The purpose of this study was to analyze midterm functional outcomes and tendon integrity in patients treated with in situ arthroscopic repair of Partial Bursal Rotator Cuff Tears (PBRCTs) without acromioplasty.
Material and methodsSixty two patients were included. Clinical assessment consisted of glenohumeral range of motion measurement and the American Shoulder and Elbow Surgeons (ASES) score. Pain was rated by using a visual analog scale (VAS). A postoperative ultrasound image control was performed at a minimum 5 years follow up to assess tendon integrity.
ResultsMean age was 57.2 years (range, 44–77 years) and mean follow up was 7 years (range of 5–9 years). Significant improvements in range of motion, functional outcomes and pain were observed postoperatively (p < .0001). The ASES score improved from 46.5 to 90.2; and the VAS improved from 6.5 to 1.73 (p < .0001). Fifty six patients (90%) performed ultrasound evaluation at the end of follow up. Fifty-one patients (91%) presented tendon integrity on ultrasound. Five patients presented re-tears (9%). Three patients (5%) had a complete tendon re-tear and two patients (4%) had a partial re-tear. No difference in range of motion or functional outcomes were found between patients with intact tendon and those who had re-tears.
ConclusionsIn the midterm follow-up, arthroscopic in situ repair PBRCTS without acromioplasty showed excellent functional outcomes and high healing rates in most patients with low complication rates.
Analizar la cicatrización mediante ecografía y el seguimiento funcional a mediano plazo de pacientes con rupturas parciales bursales del manguito rotador (RPBMR) con reparación in situ sin acromioplastia.
Materiales y métodosSe evaluaron 62 pacientes. Se realizó la medición del rango de movimiento y la puntuación en el score de American Shoulder and Elbow Surgeons (ASES). El dolor se registró usando una escala visual análoga (EVA). Se valoró ecográficamente la reparación con un mínimo de seguimiento de 5 años.
ResultadosLa edad promedio fue de 57,2 años (rango de 44 a 77 años) y el seguimiento promedio, de 7 años (rango de 5 a 9 años). Todos los parámetros del rango de movimiento activo mejoraron significativamente (p < 0,0001). El puntaje de ASES mejoró de 46,5 a 90,2 y los puntajes EVA mejoraron de 6,5 a 1,73 (p < 0,0001). Un total de 56 pacientes (90%) realizaron control ecográfico al final del seguimiento; 51 presentaron integridad del tendón (91%) en la ecografía. Cinco pacientes presentaron re-roturas (9%); 3 tuvieron una re-rotura completa del tendón (5%) y 2 una re-rotura parcial (4%). No hubieron diferencias funcionales o del rango de movilidad significativas entre aquellos pacientes con el tendón intacto y los que presentaron re- roturas.
ConclusionesA mediano plazo, la reparación in situ artroscópica de RPBMR demostró excelentes resultados funcionales en la mayoría de los pacientes con baja tasa de complicaciones. Estos mantienen un alto índice de cicatrización en el tiempo.
Partial rotator cuff tears (PRCT) are among the most common shoulder injuries, with a prevalence that increases with age but represent 20% of asymptomatic individuals overall.1 Ellman classified these lesions according to their location as partial articular, bursal and intratendinous and, in turn, into grades according to the thickness of the tendon involved.2 Both intrinsic3 (degeneration of the rotator cuff fibres, impaired local vascularisation of the tendon) and extrinsic4 (repeated microtrauma, subacromial friction syndrome) causes of rotator cuff tears have been described. Among these, subacromial friction is a widespread pathophysiological mechanism and a target for surgical treatment5 (subacromial decompression by acromioplasty). Repeated microtrauma resulting from internal impingement between the glenoid and supraspinatus tendon has been postulated as another extrinsic mechanism, especially in young patients and athletes presenting with articular PRCT.6 Several techniques have been described for the treatment of partial bursal rotator cuff tears (PBRCT). These include acromioplasty, debridement of the lesion with or without associated acromioplasty, and repairs using a minimally invasive approach or by arthroscopy with or without associated acromioplasty.7–10
Treatment of these injuries generally begins conservatively for a period of 3–6 months. Factors such as tendon involvement greater than 50%, tears located on the bursa and dominant arm injuries were associated with failure of non-surgical treatment.11 Furthermore, biomechanical studies have shown that in the presence of a partial tendon injury, the strain patterns in the remaining healthy tissue are altered, thereby involving the fibres surrounding the rear subjected to overload.12 In turn, progression from symptomatic PRCT to complete rotator cuff tears has been reported in up to 50% of cases.12,13 Currently, patients with fibre involvement >50% of thickness (grade III) are candidates for early surgical treatment. Tendon healing is the primary goal of surgery and essential for both surgeon and patient, as it affects good postoperative clinical outcomes.14 Studies analysing the rate of healing after in situ repair of PBRCT report re-tear rates ranging from 8% to 16% at short-term follow-up (minimum follow-up of 2 years).15
To our knowledge, there are no studies that report medium-term structural outcomes (minimum follow-up of 5 years) of repair of these injuries without acromioplasty. Therefore, the aim of this study was to assess the functional and structural outcomes of patients with arthroscopic PBRCT repair with a minimum follow-up period of 5 years without acromioplasty. We hypothesised that patients with PBRCT undergoing arthroscopic repair will have a significant improvement in function with a re-tear rate like that reported in the literature that is sustained in the medium term.
Materials and methodsPatient selectionWe retrospectively assessed all patients treated with arthroscopic repair of PBRCT in the period from January 2009 to January 2013 in our institution. Patients with: (1) a minimum of 3 months unresponsive to conservative treatment, which entailed modifications to daily activities associated with symptomatic treatment with non-steroidal anti-inflammatory drugs and physical therapy; (2) partial bursal rotator cuff lesions with involvement of more than 50% of the tendon thickness (or >6 mm) diagnosed by magnetic resonance imaging (MRI) and confirmed intraoperatively. The exclusion criteria were as follows: (1) previous surgeries to the affected shoulder; (2) patients who underwent procedures associated with rotator cuff repair.
Clinical and imaging evaluationThe patients were assessed pre- and postoperatively by a physiotherapist specialising in shoulder pathology who did not know the diagnosis, or the intervention performed. Postoperative follow-up was performed at 3, 6 and 12 months, and annually thereafter. All patients were contacted at final follow-up after a minimum period of 5 years. Only the final follow-up assessment was used for data analysis in this study.16
Clinical assessment consisted of active range of motion (ROM) measurement using a goniometer and American Shoulder and Elbow Surgeons Score (ASES). Pain was recorded using the visual analogue scale (VAS); a score of 0 indicates no pain, and 10 points indicates the worst possible pain.
All the patients underwent preoperative X-rays (anterior–posterior, scapular Y) and MRI; the latter confirming a PBRCT. Partial ruptures were described according to Ellman’s classification.2
A postoperative follow-up ultrasound was performed at the minimum 5-year follow-up to assess the structural integrity of the repaired tendon. All ultrasound examinations were performed by an imaging specialist with more than 10 years of experience in musculoskeletal shoulder ultrasound.
The examination was performed with the patient supine on the examination table. A standard systematic ultrasound examination of the shoulder was performed to assess the supraspinatus, infraspinatus, and subscapularis tendons in the longitudinal and transverse planes.
The research protocol for the following study was approved by our institution’s ethics and research committee (IRB 3594).
Surgical techniqueAll patients were operated in the beach chair position. Diagnostic arthroscopy of the glenohumeral joint was performed through a posterior portal in all cases to identify the lesion and determine the integrity of the joint face of the supraspinatus. A lateral subacromial visualisation portal and an anterolateral portal were then created to perform the wide bursectomy with radiofrequency until the partial bursal lesion was identified.
The lateral portion of the supraspinatus insertion footprint was measured using a palpator of known size. The thickness involved and the width of the lesion were recorded. Partial bursal lesions involving more than 6 mm of the total thickness of the supraspinatus tendon were repaired. Lesions less than 1 cm wide were repaired using a harpoon. Lesions with a width greater than 1 cm were repaired using 2 harpoons. All lesions were repaired with single stitches with preservation of undamaged joint fibres. BioComposite Corkscrew FT Suture Anchor 5.5 mm harpoons (Arthrex) were used for the repair. Two harpoons were used in two patients and one harpoon in 60 patients. None of the patients underwent subacromial decompression and distal clavicle resection.
Postoperative managementImmobilisation with a sling for 4 weeks was indicated. After the first week the patients started rehabilitation consisting of gradual passive mobility and pendular exercises. Between 2 and 3 weeks they started assisted active mobility exercises. Muscle strengthening exercises were started when the patients were able to perform anterior flexion above shoulder level, usually at 4–6 weeks following surgery. Heavy manual and overhead tasks were allowed once full mobility and strength had been regained, usually at around 6 months.
Statistical analysisContinuous variables are presented as means with their respective standard deviations, while categorical variables are expressed as absolute and relative frequencies. STATA version 14 software (Stata Corporation, College Station, Texas, USA) was used for the statistical analysis. A p-value less than .05 was considered statistically significant.
ResultsOf the 73 patients who underwent consecutive arthroscopic partial repairs over the study period, 11 were excluded. Five patients underwent concomitant procedures (3 biceps tenotomies and one tenodesis, and one patient underwent subscapularis repair). Six patients did not complete the minimum 5-year follow-up and were considered lost to follow-up. The final evaluation was performed in 62 patients, resulting in a 91% follow-up rate for the series.
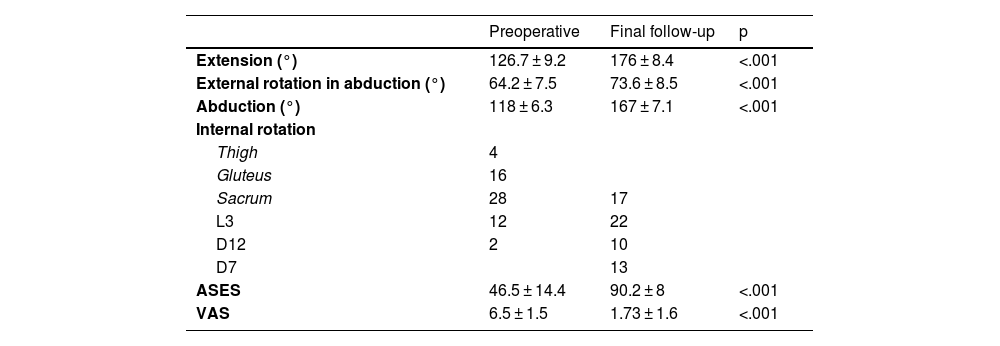
Of the 62 patients studied, 32 were male and 30 were female, with a mean age of 57.2 years (range, 44–77 years). The operated shoulder was the dominant shoulder in 36 cases (58%). The mean follow-up was 7 years (range, 5–9 years). At the end of follow-up, we observed a statistically significant improvement in range of motion and in all functional scores assessed (Table 1). The ASES score improved from 46.5 (range, 11–68) preoperatively to 90.2 (range, 77–100) at the last follow-up. VAS decreased from 6.5 points (range, 4–9) preoperatively to a mean value of 1.73 points (range, 0–6) postoperatively.
Comparative pre-and post-operative functional and range-of-motion outcomes.
| Preoperative | Final follow-up | p | |
|---|---|---|---|
| Extension (°) | 126.7 ± 9.2 | 176 ± 8.4 | <.001 |
| External rotation in abduction (°) | 64.2 ± 7.5 | 73.6 ± 8.5 | <.001 |
| Abduction (°) | 118 ± 6.3 | 167 ± 7.1 | <.001 |
| Internal rotation | |||
| Thigh | 4 | ||
| Gluteus | 16 | ||
| Sacrum | 28 | 17 | |
| L3 | 12 | 22 | |
| D12 | 2 | 10 | |
| D7 | 13 | ||
| ASES | 46.5 ± 14.4 | 90.2 ± 8 | <.001 |
| VAS | 6.5 ± 1.5 | 1.73 ± 1.6 | <.001 |
ASES: American Shoulder and Elbow Surgeons; °: degrees; VAS: visual analogue scale.
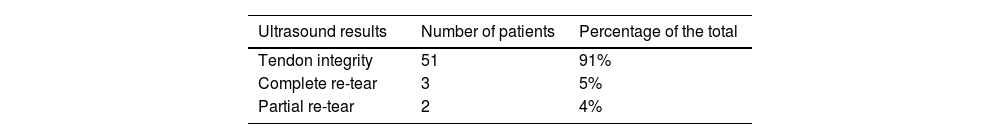
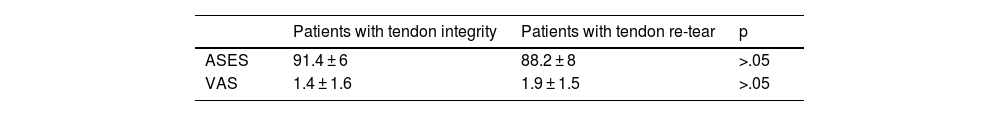
Ninety-two percent of the patients reported satisfactory or very satisfactory outcomes (27 very satisfactory, 30 satisfactory), and 8% (5 patients) reported fair outcomes. No patient considered their outcome poor. Of the 62 patients assessed at the final follow-up, 56 (90%) patients were monitored by ultrasound with a minimum follow-up of 5 years. Fifty-one patients (91%) had tendon integrity; 3 patients (5%) had complete tendon re-tear, and 2 patients (4%) had partial tendon re-tear (Table 2). We found no significant differences in range of motion and functional outcomes between the patients with tendon integrity on follow-up ultrasound and the patients who had re-tears (Table 3). Patients with tendon integrity had a mean ASES value at the last follow-up of 91.4 points (range, 85–100) and a mean VAS of 1.4 (range, 0–2); patients with re-tears at the final follow-up ultrasound had an average ASES value of 88.2 points (range, 77–95) and VAS of 1.9 points (range, 1–3).
Comparative functional outcomes between patients with ultrasound-guided tendon integrity and tendon rupture.
| Patients with tendon integrity | Patients with tendon re-tear | p | |
|---|---|---|---|
| ASES | 91.4 ± 6 | 88.2 ± 8 | >.05 |
| VAS | 1.4 ± 1.6 | 1.9 ± 1.5 | >.05 |
ASES: American Shoulder and Elbow Surgeons; VAS: visual analogue scale.
The main finding of this study was that at mid-term follow-up (mean 7 years), patients treated for partial bursal rotator cuff injuries with arthroscopic repair without acromioplasty had excellent functional outcomes in most cases that were maintained over time. In turn, 91% of patients showed tendon integrity at the final ultrasound examination.
Of the various techniques that have been described in the literature for the treatment of PBRCT, there is no clear consensus on which is the best for treating these lesions. Some authors prefer to convert PBRCT into complete lesions and then repair them in the traditional way, while others advocate repair by preserving the remaining undamaged fibres (in situ repair).17 We prefer to use the latter technique because it has the advantages of allowing anatomical restoration of the rotator cuff footprint and preservation of the articular fibres of the tendon while protecting the repair of the bursal side.10,18,19
Short-term functional outcomes of in situ repair of PBRCT have been reported in the literature previously.17–20 However, there are few medium and long-term studies. The longest follow-up period reported in the literature using this technique was 6 years (maximum 7 years).21 The authors reported an ASES of 97 points at the end of follow-up, and 76% of patients returned to their original activity level. However, of the 24 shoulders assessed, only 6 were PBRCT. In turn, all the patients underwent biceps tenodesis. Therefore, it is difficult to interpret which part of the pain comes from the repair and which part from the biceps tenodesis. In our study, we found a significant improvement in pain and functional scores at a mean 7-year follow-up. Furthermore, as patients with procedures associated with PBRCT repair were excluded, functional improvements would be explained by supraspinatus repair alone.
The need for acromioplasty to treat rotator cuff tears is a matter of debate. The theoretical benefits of acromioplasty associated with rotator cuff repair would be the increase in the subacromial space that would facilitate the repair and the decrease in extrinsic compression on the repaired tendon.22 Analysis of the literature in relation to complete rotator cuff injuries, does not show that subacromial decompression associated with rotator cuff repair has any significant advantages with respect to pain relief or symptomatic improvement in these patients.23,24 However, studies on PRCT are scarce. In a recent review of acromioplasty in PRCT surgeries, Eraghi25 concluded that there would be no significant difference in short-term functional outcomes in patients treated with or without acromioplasty associated with surgical treatment. However, the studies included have a low level of evidence and included diverse types of treatment (subacromial decompression, arthroscopic repair, open repair). In an analysis of published comparative studies, Snyder et al.8 evaluated 31 patients with a mean age of 42 years and a mean follow-up of 23 months who had low-grade PRCT (articular and bursal) that were treated with arthroscopic debridement. Eighteen of these patients underwent associated subacromial decompression and the remaining 13 only arthroscopic debridement. No significant functional differences were found between the two groups, regardless of the type of injury. However, there are no randomised controlled studies to date that study the repair of partial lesions with and without associated acromioplasty. In our study, we did not perform associated acromioplasty in any patient. Although we do not have a control group, 91% of patients had tendon integrity at the end of follow-up, which is comparable to that reported in studies of similar characteristics in which associated acromioplasty was performed.7,18,19
We found a series of studies in the literature assessing structural outcomes after in situ arthroscopic repair of PBRCT in the short term.17–19 Koh et al.18 assessed 33 patients (86% of the series) with arthroscopic repair of B3 lesions using MRI over an average of 8.2 months and reported 12% of re-tears (4 patients). However, of these, only one (3%) was a complete re-tear and the rest were partial re-tears. Xiao and Cui19 reported 16% re-tears in the treatment of type B2 and B3 lesions after repair of the bursal flap using two different techniques (single row and suture bridge) with no significant differences between the groups. MRI was performed at a mean of 10.3 months in 83% of the series (49 patients). Although this was the series with the highest percentage of re-tears, all of them were partial re-tears (type 3 Sugaya classification). Finally, Shin et al.17 studied 84 patients with PBRCT and compared two surgical techniques: 47 patients were treated with in situ repair of the lesion with the modified Mason Allen technique preserving the intact articular fibres; 37 patients were treated with the suture bridge technique after conversion of the lesion. MRI was performed at 6 months postoperative follow-up in all patients. There was no significant difference in the re-tear rate between the groups. Four of the 47 patients treated using the in-situ technique (8.5%) had re-tears and 3 of the 37 patients (8.1%) with lesion repair before conversion of the lesion had re-tears. In our series, the percentage of tears was similar (9%) at a mean follow-up of 7 years.
We found no significant functional or range of motion differences between the patients with intact tendon on postoperative ultrasound examination and those with tendon re-tears. To our knowledge, there are no comparative series in the literature between conservative and surgical treatment of PBRCT. However, a meta-analysis of randomised controlled studies recently published by Schemitsch et al.26 compares the outcomes of surgical treatment of rotator cuff tears with conservative treatment and with subacromial decompression. Three of the 6 studies included compare surgical treatment with conservative treatment. The meta-analysis of these studies showed a significant increase in favour of surgical treatment at one year postoperatively as measured by the Constant–Moorey score. In turn, the rate of conversion to surgical treatment of patients randomised to conservative treatment in all the studies included was 11.9%. However, one of the included studies reported a conversion rate to surgical treatment of 17.9% in the short term and in the medium term (average 5 years) 3 additional patients were converted from the same series.
The limitations of this series are its retrospective nature, the lack of a control group, the use of different imaging methods for diagnosis and postoperative follow-up and the postoperative imaging analysis performed by a single observer. However, ultrasound and MRI have been shown to have comparable sensitivity and specificity in the diagnosis of rotator cuff injuries.27 Assessment of healing after rotator cuff repair is challenging.28 Although MRI is the gold standard in the diagnosis of rotator cuff tears, its limitations are its cost and that it is contraindicated in certain patients or if the patients are claustrophobic. In turn, various factors, such as those related to the healing process (inflammation, haematoma, oedema, fibrosis, etc.), the presence of metallic implants or postoperative complications, can affect correct diagnosis of a re-rupture.28 In fact, it has been reported that MRI tends to over diagnose re-tears in postoperative patients.12 While these limitations must be considered, Magee et al.29 reported that MRI has a sensitivity of 84% and a specificity of 87% in detecting rotator cuff re-tears.
The advantage of ultrasound, on the other hand, is that it is a dynamic, low-cost study that can be performed in patients in whom MRI is contraindicated and can be performed by the specialist in the office.16 Several studies have reported on the use of ultrasound in the diagnosis of rotator cuff re-tears, demonstrating that this methodology is reliable in these cases. Guilat et al.30 reported a sensitivity of 80.8% and a specificity of 100% in the diagnosis of rotator cuff re-tears. They analysed rotator cuff repair patients with postoperative pain and compared ultrasound findings with arthroscopic findings. In turn, Collin et al.16 reported a sensitivity of 80% and a specificity of 98% for ultrasound in assessing healing in postoperative rotator cuff patients compared to MRI. In our series, we performed ultrasounds at a minimum of 5 years postoperatively. The studies were performed by an experienced imaging specialist. We found 9% of re-tears, with 2 partial re-tears and 3 complete re-tears.
ConclusionsAt mid-term follow-up, arthroscopic in situ repair of patients with PBRCT without associated acromioplasty has excellent functional outcomes. These results are maintained over time, and there is also a high healing rate.
Level of evidenceLevel of evidence IV.
FundingThis study received no funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Bruchmann MG, Rossi LA, Gorodischer T, Burgos Flor JA, Atala NA, Tanoira I, et al. Resultados funcionales e imagenológicos de la reparación artroscópica de lesiones parciales bursales del manguito rotador sin acromioplastia. Seguimiento a mediano plazo. Rev Esp Cir Ortop Traumatol. 2022;66:9–15.