The consequences of COVID-19 pandemic, like in any other field of medicine, had such a massive effect in the activity of spine surgeons.
ObjectivesThe main purpose of the study is quantifying the number of interventions done between 2016 and 2021 and analyze the time between the indication and the intervention as an indirect measurement of the waiting list. As secondary objectives we focused on variations of the length of stay and duration of the surgeries during this specific period.
MethodsWe performed a descriptive retrospective study including all the interventions and diagnosis made during a period including pre-pandemic data (starting on 2016) until 2021, when we considered the normalization of surgical activity was achieved. A total of 1039 registers were compiled. The data collected included age, gender, days in waiting list before the intervention, diagnosis, time of hospitalization and surgery duration.
ResultsWe found that the total number of interventions during the pandemic has significantly decreased compared to 2019 (32.15% less in 2020 and 23.5% less in 2021). After data analysis, we found an increase of data dispersion, average waiting list time and for diagnosis after 2020. No differences were found regarding hospitalization time or surgical time.
ConclusionThe number of surgeries decreased during pandemic due to the redistribution of human and material resources to face the raising of critical COVID-19 patients. The increase of data dispersion and median of waiting time, is the consequence of a growing waiting list for non-urgent surgeries during the pandemic as the urgent interventions also raised, those with a shorter waiting time.
Las consecuencias de la pandemia por COVID-19, como en otros aspectos de la medicina, se han visto reflejadas también en la actividad quirúrgica de columna vertebral.
ObjetivosEl objetivo principal del presente estudio es cuantificar el número de intervenciones realizadas entre los años 2016 y 2021 y analizar el tiempo de espera en los pacientes intervenidos como medida indirecta del volumen de la lista de espera. Como objetivos secundarios se realiza un análisis del tiempo de estancia hospitalaria y el tiempo quirúrgico a lo largo de la serie.
MétodosSe ha realizado un estudio descriptivo retrospectivo en relación con el volumen de intervenciones y diagnósticos durante un periodo que incluye desde la etapa previa a la pandemia (2016) hasta finales del año 2021, en que la situación global llegó a una cuasinormalización de la actividad. Se han identificado un total de 1.039 registros. Se incluyen las variables edad, género, días en lista de espera antes de la intervención, diagnóstico, tiempo de estancia hospitalaria y tiempo quirúrgico.
ResultadosSe objetiva una disminución en el número total de intervenciones durante la pandemia respecto al año 2019 (32,15% menos el año 2020 y 23,5% menos el 2021). Tras el análisis de los datos, se observa un aumento en la dispersión y la mediana del tiempo de espera global y por patologías a partir de 2020, sin detectarse diferencias significativas en el tiempo de hospitalización ni en el tiempo quirúrgico.
ConclusiónDurante la pandemia se ha producido una disminución del número de intervenciones debido a la necesidad de redistribuir recursos humanos y materiales para hacer frente al incremento de pacientes críticos afectados por la COVID-19. El aumento de la dispersión y de la mediana global y por patologías de la variable tiempo de espera se traduce como un incremento del tiempo de espera en las cirugías diferibles realizadas durante los años de la pandemia y un aumento de las intervenciones llevadas a cabo de manera urgente, estas con un tiempo de espera mucho menor.
The literature on the catastrophic consequences of the SARS-CoV-2 pandemic worldwide is abundant and varied.
From 7 January 2020, when an outbreak of atypical pneumonia caused by a new virus in the Coronaviridae1 family was declared in China, until two months later on 11 March 2020 the World Health Organization declared Coronavirus Disease (COVID-19) to be a pandemic,2,3 events occurred rapidly. There was confusion about the measures to adopt and the dimensions the pandemic would eventually attain. It has now led to more than 500 million diagnoses worldwide and at least 6 million deaths, according to the statistics.4
Most especially during the first months of the pandemic the increase in the demand for medical care and the high mortality rate gave rise to the collapse of normal medical care.5
The causes of this collapse are justified and multiple. On the one hand they arose due to lack of knowledge about the disease and the virus, together with the lack of scientific evidence for the design of appropriate hospital and population protocols. However, it was also enormously influenced by the lack of fungible and structural materials, as well as hospital life support systems. There was also the need to redistribute human resources in medical care, and all of these factors meant that it was impossible to care in an optimum way for all patients.6,7
During this period and thanks to adaptation made obligatory by need and at a high economic, physical and emotional cost, the attempt was made to maintain medical care work. It was possible to attend to emergencies, and some face-to-face work was complemented by the swift development of telematics care.7,8 Specific circuits were designed, with shared hospital isolation facilities and surgical protocols implemented in the attempt to continue working on medical care in fields other than COVID-19, with more or less success.3,9–15
Now there is the prospect of an infection that is under greater control – even though it has not been completely resolved – and there is also more experience in managing the pandemic, combined with the high vaccination rate (with about 12,000 million doses administered worldwide). These factors have allowed us to gradually return to quasi-normality in hospital care, so that it would seem to be a good time to reflect on the sequelae of the pandemic in each speciality of our healthcare system. This will allow us to implement an appropriate multidisciplinary reorganization in our hospitals, with surgical protocols to offer the best treatment for patients in the safest, most effective and efficient way possible.6,16–19
A sudden interruption occurred in surgical specialities for pathologies that were not considered to be urgent, while emergency surgery remained at levels of activity similar to the pre-pandemic situation.8,9,16,19–21
More specifically, for spinal surgery the operations that could not be delayed, such as unstable fractures, spinal compression, radiculopathy causing a deficit or infections were maintained as far as was possible.2,3,5,6,17
The other spinal pathologies which were more suitable for postponement and which still led to visits (face-to-face or telematic), such as degenerative pathologies, spinal stenosis or spondylolisthesis without a neurological deficit, continued to be added to waiting lists that were saturated beforehand. Due to the lack of capacity to satisfy the accumulated demand these waiting lists have quickly and massively lengthened.3,16,17,22–24 The increased delay in treating these conditions may lead to sequelae, increasing complications and leading pathologies to progress.20
The principle cause of the fall in the number of spinal surgery operations is the high rate of hospital occupation and the fall in the availability of surgical and human resources.3,8 This is because in comparison with other surgical specialities, spinal surgery requires hospitalization for longer periods of time.5,6
It is clear that the most immediate consequence that we will face will be the underlying accumulated volume of cases due to pathologies that went untreated during the pandemic because they were less urgent. However, they are no less severe because of this, and the morbidity of chronic musculoskeletal diseases has risen significantly.8,21
However, the impact was not uniform across the whole health system,7,18 as delays in diagnosis have increased in life-threatening pathologies, and treatment has been delayed in pathologies that may require long periods of hospitalization or beds in critical units following surgery.8
The main aim of this study is to quantify the number of operations performed from 2016 to 2021 and to analyze the waiting time for patients who were operated. This is an indirect way of measuring the length of the waiting list, and the study also covers hospitalization and surgical time throughout the series.
We therefore quantified the impact of the pandemic in terms of the total volume and type of surgical operations performed in the spinal column unit of a second level hospital. The aim was to measure, visualize and better understand the changes experienced in these exceptional circumstances regarding diagnoses and the delay which patients were forced to suffer.
Material and methodsThis is a descriptive observational study that analyses the patients who were subjected to surgical operations for spinal column pathology in a second-level hospital by the neurosurgery department or the traumatology department, from 1 January 2016 to 31 December 2021, as in our hospital both of these departments treat spinal pathology.
The population of the hospital catchment area amounts to 450,000 individuals, and it is the only public hospital which performs spinal column surgery, distributed between the orthopaedic and traumatology department and the neurosurgery department.
The variables included are patient age and sex, coded diagnoses, time in the waiting list to the indication of the operation (in days), the duration of the operation (in minutes) and days of hospitalization.
Diagnoses are grouped as cervical myelopathy, cervical radiculopathy, lumbar stenosis, lumbar radiculopathy, fractures and revision surgery.
A purely descriptive analysis of the data was undertaken using R-Studio software.
A statistical significance of 5% was considered to compare hypotheses.
Changes in the delay profile during the pandemic were analyzed in this study, together with changes in the diagnoses operated during the pandemic and changes in delay according to diagnosis.
The secondary objectives were to analyze surgical time and hospitalization.
ResultsThe data obtained include 1039 records of operations performed from 2016 to 2021.
The cases of emergency surgery which accumulated no delay at any time are cauda equina syndrome (3 cases) and epidural haematoma (5 cases).
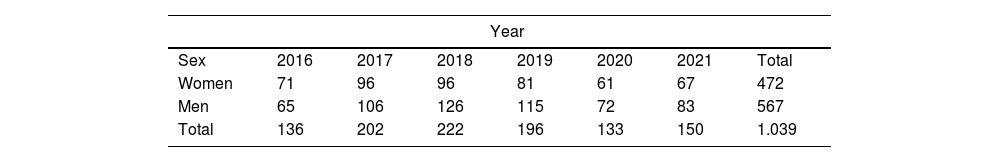
The sample is composed of a total of 472 women and 567 men, distributed according to year, as shown in Table 1.
No significant differences were detected in the proportion of the sexes of the patients operated over the years (P=.456).
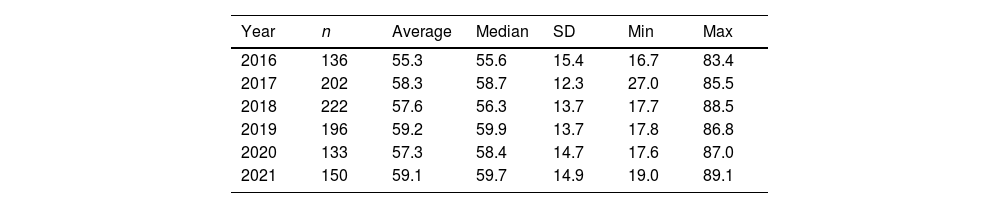
The distribution of the age variable in the operated patients is shown in Table 2. No significant differences were detected between the years studied (P=.207).
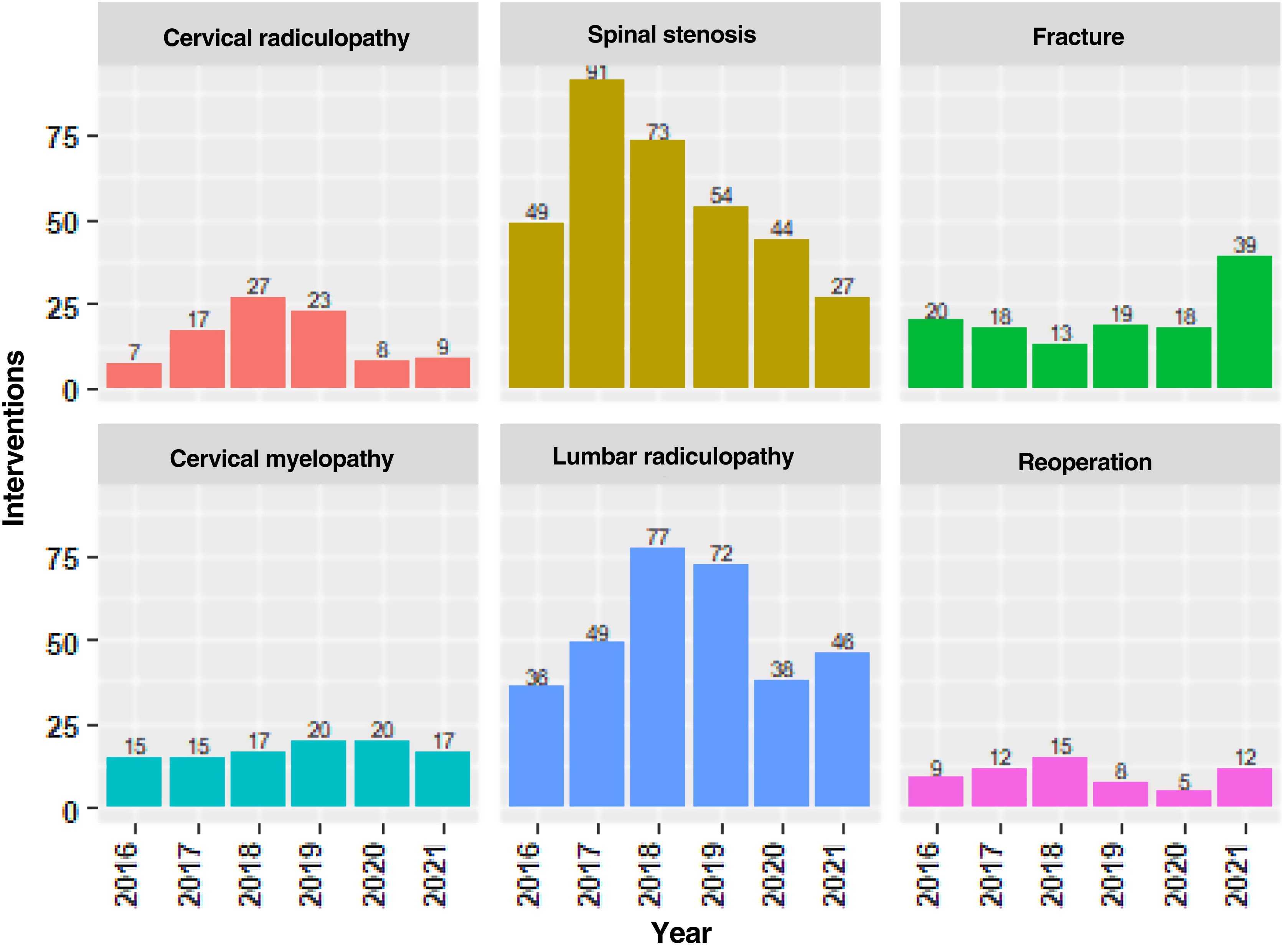
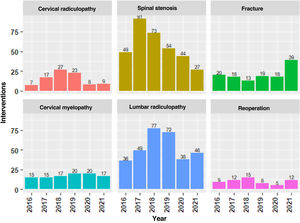
Fig. 1 shows the number of operations performed from January 2016 to December 2021, grouped according to diagnosis. The maximum number of operations were performed in 2018 (222). The year the pandemic commenced the number of spinal column operations fell to 133 (32.15% fewer than in the previous year) and in 2020 they numbered 150 (23.5% fewer than in 2019).
The number of operations for diagnoses which are considered liable to delay (cervical radiculopathy, lumbar stenosis and lumbar radiculopathy) fell in 2020 and 2021, coinciding with the restrictions of the pandemic. On the other hand, pathologies considered to be more urgent remained the same or even increased (myelopathy, revision surgery and fractures).
The surgical waiting time variable describes the number of days which passed from the indication of surgery until the performance of the operation.
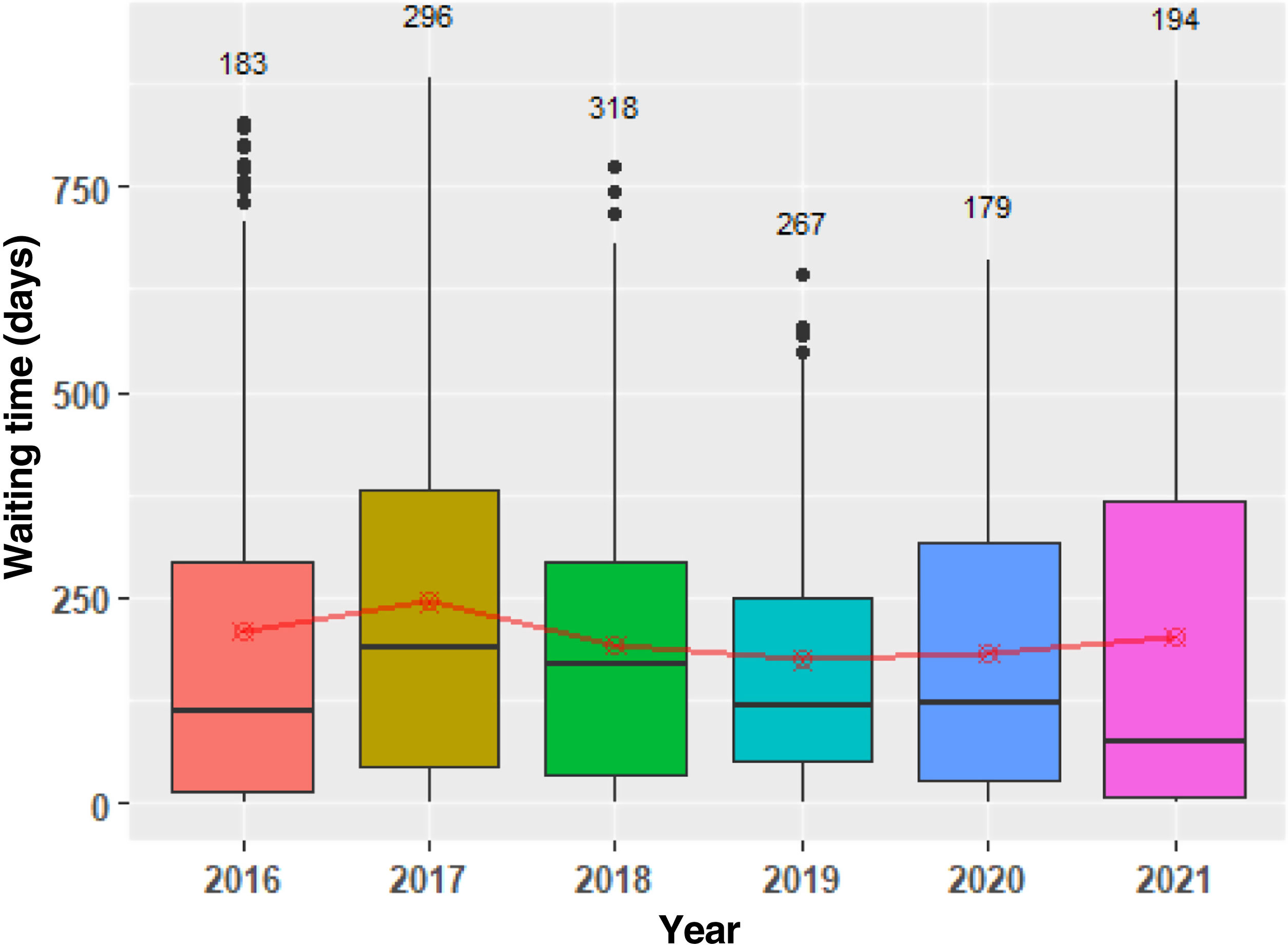
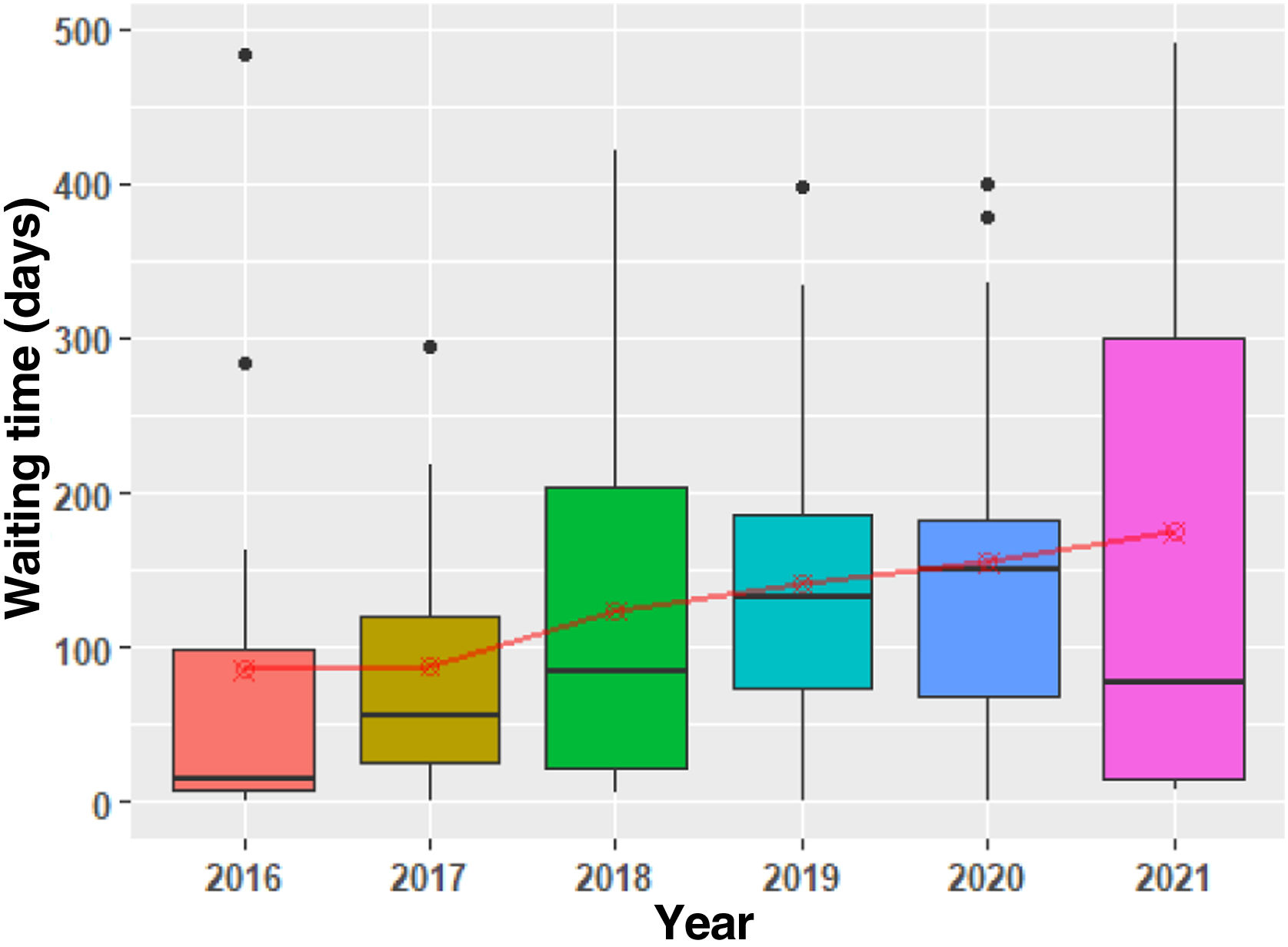
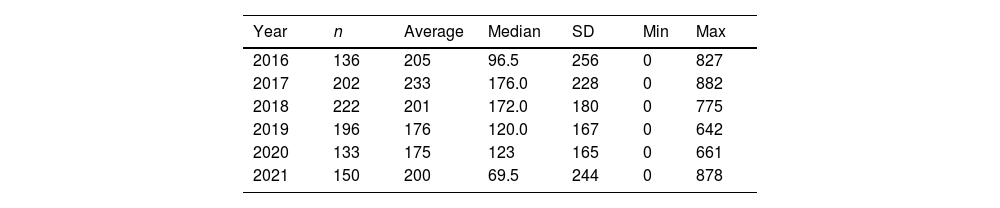
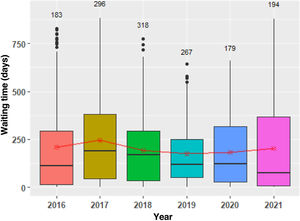
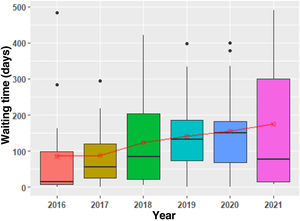
Table 3 shows the evolution of waiting time for the whole sample. It was found to be the shortest in 2019, and in the years of the pandemic the dispersion of the sample increased and the median fell (Table 3, Fig. 2). The waiting times in different years show statistically significant differences (P=.034). This is due to the combination of more urgent surgical operations with short waiting times and the increase in waiting times for less urgent surgery.
Fig. 2 shows a box diagram with the number of surgical operations performed each year at the top, and the evolution of the average in red.
When the above-mentioned pathologies are analyzed, a significant increase may be seen in lumbar pathology.
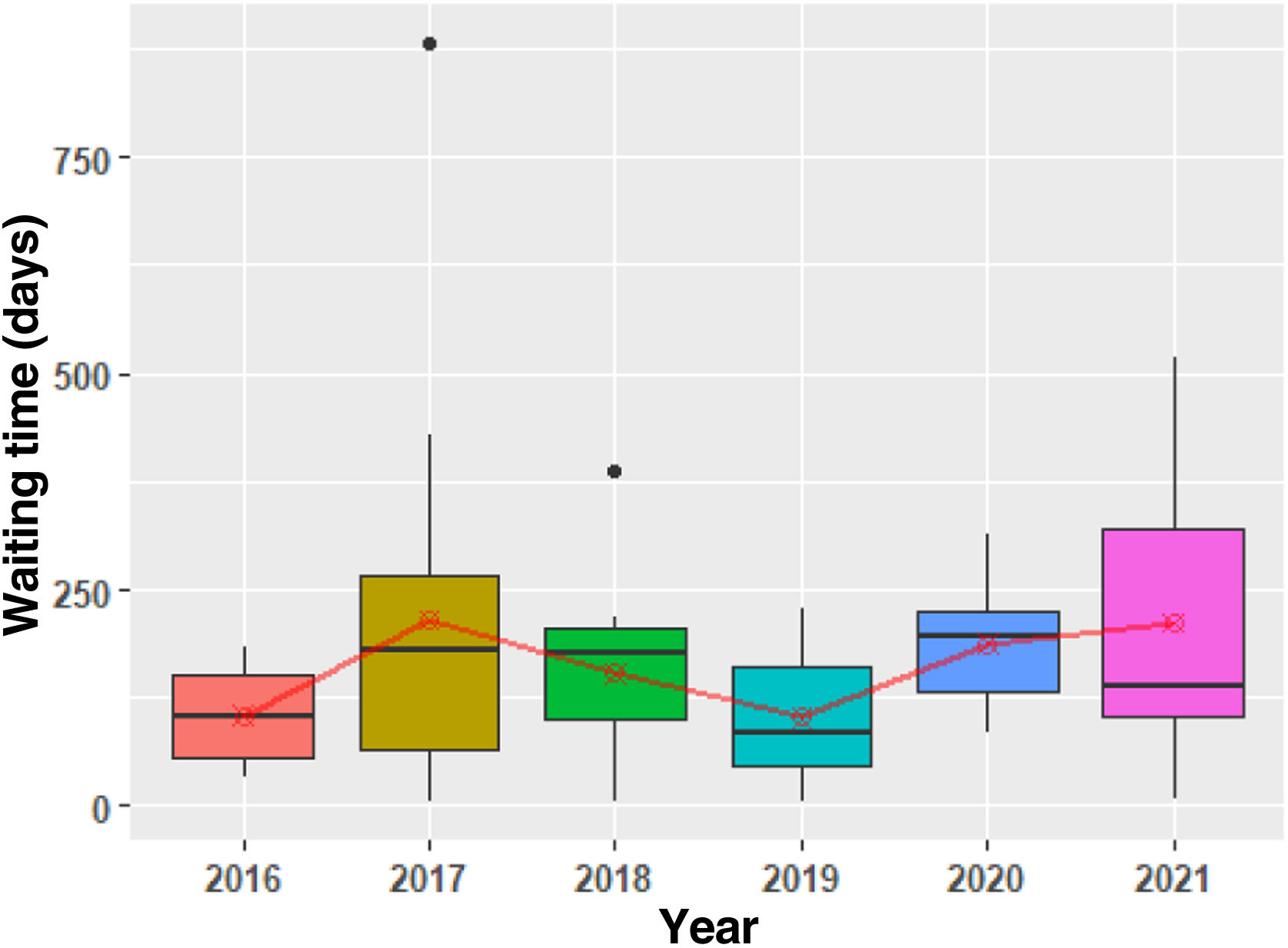
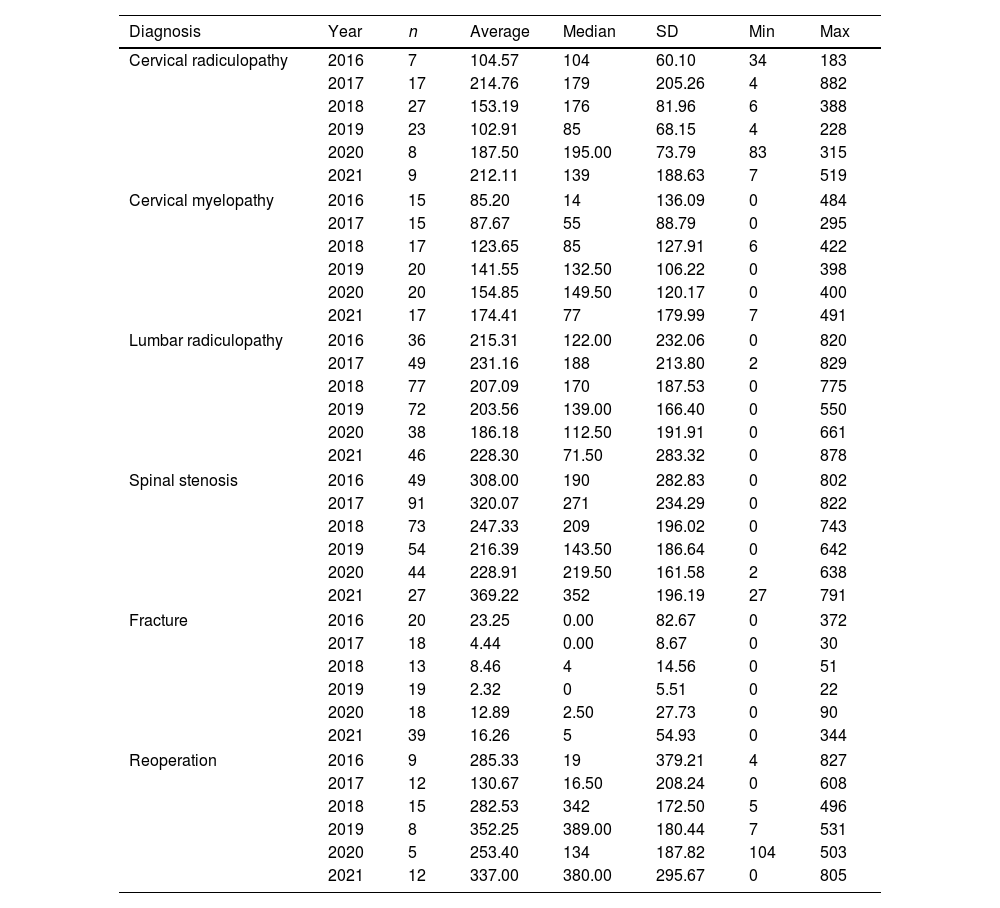
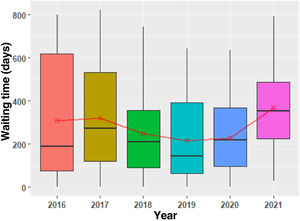
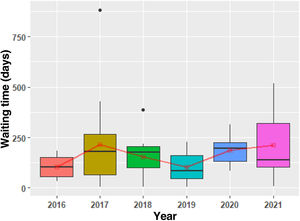
Since 2019 lumbar stenosis has shown an increase in the average and median waiting time (Fig. 3, Table 4), given that this is usually a pathology whose treatment may be delayed.
Description of waiting time per pathology and year.
| Diagnosis | Year | n | Average | Median | SD | Min | Max |
|---|---|---|---|---|---|---|---|
| Cervical radiculopathy | 2016 | 7 | 104.57 | 104 | 60.10 | 34 | 183 |
| 2017 | 17 | 214.76 | 179 | 205.26 | 4 | 882 | |
| 2018 | 27 | 153.19 | 176 | 81.96 | 6 | 388 | |
| 2019 | 23 | 102.91 | 85 | 68.15 | 4 | 228 | |
| 2020 | 8 | 187.50 | 195.00 | 73.79 | 83 | 315 | |
| 2021 | 9 | 212.11 | 139 | 188.63 | 7 | 519 | |
| Cervical myelopathy | 2016 | 15 | 85.20 | 14 | 136.09 | 0 | 484 |
| 2017 | 15 | 87.67 | 55 | 88.79 | 0 | 295 | |
| 2018 | 17 | 123.65 | 85 | 127.91 | 6 | 422 | |
| 2019 | 20 | 141.55 | 132.50 | 106.22 | 0 | 398 | |
| 2020 | 20 | 154.85 | 149.50 | 120.17 | 0 | 400 | |
| 2021 | 17 | 174.41 | 77 | 179.99 | 7 | 491 | |
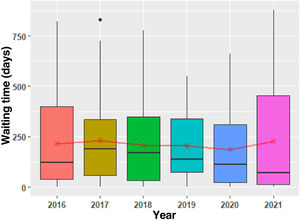
| Lumbar radiculopathy | 2016 | 36 | 215.31 | 122.00 | 232.06 | 0 | 820 |
| 2017 | 49 | 231.16 | 188 | 213.80 | 2 | 829 | |
| 2018 | 77 | 207.09 | 170 | 187.53 | 0 | 775 | |
| 2019 | 72 | 203.56 | 139.00 | 166.40 | 0 | 550 | |
| 2020 | 38 | 186.18 | 112.50 | 191.91 | 0 | 661 | |
| 2021 | 46 | 228.30 | 71.50 | 283.32 | 0 | 878 | |
| Spinal stenosis | 2016 | 49 | 308.00 | 190 | 282.83 | 0 | 802 |
| 2017 | 91 | 320.07 | 271 | 234.29 | 0 | 822 | |
| 2018 | 73 | 247.33 | 209 | 196.02 | 0 | 743 | |
| 2019 | 54 | 216.39 | 143.50 | 186.64 | 0 | 642 | |
| 2020 | 44 | 228.91 | 219.50 | 161.58 | 2 | 638 | |
| 2021 | 27 | 369.22 | 352 | 196.19 | 27 | 791 | |
| Fracture | 2016 | 20 | 23.25 | 0.00 | 82.67 | 0 | 372 |
| 2017 | 18 | 4.44 | 0.00 | 8.67 | 0 | 30 | |
| 2018 | 13 | 8.46 | 4 | 14.56 | 0 | 51 | |
| 2019 | 19 | 2.32 | 0 | 5.51 | 0 | 22 | |
| 2020 | 18 | 12.89 | 2.50 | 27.73 | 0 | 90 | |
| 2021 | 39 | 16.26 | 5 | 54.93 | 0 | 344 | |
| Reoperation | 2016 | 9 | 285.33 | 19 | 379.21 | 4 | 827 |
| 2017 | 12 | 130.67 | 16.50 | 208.24 | 0 | 608 | |
| 2018 | 15 | 282.53 | 342 | 172.50 | 5 | 496 | |
| 2019 | 8 | 352.25 | 389.00 | 180.44 | 7 | 531 | |
| 2020 | 5 | 253.40 | 134 | 187.82 | 104 | 503 | |
| 2021 | 12 | 337.00 | 380.00 | 295.67 | 0 | 805 | |
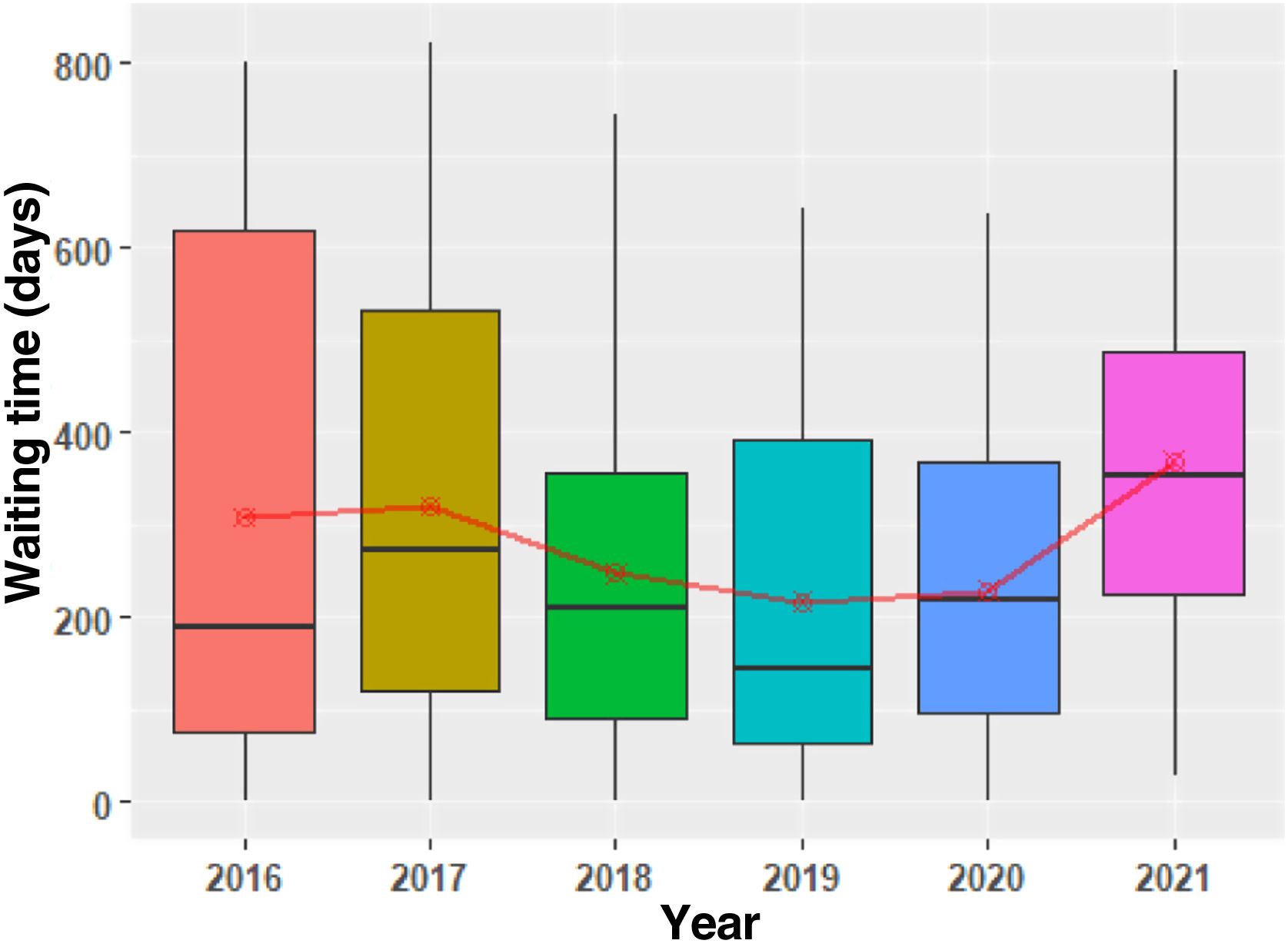
Lumbar radiculopathy includes several pathologies with different degrees of priority. A fall in median waiting time and an increase in the average was found over time, together with increased dispersion of the distribution (Fig. 4, Table 4), showing the combination of urgent and programmed operations.
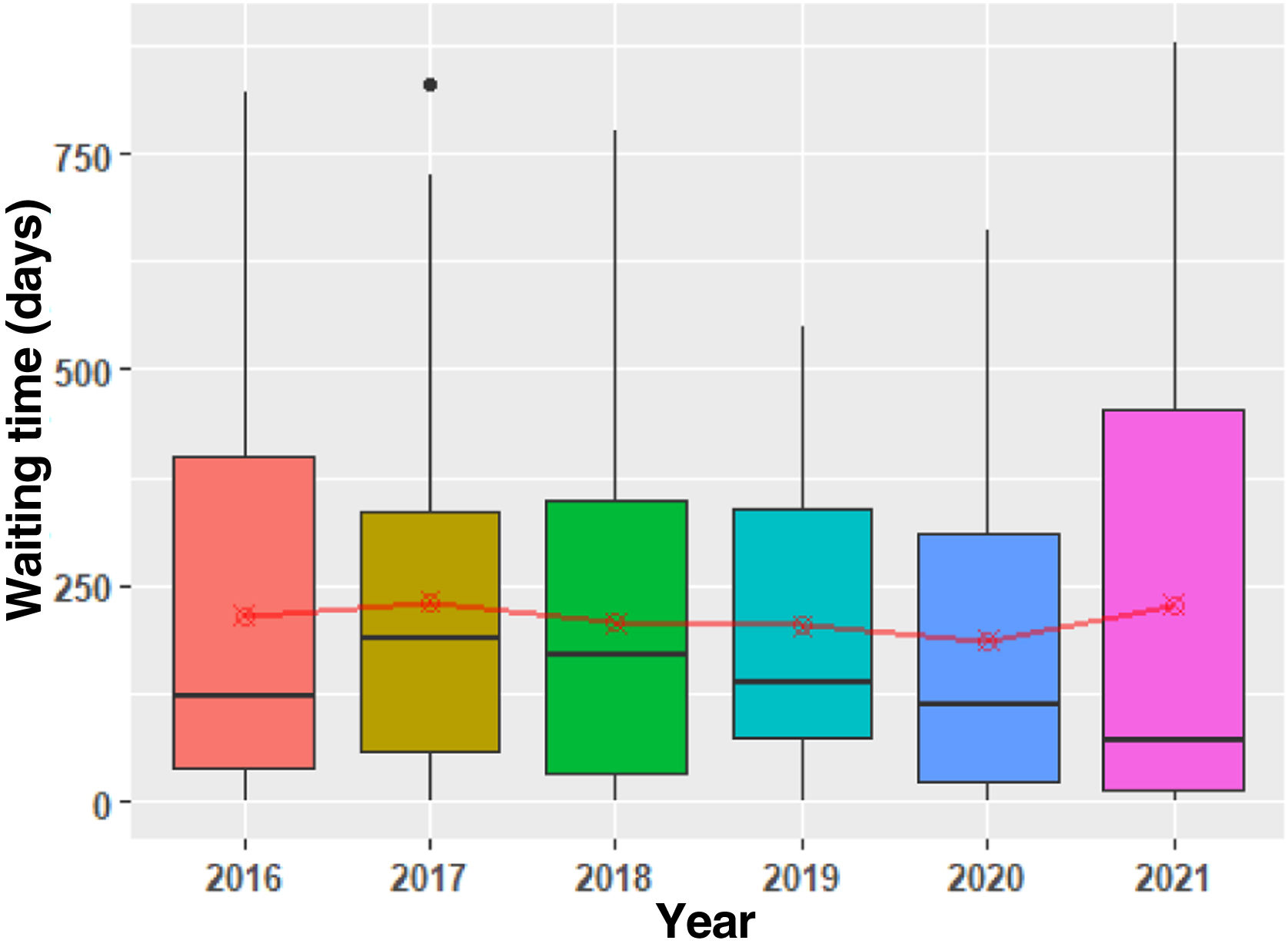
Cervical pathology was also affected by the restrictions.
A progressive increase in the length of waiting time was found in the cervical myelopathy group during the whole series (Fig. 5, Table 4), although in 2021 the median is shorter and there is greater dispersion of the distribution. This was due to the combination of urgent surgical operations (with a shorter waiting time) and the non-urgent ones included in the waiting list.
The cervical radiculopathy group (Fig. 6, Table 4), includes disc hernias with stable or progressive deficit and less urgent degenerative pathology. Before the pandemic a reduction in the waiting time for operations of this type has been achieved, although it subsequently increased. An increase in the dispersion of the distribution was found in 2021 together with a fall in the median (more urgent cases were operated combined with operations included in the waiting list without priority).
Although fractures are a relatively urgent pathology, a slight increase in waiting time was found during the pandemic. This is an indicator of the difficulty in finding an operating theatre and performing the operation, so that these patients remained admitted to hospital. The outlying values are associated with concomitant pathologies which made surgery impossible, such as in patients with multiple trauma (Table 4). Some very extreme values are found which are associated with the treatment of the sequelae of fractures.
The group of reoperations contains a variety of aetiologies, from infections to instrumentation failures (Table 4). During 2020 these operations took place sooner, showing that the ones with the highest priority took place depending on the availability of operating theatres.
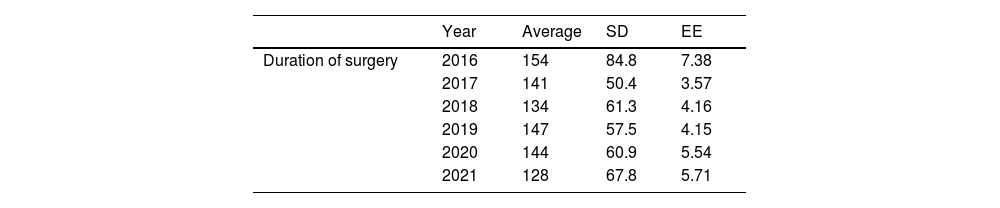
The secondary objectives of this study include analysis of the time taken for surgery as an indicator of the complexity of the operation. The duration of interventions remained stable, with few variations throughout the series, although statistical differences were found when the year 2016 was compared with the years 2018 and 2021 (P=.021) (Table 5). Certain outlying values stand out, and these are associated with the increased complexity of the interventions in question.
Description of the duration of surgery per year.
| Year | Average | SD | EE | |
|---|---|---|---|---|
| Duration of surgery | 2016 | 154 | 84.8 | 7.38 |
| 2017 | 141 | 50.4 | 3.57 | |
| 2018 | 134 | 61.3 | 4.16 | |
| 2019 | 147 | 57.5 | 4.15 | |
| 2020 | 144 | 60.9 | 5.54 | |
| 2021 | 128 | 67.8 | 5.71 |
| 2017 | 2018 | 2019 | 2020 | 2021 | ||
|---|---|---|---|---|---|---|
| 2016 | Mean difference | 13.5 | 20.65 | 7.51 | 10.29 | 26.00 |
| P | 0.403 | 0.037 | 0.900 | 0.788 | 0.009 |
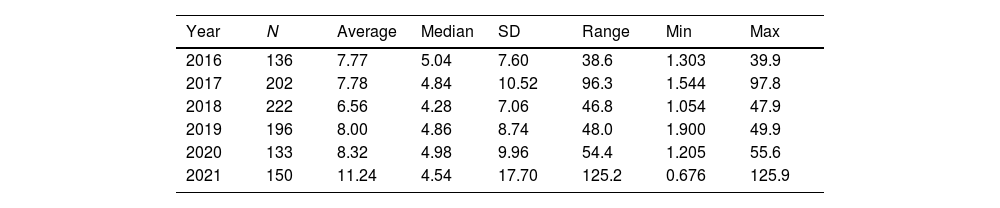
With reference to the duration of hospitalization (Table 6), this was found to increase in the years 2020 and 2021. This is because the use of social resources after discharge from hospital was limited by the restrictions in place, cases of COVID-19 in nursing homes and the increase in hospital stays prior to surgery for some urgent pathologies, due to lack of available operating theatres.
Description of the duration of hospitalization per year.
| Year | N | Average | Median | SD | Range | Min | Max |
|---|---|---|---|---|---|---|---|
| 2016 | 136 | 7.77 | 5.04 | 7.60 | 38.6 | 1.303 | 39.9 |
| 2017 | 202 | 7.78 | 4.84 | 10.52 | 96.3 | 1.544 | 97.8 |
| 2018 | 222 | 6.56 | 4.28 | 7.06 | 46.8 | 1.054 | 47.9 |
| 2019 | 196 | 8.00 | 4.86 | 8.74 | 48.0 | 1.900 | 49.9 |
| 2020 | 133 | 8.32 | 4.98 | 9.96 | 54.4 | 1.205 | 55.6 |
| 2021 | 150 | 11.24 | 4.54 | 17.70 | 125.2 | 0.676 | 125.9 |
Pathology of the spinal column which requires surgery is very prevalent in the general population. Obviously, although public health system waiting lists already existed prior to COVID-19, the pandemic increased the number of patients waiting for spinal column surgery. This was unavoidable, as it was impossible to continue operating as frequently as before, while patients still joined waiting lists, mainly for non-urgent surgery.
The results of the series studied show an increase in dispersion and a fall in the median waiting time for the patients who were operated. This is an indirect indicator that more surgical operations were performed with shorter waiting times because the pathology in question was urgent. Combined with the fact that the elective surgical operations performed accumulated longer waiting times, this caused the dispersion of the sample to increase.
Far from becoming less common during the pandemic, as would seem logical, traumatic spinal column injuries increased in spite of the lock-down and working from home. Although the data do not show this as such, this increase is due to the increase in self-harm and accidents within the catchment area of the hospital during the pandemic.
This study is a retrospective review, and it has some limitations.
The first limitation is the reliability of the codification of diagnoses and the lack of precision of some of the latter. The diagnoses were grouped into the blocks that were analyzed to minimize these effects.
There may also be distortion in the waiting times for patients who were hospitalized, as it is possible that the indication for surgery was not emitted on the same day that they were admitted, as a waiting period for complementary tests or for the availability of surgical resources may have been applied.
The data supplied do not show the waiting period for those patients who have yet to be operated which, in the light of the data analyzed, has notably increased. Moreover, if the indications for surgery remain at the same level as in recent years and the number of operations which can be performed does not change, the current accumulation of waiting time cannot be foreseen to diminish, as it will remain the same or increase.
ConclusionsCOVID-19 had a major impact on every aspect of health care.
Although spinal column surgery continued for pathologies which are considered to be urgent, pathologies which are not considered to be urgent were especially affected, with an increase in the waiting time for treatment.
Level of evidenceLevel of evidence iii.
FundingThis research received no specific grant from financing agencies in the public, commercial or for-profit sectors.
Conflict of interestsThe authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalCEIm - Hospital Universitari Arnau de Vilanova Registration number: CEIC-2635.