Knee Ostheochondritis Dissecans is an osteochondral disease, whose treatment is still debated. The purpose this study was to analyze the patients attached with bioabsorbable nail, assisted by arthroscopy.
Material and methodAnalysis was performed using median and interquartile range (P25–P75), with a follow-up of 9 patients (10 knees) operated for stage III osteochondral lesions. After a minimum of 12 months, the KOOS, IKDC, satisfaction questionnaires were evaluated and a MR control was performed.
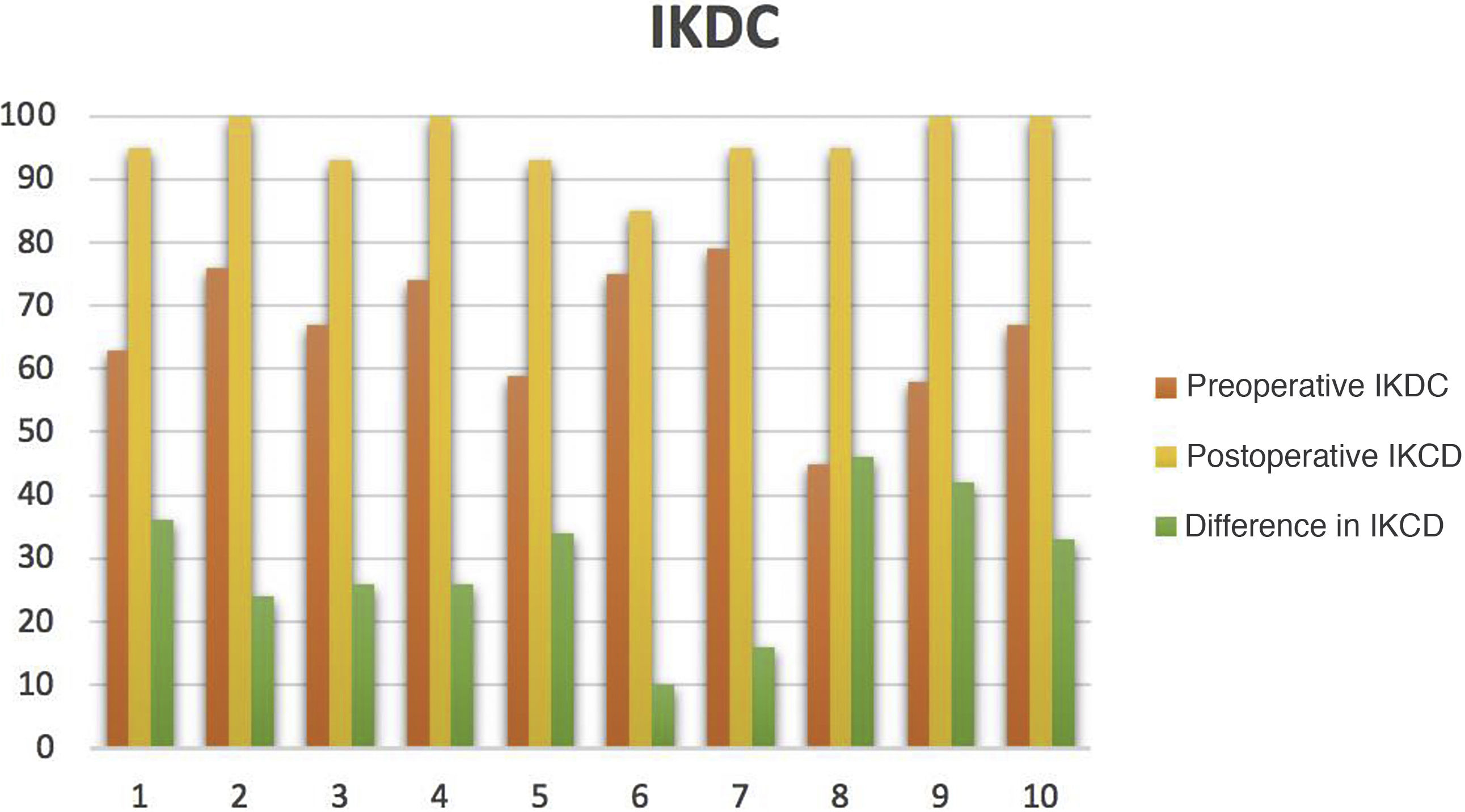
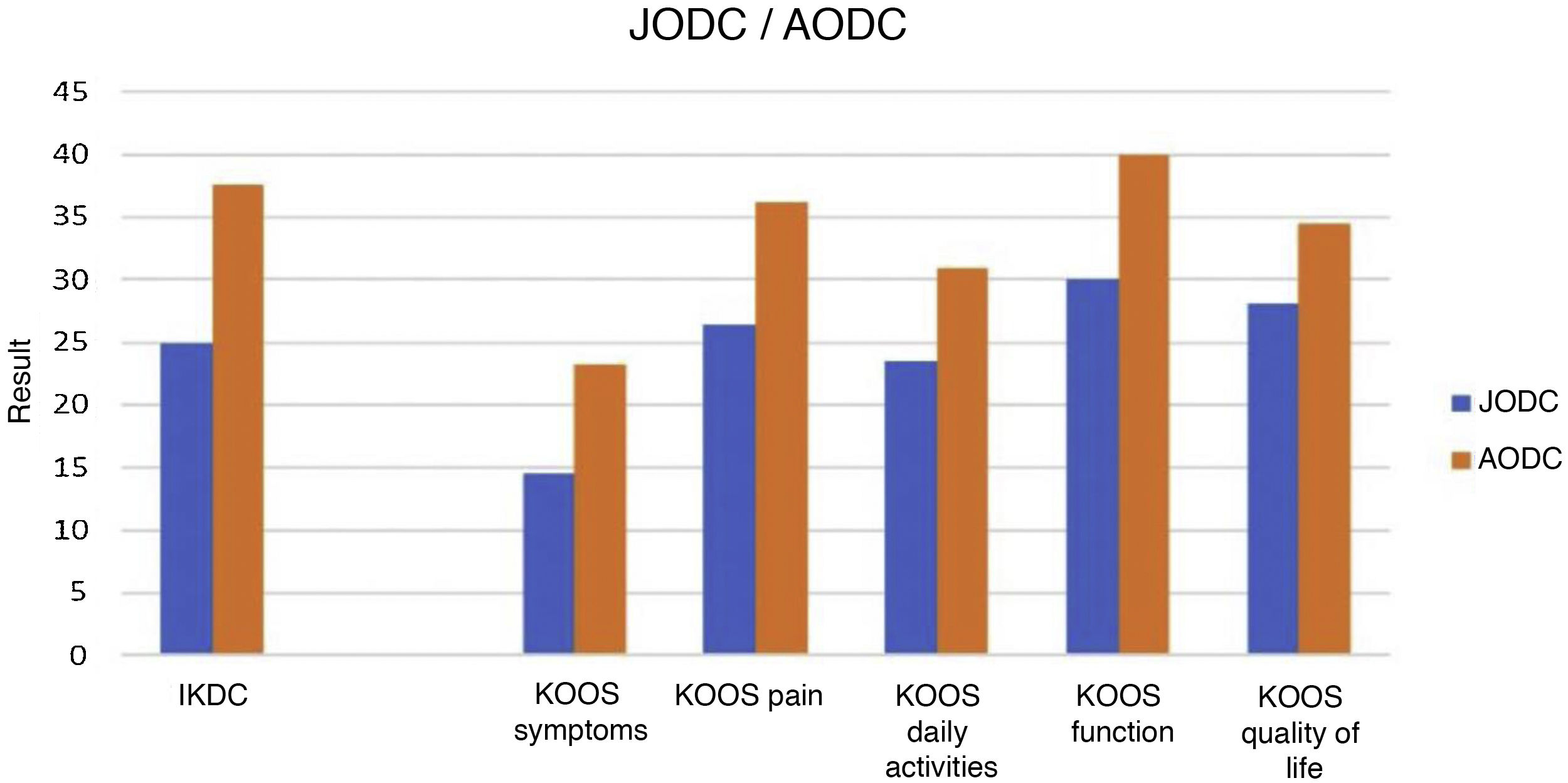
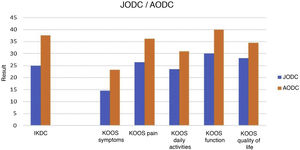
ResultsBone healing was observed in 80% of patients in the first year, with a delay in union in 20%. The median for age was 15 years. The average follow-up was 5′93 years. All cases were located in the internal condyle. The OCD lesions did not show comminution or necrosis. The 40% of stable lesions, according to preoperative MR, were unestable in arthroscopy and it were attached with internal nail. Two groups of osteochondral lesions were differentiated: juvenile OCD (60%) and adult OCD (40%); all of them were stage III lesions. IKDC questionnaire results were an improvement of 29′5 (22′25, 37′52). In the KOOS questionnaire, an improvement was obtained in symptoms of 18′07, in pain of 29′12, in daily living 25′53, in function (sports, recreational activities) of 35 and in quality of life of 34′42.
ConclusionsThe bioabsorbable nail is a valid, reproducible option for unestable entire lesions, with an improvement in function, quality of life, and with a low rate of complications.
La osteocondritis disecante (OCD) de rodilla es una patología osteoarticular, cuyo tratamiento aún sigue estando debatido. Nuestro objetivo fue analizar los pacientes intervenidos mediante fijación interna con implante bioabsorbible, asistido por artroscopia.
Material y métodosSe realizó análisis utilizando mediana y rango intercuartílico (P25–P75), con un seguimiento de 9 pacientes (10 rodillas) intervenidos con fijación por lesión osteocondral grado III. Tras un mínimo de 12 meses, fueron evaluados los cuestionarios KOOS, IKDC, la satisfacción y fue realizado un control de RNM.
ResultadosSe observó consolidación ósea por RNM en el 80% de las intervenciones en el primer año, con un retardo de consolidación en el 20%. La mediana para la edad fue de 15 años. La media de seguimiento fue de 5′93 años. Los 10 casos tuvieron localización en el cóndilo interno. Las OCD no presentaban conminución ni necrosis. El 40% de las lesiones valoradas preoperatoriamente en RNM como estables, se describieron como inestables bajo artroscopia, precisando fijación interna. Fueron diferenciados 2 grupos de osteocondritis: OCD juvenil (60%) y OCD del adulto (40%). En cuanto al cuestionario IKDC, se obtuvo una mejoría de 29′5 (22′25, 37′52). En KOOS, se obtuvo una mejoría en síntomas de 18′07, en dolor de 29′12, en actividades cotidianas de 23′53, en función (deporte, actividades recreativas) de 35 y en calidad de vida de 34′42.
ConclusiónEl implante bioabsorbible es una opción válida, reproducible, para lesiones inestables con integridad de la lesión, con una gran mejora de la función, de la calidad de vida y con escasez de complicaciones.
The natural history of osteochondritis dissecans may include spontaneous healing or progressive worsening. Age is described as a determining factor. The likelihood of healing in patients with open physis without surgical treatment can be high.1,2 However, in cases of non-union, patients may experience lingering symptoms for years until osteochondral fragment detachment occurs, resulting in early joint degeneration.2 Age being the main prognostic factor, the stability, size and location of the lesion have also been described as factors influencing the decision for surgical treatment.
The clinical picture will determine the course of treatment, irrespective of the results of complementary tests. The treatment of osteochondritis dissecans is currently controversial.3 The existing scientific evidence is based primarily on retrospective studies of small sample size and expert opinion.
Conservative treatment, with initial non-weight bearing and restriction of sports activities, is used in cases with stable lesions, especially in cases of juvenile osteochondritis dissecans (JOCD). Some studies have presented consolidation rates of 50%–60% in JOCD, with a lower percentage in patients with closed physes, adult osteochondritis dissecans (AOCD).5
Regarding surgical treatment, there are publications with variable healing rates, that reach 100% in some cases. Drilling is indicated in stable lesions when conservative treatment has not been effective. However, in unstable lesions, the fragment requires internal fixation to maintain its stability, even in displaced fragments that maintain their macroscopic structure with intact cartilage.6 Different types of implants have been described (metal pins, staples, screws with or without head and, more recently, bioabsorbable implants). Bioabsorbable implants are being used increasingly, mainly because they do not require a second surgery to remove them.7
In situations when the fragment cannot be synthesised, and there is therefore a defect in the articular surface, the option of joint preservation surgery techniques (osteochondral autograft transplantation surgery, autologous matrix-induced chondrogenesis together with bone autograft and fresh osteochondral allograft, among others) is considered. Microfractures have been described to fill spaces of up to 4cm2 and, although short-term results can be satisfactory, joint function and condition deteriorate in the long term.8
The aim of this study was to analyse the results of internal fixation, using a bioabsorbable implant, in a series of unstable OCD cases, assessing functional results and complications.
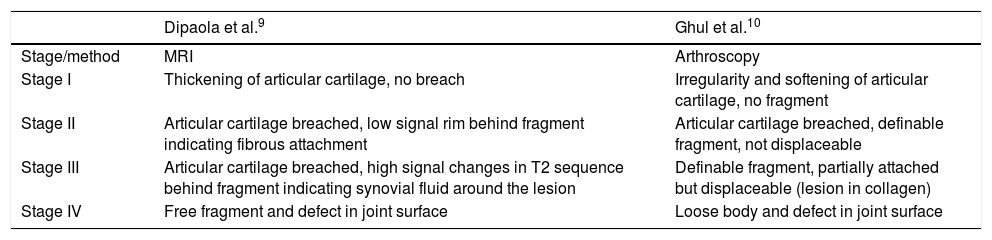
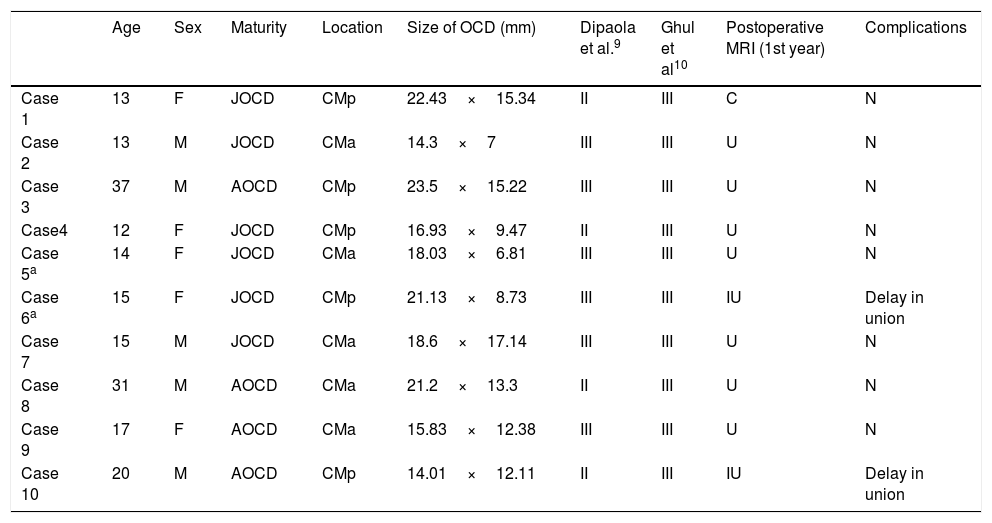
Material and methodsA retrospective study was conducted of a prospective cohort, including interventions under the diagnosis of osteochondritis dissecans, with a total of 9 patients (10 knees). This registration took place from 2007 to 2018, after approval by the Research Committee of the Hospital Universitario Costa del Sol. Patients diagnosed with unstable osteochondritis dissecans by pre-operative MRI, with failure of conservative treatment, implanted with a bioabsorbable implant and with a minimum follow-up of one year were included in the study. Records were made of preoperative and one-year follow-up questionnaires, as well as pre- and postoperative radiographs and MRI. All the patients underwent internal fixation with a bioabsorbable implant via arthroscopy. A database from our hospital was used for this purpose, by means of the HP Doctor® programme (Hewlett Packard, Palo Alto, CA, USA). The variables recorded were sex, age, laterality, date of surgery, date of last consultation, lesion location, lesion size, Dipaola staging9 according to preoperative MRI (Table 1), physis status, associated lesions, intraoperative Ghul staging10 (Table 1), complications, preoperative-postoperative International Knee Documentation Committee (IKDC) Subjective Knee Form,11 preoperative-postoperative Knee injury, and Osteoarthritis Outcome Score (KOOS) and satisfaction rating (Likert scale). One patient was excluded for not complying with follow-up.
Classifications of osteochondritis dissecans.
| Dipaola et al.9 | Ghul et al.10 | |
|---|---|---|
| Stage/method | MRI | Arthroscopy |
| Stage I | Thickening of articular cartilage, no breach | Irregularity and softening of articular cartilage, no fragment |
| Stage II | Articular cartilage breached, low signal rim behind fragment indicating fibrous attachment | Articular cartilage breached, definable fragment, not displaceable |
| Stage III | Articular cartilage breached, high signal changes in T2 sequence behind fragment indicating synovial fluid around the lesion | Definable fragment, partially attached but displaceable (lesion in collagen) |
| Stage IV | Free fragment and defect in joint surface | Loose body and defect in joint surface |
Patients presenting with a suspected OCD knee injury underwent weightbearing AP and L x-ray, axial, and tunnel projection of both knees. Teleradiography was also performed to measure the mechanical axis. An MRI was requested for x-ray results suggestive of OCD. After the initial OCD diagnosis, conservative treatment was started, consisting of non-weight bearing for 2–3 weeks, followed by physiotherapy and restriction of high-risk sports activities during this phase of treatment. The aim was to reduce oedema, improve mobility, muscle trophism and proprioception. From the 6th month onwards, surgery was considered if clinical signs persisted and MRI findings indicated signs of instability12 (line of high intensity in T2 sequence below the injury, multiple cystic area o>5mm, line of high intensity through cartilage and/or focal joint defect).
Surgical techniqueStandard exploratory arthroscopy was performed to confirm the injury and degree of instability. The patient was placed in the supine position, under intradural anaesthesia, the limb placed in a thigh support and an ischaemia cuff used at the root of the affected limb at a pressure between 250−300mmHg. Antibiotic prophylaxis consisted of intravenous cefazolin 2g, or in case of allergy, intravenous clindamycin 600mg. The injury was assessed via anteromedial and anterolateral portals and internal fixation performed in all cases using SmartNail® bioabsorbable implants (ConMed, Largo, USA) in a non-parallel arrangement. The minimum number of implants was 2; a third implant was used for larger sizes. After observing the stability of the injury, integrity, and absence of locking during flexion, extension and rotation, the surgery was completed. Correct haemostasis was performed, ending with closure of the portals and placement of a compressive bandage.
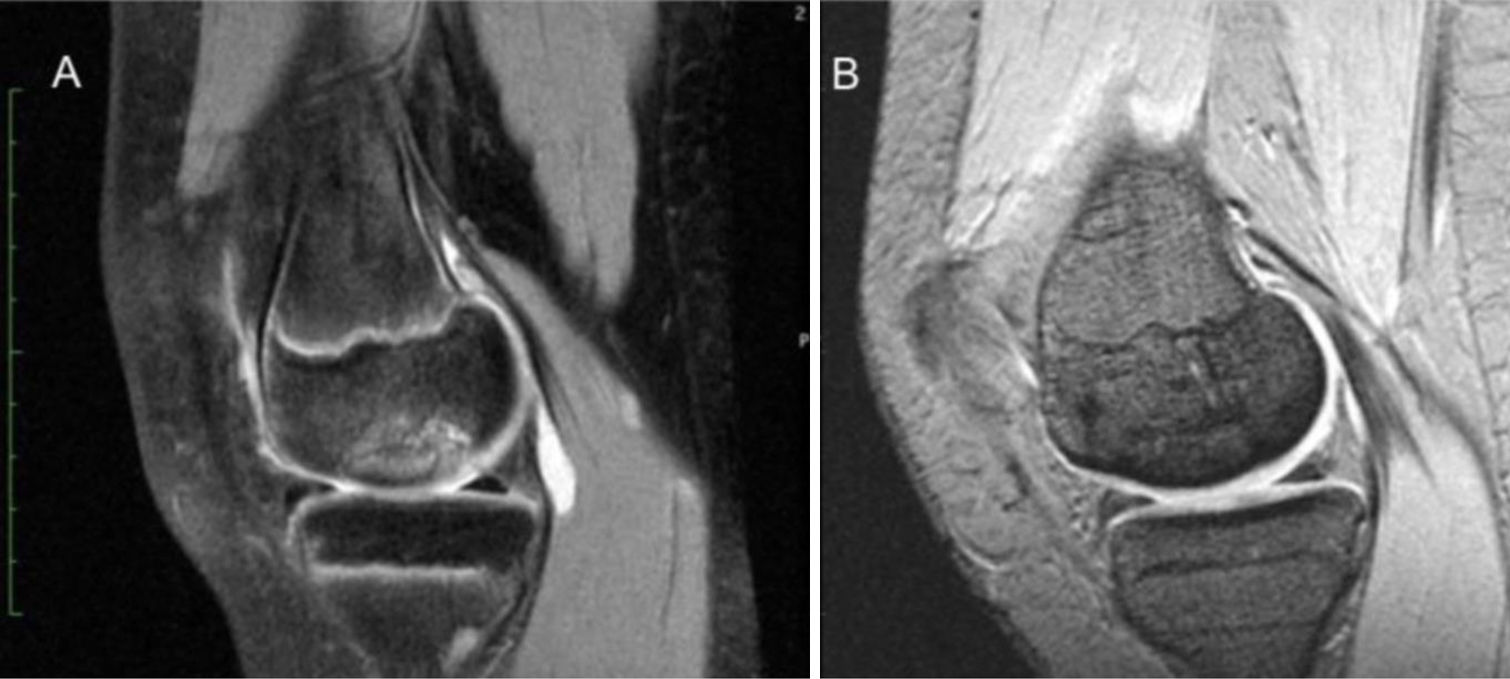
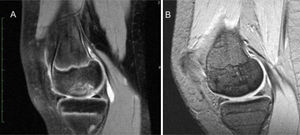
Follow-upThe patients were discharged within the first 24h, as this was an outpatient procedure, and they were kept non-weight bearing for a minimum of 4 weeks, immobilised with an extension orthosis. After 4 weeks, partial weight bearing with crutches was started and they were referred for rehabilitation to start kinesitherapy. Radiographic controls were carried out at 1, 3 and 6 months, and MRI control at 1year. In the post-surgical MRI, consolidation of the fragment was assessed through the following findings: absence of perilesional hyperintensity (T2) or presence of bone union bridging, absence of necrosis of the fragment (T1), associated or otherwise with fixation of same by the implant.6 The IKDC subjective knee form, post-surgical KOOS and Likert scale questionnaires were completed at one year.
Statistical analysisDescriptive analysis was performed using median and interquartile range (P25–P75 difference) for quantitative variables. The Wilcoxon signed-rank test was used to assess median differences in two paired assessments. The level of statistical significance was set at p<.05 in the different analyses.
ResultsA total of 9 patients (10 knees) were analysed, of which 5 were male (55%) and 4 female (45%), 50% of each if we analyse by individualising each intervention. Regarding laterality, 6 interventions were right (66%) and 4 left (34%). The median age was 15 years, 13 years (P25) and 22.75 years (P75). The median follow-up was 5.93 years, with a minimum follow-up of 12.5 months and a maximum of 11.5 years.
The location was the internal condyle in all 10 cases, 50% in the anterolateral and 50% in the posterolateral region. The median size of the major axis was 21.5mm and, the median was 15.25mm with respect to the minor axis, measured on pre-operative MRI on the axial-sagittal plane. We obtained 4 stage II cases (40%) compared to 6 stage III cases (60%) according to Dipaola's staging for MRI assessment. Analysing physeal closure on x-ray and MRI, we were able to differentiate 2 groups of osteochondritis: juvenile OCD (6 cases) and adult OCD (4 cases). Regarding associated lesions, 8 had no associated injury, one had an anterior tear of the external meniscus, and one had an injury to the posterior horn of the internal meniscus.
Stability was assessed and classified according to Ghul during surgery, 10 cases were classified as stage III. In 9 of the 10 operations, 2 implants were used: 2 cases (1.5mm [diameter]×25mm [length], 6 cases [2.4×25mm], 1 case [1.5×25mm–2.4×25mm]). In case number 3, 3 implants were required (2 implants of 2.4×25mm and 1 implant of 1.5×25mm). The median surgery time was 67.5min. No complications or reoperation were observed (Table 2).
Results.
| Age | Sex | Maturity | Location | Size of OCD (mm) | Dipaola et al.9 | Ghul et al10 | Postoperative MRI (1st year) | Complications | |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 13 | F | JOCD | CMp | 22.43×15.34 | II | III | C | N |
| Case 2 | 13 | M | JOCD | CMa | 14.3×7 | III | III | U | N |
| Case 3 | 37 | M | AOCD | CMp | 23.5×15.22 | III | III | U | N |
| Case4 | 12 | F | JOCD | CMp | 16.93×9.47 | II | III | U | N |
| Case 5a | 14 | F | JOCD | CMa | 18.03×6.81 | III | III | U | N |
| Case 6a | 15 | F | JOCD | CMp | 21.13×8.73 | III | III | IU | Delay in union |
| Case 7 | 15 | M | JOCD | CMa | 18.6×17.14 | III | III | U | N |
| Case 8 | 31 | M | AOCD | CMa | 21.2×13.3 | II | III | U | N |
| Case 9 | 17 | F | AOCD | CMa | 15.83×12.38 | III | III | U | N |
| Case 10 | 20 | M | AOCD | CMp | 14.01×12.11 | II | III | IU | Delay in union |
Case 1 had a synovial plica, not assessed by MRI, which was resected, and the lesion was left in situ with respect to the external meniscopathy. Patient 8 had an internal meniscopathy which required correction.
On the annual postoperative MRI, 8 patients had bone consolidation (we consider consolidation when there is no presence of fluid around the fragment, no signs of fragment necrosis, no oedema, and the presence of bone bridging) (Fig. 1) and only 2 patients (cases 6 and 10) had incomplete consolidation (perilesional oedema and fluid present around the fragment); as follow-up increased, both cases consolidated (15 months and 18 months).
In terms of degree of satisfaction, 9 of the 10 reported that they were very satisfied (Likert score 5), one patient (case 9) reported being satisfied (Likert score 4), with some discomfort.
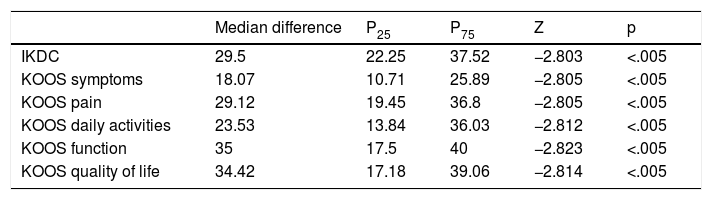
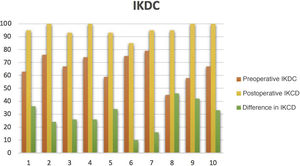
In terms of statistical analysis according to the Wilcoxon signed-rank test, statistical significance (p<.005) was observed for the before and after assessment on the IKDC and KOOS questionnaires, in favour of an improvement in these questionnaires. As for the IKDC questionnaire, subjective knee form, improvement was achieved with a median difference of 29.5 (22.25, 37.52) (Fig. 2). In the KOOS questionnaire, improvement was achieved in symptoms of 18.07 (10.71, 25.89), in pain 29.12 (19.45, 36.8), in activities of daily living 23.53 (13.84, 36.03), in function of 35 (17.5, 40), and in quality of life of 34.42 (17.18, 39.06) (Table 3).
Preoperative-postoperative difference in IKDC-KOOS questionnaires.
| Median difference | P25 | P75 | Z | p | |
|---|---|---|---|---|---|
| IKDC | 29.5 | 22.25 | 37.52 | −2.803 | <.005 |
| KOOS symptoms | 18.07 | 10.71 | 25.89 | −2.805 | <.005 |
| KOOS pain | 29.12 | 19.45 | 36.8 | −2.805 | <.005 |
| KOOS daily activities | 23.53 | 13.84 | 36.03 | −2.812 | <.005 |
| KOOS function | 35 | 17.5 | 40 | −2.823 | <.005 |
| KOOS quality of life | 34.42 | 17.18 | 39.06 | −2.814 | <.005 |
IKDC: International Knee Documentation Committee; KOOS: Knee Injury and Osteoarthritis Outcome Score.
Another point analysed was the comparison of KOOS and IKDC results in patients with JOCD versus adult osteochondritis dissecans (AOCD). Our study describes 6 cases of JOCD (60%) versus 4 cases of AOCD (40%). For the IKDC questionnaire, we obtained a median (P25, P75) pre/post-operative difference in JOCD of 25 (15.25, 34.87) and in ODCA of 37.55 (27.75, 47.27). Regarding the KOOS questionnaire for assessment of symptoms (14.5 [9.8, 26.1] in JOCD and 23.21 [13.39, 27.67] in AOCD), pain (26.34 [18, 33.33] in JOCD, 36.11 [17.36, 38.19] in AOCD), activities of daily living (25.53 in [13.84, 30.88], JOCD, 30.88 [8.08, 39.34 in AOCD]), function (30 [16.25, 42.5] in JOCD, 40 [17.5; 40] in AOCD), quality of life (28,12 [11,75, 39,06] in JOCD, 34,42 [31,27, 42,18 in AOCD]) (Fig. 3). Better clinical improvement is described in the AOCD cases.
DiscussionThe treatment of osteochondritis dissecans is still debated. Conservative treatment should always be chosen for injuries that are considered stable. Equally as important is to educate the patient to restrict sports activities, avoid jumping, pivoting and repetitive impact, and activities involving pain. There is ambiguity in the literature regarding the use of orthoses or immobilisers and they are usually reserved for non-compliant patients, since their effectiveness has not been proven.5 Our conservative treatment protocol consisted of non-weight bearing for 2–3 weeks, followed by physiotherapy (oedema control, gaining mobility, strength and proprioception) together with the restriction of high-risk sporting activities for a period of 3–6 months, considering the absence of pain or the presence of signs of re-ossification on imaging tests as union.3,4,6 If there was persistent pain after 6 months and/or the development of signs of instability on imaging tests, as described in the evaluation section, the surgical option was considered. In this regard, Krause et al.,4 analysed a cohort of 62 patients (72 stable JOCD lesions) at 6 and 12 months, with MRI control and under conservative treatment (activity restriction until pain improved). They observed a 26% success rate with conservative treatment at 6 months and 49% at 12 months. They described how age, size, area of lesion and cystlike lesion size were the best predictors of healing in the first 6 months, establishing a nomogram for the calculation of healing likelihood and a cut-off point of 48% for success of conservative treatment. In the 12-month period, cystlike lesion size <1.3mm was the only valid predictor of healing. Andriolo et al.5 conducted a systematic review on the conservative treatment of knee OCD, and found only published case series and clinical cases. The conservative treatments described were physical activity restriction, kinesitherapy, instrumental physical therapies (shockwave, iontophoresis), restricted weightbearing and immobilisation, with restriction of sport and high intensity activities, together with physiotherapy as the best conservative treatment. The overall healing rate was 61.4% (variability 10.4%–95.8%).
Two subtypes of osteochondritis dissecans are described depending on the state of the physis, juvenile (JOCD) and adult (AOCD). Some studies have argued that it is the same disease at different stages of progression.3 In cases with closure of the physis (AOCD), the treatment differs in some aspects. They present more unstable lesions initially, with a lower rate of union, and require internal fixation or reconstructive techniques more frequently.13 There is no literature available in unstable lesions that analyses conservative treatment as the first line of treatment in this type of injury. In our series, unstable injuries occurred in 2 knees with closed physes and 4 with open physes.
If conservative treatment fails, surgery is described as the next step. We observed that 4 patients considered for conservative treatment failed this therapeutic modality, surgical treatment was decided in the end. Ishikawa et al.,14 analysed in situ fixation of arthroscopically stable lesions (Ghul I-II), observing a failure rate of 23% (3/13), which corresponded to unstable lesions on MRI (Dipaola) and concluded the importance of not underestimating the potential instability of the lesion on imaging tests.
Surgical treatment in OCD is considered for stable lesions that fail to respond to conservative treatment and for unstable lesions. The therapeutic arsenal includes drilling (retrograde, antegrade), internal fixation (screws, bioabsorbable implants), reconstructive procedures and regenerative cell therapy. Stable JOCD lesions that have failed after conservative treatment can be treated by transarticular or retroarticular drilling.15 However, stability must be assessed intraoperatively, as has been proven in this study, 4 cases were stable on imaging and unstable intraoperatively. Sanders et al.16 observed that the cumulative incidence of osteoarthritis and the incidence of arthroplasty was higher with fragment excision than with fixation or osteochondral grafting, and therefore they advise treating the osteochondral fragment or the defect.
Our series achieved 80% union in the first year, with 2 cases of delayed union treated by restricting physical activity that achieved complete union at 15 and 18 months, respectively. No reoperation was necessary. Perrelli et al.6 analysed 39 AOCD interventions with different implants, 51.2% with Herbert screws, 23.1% with cannulated screws and 25.7% with bioabsorbable nails. They found no functional or union differences between the different implants, although the non-bioresorbable nails required a second-look arthroscopy for removal (74.3%). They had a failure rate of 20.5% with 4 re-interventions and 4 with low scores. They described 40.8% alteration on postoperative MRI, of which 17.9% had incomplete consolidation, and 7.6% absence of consolidation at 1year, inter alia. They observed a statistical correlation between MRI alteration and low scores in the functional tests. In our case, the lowest postoperative subjective IKDC score was in case 6 at 85, which showed incomplete union on the annual MRI. However, they made no comparison groups according to physeal closure. Schlechter et al.7 analysed a cohort of JOCDs operated with bioabsorbable implants, presenting only one failure out of 38, directly related to the surgery (slightly protruding screw). Complete consolidation of the fragment was observed at 10 months. Wu et al.17 compared internal fixation in unstable OCD according to physeal closure (JOCD/AOCD), concluding that there were no differences. They achieved a success rate of 70.4% in JOCD and 78.3% in AOCD, with no differences in 5-year survival curves. No differences were observed in our study either.
Surgical joint preservation procedures are reserved for situations when the fragment cannot be synthesized, it is comminuted or there is major cartilage deterioration. They are also reserved should any of the abovementioned techniques fail. These procedures include chondrectomy with nanofracture, mosaicplasty/OAT (osteochondral autograft transplant), hybrid, allograft, and cell repair therapy with cultured autologous chondrocytes plus bone graft (autologous chondrocyte implantation, or matrix assisted autologous chondrocyte transplantation) or acellular biomimetic scaffolds. There is little evidence for chondrectomy and nanofractures in OCDs of a smaller size (<2.5cm2), due to the poor mechanical quality of fibrocartilage and limitations in terms of the lesion defect.15 Gudas et al.18 conducted a prospective randomised study comparing OAT with microfracture, showing a 41% failure rate in the microfracture group versus 0% in the OAT group. Miniaci and Tytherleigh19 evaluated fixation of unstable OCD by mosaicplasty over the lesion, with excellent results. Chadli et al.20 proposed hybrid techniques of mosaicplasty associated with fixation of the fragment with metal screws, obtaining good long-term results and without degenerative changes. However, Filardo et al.15 conducted a systematic review of OCD, observing limitations of OAT with respect to defect size, donor site, fibrocartilage formed at the periphery, technical demand, higher cost, and less anatomical reconstruction.
For larger lesions, fresh osteocondral allograft15,21,22 has been described as an alternative without size limitation, especially in bone defects of AOCD> 2m2. Cotter et al.21 reported a 35.9% reoperation rate and a 5.1% final failure rate after 7 years of follow-up. Sadr et al.22 reported a 23% reoperation rate and an 8% failure rate, with a 95% satisfaction rate. However, the limitations of this technique are tissue availability (access to healthy donors, preservation and asepsis of the allograft, chondrocyte viability, immunological status), high cost and technical difficulty, among others.
Autologous chondrocyte implantation is a procedure to regenerate the joint surface and involves two interventions, harvesting and culture and then implantation. This technique has achieved good results in the treatment of articular cartilage defects, although OCD also involves subchondral bone. Therefore, procedures have been described that use cancellous autograft to fill the defect, and chondrocytes protected by periosteal coverings or porcine collagen membrane are implanted on the defect.23 Bhattacharjee et al.24 histologically analysed 17 OCD treated with bone graft+ACI showing cartilage repair at the histological level, although with abnormalities at the subchondral bone level (cysts) in 90% of the MRI. However, hypertrophy and periosteal delamination required revision surgery, among other problems such as inhomogeneous distribution of chondrocytes or cell loss in liquid suspension. As a result, matrix assisted autologous chondrocyte transplantation techniques have emerged for the protection and support of chondrocytes.15 However, these procedures are high cost and not free from complications (graft hypertrophy). Sadlik et al.25 have proposed using bone marrow aspirate concentrate in a hyaluronic acid-based scaffold together with autologous bone drafting to treat these defects in one step. Some recent studies have even proposed the use of three-dimensional structures composed of cell-free collagen I and hydroxyapatite26,27 or allogeneic umbilical cord blood-derived mesenchymal stem cells28 to avoid a two-step technique, facilitate the surgical technique and reduce costs. The patients who underwent surgery in our study did not present large osteochondral lesions or comminution of the fragment due to the speed of diagnosis and treatment, among other reasons, and therefore this type of procedure was not necessary.
A limitation of this study was its small sample (n=10), which made it necessary to use non-parametric tests (Wilcoxon, Mann–Whitney U), comparing medians and working on order ranges. There is also no control group with unstable lesions treated conservatively. All this implies a lower statistical power, although not a lower clinical power. With respect to the International Cartilage Repair Society classification, although it is currently the most widely used classification, this study was started using the Ghul and Dipaola staging, therefore we decided to maintain these classifications to avoid bias.
To conclude, the bioabsorbable implant is a valid, reproducible option for unstable lesions with lesion integrity, with great improvement in function, quality of life and few complications.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Bogallo JM, Godino Izquierdo M, Dalla-Rosa J, Ramos González L, Arjona Diaz M, Guerado E. Osteocondritis disecante inestable de rodilla: fijación artroscópica con implante bioabsorbible. Rev Esp Cir Ortop Traumatol. 2021;65:407–415.