Instrumentation with pedicle screws (PS) can compromise the adjacent neural structures. Triggered electromyography (tEMG) is a modality of intraoperative neuromonitoring, used to assist in the placement of these. The objective of the present study is to evaluate the reliability of this tool.
MethodRetrospective review of patients underwent posterior lumbar fusions from January 2017 to December 2019, correlating postoperative CT images (postop CT) with tEMG results for each PS with a threshold of 10mA, establishing sensitivity and specificity of this tool. Diagnostic test and receiver operating characteristic curve were performed to evaluate the area under the curve.
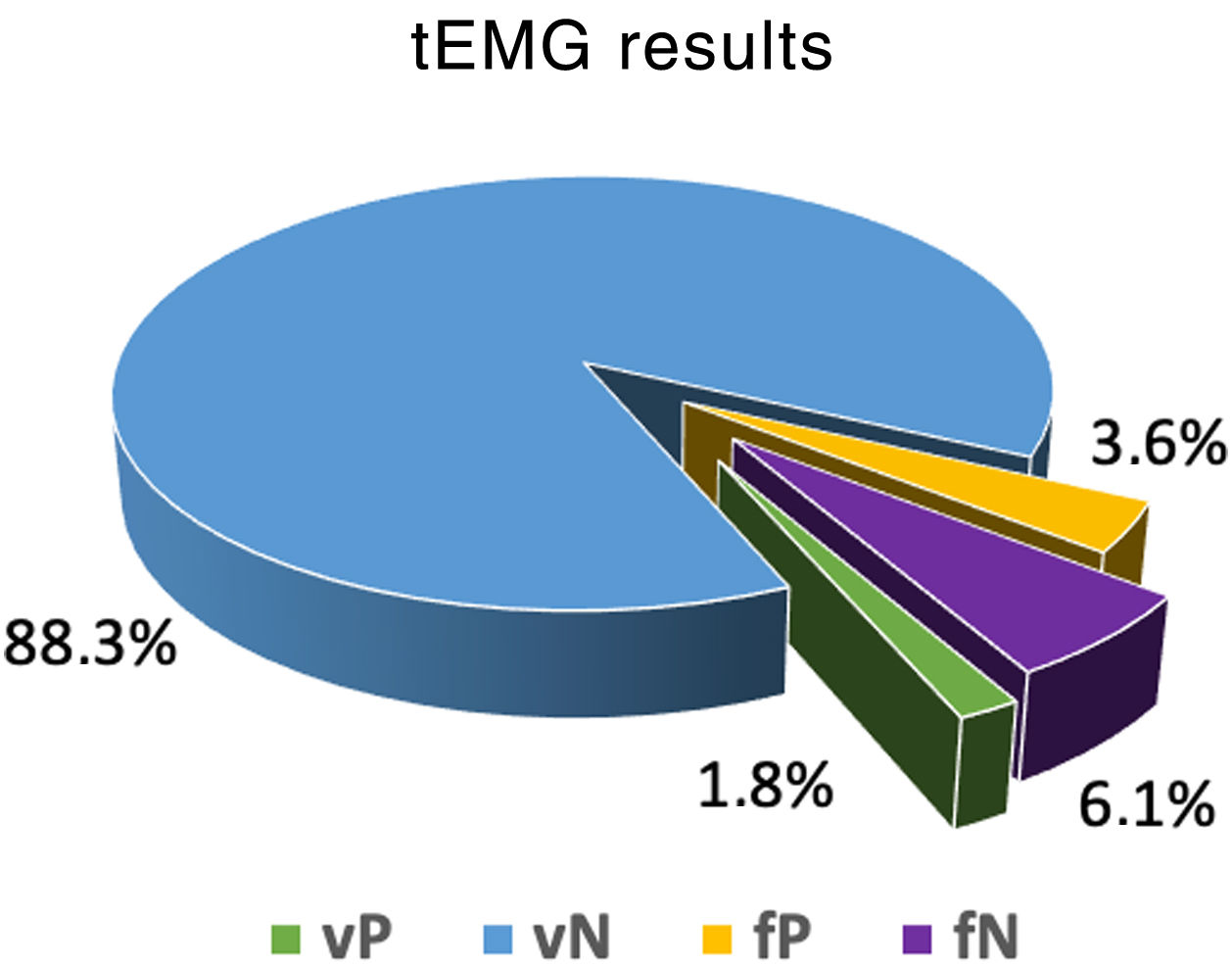
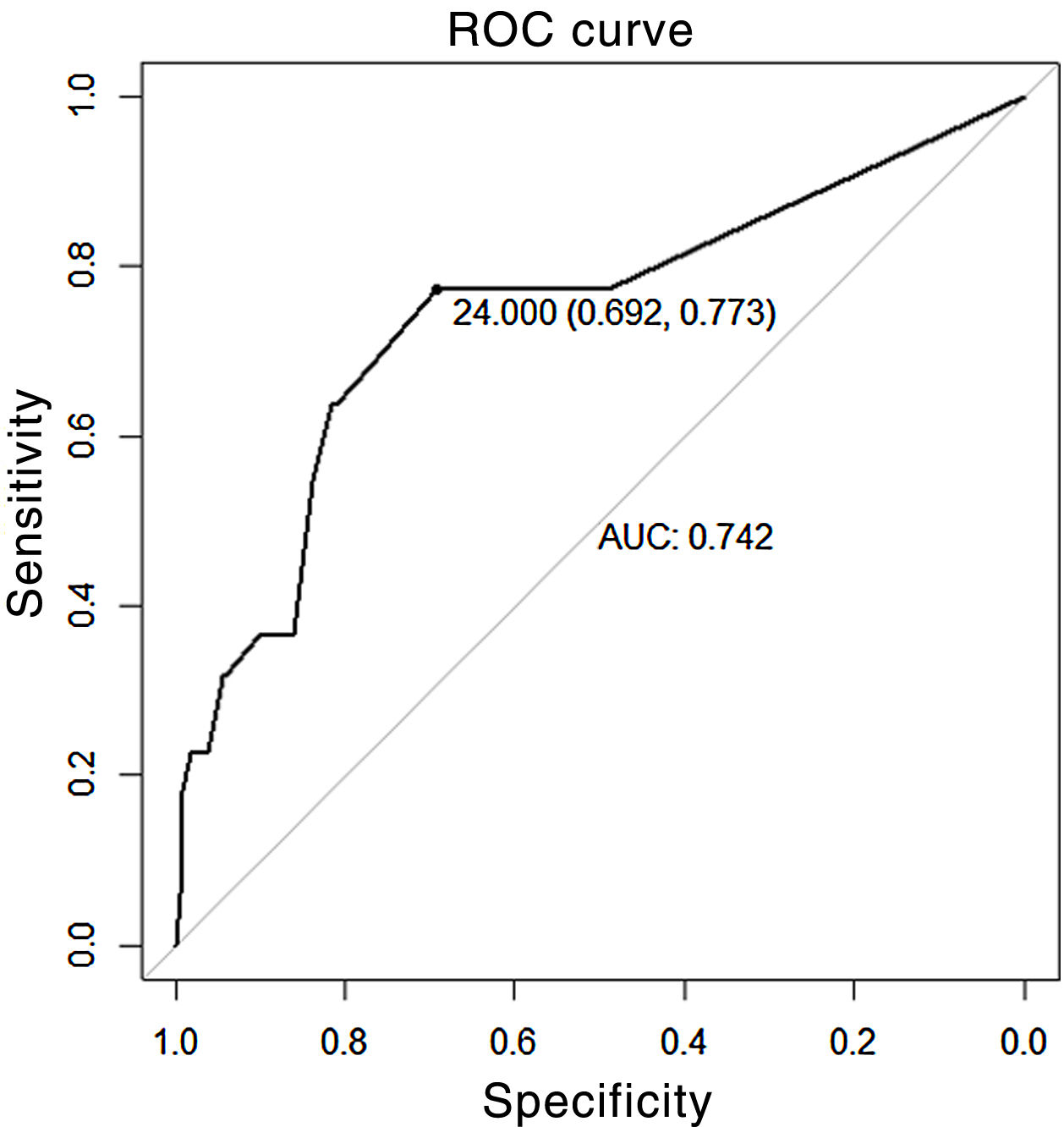
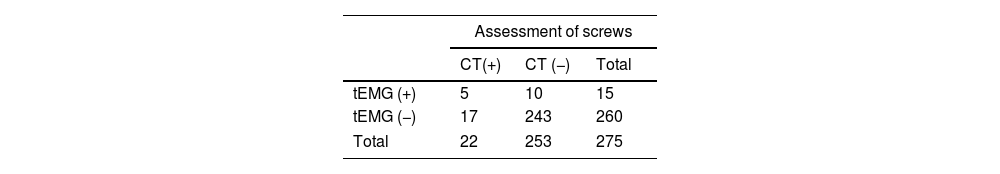
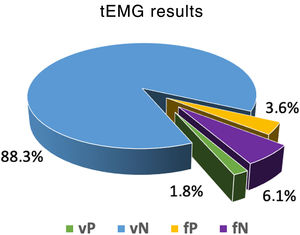
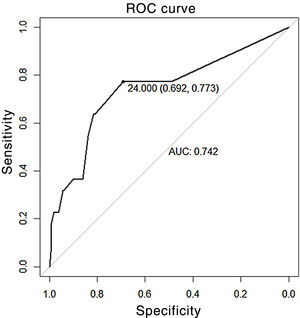
ResultA total of 275 PS were evaluated between L1 to S1; 5 PS showed concordance for an inadequate trajectory, while 10 PS, with tEMG<10mA, were correctly positioned. The postoperative CT identified 17 pedicle gaps not noticed by the tEMG. Sensitivity and specificity were 23% (95% CI: 8–45) and 96% (95% CI: 93–98), respectively, with a PPV of 33.3% and a NPV of 93.6%. The area under the curve was 0.74 (95% CI: 0.62–0.86) with a cut-off point of 24mA, showing a sensitivity of 77% (95% CI: 0.55–0.92) and specificity of 69% (95% CI: 0.63–0.75).
ConclusionGiven its low sensitivity, we do not recommend tEMG as the sole test in the verification of PS. We recommend using a cut-off point ≤8mA as it demonstrated the highest levels of sensitivity and specificity. We do not recommend using high thresholds to increase sensitivity.
La instrumentación con tornillos pediculares (TP) puede comprometer las estructuras neurales adyacentes. La electromiografía evocada (tEMG) es una modalidad del neuromonitoreo intraoperatorio utilizada para asistir la colocación de estos. El objetivo del presente estudio es evaluar la confiabilidad de esta herramienta.
MétodoRevisión retrospectiva de pacientes intervenidos de artrodesis lumbar posterolateral instrumentada desde enero del 2017 hasta diciembre del 2019. Se correlacionaron las imágenes de tomografías computarizadas postoperatorias (TC-postop) con los resultados de la tEMG para cada TP con un umbral de 10mA, y se establecieron la sensibilidad y especificidad de esta herramienta. Se realizó test diagnóstico y la curva característica operativa del receptor para evaluar el área bajo la curva.
ResultadoSe evaluaron 275 TP entre L1 y S1; 5 TP presentaban concordancia para una trayectoria inadecuada, mientras que 10 TP con tEMG<10mA se encontraban correctamente posicionados. La TC-postop identificó 17 brechas pediculares no advertidas por la tEMG. La sensibilidad y la especificidad fueron del 23% (IC 95%: 8-45) y 96% (IC 95%: 93-98), respectivamente, con un valor predictivo positivo (VPP) del 33,3% y un valor predictivo negativo (VPN) del 93,6%. El área bajo la curva fue de 0,74 (IC 95%: 0,62-0,86) con punto de corte de 24 mA, que mostró una sensibilidad del 77% (IC 95%: 0,55-0,92) y una especificidad del 69% (IC 95%: 0,63-0,75).
ConclusiónDada su baja sensibilidad, no aconsejamos la tEMG como prueba única en la verificación de TP. Recomendamos la utilización de un punto de corte ≤8mA, ya que ha demostrado los niveles más altos de sensibilidad y especificidad. No recomendamos el uso de umbrales elevados para aumentar la sensibilidad.
Correct implantation of pedicle screws (PS) is essential in spine surgery.1 An inadequate PS trajectory can cause violation of spinal canal or vertebral foramen, which can result in injury to neurological structures.
Many methods have been developed to assist PS placement. Intraoperative fluoroscopy is the most used, but is not highly accurate.2,3 The O-arm has been demonstrated as the clinical standard, due to its high sensitivity and specificity in detecting incorrect PS positioning intraoperatively,4–7 allowing repositioning in the same surgical procedure and thus avoiding revision surgery. Nevertheless, it is still an expensive technology and not available to all spine surgeons.
Intraoperative neuromonitoring (IONM), specifically in the form of triggered electromyography (tEMG) in which PS are stimulated and responses are recorded in the muscles of the lower extremities, is another tool for determining PS misplacement.8,9 This method warns of contact with underlying neural structures through a pedicle breach (PB) caused by an incorrect screw trajectory. However, the usefulness of this method has not been fully acknowledged.
The aim of the present study was to evaluate the reliability of this tool as a support element in PS placement.
MethodFollowing approval by our institution's Ethics Committee, all patients undergoing instrumented posterolateral arthrodesis of the lumbar spine for degenerative disorders were retrospectively reviewed from January 2017 to December 2019. The presence or absence of PB on postoperative computed tomography (postop CT) images was correlated with intraoperative tEMG values for each screw to establish the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of this tool. We also undertook a diagnostic test analysis, transforming the quantitative variable of mA into a qualitative variable of 2 levels, according to the cut-off threshold, established at 10mA. A receiver operating characteristic (ROC) curve was then calculated to assess the area under the curve (AUC) for this sample, and the corresponding test data were again obtained according to the threshold, with greater sensitivity and specificity. Finally, we analysed demographic data (sex and age), number of screws used, and the levels operated. The statistical analysis was performed using R software version 4.0.2.
The same 2 experienced spine surgeons placed all the screws, from L1 to S1, using the free hand technique, based on anatomical landmarks, with fluoroscopic support and after satisfactory palpation of the pedicle.
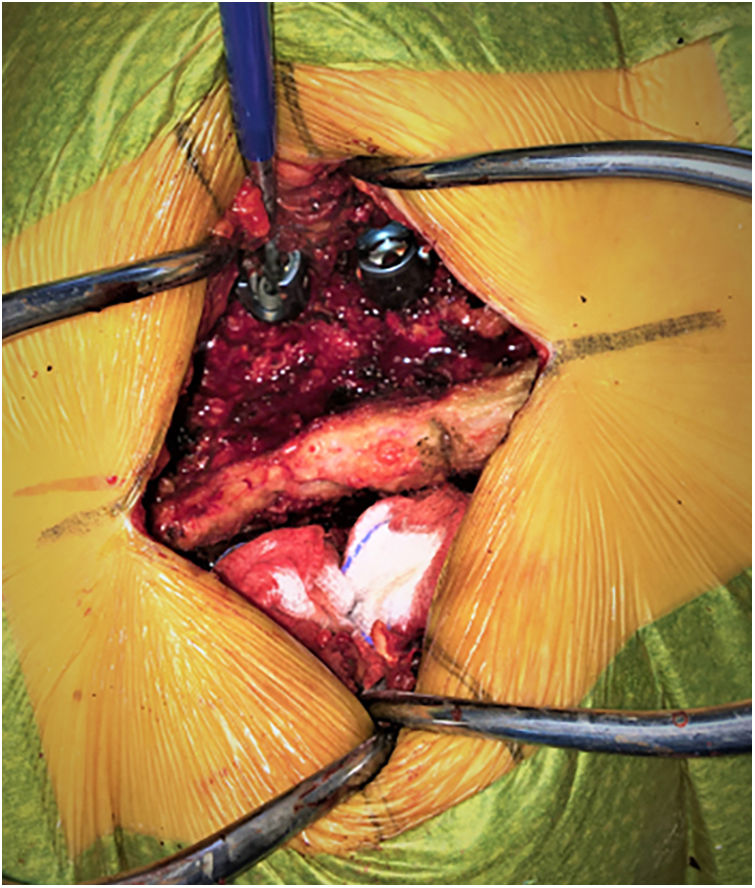
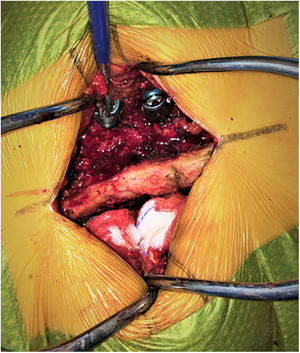
After the PS had been placed and in the absence of neuromuscular blocking agents, they were stimulated using the conventional technique described by Calancie et al.10 Through direct contact of the screw head with the stimulating probe, pulses of constant upward current (0–30mA amplitude with a duration of 200ms and a frequency of 3Hz) were applied until a muscular response was triggered, recorded by needle electrodes placed bilaterally on the lower limb muscles innervated by the roots to be evaluated: the stimulus threshold was obtained in this way for each screw (Fig. 1). Care was taken to apply the stimulation through the axis of the PS and not through its mobile crown, and biological fluids were carefully aspirated. PS with critical tEMG values (e.g., 3mA) were redirected according to surgeons’ perception and intraoperative fluoroscopy image.
The postop CT images, obtained within the first 72h, were evaluated by a third spine surgeon who did not know the tEMG results. PB was defined as protrusion of more than 25% of the diameter of the PT over the superior, inferior, lateral, or medial cortex of the pedicle.11,12
ResultsA total of 57 patients were included, 53.4% female and 47.6% male, with a mean age of 62.14 years (SD±13.74). Of this total, 275 PS were obtained placed between segments L1 and S1. L5 (34.8%) was the most frequently operated segment, followed by L4 (24.6%), and S1 (20.4%).
The tEMG recordings of the IOMN showed 15 PS (5.4%), with a response ≤10mA, while on the postop CT images, 22 PS (8%) showed PB. When correlating the tEMG values with the postop CT images, 5 PS were concordant for an inadequate trajectory (true positive, TP), while 10 PS, with values below our cut-off point, were correctly positioned on postoperative images (false positive, FP). Postop CT identified 17 BP that were not picked up by tEMG (false negative, FN). For the remaining 243 PB the correlation was correct (Table 1 and Fig. 2).
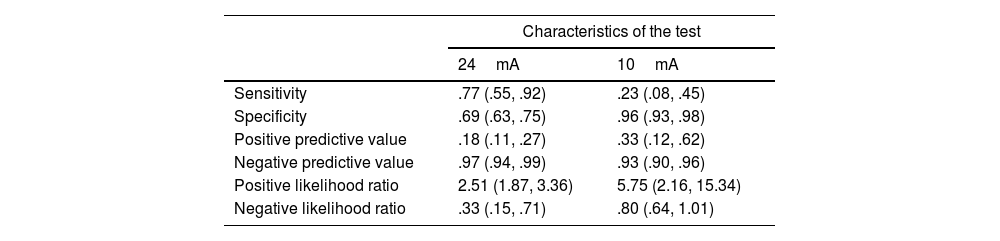
The sensitivity and specificity obtained for a cut-off point of 10mA was 23% (95% CI 8–45) and 96% (95% CI 93–98), respectively, with a PPV of 33.3% and NPV of 93.6%. The positive likelihood ratio was 5.75 (2.16–15.34) and the negative likelihood ratio was .80 (.64–1.01). Applying the COR curve for our study sample, the ABC was .74 (95% CI .62–.86) (Fig. 3), with a cut-off point of 24mA, which was the best combination of sensitivity and specificity: 77% (95% CI .55–.92) and 69% (95% CI .63–.75), respectively (Table 2).
Diagnostic utility with cut-off point of 24mA compared to 10mA.
| Characteristics of the test | ||
|---|---|---|
| 24mA | 10mA | |
| Sensitivity | .77 (.55, .92) | .23 (.08, .45) |
| Specificity | .69 (.63, .75) | .96 (.93, .98) |
| Positive predictive value | .18 (.11, .27) | .33 (.12, .62) |
| Negative predictive value | .97 (.94, .99) | .93 (.90, .96) |
| Positive likelihood ratio | 2.51 (1.87, 3.36) | 5.75 (2.16, 15.34) |
| Negative likelihood ratio | .33 (.15, .71) | .80 (.64, 1.01) |
The objective of IOMN, in its 3 forms, somatosensory evoked potentials, motor evoked potentials, and continuous electromyography (EMG), is real-time detection of iatrogenic injury to neural structures. Its usefulness in surgery for tumours and spinal deformities is recognised in the literature, but has been called into question in other types of disease.13
Electromyography is the most effective way of assessing nerve roots by monitoring the electrical activity of muscle.14 tEMG records the intensity (mA) required to activate muscle after nerve root stimulation via the PS. A correctly positioned implant will require higher intensity to stimulate the nerve root due to the insulation provided by the bone surrounding the pedicle, while the intensity to achieve this response will be much lower in the presence of a PB.15
On analysis of the results of our work we suggest, given the high specificity (96%) and high NPV (93%), that stimulus above 10mA is reliable for us to assume that there is no PB, but the low sensitivity (23%) casts doubt on the reliability of the method as a screening test.
Parker et al.12 correlated tEMG results with postop CT imaging in 2450 PS, with similar specificity (95.9%), but higher sensitivity (69.6%). Of the 115 PS (4.7%) that had a stimulus threshold less than 10mA, only 16 had images showing a PB (TP), while the remaining 99 were correctly positioned (FP); 7 PS with a stimulus threshold greater than 10mA showed PB on images (FN). Ravindra et al.1 compared intraoperative O-arm images with tEMG results with a cut-off threshold of 12mA in 1,006 PS, found 14 TP, 40 FP, and 21 FN and again obtained high specificity values (96%) with low sensitivity values (40%), and a PPV of 26% and NPV of 98% (95% CI: 15–40).
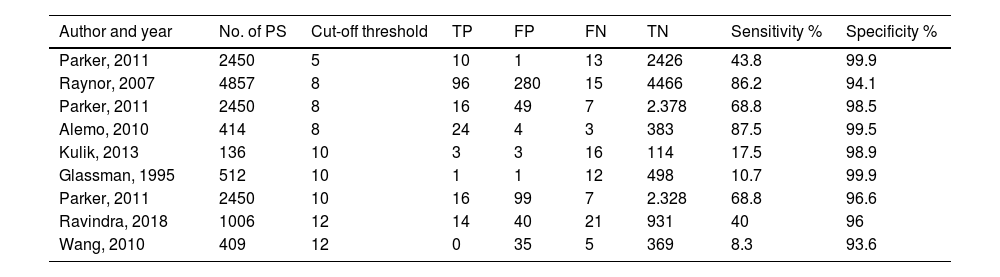
High specificity (100% to 93.6%) and variable sensitivity results (10.7% to 86.2%) have been described in other studies, which shows agreement on the ability of this method to support adequate PS positioning, but not in detecting an inadequate trajectory (Table 3). The study that demonstrated the highest sensitivity rate was that of Raynor et al.,11 who evaluated tEMG results in over 4800 PS, with a 99% likelihood of an adequate PT trajectory when the stimulus response was above 8mA. However, adequate positioning was verified by intraoperative fluoroscopy or pedicle palpation, methods that have been shown not to be fully reliable.16–18
tEMG results in different studies with their respective cut-off thresholds.
| Author and year | No. of PS | Cut-off threshold | TP | FP | FN | TN | Sensitivity % | Specificity % |
|---|---|---|---|---|---|---|---|---|
| Parker, 2011 | 2450 | 5 | 10 | 1 | 13 | 2426 | 43.8 | 99.9 |
| Raynor, 2007 | 4857 | 8 | 96 | 280 | 15 | 4466 | 86.2 | 94.1 |
| Parker, 2011 | 2450 | 8 | 16 | 49 | 7 | 2.378 | 68.8 | 98.5 |
| Alemo, 2010 | 414 | 8 | 24 | 4 | 3 | 383 | 87.5 | 99.5 |
| Kulik, 2013 | 136 | 10 | 3 | 3 | 16 | 114 | 17.5 | 98.9 |
| Glassman, 1995 | 512 | 10 | 1 | 1 | 12 | 498 | 10.7 | 99.9 |
| Parker, 2011 | 2450 | 10 | 16 | 99 | 7 | 2.328 | 68.8 | 96.6 |
| Ravindra, 2018 | 1006 | 12 | 14 | 40 | 21 | 931 | 40 | 96 |
| Wang, 2010 | 409 | 12 | 0 | 35 | 5 | 369 | 8.3 | 93.6 |
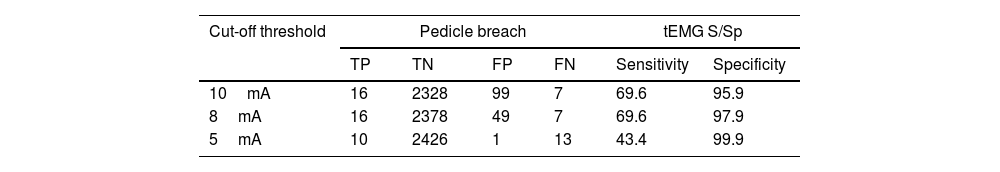
The response threshold is a variable closely related to the sensitivity and specificity of this method. In the abovementioned study by Parker et al.,12 the authors evaluated different thresholds within the same sample, and identified that, as the stimulus threshold decreases, the number of FP and TP decreases (specificity) while FN and TN increase (sensitivity), demonstrating that specificity is inversely proportional, and sensitivity is directly proportional to the stimulation threshold (Table 4).
List of tEMG results at a different threshold.
| Cut-off threshold | Pedicle breach | tEMG S/Sp | ||||
|---|---|---|---|---|---|---|
| TP | TN | FP | FN | Sensitivity | Specificity | |
| 10mA | 16 | 2328 | 99 | 7 | 69.6 | 95.9 |
| 8mA | 16 | 2378 | 49 | 7 | 69.6 | 97.9 |
| 5mA | 10 | 2426 | 1 | 13 | 43.4 | 99.9 |
Taken from Parker et al.12
The influence of the response threshold is replicated in our work through analysis of the ROC curve and evaluation of the AUC, in which, to achieve a sensitivity of 77%, a stimulus threshold of 24mA is required, at the expense of a decrease in specificity (higher number of FP).
Most studies advise using a threshold between 6 and 10mA to maintain acceptable levels of sensitivity and specificity.12,19,20 Two systematic reviews and meta-analyses showed high specificity with relatively low sensitivity (up to 22% of poorly placed PS can be missed with tEMG), where according to the ROC AUC analysis, a stimulus threshold between 8 and 12mA gives the highest sensitivity and specificity values (82% and 97%, respectively) with a diagnostic odds ratio of 147.95.21,22
Although both CT and O-arm are the most sensitive and specific methods for assessing the trajectory of the PS, the metallic artefact generated by these methods overestimates the dimensions of the PT by up to 1mm23 and makes it difficult to assess cortical margins, complicates image evaluation and makes it not always possible to distinguish between the presence and absence of a PB. This is demonstrated by the different incidence rates of BP detected this way (from 4.2% to 32.4%) in the medical literature.24
The limitations of this study are, firstly, its retrospective nature; secondly, the sensitivity result may have been affected by the study design, which is not suitable for this type of analysis, and by the relatively small sample size. In relation to this, the NPV may have been compromised by the low sensitivity (tests with high NPV classically have high sensitivity). Finally, we did not classify the size of the breach, which may influence the tEMG results, nor did we distinguish the direction of the breach (medial, lateral, superior, or inferior). Although medial breaches carry a higher risk of neurological injury, the biomechanical stability of the construct can be compromised by any type of breach and therefore they need to be identified.
ConclusionThe tEMG is an additional tool to assist in the instrumentation of the lumbar spine. Given its low sensitivity, it is not advisable to use it as a sole test to verify a PS. It is also subject to multiple external variables, such as the patient's bone density, impulse transmission by biological fluids, anaesthesia, and state of relaxation or other clinical conditions (such as hypoglycaemia, electrolyte abnormalities, hypoxia, etc.)25,26 that could alter the results of the test.
We recommend using a cut-off point ≤8mA, as this has been shown to have the highest levels of sensitivity and specificity in the medical literature. Based on our results, we do not recommend using high thresholds to maximise the sensitivity of the method, as this leads to a loss of specificity and increased FP, with the consequent risk of unnecessary PS revision and delayed surgery time.
The spine surgeon must understand the advantages and limitations of tEMG, and always use it in conjunction with other methods, ideally O-arm.
Level of evidenceLevel of evidence IV.
Conflict of interestsNone declared.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.