To analyse the incidence and survival of patients with oligometastases (solitary and normal) when they are treated in centres that are experts in multidisciplinary approach to patients with sarcoma.
Material and methodRetrospective analysis of 414 patients with bone metastases secondary to carcinomas at Hospital Universitario La Paz and Hospital MD Anderson Cancer Centre (Madrid) between May 2006 and May 2019. Metastases located in the pelvis and axial skeleton were excluded, analyzing a total of 28 patients who met the criterion for solitary metastases or oligometastases with normal criteria. The study survival estimate was carried out following the Kaplan–Meier statistical method.
ResultsThe survival of the patients following the oligometastases criteria (solitary and normal) was 53%. Breast cancer was the most prevalent and had a survival rate of more than 70%. The average age of the patients was 58 years old.
DiscussionSystemic treatments in cancer treatment have managed to improve disease-free survival curves and lead us to redirect on the paradigm for the treatment of oligometastases, stating that treatment should be carried out in the centres that are experts in the treatment of sarcomas.
ConclusionsThe choice of surgical treatment for patients with oligometastases in the strict sense (solitary) and normal should be evaluated by multidisciplinary teams according to the prognoses of the patient, anatomical location and histotype of the neoplasm.
Analizar la incidencia, factores pronósticos, indicación de tratamiento quirúrgico y supervivencia de los pacientes con criterios de oligometástasis óseas (solitaria y normal) tratados en centros expertos en la resección tumoral de lesiones óseas.
Material y métodoAnálisis retrospectivo de 414 pacientes afectos de metástasis óseas secundarias a carcinomas realizado en el Hospital Universitario La Paz y el Hospital MD Anderson Cancer Center (Madrid), entre mayo de 2006 y mayo de 2019. Fueron excluidas las metástasis localizadas en pelvis y esqueleto axial y se analizó a un total de 28 pacientes que cumplían con el criterio de metástasis solitaria u oligometástasis con criterio normal. La estimación de la supervivencia del estudio se llevó a cabo siguiendo el método estadístico de Kaplan-Meier.
ResultadosLa supervivencia de los pacientes siguiendo los criterios de oligometástasis (solitaria y normal) fue del 53%. El cáncer de mama fue el más prevalente y presentó una supervivencia superior al 70%. La edad promedio de los pacientes fue de 58 años.
DiscusiónLos tratamientos sistémicos en el tratamiento del cáncer han conseguido mejorar las curvas de supervivencia libre de enfermedad, lo que nos lleva a reflexionar sobre el paradigma del tratamiento de las oligometástasis, planteando que el tratamiento debería realizarse en centros expertos en la resección tumoral de lesiones óseas.
ConclusionesLa elección del tratamiento quirúrgico de los pacientes afectos de oligometástasis en sentido estricto (solitaria) y normal debe ser evaluada por equipos multidisciplinarios, según el pronóstico del paciente, localización anatómica e histiotipo de la neoplasia.
Metastatic bone disease is a serious problem that affects patient survival and quality of life. More patients with oligometastases have been detected in recent years, with the development of imaging technologies. In addition, these patients’ prognosis has improved markedly because of improvements in new systemic and local treatments.1
We planned this paper with the background and rationale listed below:
- 1.
Patients presenting with metastatic disease are seeing their survival rate decrease. The prognostic factors are not yet fully clear.
- 2.
The impact of bone metastases on the survival of cancer patients is that it is classified as a disease with a poor prognosis. However, cure or increased survival can sometimes be achieved by metastasectomy in patients with oligometastases.
New treatment strategies are being developed around the concept of oligometastases, introduced by Hellman and Weichselbaum in 1995,2 which is described as a state of limited metastatic burden and has been proposed as an intermediate state between localised disease and systemic metastatic disease, where aggressive local treatments can be used with curative intent.
The concept of oligometastasis is attractive and is a novel scenario compared to the local treatments given in the past, and challenges the view that metastasis is a process that inevitably leads to death, in that it can be approached with objectives other than palliation, but with the fundamental condition that patients potentially susceptible to cure or prolonged survival are those in whom all metastatic foci can be resected, and thus disease progression prevented.3
There are two types of oligometastatic disease: synchronous, detected at the time of diagnosis of the primary tumour, and metachronous, which is the development of oligometastatic disease after treatment of the primary tumour. There is no clear consensus on the oligometastatic paradigm in terms of the number of metastases defining this term,3,4 but three criteria have been proposed:
- -
Strict criterion (M1b): one target in a single organ (solitary metastasis).
- -
Normal criterion: two to three metastases in a single organ.
- -
Broad criterion: one to five metastases irrespective of the number of affected organs.
In the absence of randomised phase 3 trials, clinical studies have shown a trend towards improved survival when aggressive local therapy is added to standard systemic therapy for oligometastatic disease.5,6 There is an increasing indication for more aggressive procedures for these oligometastatic patients than are generally indicated in primary sarcomas.7 Continuing the analogies with the surgical treatment of sarcomas, as it has been shown that complete resection of pulmonary metastases in soft tissue sarcomas and osteosarcomas can be curative,8 more aggressive treatments in patients with oligometastases secondary to cancer have been indicated.
Unfortunately, with the conventional staging system of the American Joint Committee on Cancer, patients with skeletal metastases, even if they are solitary, are classified as stage IV disease,9 which may make surgeons choose palliative and less aggressive treatment in stage IV patients.
Because the concept of solitary metastasis can be encompassed by the term strict oligometastasis, we decided in this paper to refer to it also as solitary, which is a more familiar term, but to avoid confusion we have retained the two terms, therefore strict is the same as solitary. Solitary bone metastasis is a rare condition in which the metastasis is limited to a single skeletal lesion originating from a previously treated or controllable primary lesion.10 The strict and normal criteria are single organ metastases, as opposed to the broad criterion involving more organs. In this study, the organ studied was bone in both criteria (strict and normal).
We have addressed this problem with retrospectively collected progression and treatment data from two hospitals with expertise in cancer treatment. We assessed patient progression according to the criteria of the article by Palma et al.,3 which includes four factors termed the “four aces” in the article, fundamental to evaluate the indication for aggressive local treatment, which will be analysed in the discussion, such as: young age: generally defined as <70 years, Karnofsky functional scale ≥70, metachronous presentation and a prolonged disease-free interval between the original tumour and the presence of metastases.
The main objective was to analyse incidence, prognostic factors, indication for surgical treatment and survival of patients with criteria of oligometastases of bone with the criteria of solitary and normal bone, treated in centres with expertise in bone tumour resection and to determine their treatment strategy with the following secondary objectives:
- 1.
To review a cohort of patients and evaluate the correlation between diagnoses, location, and type of oligometastasis, whether synchronous or metachronous, with survival.
- 2.
To assess whether aggressive surgeries in patients with oligometastases may be superior to palliative or less invasive procedures.
Following the rationale of the work, the following inclusion and exclusion criteria were considered. Patients were included with long bone metastases treated surgically between May 2006 and May 2019, diagnosed with bone metastases secondary to carcinoma, following the criteria of strict (solitary metastasis) and normal oligometastasis.3,4 All patients with broad criteria for oligometastases were excluded, as they included organs other than bone and more than five metastases, which we considered difficult to treat locally by orthopaedic surgery, as other organs were involved. Patients without reliable follow-up data were also excluded.
The study design is retrospective and level of evidence 3,11,12 health-related and analysing medical records from the database of the Bone and Soft Tissue Tumour Units. The research did not involve intervention and/or interaction with subjects for collecting samples or biological material or data (including health or clinical data, surveys, focus groups or observation or behaviour) and no sensitive or personal information was collected. Therefore, informed consent from patients was not required to conduct the study.
The variables to be studied were sex, age, presentation of oligometastases, type of oligometastases, type of cancer, location of metastases, date of last follow-up (unknown, alive with disease, no evidence of disease, died of disease, died of other causes), date of surgery, type of surgery (wide resection, intralesional resection), type of limb reconstruction and date of death.
The medical records of a total of 414 patients with bone metastases (314 cases from Hospital Universitario La Paz and 100 from MD Anderson Cancer Hospital in Madrid), who attended orthopaedic oncological surgery consultations for surgical evaluation, were retrospectively analysed. All patients were followed until death or last follow-up and survival was assessed at 5 years.
The main limitations of the study were that only patients referred to orthopaedic oncological surgery consultations by medical oncology, radiation oncology or trauma emergency departments for risk of fracture or osteolytic lesion of unknown origin were analysed. Metastases located in the pelvis and spine were not analysed, with the aim of creating a single homogeneous group with long bones. Nor was the indication and effectiveness of local treatments, which are also effective in oligometastases, analysed, such as the different modalities of radiotherapy.5,6,13
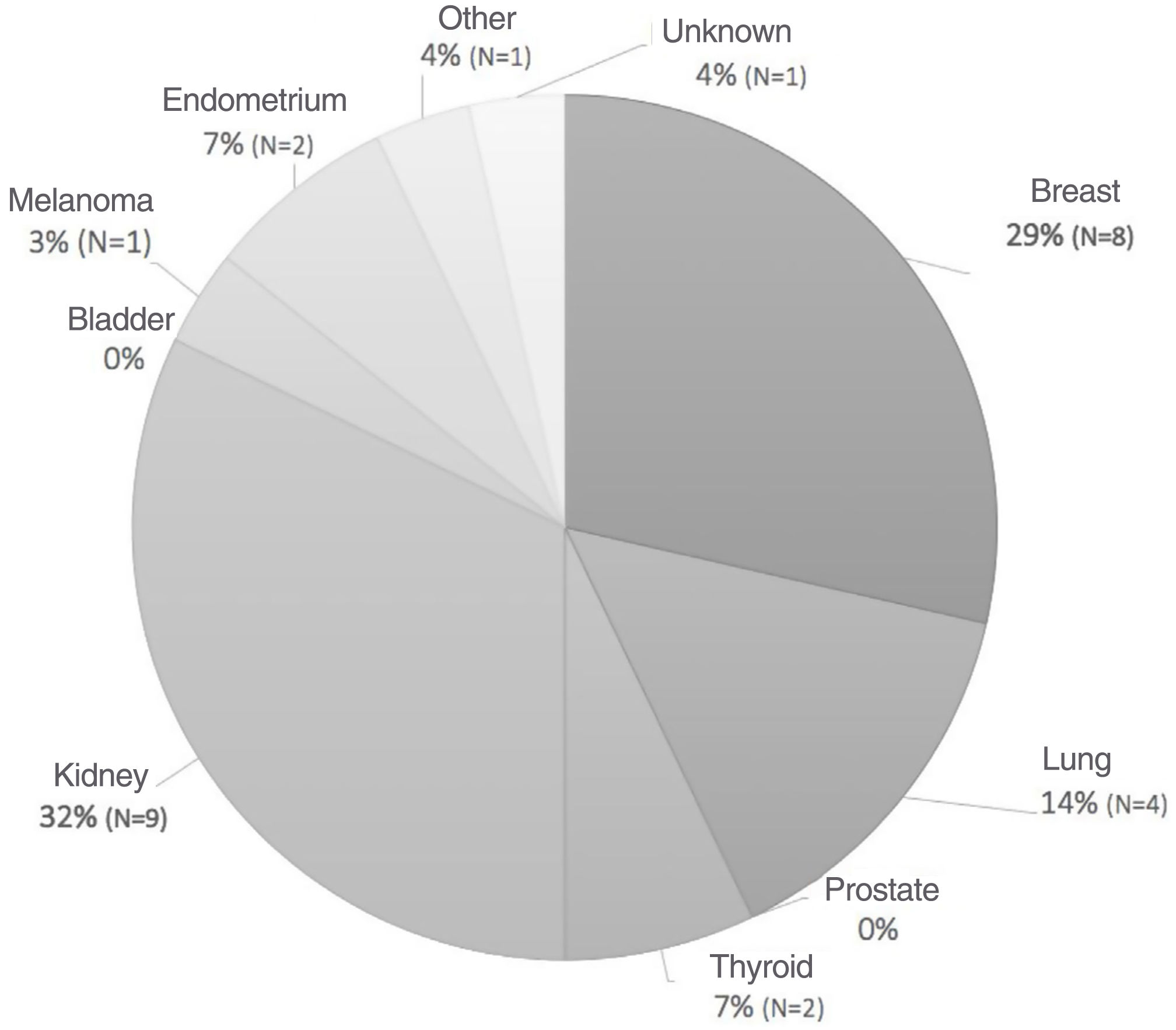
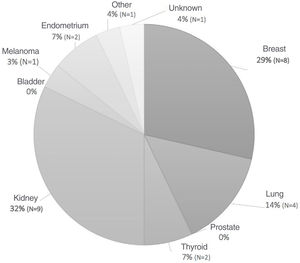
Fig. 1 shows the distribution of primary cancers.
The average age for patients at diagnosis of solitary bone metastases or with normal oligometastasis was 57.6 years (range: 38–78 years). Female sex predominated at 77% over male sex at 23%.
Of the 414 cases, only 28 (6.76%) met the criteria of solitary metastasis (strict oligometastasis) or oligometastasis with normal criteria and control of the primary tumour.
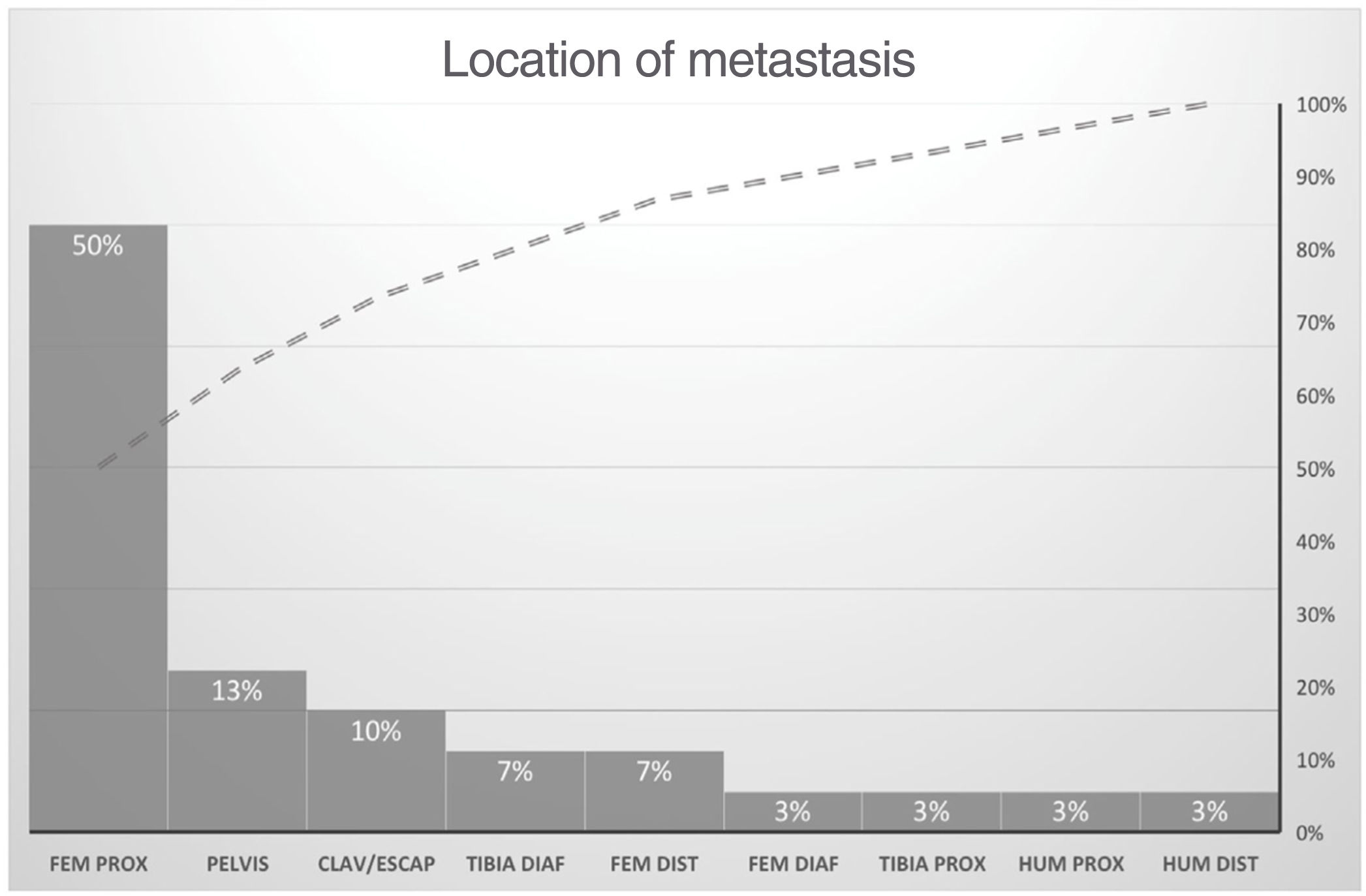
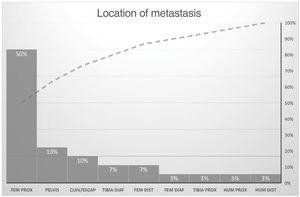
The types of cancer most frequently associated with oligometastases were breast and kidney (Fig. 1). The proximal femur was the most frequent location by far with respect to the other locations, which were distributed between 3% and 11% in other sites, such as the clavicle and scapula which came in second place (Fig. 2).
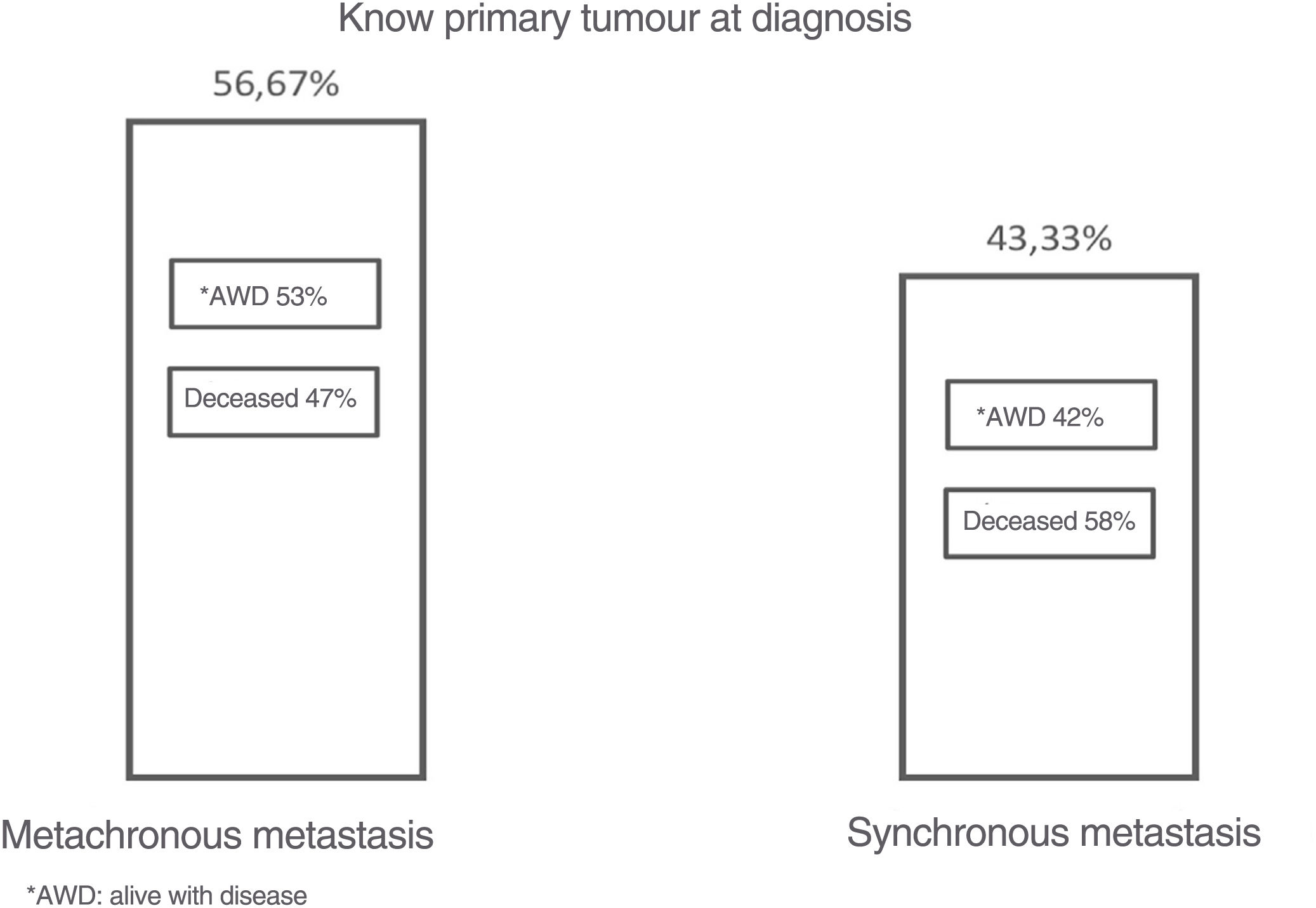
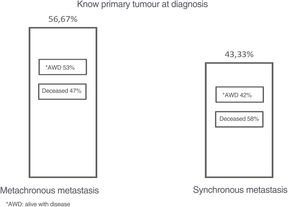
There was no significant difference in the incidence of synchronous (43.33%) or metachronous (56.67%) oligometastases and, in metachronous metastases, the average period of occurrence was 49.23 months (4 years). Pathological fractures occurred in 33% of patients. It was investigated whether the tumour was of known or unknown origin; those with known origin had disease-free survival of 52.94% and, in those in whom the primary tumour remained without a clear finding, it was 38.5%.
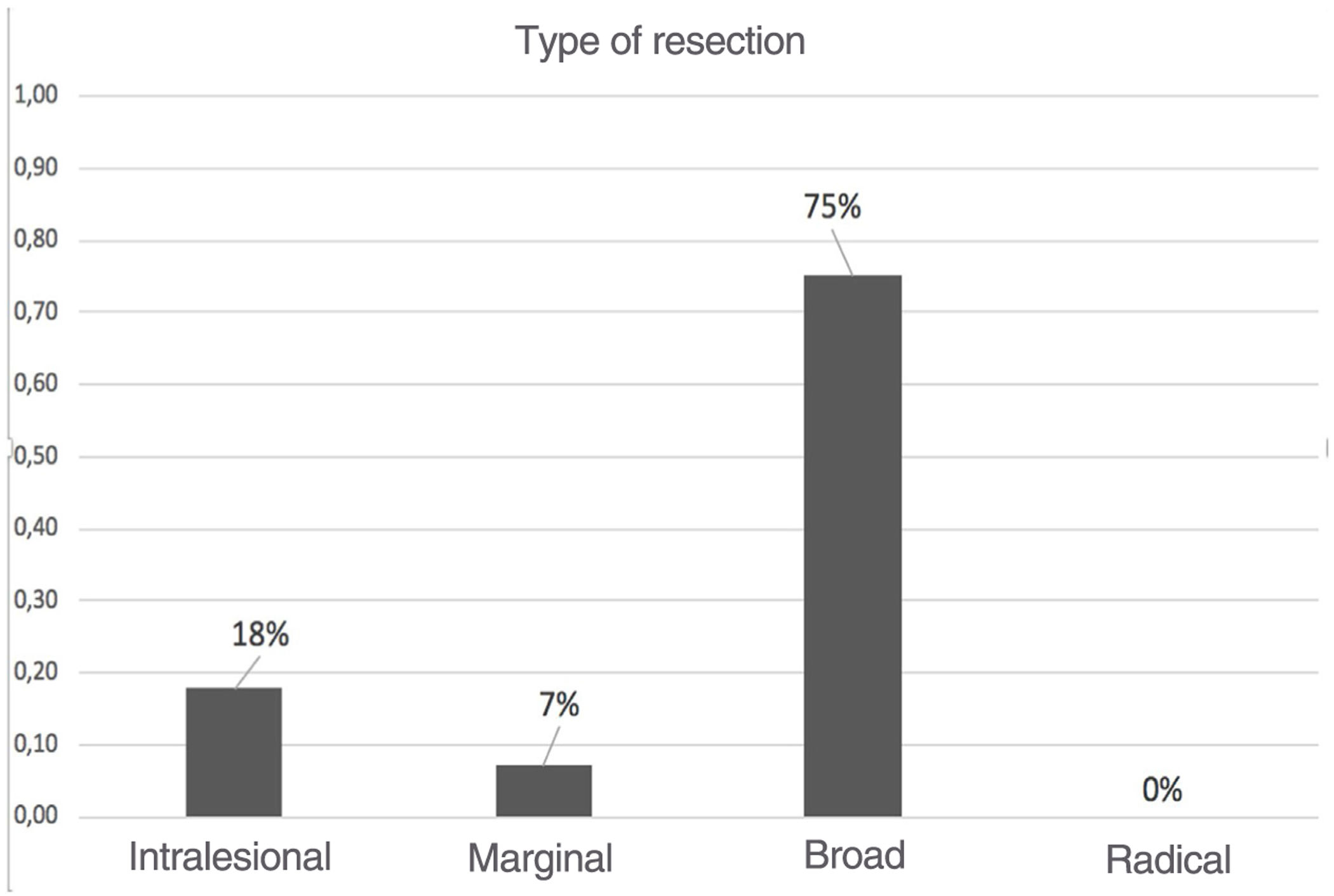
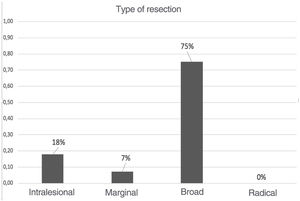
In terms of the surgical treatment and the oncological margin obtained, 28 patients underwent surgery and, in 21 of them, the surgical margin was wide, and all resections performed with wide margins maintained satisfactory survival of both the patient and the implant. The margin was marginal (two patients) or intralesional (five patients) in the remaining patients.
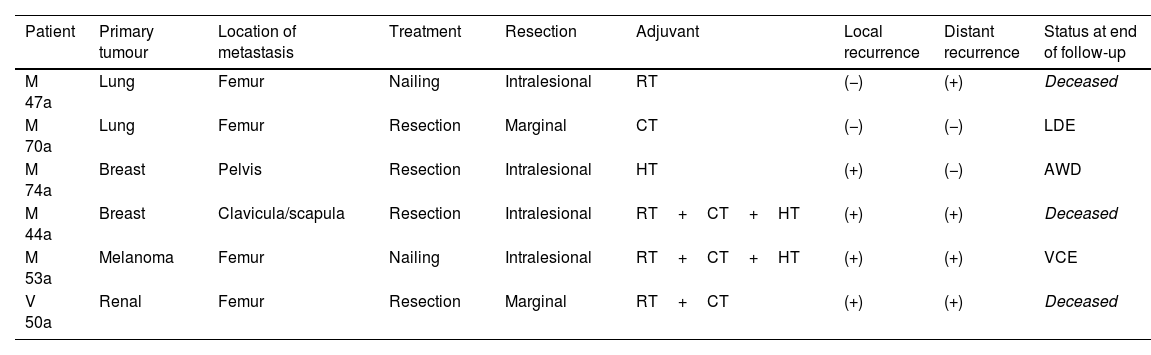
Regarding the adjuvant treatments given to patients who underwent marginal and intralesional resection (Table 1), only one patient was free of disease at the end of follow-up, the other five patients are alive with disease (AWD) or have died.
Description of adjuvant therapy given to patients who underwent marginal resection and status of patients at the end of follow-up.
| Patient | Primary tumour | Location of metastasis | Treatment | Resection | Adjuvant | Local recurrence | Distant recurrence | Status at end of follow-up |
|---|---|---|---|---|---|---|---|---|
| M 47a | Lung | Femur | Nailing | Intralesional | RT | (−) | (+) | Deceased |
| M 70a | Lung | Femur | Resection | Marginal | CT | (−) | (−) | LDE |
| M 74a | Breast | Pelvis | Resection | Intralesional | HT | (+) | (−) | AWD |
| M 44a | Breast | Clavicula/scapula | Resection | Intralesional | RT+CT+HT | (+) | (+) | Deceased |
| M 53a | Melanoma | Femur | Nailing | Intralesional | RT+CT+HT | (+) | (+) | VCE |
| V 50a | Renal | Femur | Resection | Marginal | RT+CT | (+) | (+) | Deceased |
AWD: alive with disease; CT: chemotherapy; DF: disease free; HT: hormone therapy; RT: radiotherapy.
The mean age of patients with oligometastases was 58 years, with female preponderance (77%), correlating with breast cancer, which was the most prevalent, followed by kidney (31.03%), lung (13.79%), thyroid (6.90%), endometrial (6.90%) cancer, and melanoma (3.45%) (Fig. 1).
The occurrence of synchronous metastasis was 43.33%, while that of metachronous metastasis was 56.67%.
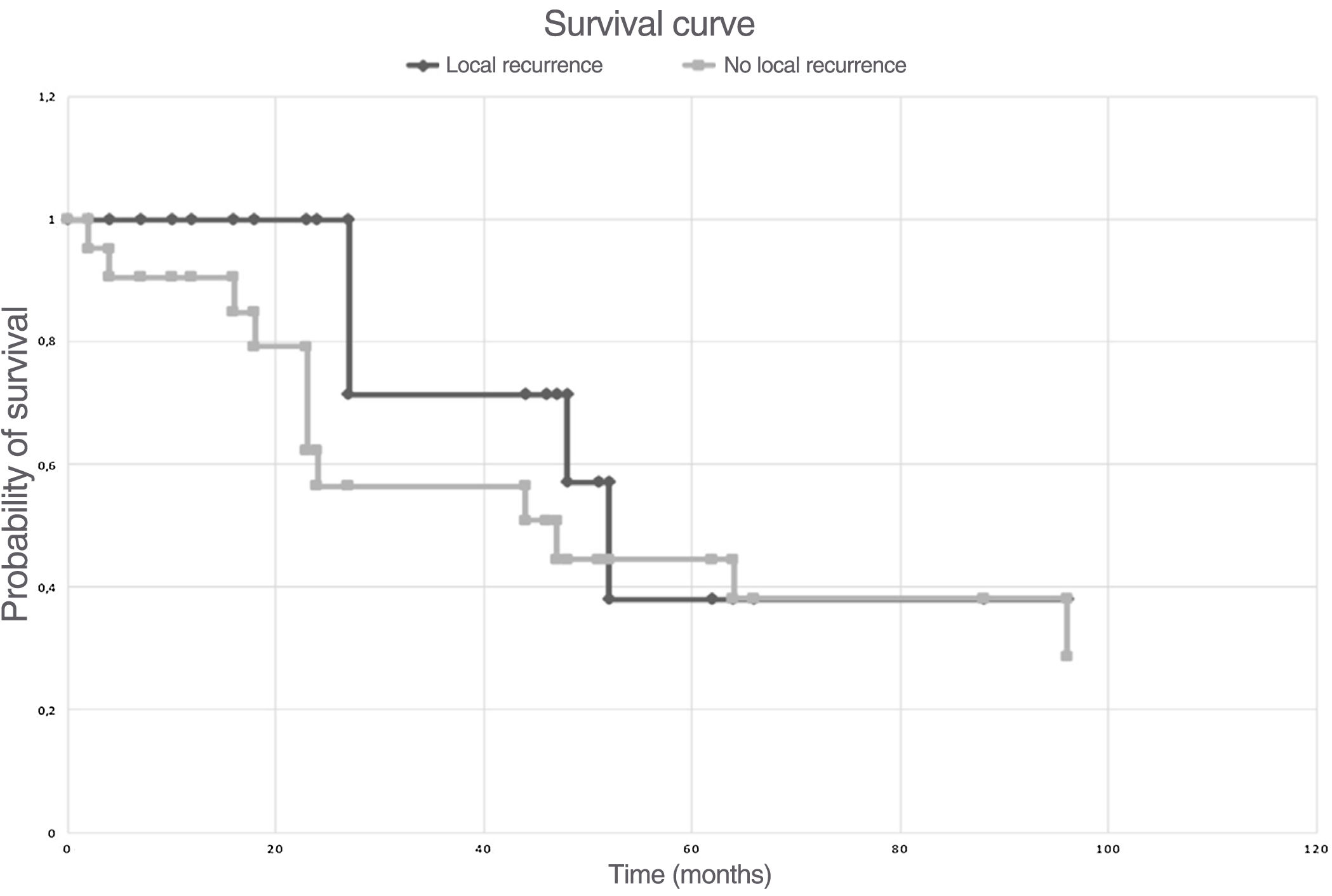
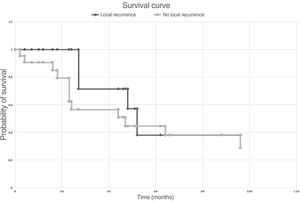
The 5-year survival of the selected patient population, following the criteria for oligometastases (solitary and normal) and considering patient selection bias, was 53%, in contrast to metachronous which was almost 40%, as shown in Fig. 3. Careful analysis of the series shows that in metachronous disease 15% were lost to follow-up and probably died.
Five-year survival study according to the Kaplan–Meier method. The vertical axis represents the probability of survival, the time is expressed in months on the horizontal axis. The black line represents the patients who presented local recurrence during follow-up and the grey line those who did not.
Patients diagnosed with breast cancer had more than 70% survival in the periods analysed, and 53% when the survival of patients in whom a wide margin was achieved is independently assessed. In 75% of the operated patients, the margin achieved was wide, intralesional in 18% and marginal in 7% (Fig. 4).
Patients with a wide margin had a survival rate of 53%, and 47% of them died within a mean 34.75 months and without reconstruction failure.
Metachronous metastases occurred late and about 4 years after diagnosis of the original tumour.
Although not significant, metachronous metastases had a lower death rate in our series (47%), in contrast to synchronous metastases at 58% (Fig. 5).
More than half of the cases, in the clinical course of their disease and after surgical treatment, developed distant metastases, and just under 27% had local recurrence. The incidence of pathological fractures was 30%.
DiscussionThe study confirms that the subgroup of oligometastases with strict (solitary) and normal criteria is not frequent and, of the 414 cases, only 7.24% met these requirements in the case series analysed. In the series of 1453 cases published by Hosaka et al. from the Department of Orthopaedic Surgery at the Shizuoka Cancer Centre in Japan, even fewer, 1.8%, had solitary metastases (strict oligometastatic criteria).10 This difference is because in the series that we analysed, patients were added with oligometastases with normal criteria.3,4
Due to the infrequency of these types of oligometastases, a clear understanding of the concepts of therapeutic indications is essential to achieve improved survival and indeed cure. It is therefore essential to work in multidisciplinary teams with expertise in these types of diseases.10 We also consider that these patients with potentially treatable oligometastases should be treated in expert centres with multidisciplinary teams, experts in bone tumour resection.
The age of the patients in the series, under 70 years and the majority with a Karnofsky scale greater than 70 and with a disease-free interval between the original tumour and metachronous metastases of 4 years, suggests to us as reported by Hellman and Weichselbaum,2 among other probabilities, that the disease burden can be considered small with a limited metastatic state and more so in our series, as the patient selection had strict criteria (solitary metastasis) or normal, which includes only one organ.
In the results, although similar to those of other publications, it is striking that metachronous oligometastases appeared approximately 4 years after the initial tumour. This data is very encouraging and leads us to conjecture that treatments against certain cancer groups are becoming increasingly effective.1 However, there are other studies that have shown that patients with synchronous bone metastases had longer survival (40 months), demonstrating the difficulty in predicting conclusive results,14,15 in the series under study, there was no significant difference in mortality, but it did tend to be somewhat better.
The preponderance in female sex demonstrates the link with breast cancer, which was the most frequent. Strangely, no oligometastases were observed in prostate, colon, or bladder cancer. Survival was highest in patients with breast cancer, almost 70% to date. Interestingly, survival in kidney cancer was not what we expected, as the literature has reported, at 33%.15
Pathological fracture was present in only 30%, which is evidence that patients may be being referred early to orthopaedic surgery and trauma services, decreasing the percentage of their diagnosis, and demonstrating that academic reporting on referring these patients prior to fracture has advantages.16
As outlined in the introduction, we analysed the four aces, according to the article by Palma et al.3 and observed that most of the series of patients analysed met these factors, with a mean age of less than 60 years, functional scales greater than 70, metachronous metastases and with a better prognosis than synchronous,1 and therefore it is crucial to consider criteria that lead the surgeon to the most appropriate therapeutic indication, updated with the concepts of oligometastases.
The occurrence of metachronous metastases in the series analysed, an average of 4 years after initial diagnosis, may reaffirm that systemic treatments in certain neoplasms have managed to prolong disease-free periods and may indicate that the paradigm of taking an aggressive therapeutic approach to oligometastases is a reality.
What is our philosophy from the point of view of orthopaedic oncological surgery? If we believe that a wide tumour margin can be performed, we always try to do so. Of the cases that underwent surgery, 72% had a wide margin, most of our cases were located in the proximal femur and therefore it is more feasible to perform a resection with wide margins and reconstruction with prosthesis than in other locations,17 but unfortunately there was no difference in survival whether we obtained a wide margin or not. Despite this finding, we consider that a wide margin helps to achieve a greater survival interval, observed in the series studied, after surgery, and we can therefore conjecture that this type of margin helped. We also observed that of more than 50% of the cases, less than 27% had local recurrence during the clinical course of their disease. It is thought that this decrease in the local recurrence rate could be related to surgical aggressiveness in terms of achieving a wide margin.
A recent study by the Department of Orthopaedics and Orthopaedic Oncology of the University of Padova (Italy) found that overall survival is significantly better in patients with solitary metastases or oligometastases than in those with multiple metastases and that patients treated with resection and prosthesis had a significantly longer survival than those treated with nailing. We agree with this, as the oncological complications that are observed in patients with endomedullary nailing are reduced.18
Another fact to consider is the anatomical location; the clavicle and scapula were in second place, after the proximal femur (Fig. 2), an anatomical situation that makes it easier for surgeons to achieve wide tumour margins in surgery.
The oligometastatic paradigm is indeed attractive for surgeons and patients. However, we must remember that to try to cure the patient, all the oligometastases must be treated and not just one. Therefore, the support of radiotherapy is essential, which is one of the limitations of this research.
The most important prognostic factors are age, metachronous metastasis and tumours that can be considered slow-growing, or with therapeutic targets such as breast cancer.
The choice of surgical treatment should always be discussed in multidisciplinary teams. The choice of the type of surgical resection is related to the prognosis of the patient, the anatomical location and the histotypes of the neoplasm.
Patients with strict (solitary) and normal oligometastases3,4 should be considered candidates for wide margin surgical treatment. Therefore, it is critical that optimal implant survival curves persist above the patient survival curves.18 Local disease control and implant stability from the perspective of orthopaedic oncological surgery are important issues for patients with long survival potential.
Clearly, further statistical studies are needed to confirm the better survival of patients with oligometastases and to avoid selection bias.
Level of evidenceLevel of evidence III.
FundingNo funding was received for this work.
Conflict of interestsThe authors have no conflict of interests to declare.
Protection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.