It is very important to treat prosthetic infections correctly in order to ensure a higher success rate. Debridement with implant retention (DAIR) is widely used in acute and late infections, however patients who fail after this surgery are known to have a higher risk of failure in subsequent surgeries. Therefore, it is important to find a scale that enables us to predict the risk of DAIR failure. Hence the KLIC and CRIME80 scores for acute and late acute infections, respectively. This study analysed the validity of both scores in acute late periprosthetic knee infections. We observed that the KLIC score has no predictive value for this type of infection, but the CRIME80 score does.
En las infecciones protésicas es muy importante realizar un tratamiento correcto con el que podamos asegurar una mayor tasa de éxito. Bien es cierto que el desbridamiento con retención de implante (DAIR) es una cirugía muy utilizada en infecciones agudas y agudas tardías, pero se sabe que los pacientes que fracasan tras esta cirugía tienen mayor riesgo de fracaso en cirugías posteriores. Es por ello, que es importante encontrar una escala que nos permita predecir el riesgo de fracaso de DAIR. Así nacieron la escala KLIC y CRIME80 para infecciones agudas e infecciones agudas tardías respectivamente. Con este estudio hemos analizado la validez de ambas escalas en infecciones periprotésicas de rodilla agudas tardías y hemos observado que el KLIC no tiene valor predictivo para este tipo de infecciones, pero sí que lo tiene la escala CRIME80.
Infection is one of the most serious complications in prosthetic surgery. The rate of infections in primary prosthetic knee surgery ranges between 1% and 2%, depending on the series,1–3 and increases up to 10% in revision surgery.1,2 Prosthetic infections may be classified into acute postoperative, chronic or late acute, with the latter being mostly haematogenous.3–5 This classification helps us to establish prognosis and treatment. In cases of acute postoperative infections, initial treatment is debridement with replacement of polyethylene, implant retention and antibiotics (debridement, antibiotics and implant retention - DAIR). Although the latest guidelines6,7 still recommend DAIR for acute, and late infections, several authors6,8,9 consider this leads to poorer control of infection than in acute postoperative infection.
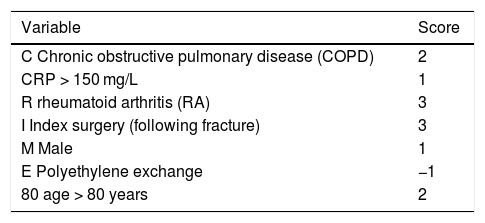
In acute postoperative prosthetic infections DAIR has an infection control rate of 31%–100% of cases.10 The standard risk factors (infection by Staphylococcus aureus, patient comorbidities, duration of symptoms and intra-articular pus) which are associated with a higher risk of failure after debridement, are related to preoperative and intraoperative medical aspects.11 When the DAIR fails, rescue with two-stage exchange presents with poorer results.9,12 In 2015, Tornero et al.13 proposed an evaluation scale called KLIC, to determine which patients were at greatest risk of failure after DAIR in the treatment of acute postoperative prosthetic infection of the knee or hip. The scale considers five preoperative risk factors (Table 1) and establishes five groups of lower to higher risk. This same scale was validated in 2018 in another centre and obtained similar results.14 In both studies the late acute infections were eliminated from analysis. A higher rate of failure of DAIR was described in late acute infections and also attempts have been made to establish a tool which may predict the risk of failure of DAIR in this type of infection.8,9 The work group dealing with implant-associated infections (ESGIAI)15 performed an analysis of the risk factors relating to the failure of DAIR in late acute infections and established the CRIME80 scale. This scale addresses seven risk factors (Table 2) and establishes a low risk group and a high risk group.
CRIME80: Score for assessing risk of failure of the DAIR in late acute prosthetic infections.
| Variable | Score |
|---|---|
| C Chronic obstructive pulmonary disease (COPD) | 2 |
| CRP > 150 mg/L | 1 |
| R rheumatoid arthritis (RA) | 3 |
| I Index surgery (following fracture) | 3 |
| M Male | 1 |
| E Polyethylene exchange | −1 |
| 80 age > 80 years | 2 |
This study analyses the validity of the KLIC and CRIME80 scale in patients who underwent DAIR after a diagnosis of late acute knee prosthetic infection.
Material and methodsA retrospective study in which the usefulness of the CLIC and CRIME80 scales for establishing risk of failure in patients diagnosed with late acute knee prosthetic infection and treated with DAIR from January 2010 to December 2017 was analysed. This study was approved by the Clinical Research Ethics Committee of our centre (PI-18-095).
Late acute prosthetic infection of the knee was defined as that which presented in patients with a previous history of normal function after primary prosthesis and who suddenly developed symptoms and signs of infection, more than three months after surgery. The prosthetic infection was diagnosed using the Musculoskeletal Infection Society (MSIS)4 criteria. Patients with an active fistula or with symptoms of over three weeks onset were not considered to be DAIR treatment-derived.
We analysed 17 patients who had undergone DAIR during this period of eight years, and we lost one patient with late acute infection due to lack of data; five patients (29%) were diagnosed with acute postoperative infection, and were therefore removed from analysis and 11 (71%) remained with late acute infection. Nin per cent of the patients were men and 91% women. The right knee was affected in 63.6% and mean age was 68 years (interquartile range:19 years).
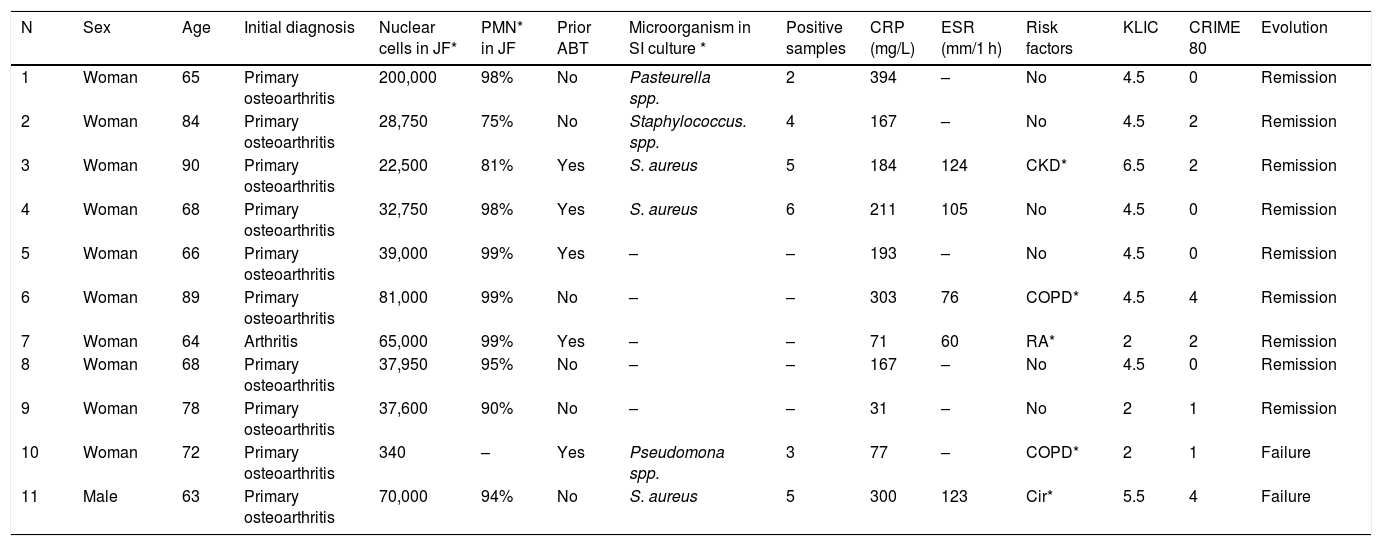
Data on comorbidities related to risk factors of the studied scales were collected (kidney disease, cirrhosis, chronic obstructive pulmonary disease, rheumatoid arthritis), the analytical markers of the blood count of the acute phase reactants, C-reactive protein (CRP mg/L) and erythrocyte sedimentation rate (ESR mm/1 h), the cell count (cells/mm3), percentage of polymophonuclears leukocytes of joint fluid samples and the microbiological results regarding number of positive cultures of joint fluid and synovial tissue and identified microorganism. The date of surgery was also recorded, together with type of surgery and patient evolution (Table 3).
Epidemiological, anatomopathological, biochemical data, KLIC, CRIME80 scales and patient evolution of patients diagnosed with acute late prosthetic infection de los patients.
| N | Sex | Age | Initial diagnosis | Nuclear cells in JF* | PMN* in JF | Prior ABT | Microorganism in SI culture * | Positive samples | CRP (mg/L) | ESR (mm/1 h) | Risk factors | KLIC | CRIME 80 | Evolution |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Woman | 65 | Primary osteoarthritis | 200,000 | 98% | No | Pasteurella spp. | 2 | 394 | – | No | 4.5 | 0 | Remission |
| 2 | Woman | 84 | Primary osteoarthritis | 28,750 | 75% | No | Staphylococcus. spp. | 4 | 167 | – | No | 4.5 | 2 | Remission |
| 3 | Woman | 90 | Primary osteoarthritis | 22,500 | 81% | Yes | S. aureus | 5 | 184 | 124 | CKD* | 6.5 | 2 | Remission |
| 4 | Woman | 68 | Primary osteoarthritis | 32,750 | 98% | Yes | S. aureus | 6 | 211 | 105 | No | 4.5 | 0 | Remission |
| 5 | Woman | 66 | Primary osteoarthritis | 39,000 | 99% | Yes | – | – | 193 | – | No | 4.5 | 0 | Remission |
| 6 | Woman | 89 | Primary osteoarthritis | 81,000 | 99% | No | – | – | 303 | 76 | COPD* | 4.5 | 4 | Remission |
| 7 | Woman | 64 | Arthritis | 65,000 | 99% | Yes | – | – | 71 | 60 | RA* | 2 | 2 | Remission |
| 8 | Woman | 68 | Primary osteoarthritis | 37,950 | 95% | No | – | – | 167 | – | No | 4.5 | 0 | Remission |
| 9 | Woman | 78 | Primary osteoarthritis | 37,600 | 90% | No | – | – | 31 | – | No | 2 | 1 | Remission |
| 10 | Woman | 72 | Primary osteoarthritis | 340 | – | Yes | Pseudomona spp. | 3 | 77 | – | COPD* | 2 | 1 | Failure |
| 11 | Male | 63 | Primary osteoarthritis | 70,000 | 94% | No | S. aureus | 5 | 300 | 123 | Cir* | 5.5 | 4 | Failure |
Surgical treatment was performed by different surgeons specialising in prosthetic knee surgery. Antibiotic prophylaxis was administered (cefazolin 2 g ev) 30−60 min prior to surgery. Debridement was performed with no expression of affected limb ischaemia. In all cases the approach was through the pre-existing site. Arthocentesis was performed and the appearance of the joint fluid was analysed, being sent to the laboratory for cell count and biochemical testing of glucose (mg/dl) and proteins (g/L) and for microbiological study in an enriched medium (Bactec™ FX culture system ). Medial arthrotomy was performed with extensive synovectomy and excision of all necrotic tissues at the back of the pouch and lateral recesses. The polyethylene insert was removed and exeresis of synovial fluid and necrotic tissues from the posterior joint capsule was performed. Three to five synovial tissue samples were taken from the back of the pouch, lateral recesses and posterior capsule, and were sent to the laboratory for microbiological testing. The site was irrigated with 9 L of physiological saline solution and in all cases the femoral and tibial component was preserved, once the absence of loosening had been confirmed. A new polyethylene prosthesis of suitable thickness was implanted to provide good joint stability and closure was performed through joint planes with intra-articular drain. This was removed after 24−48 hours when volume was below 50 mL in the last six hours.
Following debridement with implant retention, a broad spectrum intravenous antibiotic treatment was established with vancomycin (1 g/12 h) plus ceftazidime (2 g/8 h) which was maintained until the result of the culture and antigiogram was made available. Intravenous antibiotic treatment was maintained for 15 days and later changed to oral biofilm antibiotics for six weeks or more, depending on the clinical evolution of the patient and the acute phase reactants. After discharge the patients continued having clinical and analytical controls (CRP, ESR) each month up until the end of the antibiotic treatment and every three or six months up until one year. Rehabilitation commenced 24−48 hours after surgery, with isometric exercises, active and passive joint mobilization, sitting up and walking, in keeping with tolerance.
Six patients presented with infections due to a single microorganism: Three with Staphylococcus aureus, one with Pasteurella spp., one with Staphylococcus spp. and one with Pseudomona spp. The other five patients presented with negative cultures, but showed a biochemically pathological joint fluid and two of them received antibiotic therapy for two weeks prior to debridement (Table 3).
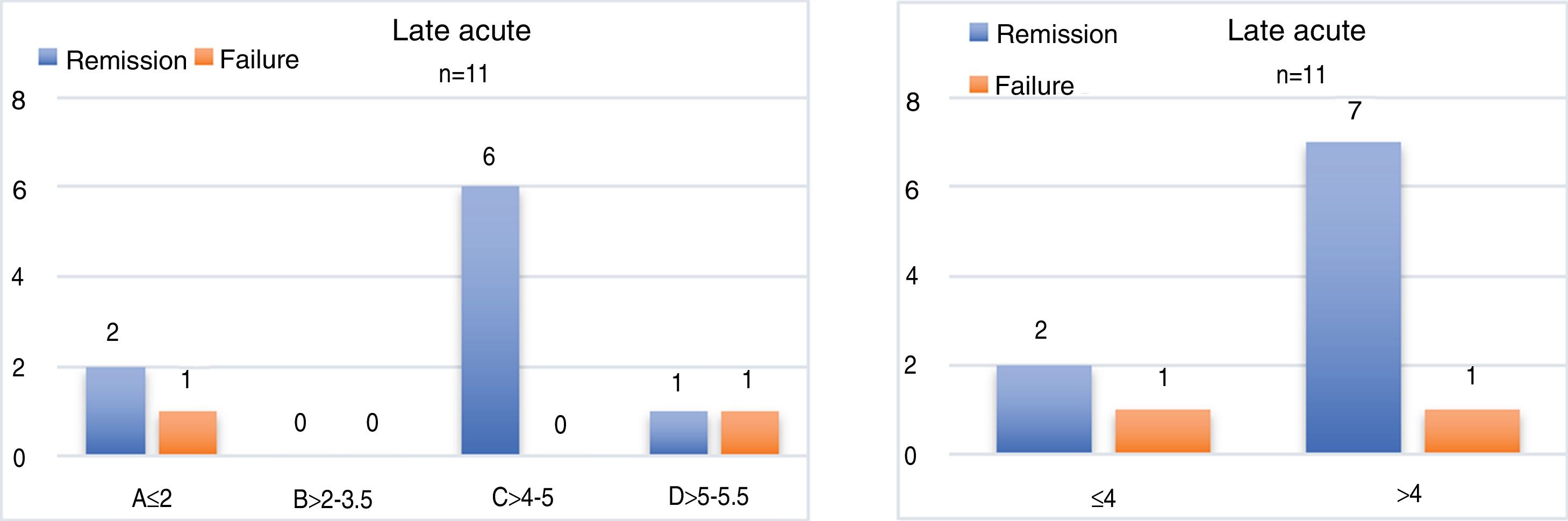
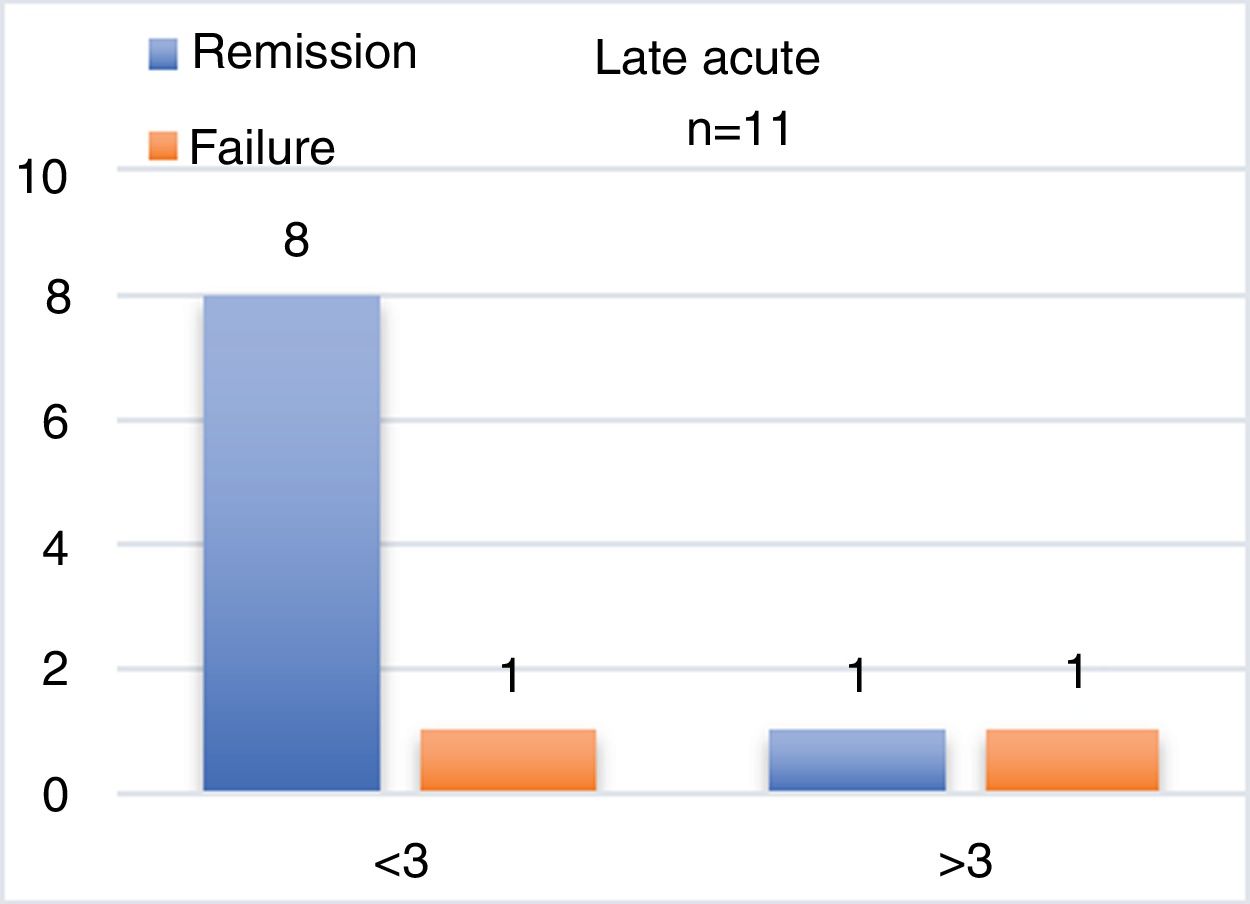
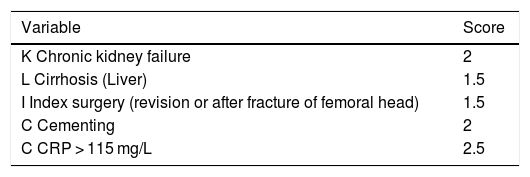
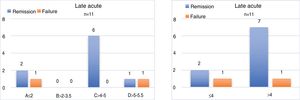
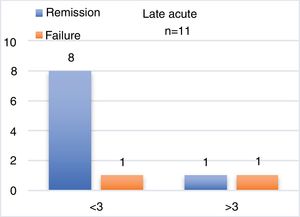
For analysis of the KLIC scale, which ranges from a score of 0–9 points, the patients were divided into five risk groups depending on the score obtained, similarly to the original study.13 Group A (<2), B (> 2–3.5), C (4–5), D (> 5–6.5), and E (>7) ranging from lesser to greater risk of failure. To increase the number of cases per group the KLICC scale was divided into two groups of low and high risk of failure, with low risk being a score <4 and high risk >4. For analysis of the CRIME80 scale, patients were divided into two groups depending on their score, with the low risk of failure group being a score <3 and the high risk of failure group being a score > 3, similarly to the ESGIAI15 study, but in contrast to this study the CRIME80 scale was used for all patients, regardless of the causal germ.
To define treatment failure the same criteria were used from the Tornero et al.13 article which are: 1) the patient needed secondary surgery during the first 60 days after DAIR to control infection (second debridement or removal of the implant, 2) death of the patient related to infection during the first 60 days after DAIR or 3) need for suppressive antibiotic therapy.
ResultsThe patients presented with the following distribution on application of the KLIC scale: Three patients belonged to group A, six to group C and two to group D. In group A we observed a patient with failure after the DAIR (33%) from the need for suppressive antibiotics. This patient had CRP of 77 mg/l which was the highest in the whole group. All the patients in group C had an infection control after DAIR and presented with a mean CRP of 223 mg/l. Finally of the two patients of group D, one (50%) had a failure after DAIR which was the patient who presented with the highest CRP (300 mg/l), and removal of the prosthetic material was required. If we consider the KLIC scale in both groups, of the three low risk patients, one failed (33%) and of the eight high risk patients also one patient presented with failure (12.5%) (Fig. 1) (Table 3).
The application of the CRIME80 scale was distributed in the following manner: nine patients belonged to the DAIR low failure risk group with CRIME80 < 3 and two patients to the high risk group with CRIME80 > 3. In the low risk group only one patient presented with failure (11%), and in the high risk group one patient presented with failure, representing 50% of this group (Fig. 2) (Table 3).
DiscussionThe KLIC scale was applied for the first time in this study, which assesses the risk of failure of DAIR in acute postoperative prosthetic infection, and in late acute postoperative prosthetic infection confirming that there is no predictive value in this type of prosthetic infection. The CRIME80 scale was also validated for the first time, which assesses the risk of failure of DAIR in late acute prosthetic infection, with confirmation of its predictive value in this type of infection.
When the KLIC scale was applied the distribution of the patients with a acute prosthetic infection into risk groups was completely different from that described in acute postoperative infections.13–15 Late acute prosthetic infection shows different clinical symptoms to acute postoperative infections, which usually results in problems of the surgical wound, such as persistent draining, and with less raised CRP markers.8 Our data do not differ from those of the literature,8,9,11,12 with a mean CRP of 190.78 mg/l whilst in patients with acute postoperative infections this was 74.7 mg/L. The KLIC scale attaches importance to cementing of the prosthesis as a risk factor, giving 2 points to all cemented prostheses. The difference in cementing probably is of significance in total hip replacements where the two types of cemented and non cemented attachments are used, mainly depending on age and bone quality, but in total knee replacements cemented attachment predominates. Previous studies13–15 have assessed cementing jointly and separately in hip and knee replacements. Bearing in mind that in our medium all knee prostheses were cemented, this parameter was of no discriminative value and led to displacement of risk to the right. In other words, raised CRP and cemented implants increased the number of patients in groups of possible risk of failure.
When applying the CRIME80 scale, we observed a distribution into risk groups which was similar to that described,16 obtaining a failure rate of 11% in the lower risk group vs. 50% in the higher risk group (Fig. 2).
The CRIME80 and KLIC scales coincided in considering as a risk factor for failure of DAIR raised CRP markers and initial indication for prosthetic surgery (fractures), but they differed in their consideration of other risk factors. There was also a discrepancy between the value of the CRP cut-off point in these two scales with it being higher in the CRIME80 (150 mg/l vs. 115 mg/l) scale. Late acute prosthetic infections present higher CRP markers than the postoperative acute infections, with this making the CRP cut-off point in the KLIC scale less discriminative, because the majority of late acute prosthetic infections are above the cut-off value of this scale.
Unlike the KLIC scale, the CRIME80 scale does not account for a history of kidney disease or chronic liver disease, but it does consider chronic obstructive pulmonary disease and rheumatoid arthritis as risk factors. It does not value the cementing of an implant as a risk factor but the male sex, polyethylene exchange on debridement and being aged over 80 years are considered risk factors. Although it has been argued17 that there is a close relationship between rheumatoid arthritis and a higher risk of failure of the treatment of late acute and chronic prosthesis infections, other authors16,18 consider that the highest risk factor of DAIR failure in late acute infections is the infection by streptococcus and not the replacement of mobile components.
When DAIR does not achieve its aim and the patient requires further debridement or a replacement implant, a higher rate of failure with repeated debridement has been described12,19 together with a poorer two-stage replacement outcome after failure of the DAIR.12,19 For this reason criteria or scales are sought as tools to help decide which patients will benefit from DAIR and which will be likely to fail. As a result a different type of initial treatment could be indicated, such as one or two stage debridement or more prolonged suppressive antibiotic treatment.
The KLIC scale provides useful information about prognosis and risk of failure of DAIR in cases of acute postoperative prosthetic infections,13–15 but it does not appear that this scale has a prognostic value in cases of late acute infection.
The CRIME80 scale assesses the risk of failure of the DAIR in cases of late acute infections.16 When applying the CRIME80 scale to our patients with late acute prosthetic knee infections we were able to confirm that characteristics were similar to the original article16 and that it was useful for assessing the risk of failure of the DAIR.
This study has certain limitations. Firstly, the small sample size may increase or reduce minor differences. Secondly, all the knee prostheses in our medium were cemented. As a result this parameter was not discriminative and since all patients were given two points, the risk of failure was to the right of the KLIC scale, increasing it. Finally, the CRIME80 scale assesses patients with Staphylococcus aureus infections separately because this scale has a higher predictive value of the risk of failure of DAIR in infections caused by other microorganisms. Due to the small sample size we did not analyze Staphylococcus aureus infections separately from those caused by other microorganism, but despite this, the predictive value of the scale was still high.
We conclude that the KLIC scale does not seem to have a predictive value of failure of DAIR in the treatment of late acute prosthetic infections, but the CRIME80 scale does.
Level of evidenceLevel of evidence III.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Sabater Martos M, Hernandez Hermoso JA, Garcia Oltra E, Molina S, Martínez-Pastor JC. Validez de las escalas KLIC y CRIME80 en la predicción del fracaso en la infección aguda tardía tratada mediante desbridamiento y retención de implantes. Rev Esp Cir Ortop Traumatol. 2020;64:415–420.