Morton's neuroma is predominantly attributed to chronic nerve entrapment within third space adjacent metatarsals, the deep transverse metatarsal ligament (DTML), and the plantar skin. While conservative treatments are of election, failures require alternative interventions such as ultrasound-guided injections and various surgical procedures, including minimally invasive neurectomy and DTML release. This study aimed to anatomically assess the risks associated with the endoscopic dorsal surgical decompression of Morton's neuroma.
Materials and methodsTwenty feet from ten fresh-frozen cadaveric specimens underwent a dorsal percutaneous approach for endoscopic access. Surgical procedures were monitored by three foot and ankle surgeons. Post-surgical anatomical dissections were conducted to evaluate potential risks to surrounding structures.
ResultsThe endoscopic technique successfully sectioned the DMTL in all specimens (100%) without iatrogenic injury of tendons, nerves, or arteries, while lumbricals may be at risk.
ConclusionEndoscopic dorsal decompression of Morton's neuroma presents as an accessible minimally invasive surgical option with low risk of collateral associated injuries.
El neuroma de Morton se produce principalmente por el atrapamiento crónico del nervio entre el tercer espacio intermetatarsiano, el ligamento transverso intermetatarsiano profundo (LTIP) y la piel plantar. El tratamiento de elección inicial es el conservador, pero en los casos refractarios se requieren intervenciones alternativas como son las infiltraciones ecoguiadas o los procedimientos quirúrgicos. Entre los procedimientos quirúrgicos disponibles se encuentra la neurectomía mínimamente invasiva y la liberación del LTIP. El objetivo de este estudio fue evaluar anatómicamente los riesgos asociados con la descompresión quirúrgica dorsal endoscópica del neuroma de Morton.
Materiales y métodosVeinte pies de 10 especímenes cadavéricos congelados frescos fueron sometidos a un abordaje percutáneo dorsal para el acceso endoscópico. Los procedimientos quirúrgicos fueron realizados por 3 cirujanos de pie y tobillo. Se realizaron disecciones anatómicas posquirúrgicas para evaluar los daños producidos en las estructuras colindantes.
ResultadosLa técnica endoscópica seccionó exitosamente el LTIP en todos los especímenes (100%) sin lesionar iatrogénicamente tendones, nervios o arterias. Los músculos lumbricales fueron las estructuras más cercanas a la zona de trabajo, y con un mayor riesgo de lesión asociada.
ConclusiónLa descompresión dorsal endoscópica del neuroma de Morton se presenta como una opción quirúrgica mínimamente invasiva accesible, con bajo riesgo de lesiones colaterales asociadas.
Morton's neuroma precise etiopathology remains unclear, and despite its name, it is not a true neuroma but rather a fibrosis of the nerve.1 Chronic nerve entrapment appears to be the most plausible cause. Morton's neuroma has been related to a compressive ethology occurring in the tunnel formed by the adjacent metatarsals, the deep transverse metatarsal ligament (DTML), and the plantar skin. An insufficient space under the deep transverse metatarsal ligament may be related to its appearance.2
Main treatment for Morton's neuroma is conservative treatment, but when fails, other interventions, or even surgery may be an option. Despite multiple treatments have been proposed, there has been no proven clinical superiority of any particular technique over others. Ultrasound-guided corticosteroid injections and local anesthetics may result in the best outcomes, reducing pain and increasing function to treat Morton's neuroma.3 Other non-surgical treatments include alcohol injections, extracorporeal shockwave therapy, radiofrequency ablation, cryoablation, capsaicin injections, botulinum toxin and orthosis.4 If this treatment fail, surgery is the option, mainly neurectomy.3 But also alternative treatments including minimally invasive surgical procedures,5,6 cryoneurolysis,7 collagen conduits8 and DTML release have been proposed. Isolated DTML release has been reported as a primary operative management for chronic Morton's neuroma,9 and has been proposed with different approaches including percutaneous DTML ultrasound-guided release,10 DTML endoscopically guided release.11,12
The aim of this study was to assess anatomically the risks associated to endoscopically dorsal surgical decompression of Morton's neuroma.
Materials & methodsCadaver specimensTwenty feet from ten fresh-frozen cadaveric specimens obtained according to the body donation program of our institution as stated by the current laws. The specimens used were sectioned below the knee and disarticulated. The mean age of the specimens was 79 years old, and 6 were female and 4 male. The anatomical study was performed by three foot and ankle surgeons. One surgeon performed the incision, while the other two monitored the procedure. The study was carried out in accordance with the ethical standards recognized by the Declaration of Helsinki (1993).
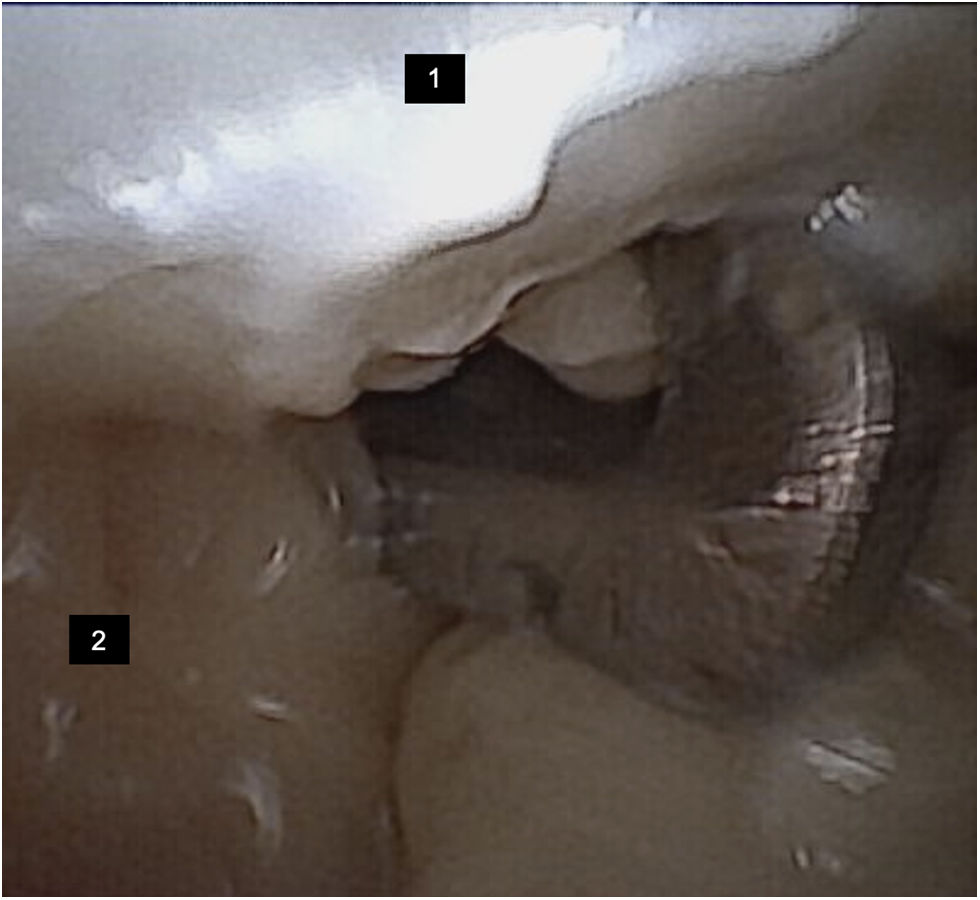
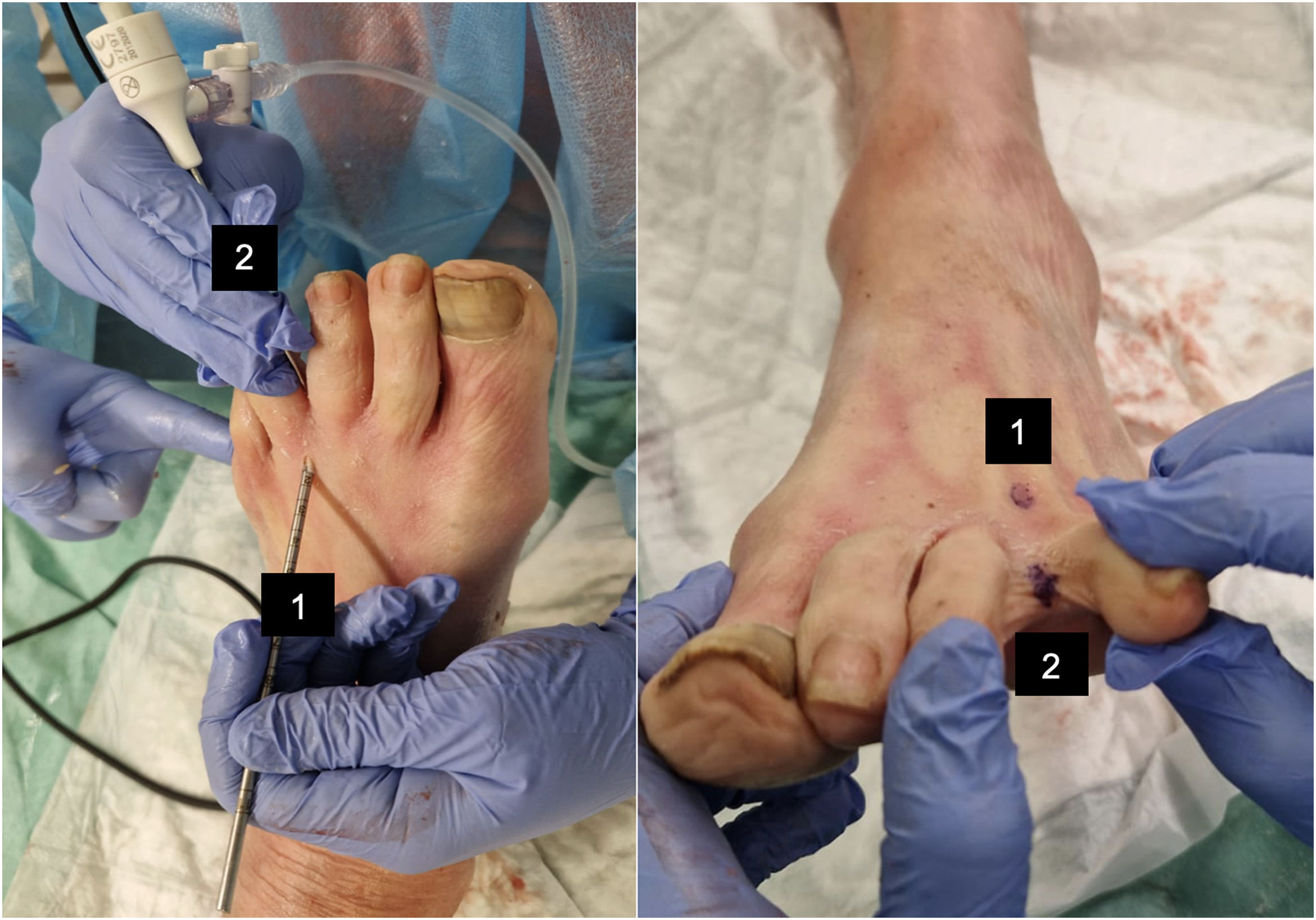
Surgical procedureThe procedure was conducted through a dorsal percutaneous approach performed through two incisions made with a 2mm blade to allow endoscopic access. The viewing portal was created in the interdigital space between the third and fourth toes at twelve o’clock, directly facing the DTML. The visualization was obtained through a 1.9-mm 0-degree Nanoscope® (Arthrex, Naples, FL) with a protective cannula for scope insertion and connection for irrigation. The working portal was created 2.5cm proximal to the level of the dorsal metatarsophalangeal joint, through which a retrograde hook was introduced. Direct visualization of the third intermetatarsal ligament allowed an endoscopically controlled section with the retrograde hook (Fig. 1, Supplementary Material 1). This technique may put the lumbrical tendon at risk due to its anatomical positioning and relationship (Fig. 2).
After the surgical procedure, each foot was carefully dissected from the dorsum to expose anatomical structures at risk in the intermetatarsal space, including the lumbrical tendon, extensor digitorum longus, extensor digitorum brevis, interdigital nerves, and dorsal digital arteries. All these structures were checked to assess any related injuries (Fig. 3).
ResultsIn the 20 feet, the technique was performed successfully, achieving the section of the deep intermetatarsal ligament under endoscopic vision in the third intermetatarsal space in 100% (20/20) of cases. In all cases, the section was complete. None of the specimens presented Morton's neuroma. No iatrogenic injuries including section or visible laceration were found in tendons, nerves, or arteries. No other incidents were reported.
DiscussionThe present study evaluates the anatomical effectiveness and safety of endoscopic dorsal decompression of Morton's neuroma. This minimally invasive endoscopic DTML release through dorsal approach to Morton's neuroma demonstrated with high effectiveness and a low incidence of collateral injuries in the analyzed anatomical specimens.
The endoscopic intermetatarsal neuroma decompression technique is less invasive, reduces the risk of complications, and facilitates a quicker return to normal activities compared to traditional open surgical methods.3 Additionally, it preserves nerve function, maintaining distal sensitivity without increasing the risk of intermetatarsal angle alteration or splayfoot, and allows patients to immediately bear weight and resume daily activities.13 Previous literature has proposed endoscopic intermetatarsal ligament decompression techniques as having the advantage of minimal incision, minimum soft tissue dissection, no ischemia, immediate weight-bearing, and quick return to daily activities,11,12 while others have stated that minimally invasive decompression could only be effective in patients presenting absence of Mulder's sign or small neuromas.14
Surgical management of Morton's neuroma involves a variety of treatment modalities, but despite the numerous options, there is a scarcity of randomized controlled trials evaluating these interventions, particularly minimally invasive techniques.3 Among them, the DTML release, which could be performed through endoscopic access or ultrasound guidance. However, the ultrasound guided DTML release has been associated to the risk of an incomplete ligament release,10 which has not been described through the endoscopic proposed approach due to direct visualization section of the ligament. Although the lumbricals were identified as potentially at risk during the procedure, no damage of lumbricals were reported in the study.
Our study includes several limitations. First, possible bias due to the same team performing both the procedure and the postoperative dissection. Second, the procedures were conducted on cadavers without a diagnosed Morton's neuroma and with no known previous interventions in this area. Finally, some microscopic lesions could not be assessed by visual analysis.
In conclusion, endoscopic dorsal decompression of Morton's neuroma presents as an accessible minimally invasive surgical option with low risk of collateral associated injuries. Further clinical studies are needed to fully establish its efficacy across refractory patients to Morton's neuroma conservative treatment.
Level of evidenceLevel of evidence iv.
FinancingThis research has not received specific support from public sector agencies, the commercial sector or non-profit entities.
Conflicts of interestNone.