Ankle syndesmosis injuries can be associated with a spiral mechanism on tibial shaft fractures. We are not aware if there is evidence of the incidence of ipsilateral syndesmotic lesson associated to high-energy tibial shaft fracture mechanisms. The aim of this study was to analyze the incidence of syndesmotic injuries associated with high-energy tibial shaft fractures.
MethodsTwo hundred thirty-three diaphyseal tibial fractures operated between January 2007 and January 2017, the fracture patterns were analyzed, they were classified according to AO, the talocrural angle was measured, they analyzed failures and reoperations and described a novel failure method.
ResultsFrom a total of 234 fractures that met the inclusion criteria, 159 (64.96%) suffered closed fractures and 75 (32.05%) where open fractures. According to the AO classification system: 152 (64.10%) were simple patterns 42.A; 49 (20.94%) wedge type patterns 42.B and 33 (14.10%) complex patterns 42.C. Ten patients, a 4.27% of the sample, shown an increased talocrural angle in the postoperative radiographs, evidencing shortening of the fibula. Nine patients underwent surgery, the remaining patient was lost to follow-up. All the treated patients presented restoration of the normal talocrural angle.
ConclusionThe incidence of syndesmotic injuries associated with high-energy tibial shaft fractures reaches 4.27%. We think that is necessary to evaluate the ankle and syndesmosis in all tibial shaft fractures, even with high-energy patterns, not only in spiral patterns.
Las fracturas diafisarias espiroideas de tibia pueden asociarse a lesiones sindesmales del tobillo. No tenemos conocimiento de que exista evidencia sobre la incidencia de lesiones sindesmales ipsilaterales asociadas a los mecanismos de fractura de tibia de alta energía con patrones oblicuos y transversos. Nuestro objetivo fue analizar retrospectivamente una serie de pacientes que presentaron rotura de la sindesmosis asociada a fracturas diafisarias de tibia con patrones oblicuos y transversos y evaluar la incidencia en nuestro medio.
MétodosDel total de 233 fracturas diafisarias de tibia operadas entre enero de 2007 y enero de 2017, se analizaron los patrones de fractura, se clasificaron según AO, se midió el ángulo talocrural, se analizaron los fracasos y reoperaciones y se describe un método poco conocido de fracaso.
ResultadosDe 234 fracturas que cumplieron los criterios de inclusión, 159 (64,96%) sufrieron fracturas cerradas y 75 (32,05%) expuestas. Según el sistema AO: 152 (64,10%) fueron patrones simples 42.A; 49 (20,94%) patrones tipo cuña 42.B, y 33 (14,10%) en patrones complejos 42.C. Diez pacientes presentaron acortamiento del peroné, evidenciado por el aumento del ángulo talocrural en las radiografías postoperatorias, suponiendo un 4,27% de la muestra. Nueve pacientes requirieron cirugía; el paciente restante se perdió en el seguimiento. Todos los pacientes presentaron restauración del ángulo talocrural normal.
ConclusiónLa incidencia de lesiones sindesmales inadvertidas asociadas a fracturas diafisarias de tibia oblicuas y transversas llega al 4,27% en nuestra serie. Consideramos necesaria la evaluación del tobillo y la sindesmosis en todas las fracturas diafisarias de tibia, aun con patrones de alta energía y no solo en patrones espiroideos, a fin de lograr mejores resultados y evitar secuelas e intervenciones futuras.
The tibia is the most frequently fractured long bone due to its location, characteristics and anatomical repairs.1 Diaphyseal tibia and fibula fractures account for 4% of all skeletal fractures, and some authors describe up to 59.6% of associated injuries.1–5
They usually present a bimodal distribution with high-and-low energy mechanisms in young and older patients respectively.1
The most common fracture pattern is the spiroid, which is why numerous studies describe the need to evaluate injuries to the distal tibioperoneal syndesmosis in spiroid fractures of the tibia.6,7 However, in high-energy tibial fractures with transverse or short oblique patterns, ankle syndesmotic and ligament injuries are often under-diagnosed due to the lack of clinical evaluation in the context of this type of fracture.8
Chronic syndesmotic and ligament injuries of the ankle are among the main causes of post-traumatic pain and osteoarthritis. Proper treatment of these injuries, often concomitant with tibial fractures, is essential to achieve better postoperative outcomes.9–11
We are not aware of the existence in the scientific reference of articles where syndesmotic lesions are related to high energy patterns with oblique and transverse patterns.
The aim of this study was to conduct a retrospective analysis of a series of patients who presented with presented syndesmotic rupture associated with high-energy tibial diaphyseal fractures with oblique and transverse patterns and evaluate the incidence in our environment. At the same time, we describe how rescue surgery has been performed in these cases.
Materials and methodsA descriptive, observational, retrospective study of patients with diaphyseal fractures of the tibia in the period from January 2007 to January 2017 was conducted. The data were extracted from the institutional electronic medical records which store the information prospectively. Patient confidentiality was respected at all times.
The sample included diaphyseal fractures of the tibia and fibula in those over 18years of age whose mechanism of production was reported as high energy. The AO classification was used to determine fracture type and subtype, with the following patterns included: 42A2, 42A3, 42B2, 42B3, 42C2 and 42C3.12
Fractures classed as low energy (42A1, 42B1 and 42C1 of the AO classification) were excluded, with joint compromise, patients with who had undergone previous surgery or those with sequelae.
Exposed fractures were also classified according to Gustilo et al.13
The median age was 43.35years and distribution according to sex was 65.81% for males (Table 1). All patients were treated initially for tibia fracture using reduction and osteosynthesis or external fixation in the acute period.
They were assessed for syndesmal lesion on the baseline radiograph.
Radiographic evaluation was carried out retrospectively at the initial fracture, after initial fracture treatment at two weeks, at one month and then monthly until healing with loaded radiographs when tolerated by the patient in the late postoperative period. Finally, annual radiographic controls were performed.
Anteroposterior and profile projections of both the leg and ipsilateral ankle were used.
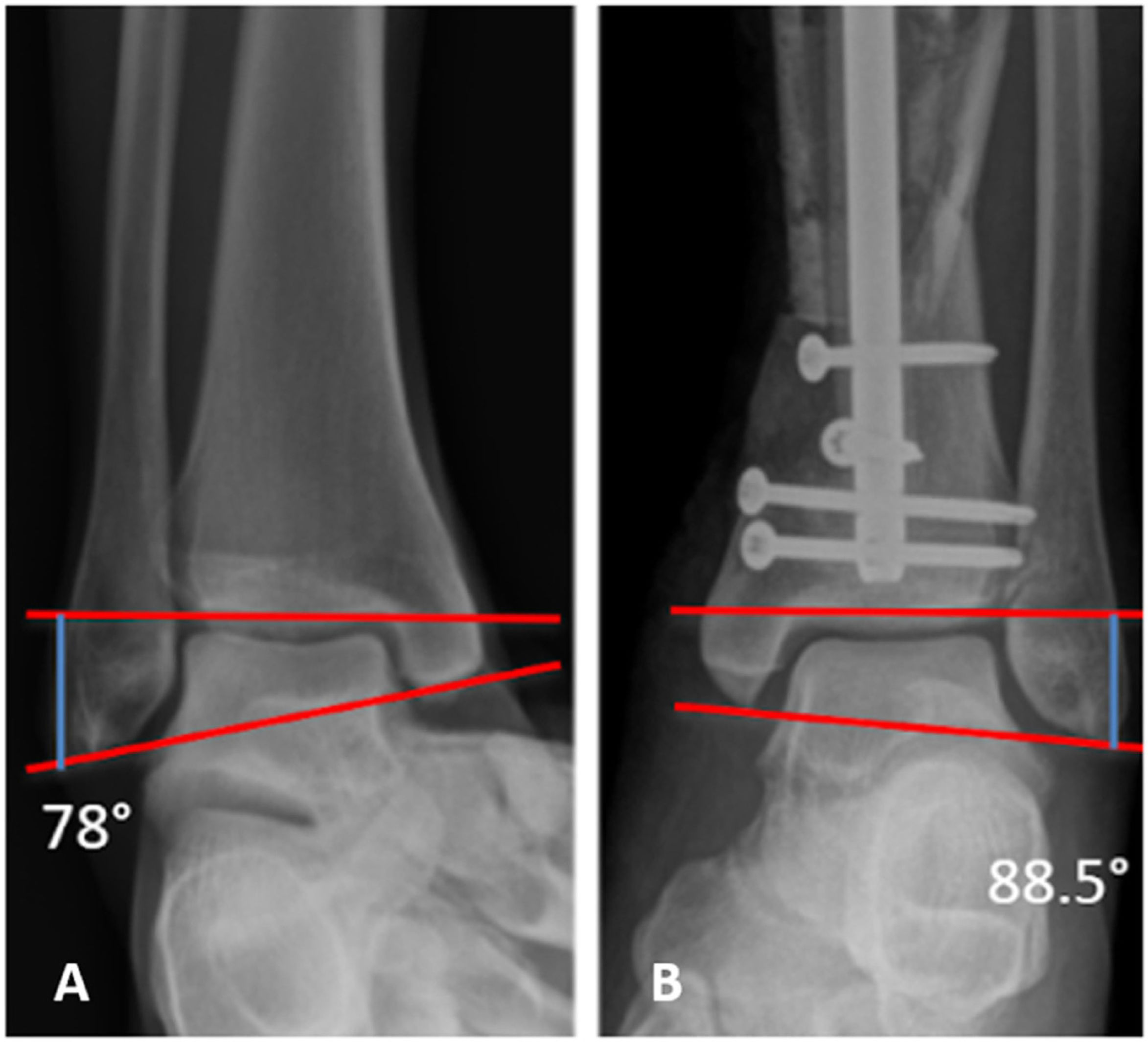
The presence of shortening of the fibula length on anteroposterior ankle radiographs was established as suggestive of a syndesmotic ligament injury. For this purpose, the talocrural angle was measured. In cases where the fibula was interpreted as shortened, radiographs of the contralateral ankle were taken for confirmation. We defined this angle as the angle formed by a line joining both malleoli and another line perpendicular to the articular surface of the distal tibia with a normal value between 75 and 87 degrees, thus defining the angle above 87 as corresponding to a shortened fibula.14 In turn, the presence of ankle pain was assessed to correlate fibula shortening with symptomatology using the visual analogue scale (VAS) at the end of follow-up.
All patients were operated on by surgeons experienced in orthopaedic trauma (CS, JB, GC, DT).
Data on the corrective surgeries performed were collected and are reported in this series. In cases where the diagnosis of syndesmotic injury was made in the distal postoperative period, the treatment performed was a fibula osteotomy lengthening the length of the fibula, restoring the talocrural angle of the ankle and subsequently fixing the distal tibioperoneal joint with transindorsal screws. When the diagnosis of a syndesmal lesion was made in the first instance, syndesmal fixation was performed and length was restored without the need for lengthening osteotomy.
Follow-up of this series was a minimum of 3 years, with a mean of 7 years (range 3–13).
ResultsOut of the total of 234 patients who met the inclusion criteria, 159 (64.96%) suffered from closed fractures and 75 (32.05%) from exposed ones. Fractures were classified according to the AO system, with the resulting: 152 (64.10%) in simple patterns 42.A; 49 (20.94%) in wedge-shaped patterns 42.B, and 33 (14.10%) in complex patterns 42.C.
Ten patients had shortening of the fibula length as measured by the talocrural angle; in 6 cases it was on X-rays after primary fracture stabilisation surgery and in 4 cases during the primary surgery itself, meaning an incidence of 4.27% (Table 2). Six of them reported mechanical ankle pain at the start of rehabilitation with full weight bearing. In the remaining 4 it was not possible to assess pain, as the syndesmal lesion was suspected during tibial fracture reduction surgery and, once this was completed, the stress manoeuvre of the distal tibioperoneal joint was confirmed.
Series of patients with syndesmal lesion associated with high energy tibial diaphyseal fracture.
| AO tibia classification | AO fibula classification | Exposed | Gustilo classification | Time of diagnosis | Operated | Talocrural angle (°) | VAS at follow-up completion | |
|---|---|---|---|---|---|---|---|---|
| 1 | 42C3 | 4F2B | Yes | III-A | 3 months | Yes | 88.5 | 4 |
| 2 | 42C2 | 4F2A | Yes | II | 12 months | Yes | 101 | 2 |
| 3 | 42A2 | 4F2A | Yes | I | 3 months | Yes | 91.3 | 0 |
| 4 | 42A3 | 4F2A | Yes | II | 3 months | Yes | 88.9 | 1 |
| 5 | 42C3 | 4F2B | Yes | II | 12 months | Yes | 89 | 3 |
| 6 | 42A3 | 4F2B | Yes | I | 2 months | No | 90.1 | 2 |
| 7 | 42A3 | 4F2B | Yes | II | Intraoperative | Yes | 90 | 0 |
| 8 | 42C3 | 4F2B | Yes | III-A | Intraoperative | Yes | 90.5 | 3 |
| 9 | 42A3 | 4F2B | Yes | II | Intraoperative | Yes | 90 | 2 |
| 10 | 42A2 | 4F2A | No | Intraoperative | Yes | 88 | 0 |
VAS: Visual Analogue Scale.
Examining the group of patients who sustained a syndesmosis injury associated with the leg fracture, we found that 9 of them had exposed fractures, and according to the AO classification, 4 resulted in fracture patterns 42-A3 (simple transverse pattern), 3 were classified as 42-C3 (complex irregular pattern) and one resulted in 42-C2 (complex segmental pattern); the remaining two cases were grouped in type 42-A2 (simple oblique pattern). All injury mechanisms could be classified as high energy and had ipsilateral fibula fractures. Fractures that were exposed were initially stabilised with external fixation prior to primary surgery (Table 2).
In 5 patients revision surgery was performed, restoring the talocrural angle by lengthening osteotomy of the fibula.
One patient who was diagnosed during the first postoperative controls was lost to follow-up. The remaining 4 were diagnosed during intraoperative radiographic assessment, confirming the injury with Cotton's manoeuvre and stress test, and were treated in the same surgical act by fixation of the syndesmosis at the first time. The VAS results are summarised in Table 2.
DiscussionOver the years the association between diaphyseal fractures of the tibia with spiroid patterns and injuries to the posterior and lateral malleoli has been demonstrated, as well as injury to the ankle in fractures of the distal third of the tibia.6,8,15 But we have found no literature evidence of associated syndesmal injuries in the ankle when fractures are transverse, oblique, wedge or multifragmentary, which are generally associated with high-energy mechanisms.
In this study we have attempted to contribute to the scientific literature our experience in relation to this type of fracture with ligament injuries of the ankle, and to highlight that they can go unnoticed at first if they are not suspected. We were able to conclude that the incidence of involvement of the syndesmosis in high-energy fractures of the ipsilateral tibia is close to 4% in our environment. This can be detected intraoperatively and treated, thus avoiding early complications with consequences for the distal tibioperoneal joint.
In their study, Stuermer and Stuermer8 describe close to 20% of ankle injuries associated with diaphyseal fractures of the tibia, where 88.4% of the latter were spiroid patterns. The remaining 11.6% of injuries were associated with malleolar fractures. In our series, we not only excluded tibial fractures with articular extension, but also did not seek to evaluate spiroid tibial fractures, as we would probably have obtained results similar to those described by Stuermer. However, our aim was to evaluate ankle injuries diagnosed perioperatively either by radiography or by distal tibioperoneal pain. In this context we were able to describe a 4% incidence of syndesmal lesions, which relatively frequently (6 cases out of 10) go primarily unnoticed in diaphyseal tibial fractures, always associated with exposed fractures and/or high energy patterns. Figs. 1–4 illustrate case 1 referred to in Table 2.
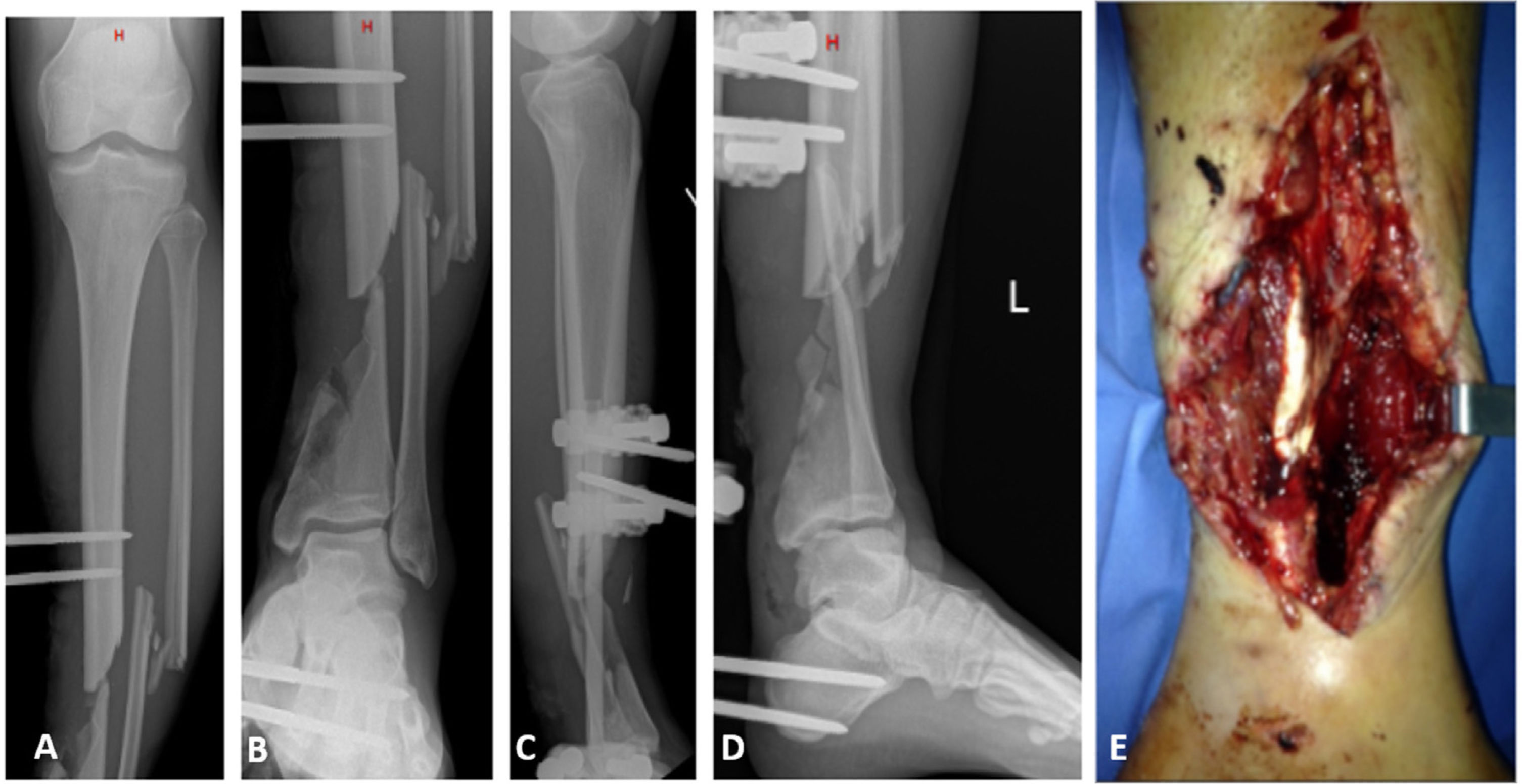
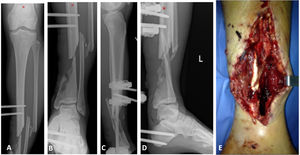
25-year-old male patient who, after a motorbike accident, was treated urgently at another centre with an external fixator and referred to our institution with the following X-rays and clinical images. (A and B) Front X-rays of the left tibia showing a fracture of the tibia and fibula, 42C3.3 without joint involvement. (C and D) Profile X-rays showing a distal diaphyseal segmental defect. (E) Clinical image of bone exposure during external tutor removal surgery.
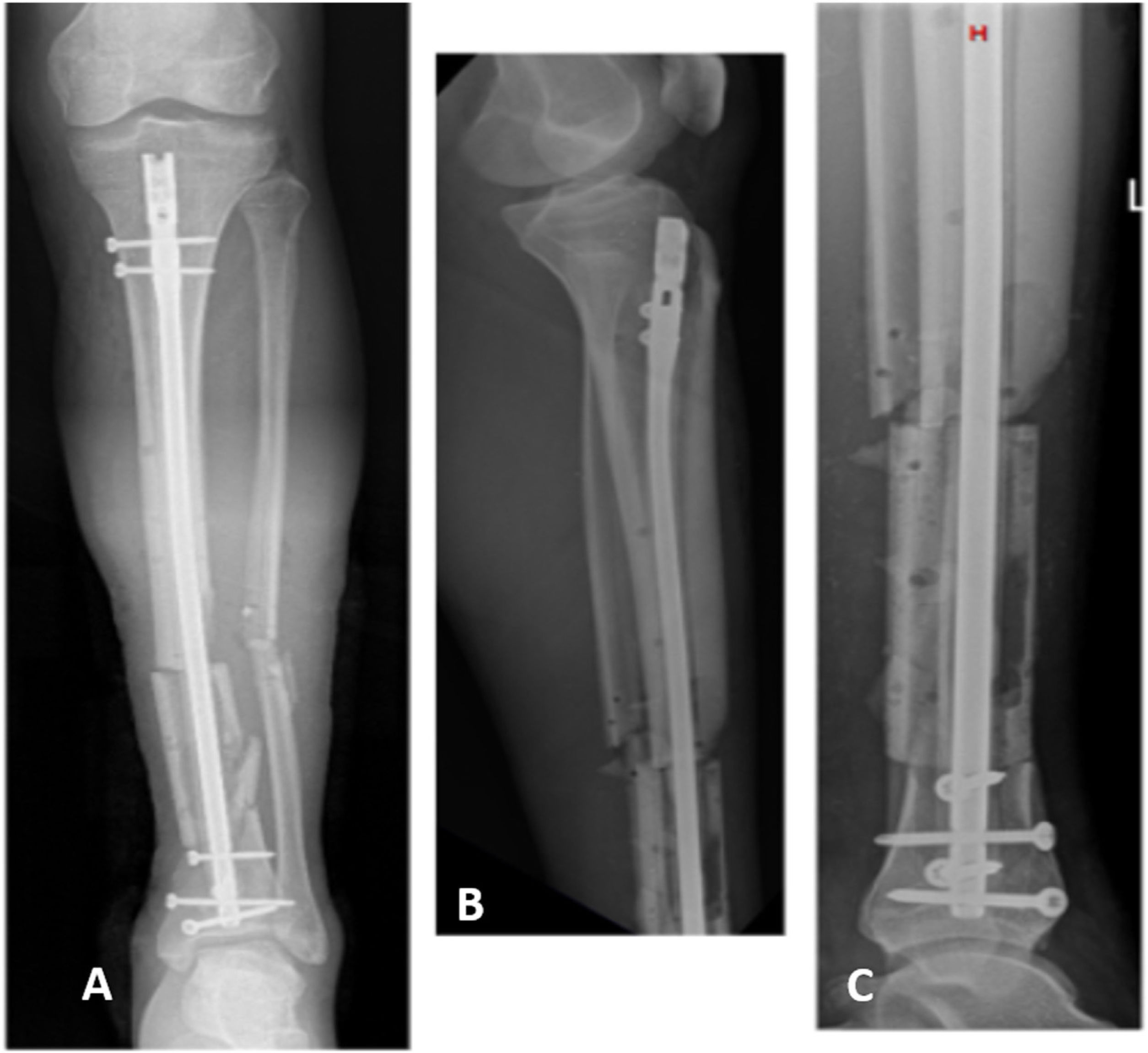
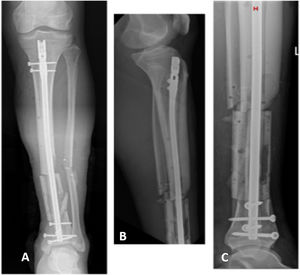
Same patient as in Fig. 1 after primary resolution of his tibial fracture using an endomedullary nail. (A) Front postoperative radiograph showing restoration of tibial length. (B and C) Profile X-rays of the leg showing correct placement of the endomedullary device and indemnity of the distal joint.
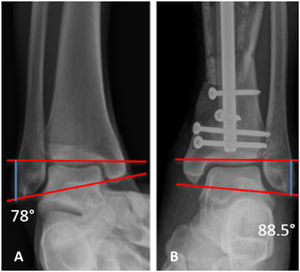
Focused radiographs of the ankle at 3 month postoperative follow-up of the same patient in Figs. 1 and 2, who presented with left distal tibioperoneal joint pain during weight bearing. (A) Radiography of the right ankle for comparison showing a talocrural angle of 75. (B) Radiograph of the ankle ipsilateral to the tibial fracture showing an increased pathological talocrural angle.
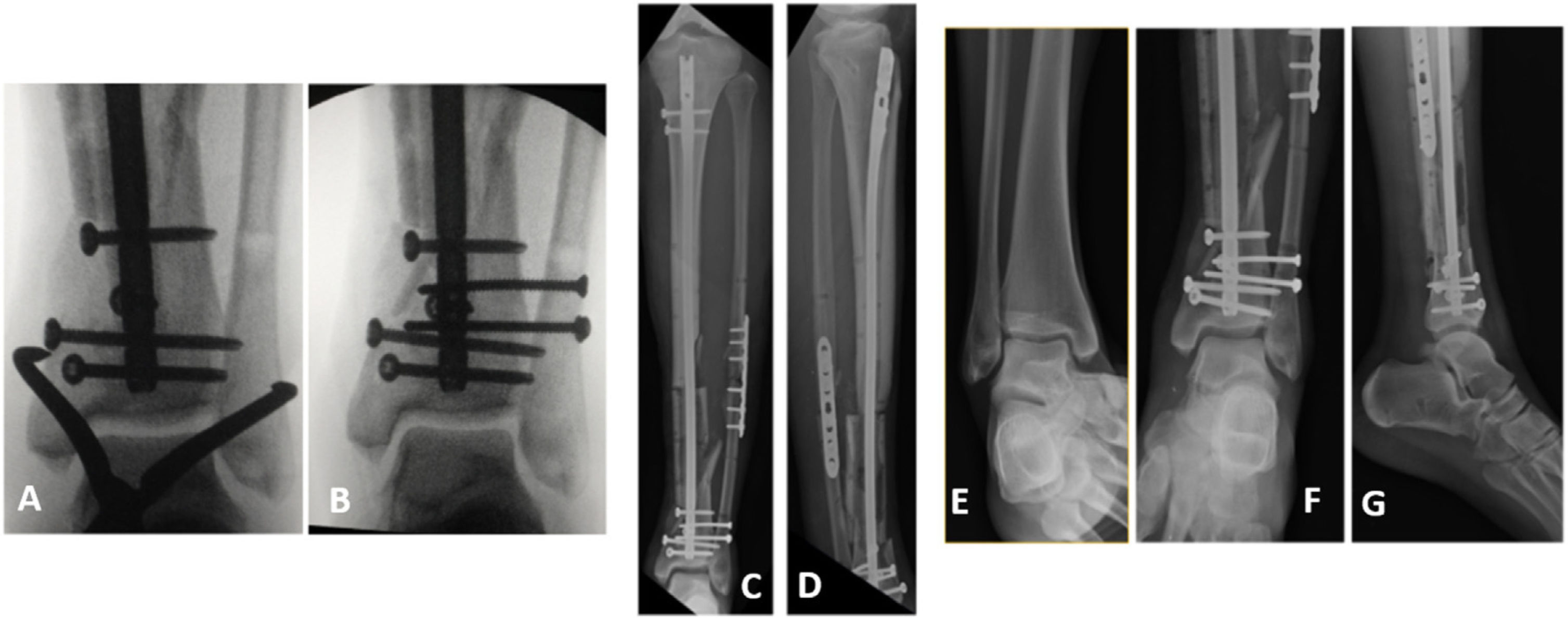
Surgical resolution of the syndesmal lesion in the same patient as in Figs. 1–3. (A) Intraoperative radioscopy of the reduction manoeuvre of the distal tibioperoneal joint. (B) Intraoperative radioscopy of fixation with two tricortical screws of the reduction achieved. (C and D) Front and profile radiographs postoperatively of the salvage surgery also showing fixation of the fibula fracture associated with fixation of the syndesmosis. (E–G) Post-operative ankle-focused radiographs of the same surgery.
In accordance with the findings of a systematic review by Kellett et al.15, where they study imaging in ankle syndesmosis injuries, we can clarify that although direct visualisation of the syndesmosis by arthroscopy or the use of nuclear magnetic resonance would be more sensitive methods to diagnose such injuries, it is often impossible to apply them. In our series all fractures were high-energy patterns, and many of them required the placement of an external fixator in acute treatment, where MRI is not possible due to the material of the external fixator, being necessary for this practice the use of carbon rods. In the same work, Kellett et al.15 studied computed axial tomography and the relationship of the fibula to the tibial incisura, and were unable to demonstrate that this method is ideal for the study of pure ligament injuries, probably due to the wide anatomical variability of this structure. Regarding the use of radiography with or without stress, they describe a low sensitivity and specificity for even complete lesions of the syndesmosis, leading to the use of ultrasound as a simple study, with minimal contraindications and high sensitivity and specificity in the diagnosis of the lesions under discussion.
In our series the radiographic method of choice was the anteroposterior ankle projection without loading in the early postoperative period and with monopodal loading in the late postoperative period. We used the measurement of the talocrural angle as a parameter for measuring the shortening of the fibula and suggestive of distal tibioperoneal ligament injury.
We are aware that there are other radiographic signs and parameters to assess the presence of syndesmosis injury, but we were limited by the fact that, when carrying out a retrospective evaluation of mostly polytraumatised patients, we did not have adequate and systematised radiographs in all the patients included.
As we evaluated the patients we sharpened our search for this association of injuries, leading us to diagnose the latter patients at first due to suspicion related to the fracture pattern. This led to the subsequent cases being diagnosed early, thus being able to prevent the sequelae with simple surgical manoeuvres in the primary fracture surgery.
It should be clarified that nowadays, in our clinical practice, the correct preoperative assessment is fundamental and, together with it, the intraoperative confirmation by means of stress manoeuvres of the distal tibioperoneal joint, in order to be able to carry out the appropriate treatment at an early stage, without having to resort to rescue surgeries.
Our findings encourage the need to evaluate the ankle even in diaphyseal fractures of the tibia, which due to their own characteristics, such as transverse and oblique traces or the context of exposed fractures, often lead to dismissing injuries that compromise the joint.
Recognising shortening of the fibula intraoperatively or assessing the stability of the syndesmosis by stress manoeuvres or by Cotton's manoeuvre would be an easy and quick screening for injuries that might go unnoticed. This is true because of the lack of suspicion of the association of these injuries in high-energy tibial fracture patterns.16,17 In our experience, in the last 13years we had an incidence of 4.27% of syndesmotic injuries associated with tibial fractures with oblique and transverse patterns, where early diagnosis could lead to an improvement in the patient's recovery and functionality with a minimal gesture, with the patient benefiting from reduction of the fibula at the tibiofibular incisura and fixation of the syndesmosis.
ConclusionBased on our study, about 4 out of 100 patients with a diaphyseal tibial fracture had loss of height in the ipsilateral fibula, suggesting an indirect sign of syndesmal injury. Regarding this association of injuries, we have found no bibliographic evidence to date. We consider it necessary to evaluate the ankle and syndesmosis in all tibial diaphyseal fractures, even with high-energy patterns, and not only in spiroid types, in order to achieve better results and avoid future interventions and sequelae.
Level of evidenceLevel of evidence IV.
FundingThe authors did not receive funding of any kind for conducting this research, nor for the authorship or publication of this article.
Conflict of interestsThe authors declare no conflict of interests relating to this research, authorship or the publication of this article.