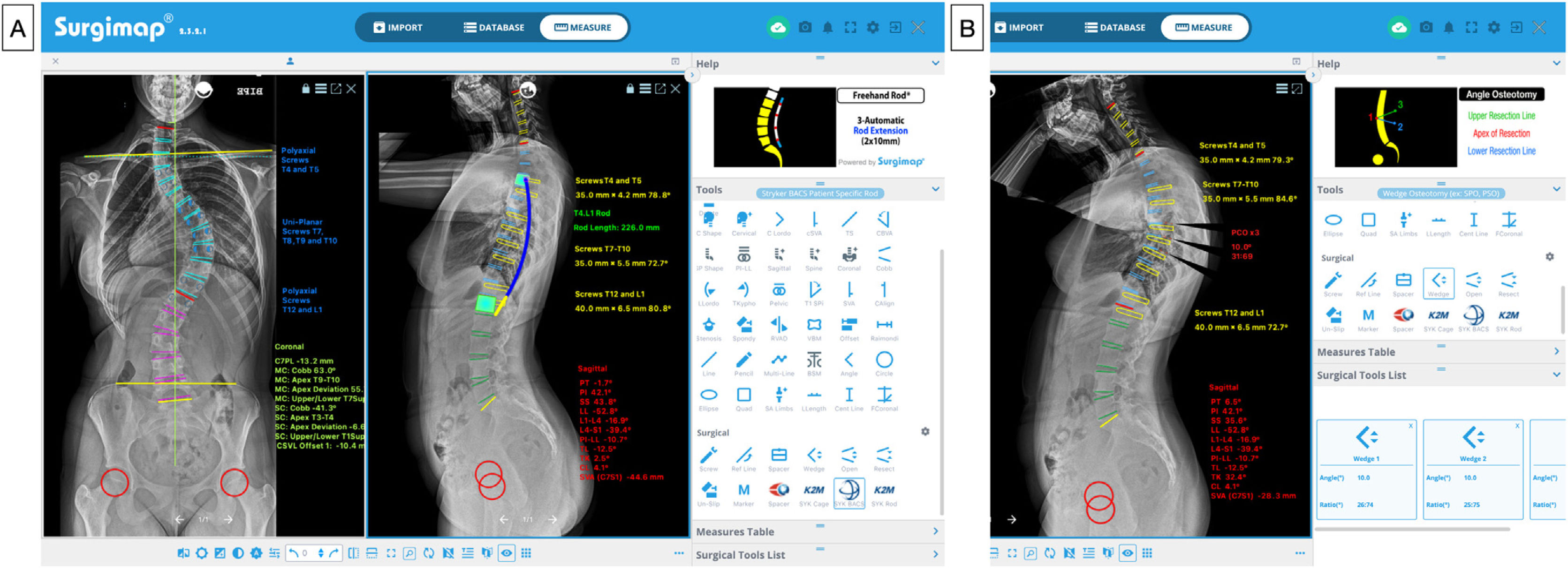
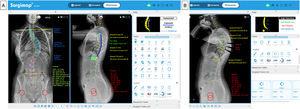
Following this theoretical knowledge, in Surgimap®, we have the option of planning the levels to be instrumented, indicating the type of screws to be used (generally uniplanar screws in the apex, as this is where most force is exerted during correction manoeuvres, and polyaxial screws at the ends),21,22 measuring their size and length, indicating the location of strategic implants (greater density of screws or screws per level in the apex and at the ends),23 planning the shaping, length, and diameter of the rods, and marking the areas where osteotomies are to be performed, as can be seen in, Fig. 3A. Similarly, using the wedge device in the sagittal plane, it is possible to simulate the correction that will be obtained after performing the osteotomy by removing a wedge-shaped portion of the image and visualising the virtual surgical correction of the radiograph and the modification of the pelvic parameters and the sagittal vertical axis (SVA) (Fig. 3B). Table 1 summarises the main data to be considered in the preoperative assessment and development of the surgical strategy in AIS.
Preoperative planning. (A) Levels to be instrumented, type and size of screws, and length and shape of rods. (B) Planning of posterior column osteotomies (PCO) at various levels at the apex of the thoracic curve to correct thoracic hypokyphosis (10° per level), and visualisation of the correction of sagittal alignment and balance.
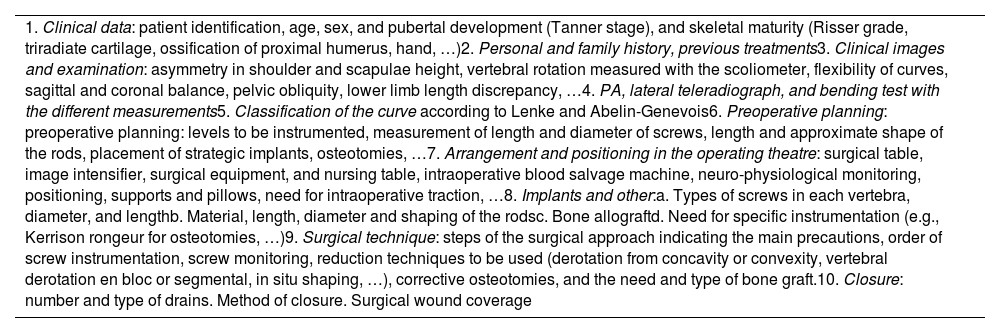
Summary of the preoperative evaluation and development of surgical strategy in AIS.
| 1. Clinical data: patient identification, age, sex, and pubertal development (Tanner stage), and skeletal maturity (Risser grade, triradiate cartilage, ossification of proximal humerus, hand, …)2. Personal and family history, previous treatments3. Clinical images and examination: asymmetry in shoulder and scapulae height, vertebral rotation measured with the scoliometer, flexibility of curves, sagittal and coronal balance, pelvic obliquity, lower limb length discrepancy, …4. PA, lateral teleradiograph, and bending test with the different measurements5. Classification of the curve according to Lenke and Abelin-Genevois6. Preoperative planning: preoperative planning: levels to be instrumented, measurement of length and diameter of screws, length and approximate shape of the rods, placement of strategic implants, osteotomies, …7. Arrangement and positioning in the operating theatre: surgical table, image intensifier, surgical equipment, and nursing table, intraoperative blood salvage machine, neuro-physiological monitoring, positioning, supports and pillows, need for intraoperative traction, …8. Implants and other:a. Types of screws in each vertebra, diameter, and lengthb. Material, length, diameter and shaping of the rodsc. Bone allograftd. Need for specific instrumentation (e.g., Kerrison rongeur for osteotomies, …)9. Surgical technique: steps of the surgical approach indicating the main precautions, order of screw instrumentation, screw monitoring, reduction techniques to be used (derotation from concavity or convexity, vertebral derotation en bloc or segmental, in situ shaping, …), corrective osteotomies, and the need and type of bone graft.10. Closure: number and type of drains. Method of closure. Surgical wound coverage |
AIS: adolescent idiopathic scoliosis.
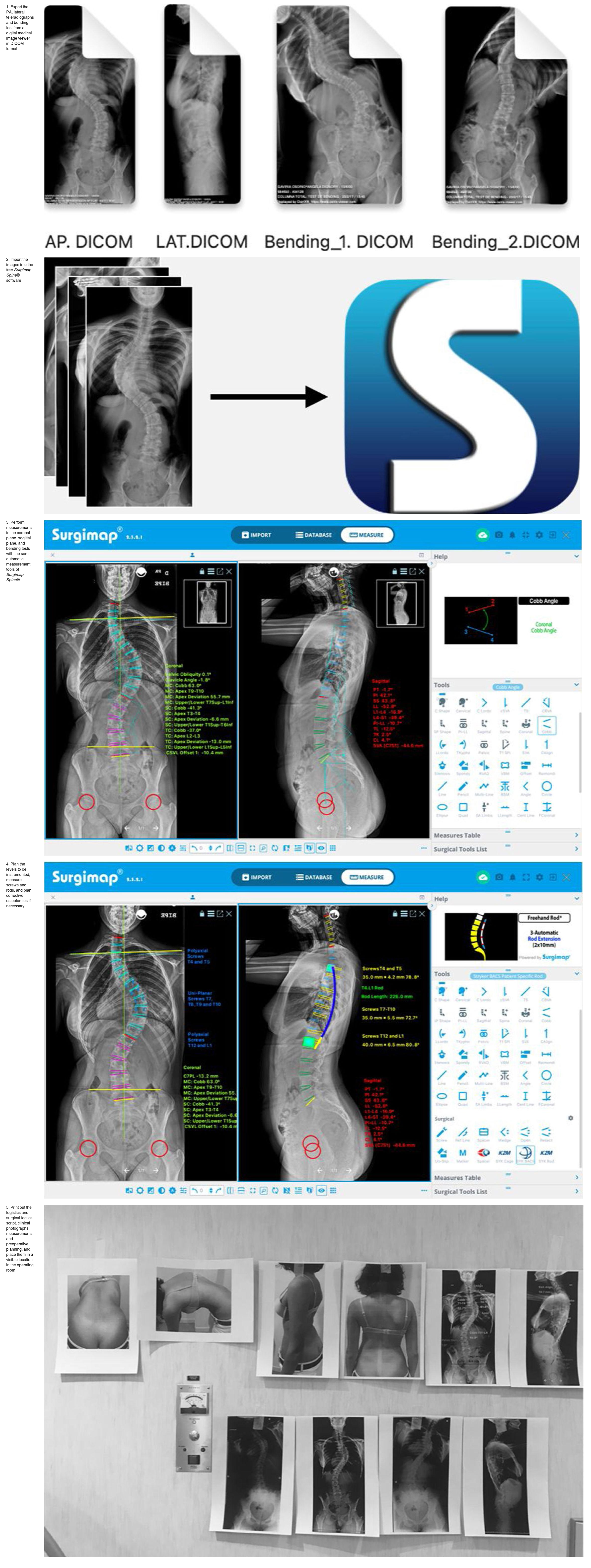
Preoperative planning with the written script (Table 2), clinical images, and radiographs with measurements and implants are printed and placed in a visible location in the operating room so that it can be used as a guide and consulted by any member of the team. It is important to note that the planning should serve as a guide, but may differ in some respects to the final execution based on intraoperative findings.
Example of written script of the surgical tactics and logistics for a patient with AIS.
| Patient identification | C.M.M. 632764 |
| Age and sex | Female, age 13 |
| Pubertal stage and skeletal maturity | Menarche at age 11, Tanner stage 4, Risser 4 |
| History | NKDA. No medical history. FA of scoliosis (mother and sister) |
| Previous treatments | Boston brace from age 11 |
| Clinical images and PE | Right shoulder higher, no pelvic obliquity, right thoracic hump of 14° scoliometer measurement, good coronal and sagittal balance, no LD |
| Radiographs | Right thoracic curve T7-L1 of 63°; proximal thoracic T1-T6 of 41°; left lumbar L1-L5 of 37°; PO of .8°; coronal imbalance 10.4 mm |
| Classification | Right thoracic curve Lenke 1BN, Genevois type 1 |
| Preoperative planning | Posterior selective thoracic fusion T4-L1 |
| Arrangement and positioning | Prone on radiolucent table, fluoroscope to right, blood salvage machine, facial support on chest, pelvis and knees, bony prominences padded, neurophysical monitoring |
| Implants and other | 6.5mm polyaxial pedicle screws at L1 and uniplanar at T12, 5.5mm uniplanar screws at T10, T9, T8, and T7, 5.5mm uniplanar screws at T5 and polyaxial screws at T4Extra strong CrCo rod of 5.5mm in diameter and 23cm length in concavity, and 5.5mm diameter and 23cm in convexity.80cm3 of bank bone allograft |
| Technique | Approach: posterior midline approach centred between T4 and L1, subperiosteal dissection of posterior elements, taking care not to injure the interspinous ligament proximally, or facet joints at the ends.Vertebral instrumentation: location and placement of screw in LIV, facetectomies, placement of distal, apex, and proximal implants starting from concavity.Reduction: 1. Correction by derotation with preshaped rod from concavity and partial closure, placement of preshaped rod in convexity; 2. vertebral derotation en bloc and definitive closure.Lavage. Decortication of posterior elements. Allografting and autografting |
| Closure | Drainage. Absorbable suture in fascia and subcutaneous. Skin with intradermal suture with absorbable monofilament. Simple dressing |
AIS: adolescent idiopathic scoliosis; CrCo: chromium cobalt; FH: family history; LD: length discrepancy; LIV: lower instrumented vertebra; NKDA: no known drug allergies; PE: physical examination; PO: pelvic obliquity.
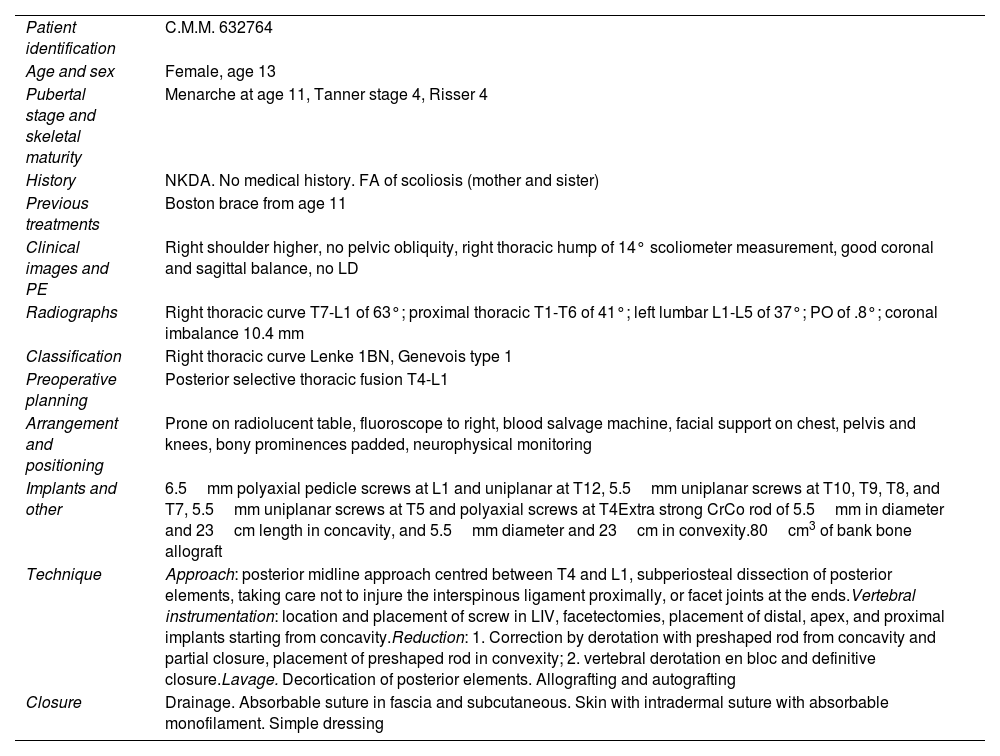
A summary of the steps outlined above for planning as per the method described is shown in Table 3.
Summary of steps for digital planning following the method described.
| 1. Export the PA, lateral teleradiographs and bending test from a digital medical image viewer in DICOM format | |
| 2. Import the images into the free Surgimap Spine® software | |
| 3. Perform measurements in the coronal plane, sagittal plane, and bending tests with the semi-automatic measurement tools of Surgimap Spine® | |
| 4. Plan the levels to be instrumented, measure screws and rods, and plan corrective osteotomies if necessary | |
| 5. Print out the logistics and surgical tactics script, clinical photographs, measurements, and preoperative planning, and place them in a visible location in the operating room |
DICOM: digital imaging and communication on medicine; PA: posteroanterior.
We show three representative cases of different types of AIS curves according to Lenke's classification and the sagittal profile, on whom a posterior vertebral fusion with pedicle screws24 was performed using the “hands-free” technique, after preoperative planning following the method described. The sizes and lengths of the implants and the levels to be fused were determined based on the measurements taken and the theoretical principles that apply to AIS surgery. We detail the basic points for the surgical planning, logistics, tactics, and postoperative radiological results of each case described.
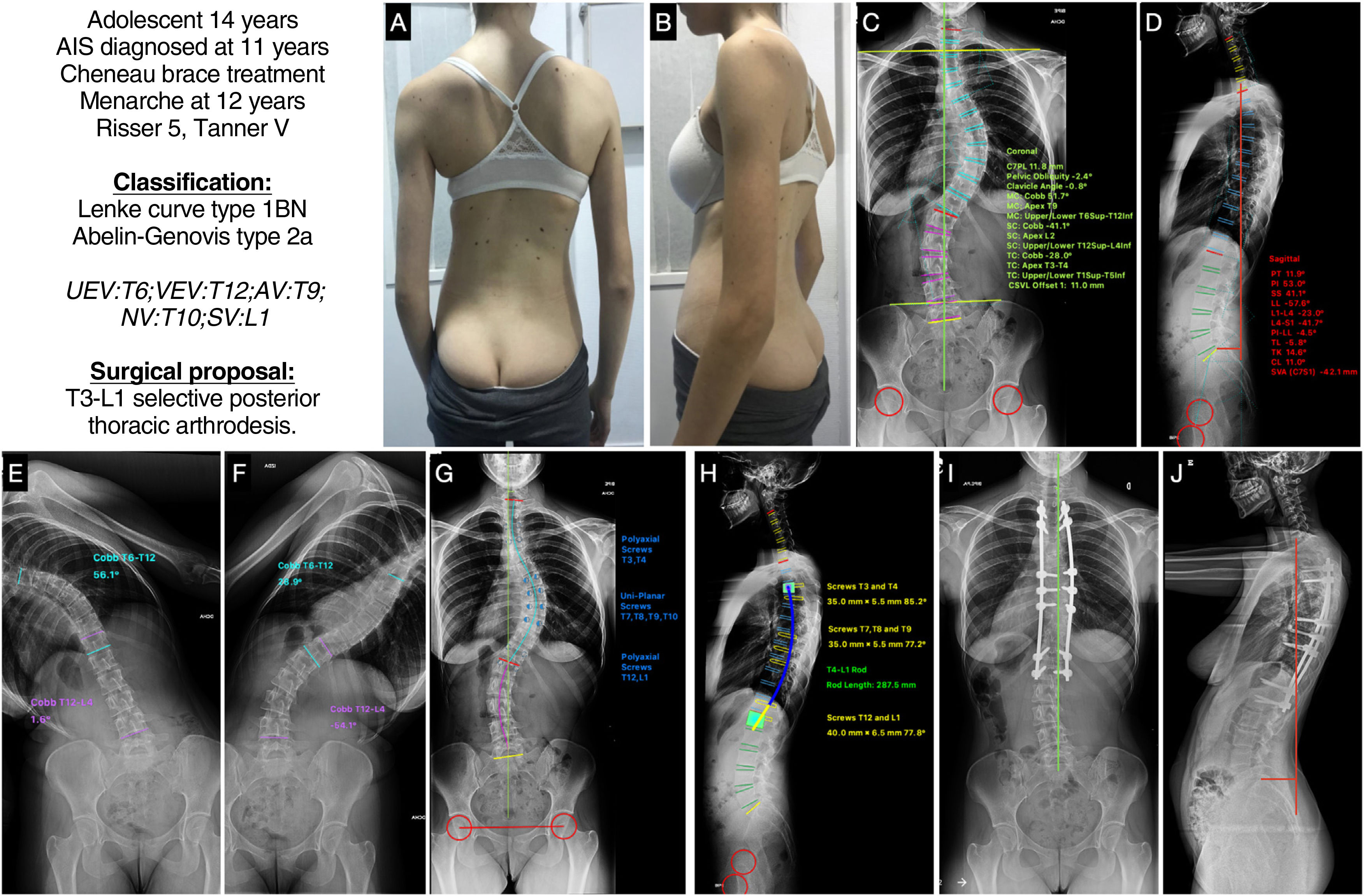
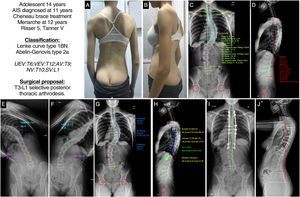
Case 1A 14-year-old female adolescent with AIS diagnosed at age 11, treated orthopaedically with a Chêneau-type brace, menarche at age 12, indicated for surgery with skeletal maturity measured by Risser grade 5 and Tanner stage 5. In the clinical images (Fig. 4A and B) we see a slight asymmetry of the shoulders, the right shoulder being slightly higher than the left, with retropulsion of the right scapula, asymmetry of the flanks, without pelvic obliquity, and with good coronal and sagittal balance. The posteroanterior radiograph (Fig. 4C) shows a major coronal curve T6-T12 of 51.7°, with the apex located at T9 and a degree of rotation I–II according to the Nash-Moe system, a proximal thoracic curve T1-T5 of 28°, and a lumbar curve T12-L4 of 41.1°, presenting a slight coronal imbalance to the right of 11.8mm, with minimal pelvic obliquity of 2.4° and a clavicular angle of .8° with the shoulders practically at the same height. The lateral X-ray (Fig. 4D) shows a cervical lordosis of +11°, a thoracic kyphosis of +14.6°, a thoracolumbar transit of −5.8°, and a lumbar lordosis (LL) of −57.6°. The SVA is −42.1mm, and the spinopelvic parameters: PT 11.9°, PI 53°, SS 41°, with a PI-LL ratio of −4.5°. In the bending tests, we can see that the lumbar curve is very flexible, correcting up to 1°, while the proximal thoracic curve is not entirely visible, and is likely to correct below 25° (Fig. 4E and F). With these data, our patient would be classified as a Lenke type 1BN and Abelin-Genevois type 2a. The surgical proposal would be to perform a selective posterior thoracic vertebral fusion, as the lumbar and proximal thoracic curve is not structured, from T3, because the shoulders are at the same height, to L1 as the vertebra is stable and has a lumbar B modifier. The planning of the screws, polyaxial at the ends and uniplanar at the apex, and the type and size of the rod, with the approximate shape, are also shown (Fig. 4G and H). Fig. 4I and J shows the postoperative radiographs of this patient, which are in accordance with the pre-planning, with good alignment and balance results in both planes.
(A and B) Clinical images of the back and profile of the patient with AIS. (C and D) Posteroanterior and lateral radiography of the patient's full spine in standing position with measurement of the different radiological parameters. (E and F) Right and left bending test to assess the flexibility of the curves and determine whether they are structural or not. (G and H) Preoperative planning of the types of pedicle screws, their location, length, and diameter, and planning of the type, length, and shaping of the rods. (I and J) Radiological result in posteroanterior and lateral projection of the complete spine in standing position similar to the preoperative planning. AV: apical vertebra; LEV: lower end vertebra; NV: neutral vertebra; SV: stable vertebra; UEV: upper end vertebra.
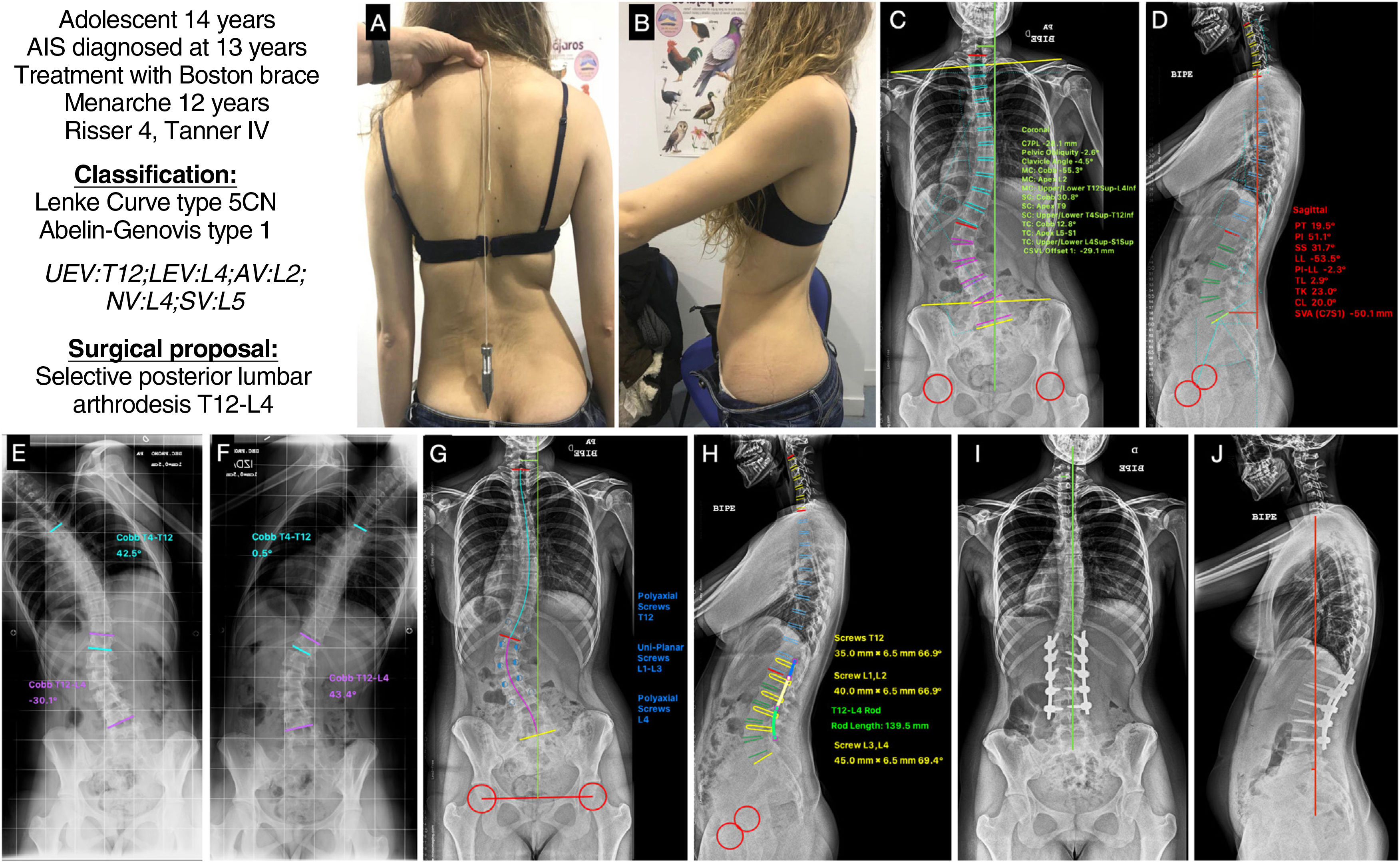
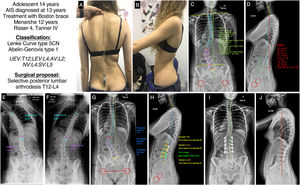
A 14-year-old female adolescent with AIS diagnosed at the age of 13. She received orthopaedic treatment with a Boston type brace. Menarche at 12 years, Tanner stage 4, and skeletal maturity measured by Risser grade 4. In the clinical images (Fig. 5A and B) we see a difference in the height of the shoulders, the right being higher than the left, asymmetry of the flanks with the right fold marked and the left erased, no pelvic obliquity, slight coronal imbalance to the left, and good sagittal balance. The posteroanterior X-ray (Fig. 5C) shows a major coronal curve T12-L4 of 55.3°, with the AV L2 showing a degree of rotation II according to Nash and Moe, a thoracic curve T4-T12 of 30.8°, a slight coronal imbalance to the left of −29.1mm, with minimal pelvic obliquity of −2.6° and a clavicular angle of −4.5° with the right shoulder positioned higher. The lateral radiograph (Fig. 5D) shows a cervical spine in kyphosis +20°, a thoracic kyphosis of +23°, a thoracolumbar transit of 2.9° and an LL of −53.5°. The SVA is −50.1mm, and the spinopelvic parameters: PT 19.5°, PI 51.1°, SS 31.7°, with a PI-LL ratio of −2.3°. In the bending tests, we can see that the thoracic curve is very flexible, correcting up to .5° (Fig. 5E and F). With these data, our patient would be classified as a Lenke type 5CN and Abelin-Genevois type 1. The surgical proposal would be to perform a selective posterior lumbar vertebral fusion, as the thoracic curves are non-structural, from UEV to LEV, i.e., from T12 to L4. The planning of the screws, polyaxial at the ends and uniplanar in the apex area, and the type and size of the rod, with the approximate shape, are also shown (Fig. 5G and H). Fig. 5I and J shows the patient's postoperative radiographs, which are in accordance with the planning undertaken beforehand, with good alignment and balance results in both planes.
(A and B) Clinical images of the back and profile of the patient with AIS. (C and D) Posteroanterior and lateral radiograph of the patient's entire spine in standing position with measurement of the different radiological parameters. (E and F) Right and left bending test to assess the flexibility of the curves and determine whether they are structural or not. (G and H) Preoperative planning of the types of pedicle screws, their location, length, and diameter, and planning of the type, length, and shaping of the rods. (I and J) Radiological result in posteroanterior and lateral projection of the entire spine in standing position, consistent with the preoperative planning. AV: apical vertebra; LEV: lower end vertebra; NV: neutral vertebra; SV: stable vertebra; UEV: upper end vertebra.
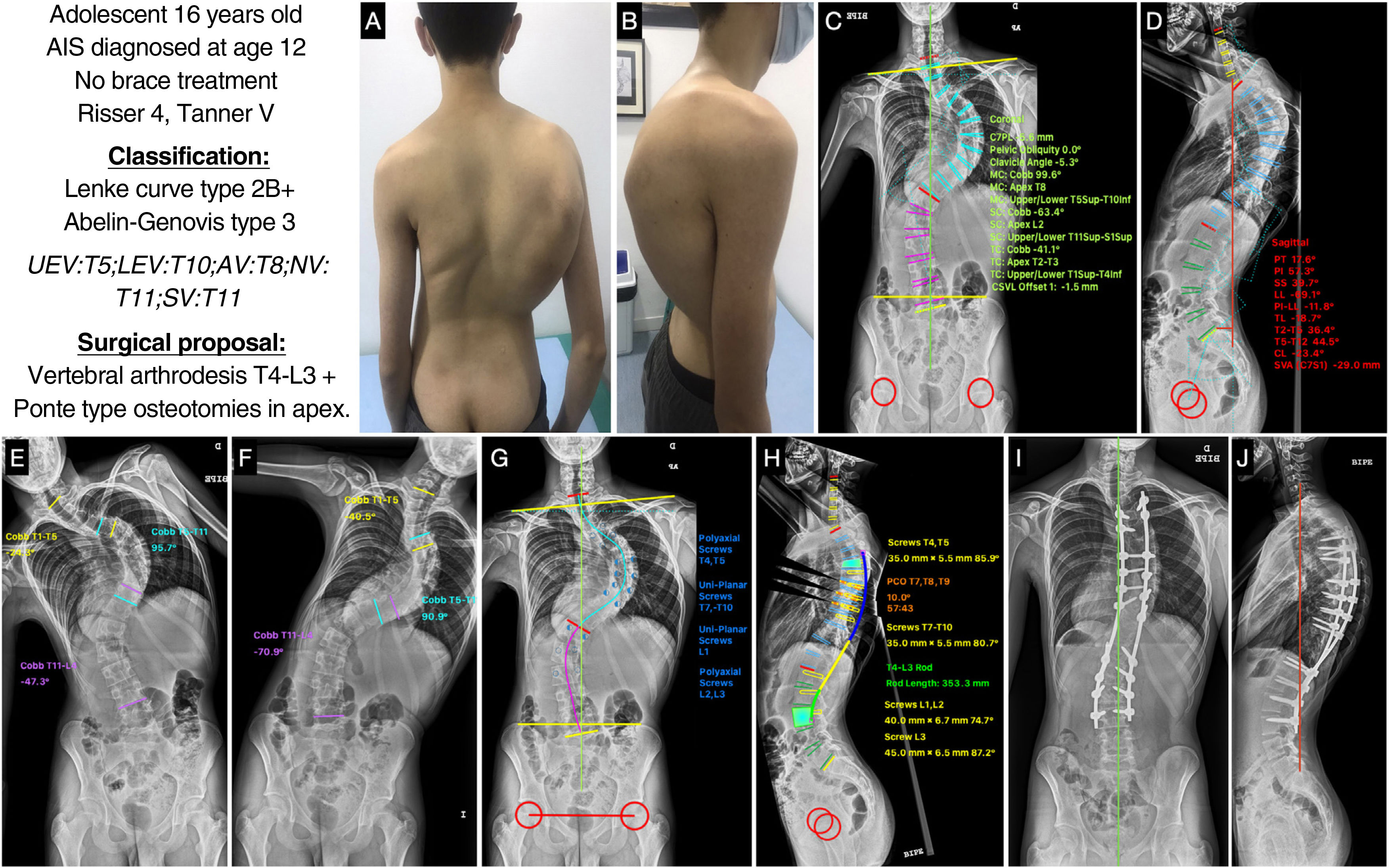
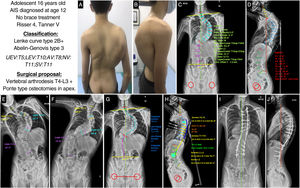
A 16-year-old male adolescent with AIS diagnosed at 12 years of age in another centre without previous treatment with brace who presented with complete ossification of the iliac process or Risser grade 5, and Tanner stage 5. The clinical images (Fig. 6A and B) show good coronal balance, asymmetry of the shoulders, the right shoulder being higher and the right shoulder blade retropulsed, asymmetry of the flanks with an erased left crease and a right thoracic hump. In the sagittal plane, the patient is well balanced and shows thoracic hyperkyphosis. Posteroanterior X-ray (Fig. 6C) shows a major curve T5-T10 of 99.6°, with the apex located at T8 and a degree of rotation 2–3 according to Nash and Moe, a proximal thoracic curve T1-T4 of 41.1°, and a lumbar curve T11-S1 of 63.4°, showing good coronal balance, no pelvic obliquity, and a clavicular angle of −5.3° with the right shoulder higher. The lateral X-ray (Fig. 6D) shows a cervical lordosis of −23.4°, a thoracic kyphosis of +44.5°, a thoracolumbar transition of −18.7° and an LL of −69.1°. The SVA is −29mm, and the spinopelvic parameters: PI 57.3°, PT 17.6°, SS 39.7°, with a PI-LL ratio of −11.8°. In the bending tests, we can see how the proximal thoracic curve corrects to 24.3° and is therefore considered non-structural, while the lumbar curve decreases to 47.3°, which is considered structural (Fig. 6E and F). With these data, our patient would be classified as a Lenke type 3B+ and Abelin-Genevois type 3 because he has an excess of lordosis in the thoracolumbar transit. Because both the main thoracic curve and the lumbar curve are structural, we must include them in the instrumentation. Furthermore, it can be seen in the bending tests that the thoracic curve barely corrects 10°, so in addition to being a severe curve, it is rigid. Therefore, the surgical proposal would be to perform a posterior vertebral fusion from T4, as it is a right thoracic curve and the right shoulder is higher, to L3 to include the lumbar curve in the instrumentation, given that the lumbar curve does not have much rotation and that this vertebra crosses the CSL in the bending tests. Ponte-type osteotomies are also proposed at the apex of the thoracic curve to make it more flexible and correct the hyperkyphosis. As an associated gesture during the procedure, the use of soft intraoperative traction is proposed, which allows gradual and progressive correction of the deformity. Fig. 6G and H shows the planning of the pedicle screws, polyaxial at the ends and uniplanar at the apex and the type and size of the rod, and the correction to be achieved in the sagittal plane with the osteotomies. Fig. 6I and J shows the patient's postoperative radiographs, which are similar to the preoperative planning, with satisfactory results in alignment and balance of the spine.
(A and B) Clinical images of the back and profile of the patient with AIS. (C and D) Posteroanterior and lateral radiographs of the patient's entire spine in standing position with measurement of the different radiological parameters. (E and F) Right and left bending test to assess the flexibility of the curves and determine whether they are structural or not. (G and H) Preoperative planning of the types of pedicle screws, their location, length, and diameter, planning of the type, length, and shaping of the rods, and planning of the Ponte-type osteotomies and simulation of the correction achieved with each. (I and J) Radiological result in posteroanterior and lateral projection with the achievement of good coronal and sagittal alignment and balance. AV: apical vertebra; LEV: lower end vertebra; NV: neutral vertebra; SV: stable vertebra; UEV: upper end vertebra.
Despite the importance of adequate preoperative planning in the surgical treatment of AIS, there are few texts that explain the process of how to plan this surgery so that it can be applied to practical day-to-day cases. Hence the detailed description in this work of each step of the preoperative planning method for AIS surgery that we use in our specialised paediatric and adolescent spine unit in a referral centre, with practical cases in which we apply the theory explained.
The combined use of different literature sources and experience allows each surgical team to use a more or less systematised planning method in their daily practice. The radiological measurement manual of the Spinal Deformity Study Group,9 or various scientific publications or review articles are used as a guide to select the curves to be fused,13 the levels to be fused,16 the instrumentation strategies, the correction manoeuvres,25 and the restoration of the sagittal plane,15 among others. Considering that carefully thought-out preoperative planning is essential for surgical efficacy and optimisation of results, we believe that a protocolised preoperative planning method is essential in AIS.
In spine deformity surgery, it is critical to choose the appropriate levels of fusion in order to obtain correct shoulder height, good coronal and sagittal balance, including the minimum number of segments in the fusion and thus obtain the best results in the short, medium, and long term.25,26 To that end, both clinical and radiological parameters must be taken into account, and the basic principles of AIS surgery, as well as the most current concepts, must be known. An incorrect proximal instrumentation level can lead to shoulder height asymmetry, proximal decompensation, or proximal junctional kyphosis with associated morbidity. Inadequate selection of the distal instrumentation level can lead to postoperative distal adding-on phenomenon,27,28 coronal imbalance,29,30 or distal junctional kyphosis, which are associated with poor outcomes and the need for future reintervention.
Including only structural curves in the instrumentation, assuming spontaneous correction of non-structural compensatory curves, implies less morbidity for the patient, saving fusion levels and leaving a more mobile spine whenever possible.31 In fact, based on our experience, we try to avoid fusion of the last lumbar levels, leaving three mobile discs below the LIV as far as possible, i.e., attempting not to go more distal to L3, except in lumbar curves where it may be necessary to further distalise the lower level.
Having an estimate of the length of the implants, the density of the pedicle screws, as well as the strategic sites to place them, logically improves intraoperative precision and the speed with which the surgical procedure will be performed. It also reduces complications, since any large difference between the planned and the intraoperative findings can warn of a potential error that must be confirmed. The shorter operative time has also been associated with a lower complication rate in spinal deformity surgery in paediatric patients. In addition, the different resources to be used should be taken into account prior to surgery, such as the use of pre- or intraoperative traction in severe or rigid curves, the need for bone allografting, and the need for added surgical gestures such as osteotomies to increase curve flexibility and assist in correction.
The type of corrective manoeuvre to be performed will depend on the surgeon's experience, as well as the type, severity, and rigidity of the deformity in question. Understanding the expected behaviour of the compensatory curves also allows the surgeon to compensate for residual deformity in these areas by intentionally under-correcting the fused segment(s) to achieve overall spinal balance.20
Although traditionally AIS surgery has focused on maximising coronal deformity, the sagittal plane, both alignment and balance, is now considered critical. Assessment of the spinopelvic parameters in conjunction with SVA provides a more complete picture of the sagittal profile of the spine. The three basic pelvic parameters show a geometric relationship in which PI is equal to the sum of PT and SS (PI=PT+SS). PI reflects an individual and constant morphological parameter. PT and SS are spatial or compensatory parameters used to maintain functional sagittal balance. The assessment of the sagittal profile is not only taken into account to select the levels to be fused, but also to preshape the rods and other additional procedures such as osteotomies to restore the most appropriate type of Roussouly sagittal profile for each patient,14 following the recommendations of Abelin-Genevois et al.,15 for patients with AIS and adapting the LL to the PI,32 and other parameters that are associated with an increase in the patient's health-related quality of life, such as a PT of less than 20°, an SVA less than 5cm and a PI around ±10° of the LL PI=LL±10°).
Although other more advanced planning software is available on the market, Surgimap® is currently the most widely used, freely available, stand-alone planning software in both research and clinical practice33 and its use has been validated, demonstrating its accuracy,7 inter- and intra-observer reliability, and reproducibility,34 and it is simple and effective.
As limitations of the method described, we find that surgical correction of AIS is a complex procedure and, although different schemes have been proposed to guide preoperative planning and selection of the correct fusion levels, there is no algorithm that can be used for the standardised treatment of all deformities and, therefore, treatment must be tailored to each patient and each deformity. In addition, due to constant research and advances in various aspects of AIS, and improvements in implants and surgical techniques, the different indications may be modified with scientific progress. Nevertheless, we consider it very useful for specialists in training on the spine to learn a preoperative planning method that can be easily put into practice, to initiate them in the surgical management of this disease.
In conclusion, the method of preoperative planning in AIS that we describe, based on the clinical analysis of the patient and radiological analysis of the deformity, together with the free Surgimap® software, allows the design of a treatment strategy following the current principles of surgical correction of vertebral deformity. Knowledge of the basics of planning in AIS surgery is essential for any specialist training in spine surgery, and its understanding is necessary before using more advanced technology systems. In addition to its formative nature and the fact that it gives the surgeon the opportunity to confront management of the deformity before surgery, it is a simple, low-cost, very accessible, and widely reproducible method, which makes it ideal for its application in daily practice.
Level of evidenceLevel of evidence IV.
Ethical approvalThis is not a research project involving experimentation on animals or human subjects; therefore, approval from the Clinical Research Ethics Committee (CREC) was not required.
FundingNone of the authors have received financial payments or other benefits from any commercial entity related to the topic of this article.
Conflict of interestsThe authors have no conflict of interests to declare.