Our aim was to describe whether Latarjet's technique affects subscapularis muscle innervation.
Materials and methodsWe studied 12 embalmed shoulders. Subscapularis muscle innervation pattern was registered. Dimensions of the subscapularis at the glenohumeral joint line and the nerves entry point were measured. Horizontal distances from the nerves to the glenohumeral joint line as well as vertical ones to the split were measured before and after Latarjet procedure. A safe zone for the split was designed to avoid damage to subscapularis innervation.
ResultsSubscapularis muscle is innervated by three principal branches: upper, middle, and inferior subscapularis nerves. No statistical differences were found between innervation distances before and after Latarjet procedure. To perform subscapularis split along the muscle safe zone, two thirds’ proportions throughout all the split must be maintained.
ConclusionsSubscapularis muscle has a triple innervation and was not altered after Latarjet procedure. Therefore, Latarjet technique seems to respect subscapularis muscle innervation if its split is placed through the subscapularis muscle safe zone.
El objetivo de este estudio es analizar la relación existente entre la inervación del músculo subescapular y los pasos quirúrgicos de la técnica de Latarjet.
Material y métodoSe realizó un estudio anatómico mediante disección de 12 hombros fijados en formol, y se analizó el patrón de inervación del músculo subescapular. Se midió el tamaño del tendón en la interlínea articular, la distancia cráneo-caudal desde el borde superior al borde inferior del subescapular, en la entrada de los nervios, y la distancia mediolateral, desde los nervios hasta la interlínea articular. Se realizó la técnica de Latarjet y se midieron las distancias horizontales de los nervios subescapulares a la interlínea articular y de los nervios a la división del subescapular. Se describió la zona de seguridad por la que transcurre la división del subescapular sin dañar los nervios.
ResultadosEl músculo subescapular está inervado por 3 ramas del nervio subescapular: superior, medio e inferior, que siguen una distribución constante. No se encontraron diferencias estadísticamente significativas en las distancias de los nervios medidas antes y después de la técnica de Latarjet. Para evitar lesionar los nervios, es preciso realizar la división del subescapular entre los 2 tercios superiores y el tercio inferior a lo largo del músculo.
ConclusiónEl músculo subescapular presenta una triple inervación constante. No hemos apreciado cambios estadísticamente significativos en la inervación tras la cirugía de Latarjet. Por tanto, la técnica de Latarjet parece respetar esta inervación al realizar la división del subescapular en su zona de seguridad.
Among the surgical techniques described for the treatment of anterior shoulder instability, the Latarjet operation has obtained satisfactory clinical results in the medium and long term.1 The Latarjet operation consists of osteotomy and transfer of the coracoid process to the anteroinferior edge of the glenoid. Its stabilising effect is based on the increase in the glenoid surface provided by the bone graft and on the “hammock effect” in abduction and external rotation positions exerted by the conjoint tendon.2 The transfer of the coracoid process is carried out through the horizontal opening of the subscapularis muscle at the junction of the upper two thirds with the lower third and in a direction parallel to its fibres.3 This step through the subscapularis has shown clear advantages over tenotomy or osteotomy of the greater trochin,3,4 but it is considered one of the most technically demanding steps. Some authors have identified minor postoperative complications associated with this technique, such as limitation in internal rotation and atrophy and fatty infiltration of the subscapularis muscle.3–9 Our group has reported excellent clinical outcomes with the Latarjet technique performed by arthroscopy, although in the postoperative image follow-up of the subscapularis muscle, signs of fatty degeneration were detected in the region cranial to the division of its fibres.10–13 We started from the hypothesis that this fatty degeneration found could be a consequence of a partial injury to the innervation of the subscapularis produced during the surgical procedure. The potential neurovascular injuries associated with this surgical technique have been established in different publications.14 Despite this, there is no consensus about the anatomical arrangement of the innervation of the subscapularis15–19 nor has it been analysed in detail how the horizontal division of the subscapularis muscle fibres may affect it.
The objective of this study is to describe in detail the innervation of the subscapularis muscle and analyse the anatomical changes it undergoes during the Latarjet operation. We start from the hypothesis that the recommended level of union between the upper two thirds and the lower third of the muscle fibres of the subscapularis is safe and does not injure any nerve responsible for the innervation of the muscle.
Material and methodsIn this research project, the 12 shoulders of 6 corpses fixed in formalin with a standardised embalming were studied, which had been donated under the legal requirements demanded by the Department of Anatomy, Histology and Neuroscience of the Faculty of Medicine of the Autonomous University of Madrid. All had undamaged shoulder anatomy. Any macroscopic sign of pathology or previous surgery that could alter the anatomy of the shoulder girdle was considered an exclusion criterion.
Superficial and deep dissection of the innervation of the subcapularis muscleThe dissection was carried out following the same order in all corpses. From an extended deltopectoral approach over the clavicle, the anterior deltoid and pectoralis major muscles were fully exposed. The anterior deltoid was disinserted at its clavicular and acromial origins, and the muscle was retracted while preserving its distal insertion. After identifying the bicipital groove, the insertion of the subscapularis muscle was defined by blunt dissection. After continuing this dissection distally, the insertion of the pectoralis major muscle was identified and rejected medially, sectioning the innervation and vascularisation on its deep surface. The coracoid process was dissected, releasing the insertions of the coracoclavicular, coracoacromial and coracohumeral ligaments, as well as the insertion of the pectoralis minor muscle, which was rejected medially. Next, a blunt dissection of the conjoint tendon was performed until the brachial plexus was accessed. To avoid injuries to the plexus, the dissection began at the musculocutaneous nerve at the level of its entry into the coracobrachialis muscle as it was easily identifiable given its more superficial position, and progressed proximally towards the fascicles, avoiding traction on the nerves. This allowed us to systematically identify all the nerves and fascicles that make up the brachial plexus, and especially those involved in the innervation of the subscapularis. With proximal dissection of the musculocutaneous nerve, at the level of the lateral fasciculus, the axillary artery was exposed along with the radial nerve. Both structures were carefully separated, and after completely identifying the radial nerve, the distal and proximal dissection was continued in this way to locate the axillary nerve and the posterior fascicle of the plexus. Nerves arising from the posterior fasciculus were isolated and labelled. Following the most superior divisions of the plexus, the upper trunk from which the suprascapular nerve arises was identified. This was the point considered to be the end of the dissection. Once the plexus had been dissected, the detailed dissection of the entire anterior face of the subscapular muscle from lateral to medial was carried out. The fat was removed, as well as the connective tissue to expose all possible muscle. This dissection was accompanied with the identification and dissection of the nerves that innervate the subscapular muscle.
LatarjetThe Latarjet technique was carried out according to the description of Young et al.1 After performing the osteotomy of the coracoid process about 25mm from its anterior end, it was transferred with the conjoint tendon to the anterior surface of the glenoid through a horizontal opening of the subscapularis made at the junction between the upper two thirds with the lower third of the muscle at the level of the glenohumeral joint interline. In order to maintain the proportion at the junction of the upper two thirds with the junction of the lower third, the division of the subscapularis muscle was calculated both at the level of the joint interline and at the entrance of the nerves into the muscle. Subsequently, the division was completed with blunt scissors, joining both points and laterally until the insertion of the muscle in the lesser tuberosity. Once passed, the coracoid graft was fixed on the anterior cortex of the glenoid neck using an electric drill (Bosch®, Stuttgart, Germany), a 3.2mm drill bit (Dexter®, China), and two partial 4.5mm lag screws (Dexter®, China). In all bodies it was confirmed that the graft was fixed in the lower half of the neck and with its lateral surface at the same level as the glenoid articular surface.
Study of the dimensions and innervation of the subscapularis muscleThe number, origin and entire anatomical distribution until their entry into the muscle of the different nerves responsible for the innervation of the subscapularis muscle in each shoulder were recorded preoperatively.
Since in the Latarjet technique the coracoid graft is introduced into the joint through the division of the muscle at the junction of the upper two thirds with the lower third,1 the anterior joint interlines and the cranial and caudal borders of the muscle were taken as references to measure the distances of the subscapularis nerves and thus subsequently evaluate their modifications during surgery. The objective of these anatomical references was, firstly, to know the distribution of the nerves and the modifications experienced during surgery at the level of the anatomical area where the coracoid graft is introduced and fixed. Secondly, we considered it important to analyse how the anatomy of the nerves was modified in relation to the muscle they innervate. Theoretically, the superior and inferior borders of the subscapularis are hardly modified in the Latarjet operation.
With respect to these anatomical references, the following measurements were carried out on the anterior surface of the subscapularis before and after surgery (Fig. 1).
(A) Measurement outline. Yellow dot: superior subscapular nerve. Blue dot: median subscapular nerve. Red dot: inferior subscapular nerve. 1: craniocaudal distance at the level of the interline (ScIn); 2: craniocaudal distance at the level of the nerves (ScNv); 3: superior subscapular nerve distance to the interline (Sint); 4: middle subscapular nerve distance to the interline (MInt); 5: inferior subscapular nerve distance to the interline (IInt). (B) Measurement outline. Yellow dot: superior subscapular nerve. Blue dot: middle subscapular nerve. Red dot: inferior subscapular nerve. 6: subscapularis muscle division; 7: distance superior subscapular nerve to division (SupSplit); 8: middle subscapular nerve to split distance (MedSplit); 9: distance inferior subscapular nerve to division (ISplit).
- -
Craniocaudal width of the subscapularis muscle at the level of the joint interline measured from the upper edge of the subscapularis muscle to its lower edge (ScIn).
- -
Craniocaudal width of the subscapularis muscle at the level of the entrance of the subscapularis nerves measured from the upper edge of the subscapularis muscle to its lower edge (ScNv).
- -
Vertical distance of the subscapular nerves to a line corresponding to the division of the upper two thirds with the lower third of the muscular belly of the subscapularis (upper: SupSplit; middle: MedSplit; lower: ISplit).
- -
The distance of each subscapular nerve to the joint interline was measured (superior: Sint; middle: MInt: lower: Iint).
All measurements were made in millimetres (mm) with the consensus of two observers (IC and AA), with the shoulder in anatomical neutral rotation and using an analogue calliper of the “vernier calliper” type with a precision of .02mm (Dexter®, China).
The recording of the nerve anatomy was completed with digital photographs of the anterior aspect of the subscapularis muscle in all bodies at the end of the anatomical dissection, before performing the Latarjet operation and once it was completed. These photographs were used for illustrative purposes and to recover the image in the event that the investigation required it.
Statistical studyAll statistical analyses were performed with the R programme version 4.0.5 (R: A language and environment for statistical computing, R Foundation for Statistical Computing®, Vienna, Austria). Pre- and post-surgical values are described with median and interquartile range (IQR). The differences between the pre and post values are described with the difference in medians and their 95% confidence interval, and the comparison is made using the Wilcoxon signed rank test.
ResultsOf the six corpses studied, four were women and two were men. The median age was 74 years (IQR: 12.5), the median weight was 80kg (IQR: 22.5) and the median height was 170cm (IQR: 3.8). The 12 shoulders showed a constant pattern of innervation of the subscapularis muscle formed by three branches corresponding to the superior, middle and inferior subscapular nerves. Both the superior subscapularis and middle subscapularis nerves were independent branches emerging from the posterior fasciculus in all 12 shoulders (100%). The pattern of origin of the inferior subscapular nerve was inconsistent. In six shoulders (50%) it started from the posterior fasciculus, in four (34%) it started from a common trunk together with the thoracodorsal nerve, and in two (16%) it was a branch that started from the axillary nerve (Figs. 2–5). Table 1 shows all the results of the described measures.
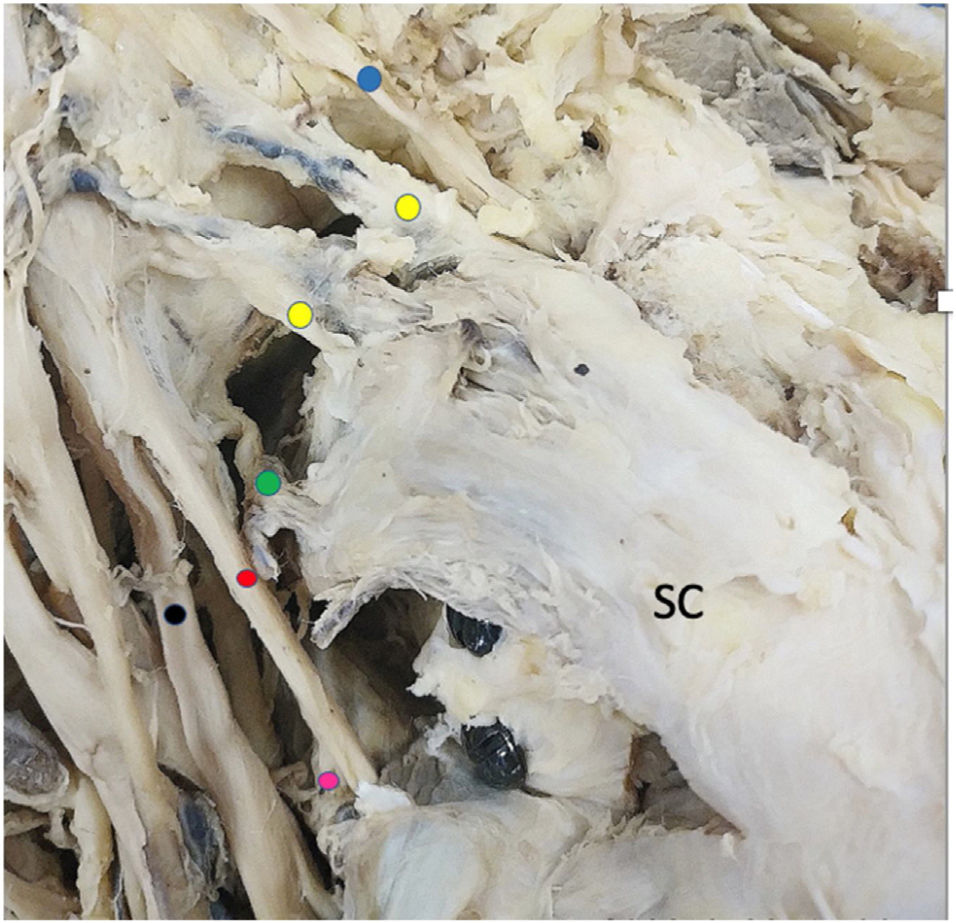
Detail of branches of the posterior fascicle, anterior face. SC: subscapularis. Blue dot: suprascapular nerve. Yellow dot: superior subscapular nerve. Green dot: middle subscapular nerve. Red dot: axillary nerve. Fuchsia point: inferior subscapular nerve. Black point: radial nerve.
Detail of branches of the posterior fascicle, anterior face. SC: subscapularis. Blue dot: suprascapular nerve. Yellow dot: superior subscapular nerve. Green dot: middle subscapular nerve. Red dot: axillary nerve. Fuchsia point: inferior subscapular nerve. Black point: radial nerve.
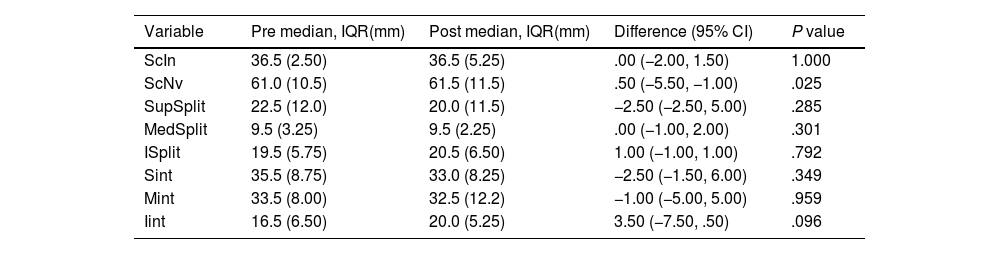
Table of pre- and post-surgery comparison results.
| Variable | Pre median, IQR(mm) | Post median, IQR(mm) | Difference (95% CI) | P value |
|---|---|---|---|---|
| ScIn | 36.5 (2.50) | 36.5 (5.25) | .00 (−2.00, 1.50) | 1.000 |
| ScNv | 61.0 (10.5) | 61.5 (11.5) | .50 (−5.50, −1.00) | .025 |
| SupSplit | 22.5 (12.0) | 20.0 (11.5) | −2.50 (−2.50, 5.00) | .285 |
| MedSplit | 9.5 (3.25) | 9.5 (2.25) | .00 (−1.00, 2.00) | .301 |
| ISplit | 19.5 (5.75) | 20.5 (6.50) | 1.00 (−1.00, 1.00) | .792 |
| Sint | 35.5 (8.75) | 33.0 (8.25) | −2.50 (−1.50, 6.00) | .349 |
| Mint | 33.5 (8.00) | 32.5 (12.2) | −1.00 (−5.00, 5.00) | .959 |
| Iint | 16.5 (6.50) | 20.0 (5.25) | 3.50 (−7.50, .50) | .096 |
95% CI: 95% confidence interval; IInt: inferior subscapular nerve distance to the interline; IQR: interquartile range; ISplit: inferior subscapular nerve distance to division; MedSplit: middle subscapular nerve to split distance; MInt: middle subscapular nerve distance to the interline; ScIn: craniocaudal distance at the level of the interline; ScNv: craniocaudal distance at the level of the nerves; Sint: superior subscapular nerve distance to the interline; SupSplit: distance superior subscapular nerve to division.
No statistically significant differences were found between the horizontal measurements of the nerves to the joint interline or the vertical distance of the nerves to the pre- and post-surgical division of the subscapularis muscle. A significant difference was detected between the vertical measurement of the subscapularis muscle (ScNv) pre- and post-surgery.
The number of branches and nomenclature of the subscapular nerves remains unclear or consistent in studies published to date. The main anatomical finding of this study is that all the dissected cadavers presented a triple innervation formed by the superior, middle and inferior subscapular nerves. Our findings differ from those published in the literatura,15,16,19–21 which report innervation patterns cantered on one superior and one inferior nerve. In contrast, Leschinger et al.18 and Kato22 already raised the possibility of a triple innervation, although in many cases subject to branches of the superior subscapular nerve and not as a direct branch of the posterior fasciculus as described in our dissections. Detailed dissection of all the branches that innervate the subscapularis muscle requires the removal of abundant fatty and connective tissue over the muscle belly. The branches that innervate the subscapularis muscle are millimetres so they could be easily disinserted when removing the tissue over the muscle, thus giving the image of only two branches.
Regarding the variability of the inferior subscapular nerve, the findings of this anatomical study are consistent with the great variability reported regarding its origin, but differ in the most predominant patterns reported.16,18,20,22,23 Despite this variability, the innervation of the lower portion was distributed more homogeneously among the possible origins, and came from the axillary nerve in 16% of the dissections, as opposed to the 90% reported by Bustamante et al.23 or the 55% reported by Kerr et al.20
Regarding the study of the references of the Latarjet operation and its relationship with the nerves of the subscapularis muscle, in this investigation measurements were made of the distances of the nerves to the joint interline and the division of the subscapularis muscle both before and after the operation. These are two references clearly visible during surgery, open and arthroscopic, not used to date for this surgery and that are of anatomical and surgical interest, since it is the anatomical region where the intervention is performed and, therefore, where the greatest risk resides of a possibility that the anatomy of the nerves may be altered. In this study it was found that the horizontal distances of the nerves from the joint line did not vary significantly for any nerve. Regarding the vertical distances of the nerves to the division of the subscapularis, both pre- and post-surgery, these allow us to appreciate how close the nerves are to this critical step of the surgery. The closest median distance found was 9.5mm for the middle subscapular nerve, with the closest observation being only 4mm. Therefore, the medial subscapularis could be affected by small changes in the division of the muscle. No vertical distance from the nerves to the muscle division was significantly modified after the Latarjet technique. A statistically significant difference was detected in the measurement of the craniocaudal distance of the subscapularis muscle at the level of the entry of the subscapularis nerves (ScNv) pre- and post-surgery. This small increase in the distance between the upper and lower edges of the subscapularis muscle could be related to the effect of the division of the muscle on a devitalized tissue without muscle tone, as well as to the beach chair position of the dissection and the effect of gravity on the tissue. This minimal increase, although statistically significant, should not be clinically relevant.
The division of the subscapularis muscle could be related to the decrease in internal rotation strength observed during the first postoperative year in patients operated on using the Latarjet technique reported by our group.10 This loss of strength in internal rotation could be due to an inadvertent injury to the subscapular nerves during the division of the muscle if the extension and orientation of the division is not carried out following the proportionality of the upper two thirds with the lower third throughout the entire surface of the subscapularis muscle, as described.
With the findings of this study, a safety zone can be established to avoid damage to the innervation of the subscapularis muscle. This area corresponds to the space that exists from the middle subscapular nerve to the inferior subscapular nerve, the area above the muscular belly where no neurovascular structures were observed in any of the dissected cadavers. For the division of the subscapularis to enter this area, it is essential to preserve the proportionality of the upper two thirds with the lower third throughout the entire division of the muscle. In this way we performed a division with a downward inclination in a lateromedial direction and parallel to the inferior border of the subscapularis muscle (Fig. 6). Other anatomical studies have also attempted to characterise safety zones around the subscapular nerves. Leschinger et al.18 provides, for example, information on the distances of the nerves from the myotendinous junction and the base of the coracoid, two references that are difficult to see during open or arthroscopic surgery. Walley et al.,21 for their part, reported a safe zone for the inferior subscapular nerve, but their injury could not be the only cause of the observed deficit since they did not evaluate the middle subscapular nerve. In contrast, Valencia et al.10 show how the most affected portion corresponds to the upper area of the subscapularis muscle, with a predominant innervation of the superior and middle subscapular nerves. The existence of so much variability reported regarding the origin of the inferior subscapular nerve and accessory branches seems to grant the inferior region of the subscapularis muscle some protection after its approach.
Our study is not without limitations. The use of a short series of 12 shoulders is justified by the obvious and inherent difficulties of performing studies on cadavers. Although, given the similarity of our results with previous publications, an increase in the sample size does not seem necessary. It is possible that due to formalin fixation, mobilisation of the structures is difficult and does not reproduce the exact elasticity of the muscle. To avoid damage to the shoulder structures after fixation, the study was performed in an anatomical position with the glenohumeral joint in neutral rotation. More studies are needed with cadavers with other fixation systems that allow these measurements to be analysed in shoulder abduction and external rotation. All measurements were made in the coronal plane and, therefore, variations in the superior and middle subscapular nerves in the axial plane secondary to the discreet displacement of the upper portion of the muscle once fixed cannot be ruled out. However, it is very unlikely that such a displacement could have consequences, given that it is small, and occurs on the deep surface of the muscle, and to date there has been no report of it in the literature. Finally, the median age of the cadavers used is far from the target population in which this technique is performed, so aspects such as the quality and volume of the muscle could be modified.
ConclusionThe subscapularis muscle has a constant triple innervation that corresponds to the superior, middle and inferior subscapular nerves. In this study, no statistically significant changes were found in the innervation of the subscapularis muscle after shoulder stabilisation with the Latarjet technique. There is a safe zone on the subscapularis muscle between the middle and inferior subscapularis nerve, accessible if the proportions of the subscapularis muscle are preserved to carry out the division of its fibres. The proximity of the subscapularis division, despite the proposed modification, could be the cause of the internal rotation strength deficiencies observed after the subscapularis approach. However, more studies are required to dynamically contrast the relationship of the nerves with the critical steps of this surgery.
Level of evidenceLevel of evidence IV.
FundingThe study has been conducted thanks to a financial grant provided by the Foundation of the Spanish Society of Orthopaedic Surgery and Trauma Research Initiation Projects Fundación SECOTconvened in 2019.
Conflict of interestsThe authors have no conflict of interests to declare.
Our thanks to Ignacio Mahillo Fernández and Camino Braojos Rodríguez.