This study aims to compare clinical and functional results after distal biceps tendon repair in manual workers vs. non-manual workers.
MethodsThis is a retrospective comparative study which refers to 57 cases with distal biceps tendon rupture, divided in manual workers (24 elbows) and non-manual workers (33), that were treated by a single incision with cortical button and interference screw fixation. Included cases have a minimum of 3 months follow-up, post-operative X-ray and signed informed consent for the investigation.
ResultsSupination and flexion strength was higher in manual workers vs. non-manual workers (p-value=0.192 and 0.878, respectively). Nine patients showed loss of range of motion, concerning supination and pronation, and this was correlated to worse functional scores. Functional scores tend to be superior in non-manual workers. Ten patients had heterotopic ossification and 20 patients reported lateral antebrachial cutaneous nerve neuropraxia; one had both. Most of them had a full recovery.
ConclusionAccording to clinical evaluation and post-operative scores, the performed surgical procedure provides good to excellent mid-term functional results. Nevertheless, there were not any differences between manual or non-manual workers.
Este estudio tiene como objetivo comparar los resultados clínicos y funcionales tras de la reparación del tendón distal del bíceps braquial (RTDBB) entre trabajadores manuales y no manuales.
Material y MétodoEstudio retrospectivo comparativo de 57 casos con rotura del tendón distal del bíceps, divididos en trabajadores manuales (24 codos) y no manuales (33), tratados mediante una única incisión de la piel con botón cortical y fijación con tornillos de interferencia. Los casos incluidos tienen un seguimiento mínimo de 3 meses, radiografía postoperatoria y consentimiento informado firmado para la investigación.
ResultadosLa fuerza de supinación y flexión fue mayor superior en los trabajadores manuales que en los trabajadores no manuales (valor de p 0,192 y 0,878, respectivamente). Nueve pacientes presentaron pérdida de rango de movimiento, relativo a supinación y pronación, y se han correlacionado con peores puntuaciones funcionales. Las puntuaciones funcionales tienden a ser superiores en los trabajadores no manuales. Diez pacientes han presentado osificación heterotópica y 20 pacientes neuropraxia del nervio cutáneo antebraquial lateral; uno ha tenido ambas. La mayoría se recuperaron por completo.
ConclusiónEn consecuencia de los resultados clínicos y los funcionales, la RTDBB aporta buenos a excelentes a mediano plazo, sin complicaciones significativas. Aunque no han podido apreciarse diferencias entre trabajadores manuales y no manuales.
Distal biceps tendon rupture is a rare injury with an estimated incidence of 1.2–2.55/100,000 per year, representing 3% of all biceps injuries.1–10
It is more common in middle-aged men and usually involves the dominant arm1,7,11–15; it is often related to sports practice or heavy work, but it can also affect older and less active people in their daily life.7
A manual worker was considered, in this study, as a person who undertakes physical work including not only construction, installation, assembly, and building works but also an occupation involving labor, such as bar and restaurant staff or musicians and singers and fruit pickers (who do not use machinery).
Comparing to non-operative management, surgical treatment superiority has been established in the literature, concerning functional outcome, evaluation scores and the ability to resume work. Several studies show a loss of up to 40% in supination and 30% in flexion strength with conservative approach.3,12,14,16–20
In this study, we try to verify if being a manual worker could influence outcomes after the repair of a distal biceps injury. We hypothesize that the described technique allows full return to work with no limitations and low rate of permanent complications, taking advantage by using a single incision with a cortical button fixation coupled with an interference screw. Additionally, we analyze the complication rate and if its occurrence will affect the outcomes.
Material and methodsStudy design and populationRetrospective comparative case study which includes patients admitted sequentially in the same institution with the diagnosis of distal biceps tendon rupture between 1st January 2010 and 31st December 2021.
Data sourceAll study activities were approved by the institutional research ethics board, and all patients signed an informed consent form prior to study participation.
All the events were confirmed by consulting individual casefile. Query was performed using Glintt HS® (Glintt, Lisboa, Portugal) and the imaging studies review by Xero® (Agfa Healthcare, Greenville, SC).
Case definitionAll patients in the database with the diagnosis of distal biceps tendon rupture were screened. Only those who were managed by a single-incision approach and a cortical button fixation were included in the study. Other inclusion criteria are: minimum of 3 months follow-up, post-operative X-ray, signed informed consent for the investigation and functional evaluation. Patients who have had previous surgery on the assessed elbow, and those who have refused to participate or did not answer the clinical evaluation were excluded.
Data collectedGender, age, type of professional labor (manual worker or non-manual worker), injury side (dominant or non-dominant side), image studies (MRI or ultrasound scan and post-operative X-ray), time since injury to surgery and complications were recorded from the medical registry. Follow-up period was defined as the time between surgery and the last clinical assessment.
Elbow range of motion (ROM) (flexion, extension, supination and pronation at 90° of elbow flexion) from both sides, supination–pronation and flexion–extension isokinetic strength of the elbow were assessed using the MicroFet 2® dynamometer (Hoggan Scientific, Salt Lake City, UT) and were recorded in Newton (N). Flexion–extension strength was assessed with elbow at 90° of flexion, close to the body, and with dynamometer at the level of the wrist. In supination–pronation strength assessment, the patient held a stick in a fist, with the elbow in the same 90° of flexion position, close to the body, and started supination or pronation movement, connecting the dynamometer to the stick.
Visual analogue pain scale (VAS 0–10), overall satisfaction (subjective 1–5 scale), QuickDASH21 and Mayo Elbow Performance Scores (MEPS)22 were assessed.
Concerning that group of patients who have just answered questions by phone, we were not able to measure either ROM or strength, only the demographics and functional scores.
The questionnaire and functional assessment were performed by an independent investigator not involved in any surgery.
Treatment protocol – surgical techniqueA single anterior incision technique was performed. A transverse 3cm incision is made 3cm distal to the anterior elbow skin crease in every acute case, which could be enlarged until 5cm to deal with a possible retracted tendon in subacute cases.
Identification of the tendon stump is carried out. A whipstitch suture is made throughout the 2cm distal tendon, and tendon stump trimmed to fit an 8mm hole. The lateral antebrachial cutaneous nerve (LABCN) is identified and protected, lateral to the biceps tendon stump.
A limited vertical dissection between brachioradialis and pronator teres, with the forearm in full supination, allows radial tuberosity identification.
Placement of two Hohmann retractors centers the 3.2mm drill guide in radial tuberosity that should be inserted after maximal supination of the forearm in combination with a slight elbow flexion, inserted at 30° angle in lateral inclination from the vertical, simulating the original biceps insertion. An 8mm cannulated drill is inserted through the 3.2mm drill guide, perforating only the anterior cortex. After removing the drill and the guide, care should be taken to remove all visible bony remaining debris to prevent heterotopic bone formation.
After tuberosity preparation, free limbs of the biceps tendon suture are passed through the biceps button. The button is inserted in the tunnel using a dedicated introducer, flipped after reaching the posterior radius bone cortex and the tendon stump inserted through the anterior radius cortex by alternating pulling on the sutures, often with the elbow in flexion as needed (at least 10mm should be inserted). The system is locked by passing one of the suture limbs through the tendon.
Finally, a tenodesis PEEK 7mm screw is inserted through the anterior radius cortex in a radial position to push the bicipital tendon towards ulnar position, closer to its native position, maximizing supination strength, until it seats flush in the radial cortex.
Treatment protocol – post-operative rehabilitationOur protocol comprises immediate mobilization, using a sling just for comfort in the first week followed by active motion with load limitation (up to ½kg) in the first two weeks and strengthening exercises allowed at 6–8 weeks after surgery. All patients are allowed to return to unrestricted function, either involving sports or work environment, 3 months after surgery.
Statistical analysisWe conducted a patient descriptive analysis: gender, age at injury time, type of professional labor (manual worker or other), injury side (dominant/non-dominant), image evaluation, time-lapse since injury to treatment, and complications. Clinical evaluation and clinical scores using Microsoft Excel® were reported.
Comparison between the range of motion and strength of both sides using a Wilcoxon statistical test for paired samples was performed; heterotopic ossification and paresthesia occurrence with χ2 test, and the Mann–Whitney test for range of motion, strength, VAS, QuickDASH, Mayo and satisfaction scores (subjective 1–5 scale). All the statistical tests were performed with IBM SPSS Statistics 28.0.
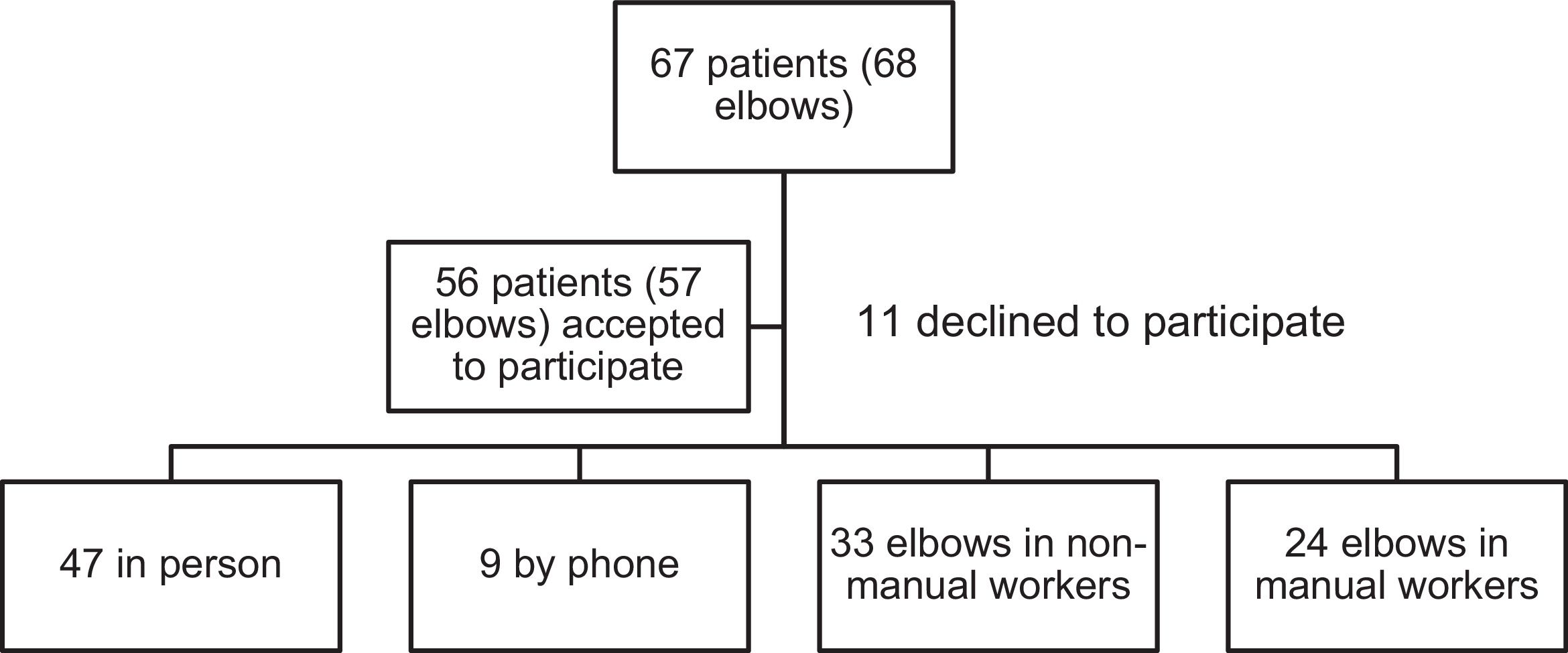
ResultsSixty seven patients (68 injuries – one patient had bilateral injury) in our database with the diagnosis of distal biceps tendon rupture were found, who were surgically treated with a single-incision approach and using Biceps Button® (Arthrex, Naples, FL) fixation. All surgeries were performed by the same team. From the 67 patients (68 cases) treated, 56 patients (57 cases) accepted to participate in this study – 47 patients have attended our clinical evaluation and 9 have answered by phone (Fig. 1). So, 56 patients (57 cases) were included for demographic data and questionnaire responses (VAS, Subjective Scale, QuickDASH and MEPS). Moreover, for clinical assessment of range of motion and strength, only patients who attended in person to the clinics were included (47 patients/48 cases).
All patients were male. Mean age at injury time was 47 years old (27–76). Twenty-four elbows corresponding to manual workers vs. 33 non-manual workers (Fig. 1). Right side was the most affected (n=32; 56%). In 23 cases (40%), the affected side was the non-dominant one.
Mean time between injury and surgery was 25 days (3–133).
Mean follow-up between surgery and last visit was 33 (±29.5) months.
Mean supination strength on the affected and contralateral side was 5,746±2,365N and 5,911±2,156N, respectively (p-value=0.058).
Mean flexion strength on the affected and contralateral side was 25,893±6,623N and 26,291±6,279N, respectively, with no statistically significant difference (p-value=0.238).
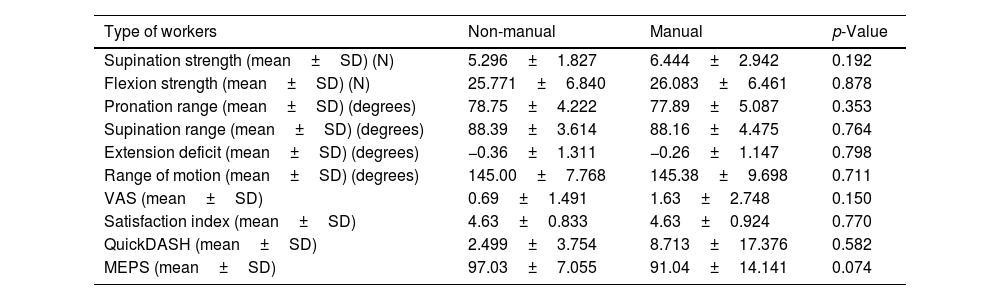
Supination and flexion strength was higher in manual workers without statistically significant difference to the non-manual workers (p-value=0.192 and 0.878, respectively).
A total of 9 patients showed reduced range of motion compared to the contralateral side. There were deficits of pronation in 7 patients, supination in 9 patients and extension in 3 patients. In these patients, mean loss of pronation was 10.7° (5–20°), mean loss of supination was 8.9° (5–15°) and the mean loss of extension was 5°. Overall, comparing mean supination, pronation and extension of the injured limb with standard values, considering 90° for supination, 80° for pronation and 0° for extension, there were statistically differences for mean supination (88.3±3.9°) and mean pronation (78.4±4.6°), but not for extension. No differences were verified in VAS and satisfaction scores. In those with a reduced range of motion, a worse QuickDASH score (p-value=0.031) was verified and it was closely correlated to lower MEPS (p-value=0.051).
Mean total range of motion on the affected and contralateral side was 145.2±8.5° and 145.9±7.9°, respectively, with no statistically significant difference between both sides (p-value=0.068). The range of motion was not different between manual or non-manual workers.
The mean overall VAS was 1.04 (0.00–10.00) and satisfaction score was 4.6 (1–5). Manual workers reported more intense pain than non-manual workers (1.63 vs. 0.69), without statistically significant difference. The satisfaction index was similar in both groups (4.63).
Mean overall QuickDASH and Mayo Elbow Scores were 5.2 (0–65.9) and 94.5 (45–100), respectively. The functional scores tend to be superior in non-manual workers as shown by mean QuickDASH (2,499 vs. 8,713) and MEPS (97.03 vs. 91.04).
Data comparing manual and non-manual workers are resumed in Table 1.
Comparison of clinical and functional scores between manual and non-manual workers.
| Type of workers | Non-manual | Manual | p-Value |
|---|---|---|---|
| Supination strength (mean±SD) (N) | 5.296±1.827 | 6.444±2.942 | 0.192 |
| Flexion strength (mean±SD) (N) | 25.771±6.840 | 26.083±6.461 | 0.878 |
| Pronation range (mean±SD) (degrees) | 78.75±4.222 | 77.89±5.087 | 0.353 |
| Supination range (mean±SD) (degrees) | 88.39±3.614 | 88.16±4.475 | 0.764 |
| Extension deficit (mean±SD) (degrees) | −0.36±1.311 | −0.26±1.147 | 0.798 |
| Range of motion (mean±SD) (degrees) | 145.00±7.768 | 145.38±9.698 | 0.711 |
| VAS (mean±SD) | 0.69±1.491 | 1.63±2.748 | 0.150 |
| Satisfaction index (mean±SD) | 4.63±0.833 | 4.63±0.924 | 0.770 |
| QuickDASH (mean±SD) | 2.499±3.754 | 8.713±17.376 | 0.582 |
| MEPS (mean±SD) | 97.03±7.055 | 91.04±14.141 | 0.074 |
SD: standard deviation; N: Newton (strength); VAS: visual analogue scale; MEPS: Mayo Elbow Performance Score.
Ten patients had heterotopic ossification (HO) and 20 patients reported lateral antebrachial cutaneous nerve (LABCN) neuropraxia; one had both complications. All patients who presented HO were asymptomatic and no range of motion restriction was noted. Those who reported LABCN neuropraxia had a full recovery, with all but one referring no significant impairment on daily activities. The occurrence of any complication did not affect VAS (p=0.488), overall satisfaction (p=0.786), QuickDASH (p=0.356) and Mayo Elbow (p=0.177) Scores.
DiscussionRupture of the distal biceps tendon is prevalent among middle-aged males, affecting mostly the dominant arm which is consistent with our results and the published literature.3,7,8,12,14,16,23–25 Although this injury usually occurs in manual laborers, only 41% of the patients included in our study could be considered so – Siebenlist et al. presented a sample consisting of 50% of patients with this feature.24
In our study population, with a mean follow-up of 33 (±29.5) months, there was a mean loss of 2.8% in supination and 1.5% in flexion strength when compared to the contralateral side, which means that it is not statistically different from one to another, as well as Redmond et al.5 reported on their study. Our patients retained a slightly increased percentage of post-operative strength ratio, compared to the results of Alech-Tournier et al.,1 Siebenlist et al.,24 and Dillon et al.25 with 15, 28 and 30.9 months of follow-up, respectively. Huynh et al. reported that, in their case series of 60 patients, elbow flexion and supination strength values were decreased in the affected arm compared to the unaffected one.3 Combining data from these studies and ours, it seems evident that patients regain the majority of strength post-operatively, but some deficits remain. For the most, these minimal differences in strength were not clinically relevant.
Our overall ROM was 145° which is in line with published literature1,10,23,24 and there was no significant statistical difference between the affected side and the unaffected one.
Patients’ final analysis revealed a mean supination of 88.30°, mean pronation of 78.40° and mean extension of 0°. In comparison to other studies, our results were similar.3,23,24,26,27 Supination and pronation are the parameters that were significantly impaired in relation to the contralateral limb, with a mean difference of 1.70° and 1.60°, respectively, as it was found by Huynh et al. in their investigation.3 Siebenlist et al. reported an average of 82.2° of supination, 85° of pronation and 0.2° of extension,23 while Lang et al. achieved 73.4° of supination and 78.3° of pronation.24 Our mean QuickDASH score was 5.16 and Mayo Elbow Score was 94.46 which are similar to other studies.3,5,8,14 Concerning heterotopic ossification, our results are consistent with the majority of the case series, which present a great variability in incidence (2.9–56.7%).1,3,4,23,24 Considering the occurrence of LABCN paresthesia, our results are also in agreement with the literature as this complication is also very heterogeneous in published papers, with reports between 7% and 44%.1,3–8,12–14,24,25 We had no infections – superficial or otherwise.
None of the patients had re-ruptures and therefore there were no revision surgeries in the studied sample. Differently, reviewing the published information abroad, it is reported a 1.3–5% re-rupture rate.3,4 No failure of implants was recorded.
We found a correlation between a lower QuickDASH score and a reduced range of motion. MEPS was nearly statistically different (p=0.051). There were no differences with respect to VAS or satisfaction rate. Only 9 patients had impaired range of motion, with significantly lower functional scores, but we could not attribute it to any particular characteristic of the patients or surgical management.
We could not find any differences regarding range of motion, strength or all assessed scores (VAS, satisfaction, QuickDASH and MEPS) if injury was sustained by a manual worker or not, although there is a trend to lower QuickDASH and MEPS between manual workers. Maybe this aspect could be related to seeking compensation by the laborer from the Insurance Company. However, it is shown in our study that this procedure leads to excellent results. To our knowledge, this is the first study comparing scores between these two groups.
The study has some limitations: it is a retrospective assessment of an heterogeneous population; functional results (both strength and range of motion evaluation) were compared to the contralateral side which can lead to erroneous values, because usually they are not an exact comparison to the pre-injury levels of the affected arm; moreover, we did not take into account the dominant limb pre-injury values, which can alter the strength of the results, being that it is on average 10% stronger than the non-dominant hand.18
Face-to-face evaluation of patients with objective strength measures for supination and flexion and range of motion, complemented with radiographic analysis achieved from all patients, are the strengths of our study. We report the first study comparing results between manual and non-manual workers.
ConclusionAccording to our clinical evaluation and post-operative scores, we can state that surgical technique of a single-incision approach with a cortical button and an interference screw for the reattachment of the distal biceps tendon provides good to excellent functional results, with near complete recovery to the previous biceps function, low major complication rate and a fast return to previous condition.
To our knowledge, we report the first study comparing results between manual and non-manual workers, and we could not find any significant difference. So, it would be interesting to have further investigation on this issue to assess this finding and to optimize the outcomes regarding this population of heavy workers in whom full recovery takes greater importance, due to more exigent loads.
Level of evidenceLevel of evidence III.
Ethical committee approvalJosé Mello Saúde – Hospital CUF Descobertas, study no. 166.
FundingNo financial support was provided for conducting this research.
Conflict of interestsNo conflict of interests.
This manuscript has been read and approved by all authors, and each author believes that this manuscript represents honest work.