Complex distal femoral fracture (DFF) in the elderly patient is an infrequent but challenging scenario. In these fragile patients, DFF is associated with a high rate of medical complications and mortality. The optimum treatment remains controversial. Our aim is to propose our standard treatment, describe our results and discuss its clinical relevance. We describe three cases of elderly and fragile patients with multiple comorbidities who suffered a complex DFF after low energy trauma. They were successfully treated through a primary arthroplasty with distal femoral replacement (DFR). All the three patients presented early full weight-bearing mobilization (average time to first ambulation was five days), good functional outcome (mean knee range of motion was 103°) and short hospital length of stay (mean of ten days). According to our experience, primary arthroplasty with DFR could be a good therapeutic option for complex DFF in elderly patients.
La fractura femoral distal (FFD) compleja en el paciente anciano es infrecuente, pero su manejo es un desafío. En estos pacientes frágiles, la FFD se asocia a un elevado riesgo de complicaciones médicas y mortalidad. Su tratamiento óptimo sigue siendo controvertido. El objetivo del estudio es proponer nuestro tratamiento estándar, describir nuestros resultados y discutir su relevancia clínica. Reportamos 3 casos de pacientes ancianos y frágiles con múltiples comorbilidades que sufrieron una FFD compleja a causa de un traumatismo de baja energía. Fueron tratados con éxito mediante un reemplazo femoral distal (RFD). Los 3 pacientes presentaron una movilización precoz con carga completa (la media hasta la primera deambulación fue 5 días), buenos resultados funcionales (la media de rango de movimiento de la rodilla fue 103̊) y una estancia hospitalaria breve (media de 10 días). Según nuestra experiencia, la artroplastia primaria podría ser una buena elección terapéutica para las FFD complejas en los pacientes ancianos.
Complex distal femur fracture (DFF) (type 33C in the AO/OTA classification) in the elderly and fragile patient is a challenging scenario. This intra-articular fracture is usually linked to bone fragility, comminution and bone loss stock. Although they account for less than 1% of all fractures, their incidence is likely to increase with the rising geriatric populations.1 DFF is associated with a high rate of medical complications. Mortality at one year has been found to be as high as 25–50%.2–4 Current therapeutic options broadly include conservative management, internal fixation and primary total knee arthroplasty (TKA).1 Arthroplasty aim to be a single definitive procedure allowing early post-operative mobilization and functionality restoration.1
Reports on TKA with distal femoral replacement (DFR) is limited due to the low incidence of these fractures. There are mixed results and poor evidence.4–10 Therefore, it is difficult to have large samples and make comparisons between groups. Follow up is also short due to the high mortality of these fragile patients.
We present a retrospective report of three fragile elderly patients who suffer a complex DFF and are treated through a DFR. Our aim is to propose our standard treatment, describe our results and discuss its clinical relevance.
Clinical caseCase 1: An eighty-seven-year-old woman presented to our emergency room with pain, immobility and deformity in her right knee after a low energy trauma. Her past medical history reflected diabetes, hypertension and peripheral vascular disease (Table 1). She lived at home, was independent in basic activities of daily living (BADL) and was able to walk with an assistive device. The patient also had a history of previous knee osteoarthritis. X-ray images (Fig. 1A and B) demonstrated a supraintercondylar femoral fracture (type 33-C3). Hyperglycemia and hypertension were controlled before surgery. Anemia, bleeding disorders and urinary tract infection (UTI) were ruled out. Finally, a primary arthroplasty (DFR) was performed.
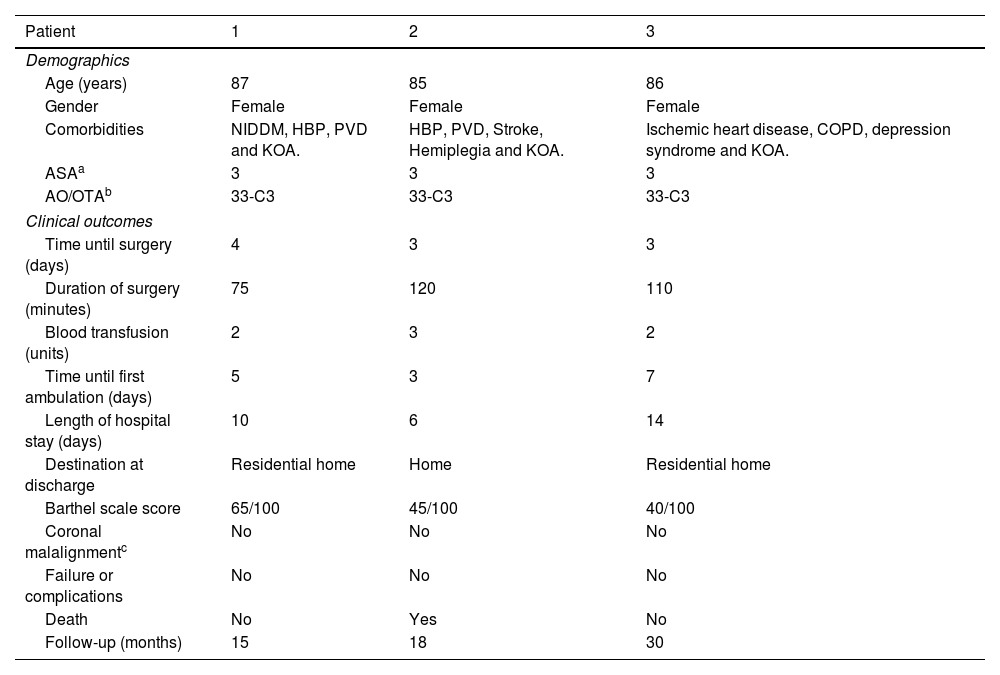
Characteristics of the patients, peri-operative and post-operative clinical outcomes.
| Patient | 1 | 2 | 3 |
|---|---|---|---|
| Demographics | |||
| Age (years) | 87 | 85 | 86 |
| Gender | Female | Female | Female |
| Comorbidities | NIDDM, HBP, PVD and KOA. | HBP, PVD, Stroke, Hemiplegia and KOA. | Ischemic heart disease, COPD, depression syndrome and KOA. |
| ASAa | 3 | 3 | 3 |
| AO/OTAb | 33-C3 | 33-C3 | 33-C3 |
| Clinical outcomes | |||
| Time until surgery (days) | 4 | 3 | 3 |
| Duration of surgery (minutes) | 75 | 120 | 110 |
| Blood transfusion (units) | 2 | 3 | 2 |
| Time until first ambulation (days) | 5 | 3 | 7 |
| Length of hospital stay (days) | 10 | 6 | 14 |
| Destination at discharge | Residential home | Home | Residential home |
| Barthel scale score | 65/100 | 45/100 | 40/100 |
| Coronal malalignmentc | No | No | No |
| Failure or complications | No | No | No |
| Death | No | Yes | No |
| Follow-up (months) | 15 | 18 | 30 |
NIDDM: Non-Insulin-Dependent Diabetes Mellitus. HBP: High Blood Pressure. PVD: Peripheral Vascular Disease. COPD: Chronic Obstructive Pulmonary Disease. KOA: Knee Osteoarthritis.
Case 2: An eighty-five-year-old woman was referred to our hospital presenting a supraintercondylar femoral fracture (type 33-C3). She suffered from multiple medical comorbidities; highlighted among them were stroke with residual hemiplegia and peripheral vascular disease (Table 1). She also had pre-existing knee osteoarthritis. The patient presented mild-moderate dementia and was dependent in BADL. She lived at home and was able to walk indoors with an assistive device. Medical optimization consisted on pharmacologically controlling her hypertension and ruling out anemia, bleeding disorders and UTI. We decided that a DFR would be the best option.
Case 3: An eighty-six-year-old woman presented to our hospital with the diagnosis of a supraintercondylar femoral fracture (type 33-C3) after a ground-level fall. She suffered from severe comorbidities; ischemic heart disease and chronic obstructive pulmonary disease (Table 1). She presented previous knee osteoarthritis. The patient lived at home and walked with assistive device. She was dependent in BADL. Blood and urine tests showed no abnormalities. Pharmacological treatment was adjusted to improve pulmonary and cardiac function. After medical optimization, a DFR was implanted.
ResultsSurgical techniquePreoperatively, a CT scan was performed to determine fracture's morphology and plan the surgery. Patients were medically optimized through a multidisciplinary approach (including ortho-geriatrics). Blood and urine tests were performed to rule out anemia, bleeding disorders or UTI. When medical conditions were controlled and anesthesia and surgery were considered safe, the patient was fit to undergo surgery. The operations were performed by senior orthopedic surgeons from the knee unit.
Under antibiotic prophylaxis (intravenous cefazolin: 2g preoperatively, and 1g every 8h for 24h postoperatively) and spinal anesthesia, the patient was placed in the supine position. Anterior skin incision, under tourniquet, was made with a medial para-patellar arthrotomy extended proximally as needed. No osteotomy of the anterior tibial tubercle was necessary. Before removing the distal femur, a ruler was used to measure the distance between the level of the fracture and the native joint-line. This distance was then used for femoral reconstruction. The distal femur was cut immediately above the proximal extent of the fracture and measured to get the proper length and tension to the implant. By protocol, cultures were taken to rule out infection. TKA with DFR (Endo-Model Modular rotational with DFR component; Waldemar Link®, Gmbh, Hamburg, Germany) and fully cemented stem was implanted in the femoral side. Tibia and patella were also revised, using a long and fully cemented stem for tibia. In all cases, antibiotic-loaded cement was preferred (Vancogenx®, Tecres, Verona, Italy). Distal plug, pulsatile lavage, cement gun and cement pressuring devices were used. Finally, hemostasis was reviewed before wound closure. Drains were not used. Post-operatively, immediate full weight-bearing was allowed as tolerated and rehabilitation was conducted under supervision.
The patients were reviewed at two weeks, one, three, and six months after surgery. Thereafter, they were controlled annually. Anteroposterior and lateral knee X-ray and lower limb telemetry were performed. Radiographic controls were considered adequate if no complications were observed (osteolysis, loosening, stress shielding, radiolucent lines, etc.). Operated knees were examined to asses surgical wound, stability, ROM and pain.
Case 1: The duration of the surgery was 75min, and she required two units of blood transfusions. Post-operative X-ray images showed a correct implantation (Fig. 1C and D). Although immediate full-weight bearing was authorized, time until first ambulation was five days (Table 1). Ten days after surgery, the patient was discharged to a residential home. After fifteen months of follow up, she presented good functionality and no complications have appeared. Her Barthel scale score was 65/100 (moderate dependency), her knee range of motion (ROM) was 90° (0–90°) and she was able to walk with an assistive device.
Case 2: Surgery lasted 120min, and three units of blood transfusions were required. Post-operative evolution was satisfactory. The patient started ambulation three days after surgery and was discharged to her own home three days later (Table 1). Her Barthel scale score was 45/100 (severe dependency), the knee ROM was 120° (0–120°) and she was able to walk indoors with an assistive device. Unfortunately, after eighteen months of follow-up, the patient dead due to a non-related to the knee cause.
Case 3: Surgery duration was 110min, and two units of blood transfusions were used. First ambulation was achieved seven days later. During hospitalization, she did not present medical complications. However, as the patient was especially fragile and presented severe comorbidities, we decided to keep her admitted until she was fully recovered. The patient presented a relatively longer length of hospital stay (fourteen days). She was discharged to a residential home (Table 1). Her Barthel scale score was 40/100 (severe dependency). She was able to walk with assistive device, with a knee ROM of 100° (5–105°). After thirty months of follow up, the patient still satisfied with the procedure.
DiscussionWe present a report of three elderly patients suffering a DFF and being successfully treated through a DFR. Although each case presents its unique characteristics, the three patients have similar medical history and common therapeutic objectives.
Internal fixation is a therapeutic option for DFF in elderly. However, despite new fixation methods (including minimally invasive plate osteosynthesis and retrograde intramedullary nailing), complications such as non-union remain common, with a reported incidence between 6% and 20%.1,9 Bone fragility, comminution and bone loss stock at the fracture site are responsible for the difficulty of fixation and the secondary loss of reduction. Besides, extensive intra-articular involvement and previous osteoarthritis are not unusual. Taking in account that the best for the fragile patient with a high morbidity and disability is to make a single-definitive surgery, it seems that primary TKA would provide a rapid and functional recovery. In addition, TKA provides immediate post-operative mobilization and weight-bearing, avoiding bedridden and decreasing the risk of decubitus-related complications. In consequence, TKA with DFR could be especially recommended in elder and fragile patients suffering complex DFF with intra-articular involvement, comminution, bone loss stock and previous osteoarthritis. Hart et al.9 found no statistically significant differences in post-operative complications nor in reoperations when comparing DFR and internal fixation. However, they highlighted that all patients in the DFR group were ambulatory after one year, while 25% of patients in the internal fixation group were wheelchair bound. Pearse et al.8 defended that advantages of primary arthroplasty were a greater proportion of patients returning to independent walking, more rapid rehabilitation and better knee flexion. On the other hand, internal fixation was associated with a decreased need of blood transfusion, lower rate of knee pain and better Oxford knee score at follow up.
Following DFR, our patients presented early mobilization and good functional outcome. Their knee ROM were 90°, 120° and 100° respectively, their average time to first ambulation was five days and all of them returned to full weight-bearing ambulation with an assistive device. This delay until first ambulation could be explained by their age, fragility and previously limited functionality. Other series using DFR reported similar functional outcomes. Hart et al.9 and Appleton et al.4 defended that at one year after injury all patients had regained their previous level of mobility. Other studies1,5,8 reported a post-operative ROM between 75° and 140°, and a time until first ambulation of 3–4 days. However, Boureau et al.6 stated that despite immediate weight-bearing, patients suffered a considerable loss of autonomy. On the other hand, internal fixation series tend to offer worse early functional outcomes.8,9 The rate of wheelchair dependent patients has been reported to be between 23% and 25%, and length of hospital stay between 7.5 days and 23 days. Pearse et al.8 presented a mean time until first ambulation of 9.5 days and a mean knee flexion of 75°.
Complications in these patients undergoing primary TKA are not uncommon, but it is unclear if the complication rate is higher or lower than that of the fixation procedures.1,8–10 We did not have any medical or implant complication during hospitalization despite patients’ comorbidities (all patients were ASA-3). Appleton et al.4 reported an all-cause reoperation rate of 18.1% at three-year follow-up. Boureau et al.,6 despite of high comorbidity rate (62% ASA-3), had a revision rate of 9.5%. Infection was the most common complication with a reported incidence between 4% and 50% among series.4–7,9 Another controversial aspect regarding the use of constrained prosthesis is their high loosening rate. Although long-term survival is not well studied due to the limited follow-up, most of the studies present a low revision rate (0–18%).4,6,10 These patients tend to be low demanding and, therefore, with less loosening probability.10
Our mean time of surgery was 102min, and mean transfusion units required were two; similar than other published series.5,8
In order to minimize the incidence of complications in fragile patients, a multidisciplinary management including ortho-geriatrics is recommended. As in hip elderly fractures, it is very important to stabilize and optimize the patient before, during and after surgery in order to reduce mortality and disability.3 Complex DFF entails a high mortality rate, 25–50% after one year.2–4 In our series, one patient died at 18 months after surgery. Appleton et al.4 found that the mortality within the first year after fracture was 41.1%, rising to 82.0% after five years and 97.3% after 10 years.
There are some limitations to the current study, including those inherent in any retrospective study without a control group. As it is a report of three cases, sample size is small. Follow up is relatively short, but similar to other articles. On the other hand, the patients’ homogeneous treatment is a strength of this study.
In conclusion, the approach to this type of fracture is highly complex. According to our experience, DFR could be a good therapeutic option for complex DFF in elderly patients. It restores functionality rapidly, allowing immediate post-operative mobilization, full weight-bearing and relatively short hospital length of stay.
Authors’ contributionsAll authors contributed equally to this work. All authors (NJ, OP and SP) contributed to the design of the study, data recollection, statistical analysis and writing of the manuscript. All authors read and approved the final manuscript.
Consent to participate and publicationPatients or familiars accepted to participate in this retrospective observational study. They were informed that data concerning their cases might be submitted for publication, and they gave their consent.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Level of evidenceLevel of evidence iv.
Conflict of interestsThe authors have no conflict of interests to declare.
We wish to thank Russell Williams of RoundlyWorded.com for his editorial recommendations.