To analyse the current scientific and/or clinical evidence supporting the use of platelet-rich plasma (PRP) in the treatment of rotator cuff pathology.
MethodsAfter a systematic review in PubMed, studies assessing PRP efficacy in the treatment of rotator cuff pathology published since 2013 to date were identified. Data were grouped based on type of study (laboratory, clinical or meta-analysis); accordingly study design, pathology treated and clinical outcomes were summarised.
ResultsThirty-five articles have been analysed: 10 laboratory studies, 17 clinical assays and 8 meta-analyses. While laboratory studies report positive or partially positive results for the use of PRP, 70.6% of clinical studies and 75% of meta-analysis found no statistically significant differences between the PRP group and the control group.
DiscussionThe positive results of laboratory studies do not translate well to clinical practice. There is no concordance among the few positive results reported in the clinical studies, and even some contradictory effects have been reported.
ConclusionsThere is no solid scientific and/or clinical evidence supporting the use of PRP in the treatment of rotator cuff pathology in routine clinical practice.
Obtener una visión objetiva de las evidencias científicas y/o clínicas actuales sobre el uso de plasma rico en plaquetas (PRP) en el tratamiento de la patología del manguito de los rotadores.
MétodoRevisión sistemática en Pubmed e identificación de estudios que evalúen la eficacia de PRP en el tratamiento de la patología del manguito de los rotadores desde 2013 hasta la actualidad. Los datos se agrupan según el tipo de estudio (laboratorio, clínico o metaanálisis); se obtienen datos sobre el diseño del estudio, la patología tratada y los resultados clínicos.
ResultadosSe han analizado 35 artículos: 10 estudios de laboratorio, 17 estudios clínicos y 8 metaanálisis. Mientras que los estudios de laboratorio observan resultados positivos o parcialmente positivos para el uso de PRP, el 70,6% de los estudios clínicos y el 75% de los metaanálisis no encuentran diferencias estadísticamente significativas entre el grupo con PRP y el grupo control.
DiscusiónLos resultados positivos de los estudios de laboratorio tienen una baja traslación a los estudios clínicos. No hay concordancia entre los escasos resultados positivos observados en los diferentes estudios clínicos, habiéndose observado incluso resultados contradictorios.
ConclusionesNo existen evidencias científicas y/o clínicas sólidas para el uso de PRP en el tratamiento de la patología del manguito de los rotadores en la práctica clínica habitual.
Pain and functional impotence of the shoulder are very common symptoms (between 4% and 26% of the general population suffer from this)1,2 and are a diagnostic challenge since they may present for many reasons. Rotator cuff injuries are among the causes of these symptoms.3 The rotator cuff injury or tear is a common pathology which increases with age4 and with overuse of the shoulder.5
The treatment of these injuries is initially symptomatic and rehabilitating. When conservative treatment fails, rotator cuff injuries must be treated surgically with tendon repair.4 Several open surgery techniques have been described for the repair of the rotator cuff, using mini-approach and arthroscopic techniques. Many studies have been conducted to evaluate which offers greater resistance or the best outcome.4,6
Over the last few years new adjuvant treatments have been evaluated which may help with cures and wound healing of the rotator cuff in attachment with the bone and which reduce the rate of re-tears.7–9 Several products are under study: morphogenetic proteins (BMP), osteoprotegerins, mesenchymal cells, different animal or human cell matrices, etc.7,10–12 The most abundant studies are the ones which try to assess the efficacy of platelet-rich plasma (PRP) or fibrin-rich plasma (PRF) in the cure of rotator cuffs. Particular study is being made of the possible benefit its application could have in the arthroscopic suturing of the rotator cuff.8,9 The platelets are a source of growth factors which are capable of stimulating cellular proliferation and providing a temporary matrix that may fill the defect and serve as a matrix for cellular migration and tissue remodelling. As a result, the PRP may have, at least theoretically, great potential for helping tissue repair.9,12,13
The aim of this study was to obtain a complete vision of scientific and/or clinical evidence offered by the current literature on the use of PRP in the treatment of the rotator cuff pathology and to assess whether its use is justified in standard clinical practice.
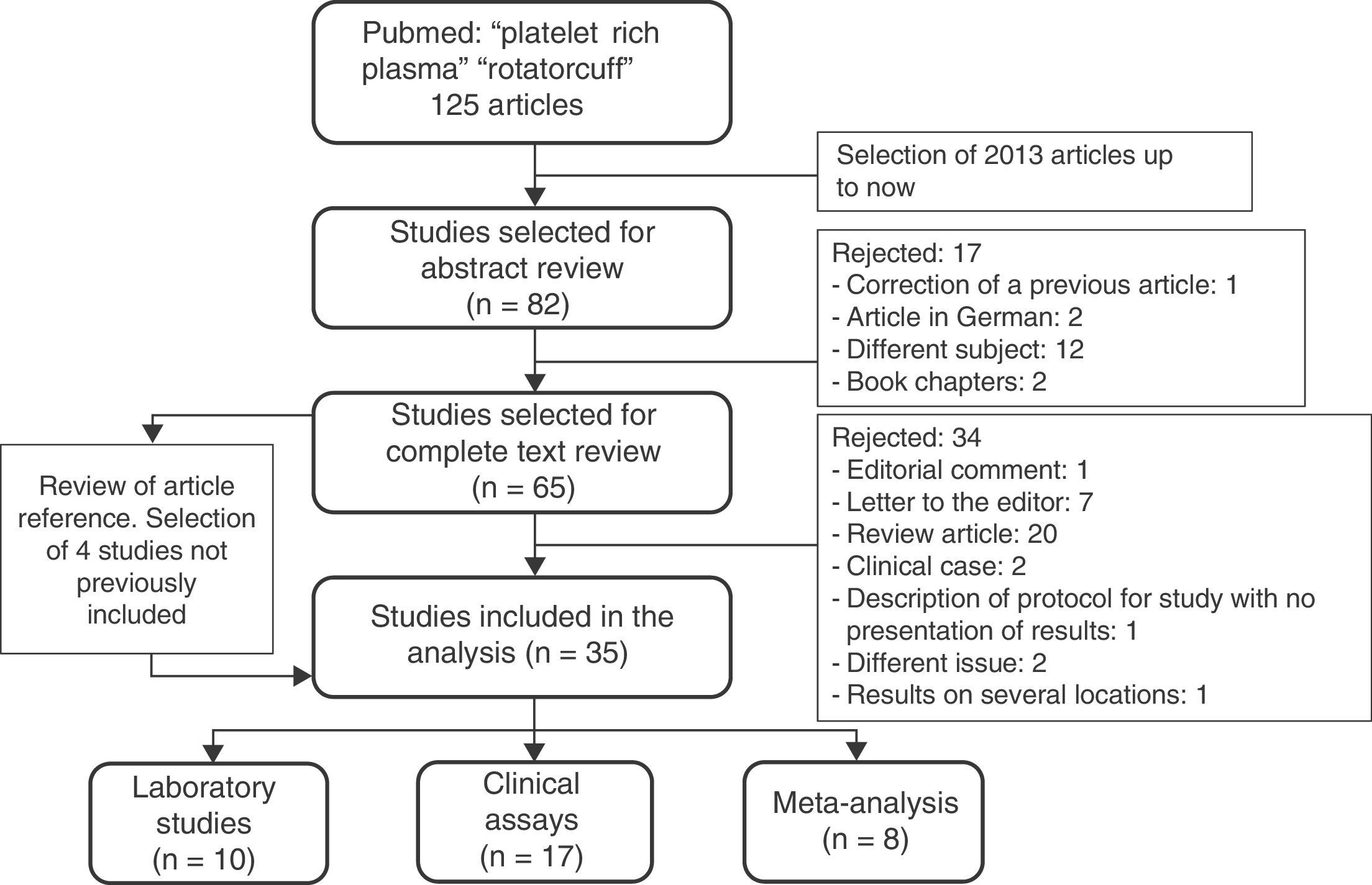
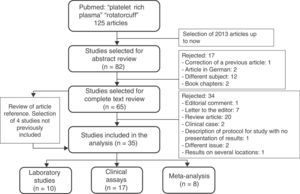
MethodsA systematic review of useful studies was made on the treatment of the rotator cuff pathology with PRP. On 18th January 2016 a search in Pubmed was made with the combination of the terms platelet rich plasma and rotator cuff. The articles published from 2013 until the present day were selected. A cross-check was also made of the references of this article (Fig. 1).
The analysis also included studies published in Spanish or English, with a scientific level of evidence from I to IV, which assessed some aspect of the treatment of rotator cuffs with PRP (alone or combined with other treatments). The review of the letters to the editor was excluded, as were editorial comments, review articles, clinical cases and chapters from book. Studies which did not present outcome or which presented outcome combined with the application of PRP on several locations (lateral epicondyl, patellar tendon, etc.) (Fig. 1) were also included.
To carry out analysis the studies were grouped according to types: (1) laboratory study, (2) clinical study (clinical assay, cohort study or case series) or (3) meta-analysis. Data relating to the publication was obtained (journal and impact factor about the same according to the Journal Citation Report – JCR-2014) and scientific level of evidence, study design, aspect of the rotator cuff pathology studied, where, how and when the PRP was administered and whether if was combined or not with other treatments, the number of patients (and of studies, in the case of meta-analysis) included, the systems of measuring the outcome, the follow-up time and the study conclusions.
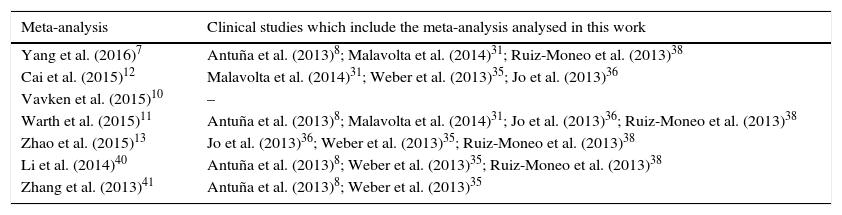
Several reviewed clinical studies in this work are included in the meta-analysis studied. Although there is no bias, because a new statistical analysis of findings is not being made, this should be taken into account in its interpretation, since several findings are repeated.
ResultsAfter the search for studies and the analysis of their content, a total of 35 articles, 10 laboratory studies, 17 clinical assays and 8 meta-analyses were selected (Fig. 1).
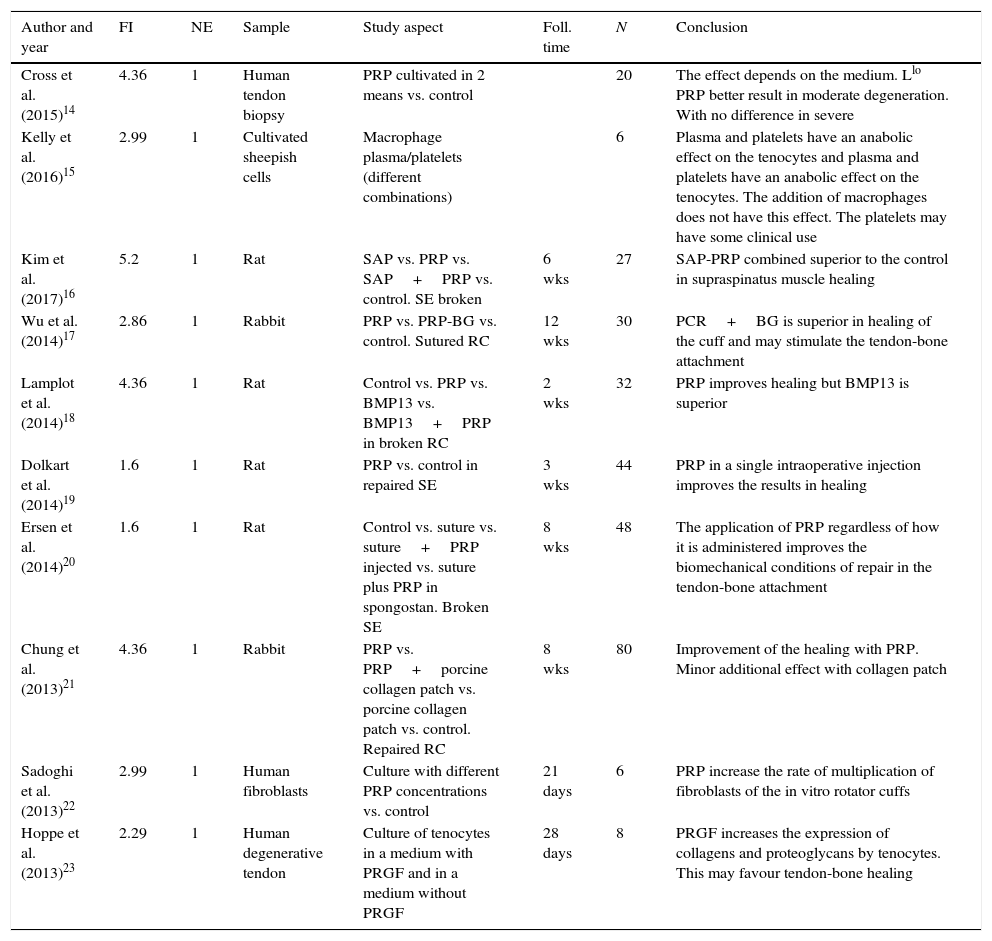
Laboratory (Table 1)14–23Table 1 includes 10 reviewed articles which present the results of PRP usage in different laboratory situations. The 10 studies have a scientific evidence level of 1 and were published in journals included in the 2014 JCR. The mean impact factor of the journals in which these articles were published is 3.26 (range between 1.6 and 5.2). In three studies cells were used which were obtained from human tendons and in the other cells from sheep were used. In the remaining six studies an animal model of the rotator cuff was used (four from rat and two from rabbit). These studies used a mean of 30 individuals (range from 6 to 80) with a mean follow-up time of 5.75 weeks (range from 2 to 12). 100% of the studies which used the torn rotator cuff model concluded that the PRP (or the PRP linked to another substance) improved the healing of the rotator cuff. The four studies which presented results from the application of PRP on cells obtained by biopsy also showed positive or partially positive results.
Laboratory studies.
| Author and year | FI | NE | Sample | Study aspect | Foll. time | N | Conclusion |
|---|---|---|---|---|---|---|---|
| Cross et al. (2015)14 | 4.36 | 1 | Human tendon biopsy | PRP cultivated in 2 means vs. control | 20 | The effect depends on the medium. Llo PRP better result in moderate degeneration. With no difference in severe | |
| Kelly et al. (2016)15 | 2.99 | 1 | Cultivated sheepish cells | Macrophage plasma/platelets (different combinations) | 6 | Plasma and platelets have an anabolic effect on the tenocytes and plasma and platelets have an anabolic effect on the tenocytes. The addition of macrophages does not have this effect. The platelets may have some clinical use | |
| Kim et al. (2017)16 | 5.2 | 1 | Rat | SAP vs. PRP vs. SAP+PRP vs. control. SE broken | 6 wks | 27 | SAP-PRP combined superior to the control in supraspinatus muscle healing |
| Wu et al. (2014)17 | 2.86 | 1 | Rabbit | PRP vs. PRP-BG vs. control. Sutured RC | 12 wks | 30 | PCR+BG is superior in healing of the cuff and may stimulate the tendon-bone attachment |
| Lamplot et al. (2014)18 | 4.36 | 1 | Rat | Control vs. PRP vs. BMP13 vs. BMP13+PRP in broken RC | 2 wks | 32 | PRP improves healing but BMP13 is superior |
| Dolkart et al. (2014)19 | 1.6 | 1 | Rat | PRP vs. control in repaired SE | 3 wks | 44 | PRP in a single intraoperative injection improves the results in healing |
| Ersen et al. (2014)20 | 1.6 | 1 | Rat | Control vs. suture vs. suture+PRP injected vs. suture plus PRP in spongostan. Broken SE | 8 wks | 48 | The application of PRP regardless of how it is administered improves the biomechanical conditions of repair in the tendon-bone attachment |
| Chung et al. (2013)21 | 4.36 | 1 | Rabbit | PRP vs. PRP+porcine collagen patch vs. porcine collagen patch vs. control. Repaired RC | 8 wks | 80 | Improvement of the healing with PRP. Minor additional effect with collagen patch |
| Sadoghi et al. (2013)22 | 2.99 | 1 | Human fibroblasts | Culture with different PRP concentrations vs. control | 21 days | 6 | PRP increase the rate of multiplication of fibroblasts of the in vitro rotator cuffs |
| Hoppe et al. (2013)23 | 2.29 | 1 | Human degenerative tendon | Culture of tenocytes in a medium with PRGF and in a medium without PRGF | 28 days | 8 | PRGF increases the expression of collagens and proteoglycans by tenocytes. This may favour tendon-bone healing |
BG: bioactive glass; BMP-13: bone morphogenetic protein-13; IF: impact factor; Llo PRP: platelet-rich plasma prepared with the commercial system Arthrex Autologous Conditioned Plasma Double Syringe System; RC: rotator cuff; N: number of individuals; LE: level of scientific evidence; PRGF: platelet-released growth factors; PRP: platelet-rich plasma; SAP: self-assembled peptide; SE: supraspinatus; foll.: follow-up; wks: weeks.
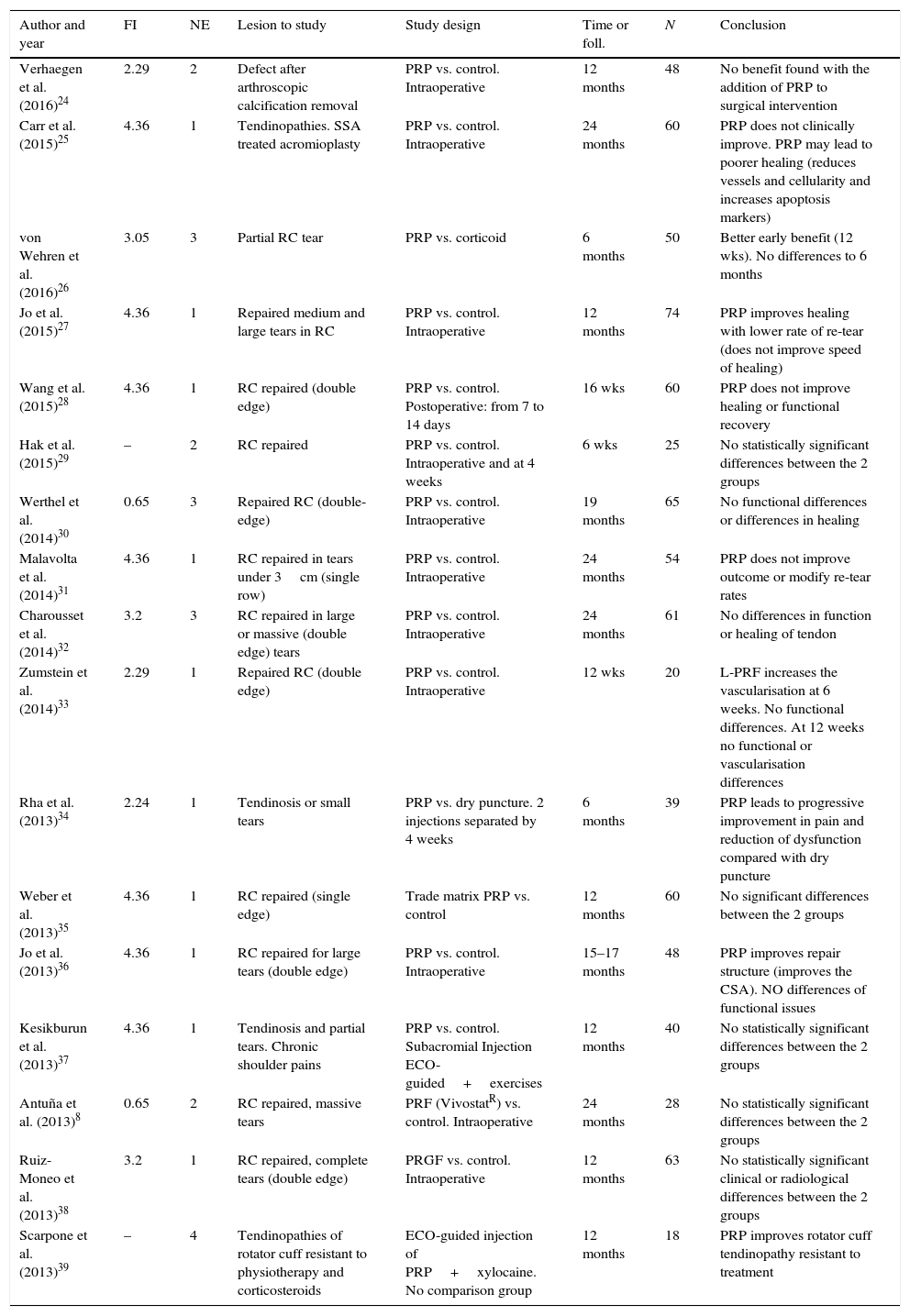
17 clinical assays with patients were included in analysis, 16 of which presented the results of PRP used in comparison with a control group, and one of the studies39 presented a case series. Ten studies had a scientific evidence level of 1, three had level 2, another three level 3 and the remaining one had a scientific evidence level of 4. 88% of these clinical assays were published in journals included in the 2014 JCR. The mean impact factor of the journals in which these articles were published was 2.83 (range between 0 and 4.36). Eleven assays presented comparison of the use of PRP compared with a control group in repaired rotator cuffs (in ten studies this was applied intraoperatively and in the other,28 with two postoperative applications). Another study24 used intraoperative PRP for the healing of the cuff, after removal of a calcification without doing any repair. One article25 compared the use or non-use of intraoperative PRP in the case of tendinosis produced by an impingement syndrome treated with arthroscopic acromioplasty without touching the cuff. The other four studies report the application of PRP in patients with tendinosis or partial fractures on which no surgical intervention has ever been performed. These studies included a mean of 48 individuals (range between 18 and 74), which total 795 patients, with a mean follow-up time of the patients of 13.15 months (range between 1.5 and 24). In twelve (70.6%) studies no statistically significant differences were found between the group of patients treated with PRP and the control group, and Carr et al.25 even concluded in their study that the use of PRP may lead to poorer healing (reducing blood vessels and cellularity and increasing apoptosis markers). Two of the comparative studies found a better result in the group of patients treated with PRP compared with the control group (one in repaired cuff27 and the other in cuff tendinosis that had not had surgery performed on it34). The work which presented a case series without a control group also presented good results.39 Two articles had partial positive results (in the short term or in repair structure), but no differences in the final outcome26,36 (Table 2).
Clinical studies.
| Author and year | FI | NE | Lesion to study | Study design | Time or foll. | N | Conclusion |
|---|---|---|---|---|---|---|---|
| Verhaegen et al. (2016)24 | 2.29 | 2 | Defect after arthroscopic calcification removal | PRP vs. control. Intraoperative | 12 months | 48 | No benefit found with the addition of PRP to surgical intervention |
| Carr et al. (2015)25 | 4.36 | 1 | Tendinopathies. SSA treated acromioplasty | PRP vs. control. Intraoperative | 24 months | 60 | PRP does not clinically improve. PRP may lead to poorer healing (reduces vessels and cellularity and increases apoptosis markers) |
| von Wehren et al. (2016)26 | 3.05 | 3 | Partial RC tear | PRP vs. corticoid | 6 months | 50 | Better early benefit (12 wks). No differences to 6 months |
| Jo et al. (2015)27 | 4.36 | 1 | Repaired medium and large tears in RC | PRP vs. control. Intraoperative | 12 months | 74 | PRP improves healing with lower rate of re-tear (does not improve speed of healing) |
| Wang et al. (2015)28 | 4.36 | 1 | RC repaired (double edge) | PRP vs. control. Postoperative: from 7 to 14 days | 16 wks | 60 | PRP does not improve healing or functional recovery |
| Hak et al. (2015)29 | – | 2 | RC repaired | PRP vs. control. Intraoperative and at 4 weeks | 6 wks | 25 | No statistically significant differences between the 2 groups |
| Werthel et al. (2014)30 | 0.65 | 3 | Repaired RC (double-edge) | PRP vs. control. Intraoperative | 19 months | 65 | No functional differences or differences in healing |
| Malavolta et al. (2014)31 | 4.36 | 1 | RC repaired in tears under 3cm (single row) | PRP vs. control. Intraoperative | 24 months | 54 | PRP does not improve outcome or modify re-tear rates |
| Charousset et al. (2014)32 | 3.2 | 3 | RC repaired in large or massive (double edge) tears | PRP vs. control. Intraoperative | 24 months | 61 | No differences in function or healing of tendon |
| Zumstein et al. (2014)33 | 2.29 | 1 | Repaired RC (double edge) | PRP vs. control. Intraoperative | 12 wks | 20 | L-PRF increases the vascularisation at 6 weeks. No functional differences. At 12 weeks no functional or vascularisation differences |
| Rha et al. (2013)34 | 2.24 | 1 | Tendinosis or small tears | PRP vs. dry puncture. 2 injections separated by 4 weeks | 6 months | 39 | PRP leads to progressive improvement in pain and reduction of dysfunction compared with dry puncture |
| Weber et al. (2013)35 | 4.36 | 1 | RC repaired (single edge) | Trade matrix PRP vs. control | 12 months | 60 | No significant differences between the 2 groups |
| Jo et al. (2013)36 | 4.36 | 1 | RC repaired for large tears (double edge) | PRP vs. control. Intraoperative | 15–17 months | 48 | PRP improves repair structure (improves the CSA). NO differences of functional issues |
| Kesikburun et al. (2013)37 | 4.36 | 1 | Tendinosis and partial tears. Chronic shoulder pains | PRP vs. control. Subacromial Injection ECO-guided+exercises | 12 months | 40 | No statistically significant differences between the 2 groups |
| Antuña et al. (2013)8 | 0.65 | 2 | RC repaired, massive tears | PRF (VivostatR) vs. control. Intraoperative | 24 months | 28 | No statistically significant differences between the 2 groups |
| Ruiz-Moneo et al. (2013)38 | 3.2 | 1 | RC repaired, complete tears (double edge) | PRGF vs. control. Intraoperative | 12 months | 63 | No statistically significant clinical or radiological differences between the 2 groups |
| Scarpone et al. (2013)39 | – | 4 | Tendinopathies of rotator cuff resistant to physiotherapy and corticosteroids | ECO-guided injection of PRP+xylocaine. No comparison group | 12 months | 18 | PRP improves rotator cuff tendinopathy resistant to treatment |
IF: impact factor; L-PRF: leucocyte- and platelet-rich fibrin; RC: rotator cuff; N: number of patients; LE: level of scientific evidence; PRF: Platelet Rich Fibrin; PRP: platelet-rich plasma; SAS: subacromial syndrome; foll.: follow-up; wks: weeks.
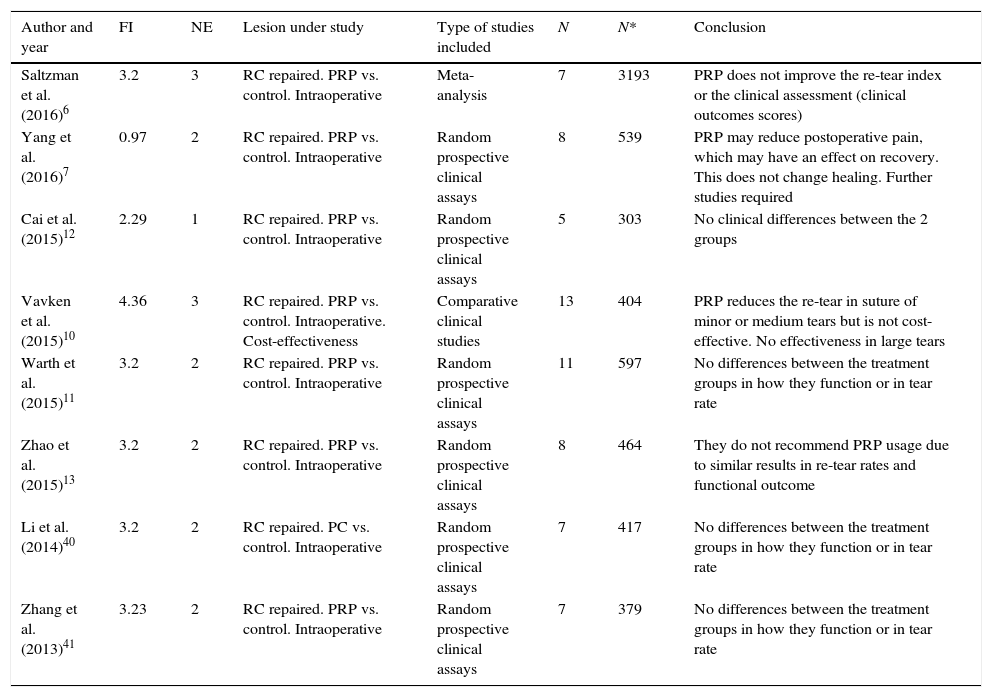
Table 3 contains eight meta-analyses and in all of them the results of the use of PRP are compared with a control group. Some of the clinical studies reviewed in this work in the previous paragraph are included in these meta-analyses (Table 4). Six of the studies have a scientific evidence level of 1 or 2, and the other two have a level of 3. All these meta-analyses are published in journals included in the 2014 JCR. The mean impact factor of the journals in which these articles were published is 2.96 (range between 0.97 and 4.36). All the studies present a comparison of the use of PRP compared with control in repaired rotator cuffs. A mean of 8.25 studies are included in each meta-analyses (range between 5 and 13), with a mean of 787 patients (range between 303 and 3193). Out of the eight meta-analyses, there were no statistical significances between the group of patients treated with PRP and the control group. The other two studies presented partial positive results (with regard to pain or the rate of small or medium tears in re-tears). There is only one article which includes a financial study and concludes that despite small or medium tears, the results with PRP are superior to the control, its application is not cost-effective and in large tears there is no difference between the groups with PRP and the control group.10
Meta-analysis.
| Author and year | FI | NE | Lesion under study | Type of studies included | N | N* | Conclusion |
|---|---|---|---|---|---|---|---|
| Saltzman et al. (2016)6 | 3.2 | 3 | RC repaired. PRP vs. control. Intraoperative | Meta-analysis | 7 | 3193 | PRP does not improve the re-tear index or the clinical assessment (clinical outcomes scores) |
| Yang et al. (2016)7 | 0.97 | 2 | RC repaired. PRP vs. control. Intraoperative | Random prospective clinical assays | 8 | 539 | PRP may reduce postoperative pain, which may have an effect on recovery. This does not change healing. Further studies required |
| Cai et al. (2015)12 | 2.29 | 1 | RC repaired. PRP vs. control. Intraoperative | Random prospective clinical assays | 5 | 303 | No clinical differences between the 2 groups |
| Vavken et al. (2015)10 | 4.36 | 3 | RC repaired. PRP vs. control. Intraoperative. Cost-effectiveness | Comparative clinical studies | 13 | 404 | PRP reduces the re-tear in suture of minor or medium tears but is not cost-effective. No effectiveness in large tears |
| Warth et al. (2015)11 | 3.2 | 2 | RC repaired. PRP vs. control. Intraoperative | Random prospective clinical assays | 11 | 597 | No differences between the treatment groups in how they function or in tear rate |
| Zhao et al. (2015)13 | 3.2 | 2 | RC repaired. PRP vs. control. Intraoperative | Random prospective clinical assays | 8 | 464 | They do not recommend PRP usage due to similar results in re-tear rates and functional outcome |
| Li et al. (2014)40 | 3.2 | 2 | RC repaired. PC vs. control. Intraoperative | Random prospective clinical assays | 7 | 417 | No differences between the treatment groups in how they function or in tear rate |
| Zhang et al. (2013)41 | 3.23 | 2 | RC repaired. PRP vs. control. Intraoperative | Random prospective clinical assays | 7 | 379 | No differences between the treatment groups in how they function or in tear rate |
IF: impact factor; RC: rotator cuff; N: number of studies included; N*: total number of patients; LE: level of scientific evidence; PC: platelet concentrates; PRP: platelet-rich plasma.
Clinical studies included in reviewed meta-analysis.
| Meta-analysis | Clinical studies which include the meta-analysis analysed in this work |
|---|---|
| Yang et al. (2016)7 | Antuña et al. (2013)8; Malavolta et al. (2014)31; Ruiz-Moneo et al. (2013)38 |
| Cai et al. (2015)12 | Malavolta et al. (2014)31; Weber et al. (2013)35; Jo et al. (2013)36 |
| Vavken et al. (2015)10 | – |
| Warth et al. (2015)11 | Antuña et al. (2013)8; Malavolta et al. (2014)31; Jo et al. (2013)36; Ruiz-Moneo et al. (2013)38 |
| Zhao et al. (2015)13 | Jo et al. (2013)36; Weber et al. (2013)35; Ruiz-Moneo et al. (2013)38 |
| Li et al. (2014)40 | Antuña et al. (2013)8; Weber et al. (2013)35; Ruiz-Moneo et al. (2013)38 |
| Zhang et al. (2013)41 | Antuña et al. (2013)8; Weber et al. (2013)35 |
Of the 25 studies which present patient results (17 clinical studies – Table 2 – and 8 meta-analyses – Table 3), 19 present comparative results of the application of PRP compared with a control group in rotator cuffs repaired arthroscopically (11 of the 17 clinical studies and 8 meta-analyses). 79% of the studies offered no statistically significant differences between the 2 groups. Only one work found that in the group in which PRP was applied there was better wound healing and a lower rate or re-tear (in large or medium tears).27 Another three studies found partial positive results with the application of PRP: one showed a lower rate of re-tear in small or medium tears (noting large ones)10; another indicated that in the PRP group there was less postoperative pain (although it concluded that further studies were required)7 and a third concluded that in the PRP group there was a better repair structure, although no differences were found with regard to function.36
DiscussionThe use of platelet rich plasma in the pathology of rotator cuffs is a relevant topical issue as is demonstrated in the 35 original articles published on this subject from 2013 to 18th January 2016 (in journals indexed in Pubmed). If the studies which were rejected for this systematic review (Fig. 1) were analysed 20 reviews would be found that were published in this respect about this issue during the same period, one editorial and 7 letters to the editor. Apart from indicating that this is a very up to date subject, this indicates that there is a high level of contrasting opinions.42,43 There is a particular interest in promoting the use of PRP in rotator cuffs which have been torn and repaired, and 19 studies have been published on this matter, which comprises 76% of the clinical studies.
PRP has had very good results in the laboratory studies, but these results drastically worsen when there is an attempt to remove its use to clinical practice. PRP has widely demonstrated in vitro studies that it has an anabolic effect and that it leads to an increase in cellular multiplication and in the expression of collagen and proteoglycans by tenocytes.15,22,23 PRP has also clearly demonstrated its superiority with regard to the control group in the models of rotator cuff tears in animals (both if the tear was repaired and if it was not). The majority of these studies presented biomechanical and histological studies which support their conclusions.16–21 There are several reasons which could explain why the results obtained in these laboratory studies are not taking into consideration a correlation in the clinical studies. Firstly, in the animal models, young healthy individuals were used (and therefore with good quality tendon tissue) on which a controlled tendon tear was practiced (the same for all subjects) and immediately afterwards suture and/or the administration of PRP was given. In contrast, patients who suffer from rotator cuff tears are greatly heterogeneous in tears. They are usually individuals who get a tear in degenerated tendons or previously impaired tendons and also repair and/or the administration of PRP is not always administered at the time of tearing, but several weeks or months may pass before treatment is administered. Secondly, it must be borne in mind that the laboratory studies are performed with a mean follow-up time of 5.75 weeks, much less (over 9 times less) than that of the clinical studies (13.15 months). This could indicate that the PRP may have a positive effect during the initial weeks, but that this effect is lost, or at least the result is the same with the passing of time, as several of the reviewed clinical studies suggest.26 In several laboratory studies, other substances have been linked with PRP to enhance its action: bioactive glass (BG),17bone morphogenetic protein-13 (BMP-13),18self-assembled peptide (SAP),16 spongostan20 and collagen swine patch.21 There are 6 laboratory studies with 5 different adjuvant studies (one without adjuvant) and also that neither of the reviewed clinical studies use any of these adjuvant studies. It is not possible to establish which of them is better or which could have a good outcome in clinical studies. Only one of the PRP preparations used in one of these laboratory studies20 has also been used in some of the analysed clinical studies,24,32,37 obtaining good results in the laboratory study20 and with no differences in the clinical studies.24,32,37 Lastly, the majority of the laboratory studies which present positive results on tears, carry out histological tests and biomechanical tests on the specimens after the animal has been sacrificed,16–21 whilst the results of clinical suites are based mainly on physical exploration, functional tests or imaging tests (in the majority of cases, magnetic resonance). It would appear that the histology and ex vivo biomechanical tests have little in common with the real functioning of the shoulder. To make a suitable comparison, the workability of the shoulder should be measured prior to sacrificing the animals or prior to carrying out histological analysis in humans with a repaired rotator cuff (which may be difficult and prone to ethical conflicts in clinical practice, since performing a biopsy is an invasive diagnostic test and may lead to complications).
In studies in human in vivo which compare the use of PRP with a control group, 75% conclude that they do not find any statistically significant differences between the 2 groups and this increases up to 79% if we analyse only the studies which present results in repaired rotator cuffs.6–8,10–13,27–33,35,36,38,40,41 Several authors find positive results or partially positive results in some aspects or some type of specific lesions: better repair structure,36 less postoperative pain,7 lower rate of re-tears in small or mediums sized tears,10 better wound healing and a lower rate of re-tears in large or medium sized tears.27 It should be noted that these positive results are not constant in the studies presented by the different authors. Only in one article can an improvement in pain be found, whilst in the others no improvement is to be found.7 One work presents good results in large or medium sized tears,27 whilst another finds benefits in small or medium sized tears, but not in large ones.10 This all suggests that for some unidentified reason (type of tear, preparation or form of PRP administration, adjuvant treatments used, moment of administration, etc.), there is no concordance between the low positive results observed in the different clinical studies, and sometimes there are contradictory results. The 5 studies which had positive or partially positive results used different PRP preparations and different administration protocols,26,27,34,36,39 and it is therefore not possible to establish with which PRP preparation or which administration protocol the best outcome was obtained. Moreover, Vavken et al.10 carried out a cost-effectiveness study, and concluded that the use of PRP is not cost-effective, not even in the group of tears in which it was effective (small and medium sized tears).
In the studies which dealt with the application of PRP in tendinopathies or in partial tears without cuff repair, results were not constant either, and we found that in several series there was an improvement with PRP.34,39 In other studies no statistically significant differences were found24,25,37 and in another only partially positive results were found (early benefit, with no differences in the mid and long term).26
It is important to bear in mind that, in the different studies, PRP is prepared differently, with different protocols, or with different adjuvant treatments. The laboratory studies demonstrated that the effects of PRP vary in relation to the medium used for its preparation14 or the coadjutants used.16–18,20,21 For this reason, when designing a protocol for a clinical study or when using PRP in patients one would have to take into account the form of preparing the PRP, the form of application and whether it was necessary to use a combination of adjuvant treatments.
ConclusionsThis work shows that no solid scientific and/clinical evidence exists for the use of PRP in the treatment of rotator cuff pathology in standard clinical practice. Prior to its general use further studies would be needed to define into what types of injury of the cuff it would be useful to apply PRP, how it should be prepared and applied and whether it would also be necessary to include some type of adjuvant treatment. Furthermore, precise objectivity is required to state how PRP improves (if it does) the cuff tear (in a constant and reproducible manner): time of wound healing, quality of tissue, pain, workability, etc. and lastly, whether it can be demonstrated that PRP is effective, the cost-effectiveness of its usefulness would need to be defined.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that for this research investigation no experiments have been performed on humans or animals.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestsThey have no conflict of interests to declare.
Please cite this article as: Miranda I, Sánchez-Alepuz E, Lucas FJ, Carratalá V, González-Jofre CA. Utilización del plasma rico en plaquetas en el tratamiento de la patología del manguito de los rotadores. ¿Qué hay demostrado científicamente? Rev Esp Cir Ortop Traumatol. 2017;61:249–258.