The lateral antebrachial cutaneous nerve (LACN) is the sensory branch of the musculocutaneous nerve and usually innervates the lateral aspect of the forearm. Isolated lesions are rare, of varied aetiology and generally underdiagnosed. We present a retrospective descriptive study of electromyography performed at the General University Hospital of Castellón in the last 20 years with isolated NCAL lesion. We identified 11 cases (8 men and 3 women), average age 44 years (15–73 years). 73% were referred from traumatology. Only one patient was correctly guided in the application. 63.6% of cases noted hypoesthesia extending to the wrist and 18.2% to the thumb. The electromyographic study showed severe axonal involvement in 3 patients and moderate in 8. The symptoms were observed associated with surgery in 4 patients, manipulation of the elbow flexure in 4 cases and bicipital tendonitis in the rest. Four patients had a poor clinical outcome (3 with severe axonal involvement and 1 with moderate involvement). Isolated involvement of the NCAL is a rare and underdiagnosed alteration. It is important to suspect it in patients with hypoesthesia in the forearm, including the radial edge of the wrist or thumb, especially if it is associated with manipulations around the elbow flexure or bicipital tendonitis. Electromyography is useful in confirming the diagnosis, ruling out other differential diagnoses, and predicting prognosis. Knowing the location of this nerve during manipulations on the arm and placing patients in an appropriate posture during surgeries can help minimize cases.
El nervio cutáneo antebraquial lateral (NCAL) es la rama sensitiva del nervio musculocutáneo y habitualmente inerva la cara lateral del antebrazo. Las lesiones aisladas son poco frecuentes, de etiología variada y generalmente están infradiagnosticadas. Presentamos un estudio descriptivo retrospectivo de las electromiografías realizadas en el Hospital General Universitario de Castellón en los últimos 20 años con lesión aislada del NCAL. Identificamos 11 casos (8 hombres y 3 mujeres), con edad media de 44 años (15-73 años). El 73% fueron remitidos desde traumatología. Solo un paciente fue orientado correctamente en la solicitud. El 63,6% de los casos notaba hipoestesia extendida hasta la muñeca y el 18,2% hasta el pulgar. El estudio electromiográfico mostró afectación axonal grave en 3 pacientes y moderada en 8. La clínica se observó asociada a: cirugía en 4 pacientes, manipulación en la flexura del codo en 4 casos y tendinitis bicipital en el resto. Presentaron mala evolución clínica 4 pacientes (3 con afectación axonal grave y uno moderada). La afectación aislada del NCAL es una alteración infrecuente e infradiagnosticada. Es importante sospecharla en pacientes con hipoestesia en el antebrazo, incluso en el borde radial de la muñeca o el pulgar, especialmente si se asocia a manipulaciones alrededor de la flexura del codo o tendinitis bicipital. La electromiografía es útil para confirmar el diagnóstico, descartar otros diagnósticos diferenciales y predecir el pronóstico. Conocer la localización de este nervio durante las manipulaciones en el brazo y colocar a los pacientes en una postura adecuada durante las cirugías puede ayudar a minimizar los casos.
The musculocutaneous nerve is a mixed nerve that originates from the lateral cord of the brachial plexus. In the arm it innervates the coracobrachialis, brachialis and biceps muscles, while at the level of the antecubital fossa of the elbow it becomes subcutaneous, becoming known as the lateral antebrachial cutaneous nerve (LACN), and provides sensory innervation to the anterolateral side of the forearm. Lesions of this nerve are rare, of varied aetiology, and are often under-diagnosed.1–3
ObjectiveTo describe the clinical and electrophysiological characteristics of patients with isolated lesions of the LACN.
Material and methodsRetrospective descriptive study of electromyography (EMG) performed at the Clinical Neurophysiology Service of the Hospital General Universitario de Castellón (HGUCS). Studies with NCAL lesions performed from January 2004 to December 2023 were included. Those with brachial plexus lesions or previous neurological disorders were excluded. We analysed the symptoms reported by the patient and the neurological examination by reviewing the electronic medical record, reviewing the findings in the EMG and the possible triggers. The study was conducted in accordance with the ethical standards recognized by the Declaration of Helsinki and resolution 008430 of 1993.
Sensory conduction of the NCAL was performed by stimulating the elbow flexure, slightly lateral to the biceps tendon and recording 12cm distal to the stimulus, in the anterolateral area of the forearm.1 The latency and amplitude of the NCAL were assessed, compared with the contralateral asymptomatic side. Asymmetries greater than 30% were considered pathological. Lesions were grouped into mild when the amplitude was decreased by less than 50%, moderate if the amplitude decrease was greater than 50% and severe when the potential was absent. In addition, sensory and motor conductions of other nerves in the same extremity were performed and the muscles dependent on the musculocutaneous nerve (C5–C6 territory) were evaluated.
ResultsEleven cases were identified (8 men and 3 women), with a mean age of 44 years (15–73) and referred mainly from traumatology (73%), neurology (18%) and haematology (9%). Only one patient was correctly referred. Four were referred as a possible radial nerve injury, one as cervical radiculopathy and in the rest there was no specific suspicion.
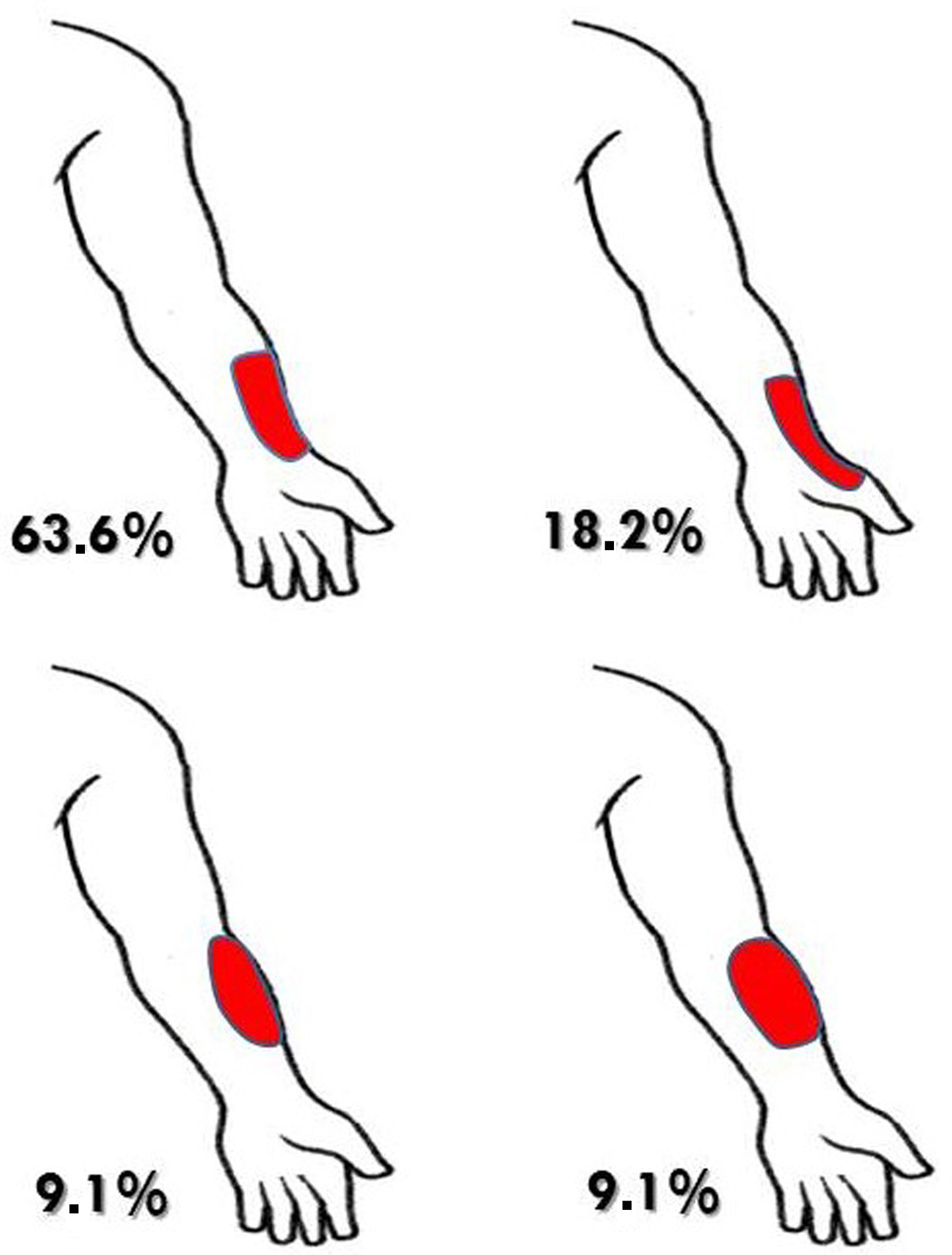
Clinically, all of them reported sensory alteration in some part of the forearm without weakness, but the majority (63.6% of cases) noticed the sensory alteration extended to the radial edge of the wrist and 18.2% to the thumb. The remaining 18.2% had sensory alteration restricted to the forearm (one patient on the lateral side and the other on the lateral and medial side) (Fig. 1). The EMG study was performed with a mean evolution time of 8 months (range 3–19 months), and showed moderate axonal degeneration in 8 patients (only one of them with altered latency) and severe degeneration in 3 patients. The rest of the nerve conductions and muscles examined in these patients were normal.
The symptoms observed in association with surgery in 4 cases were: re-anchoring of the distal biceps tendon using the Arthrex technique due to complete rupture of the tendon; osteosynthesis using 2 Kirschner wires for an olecranon fracture; osteosynthesis with a minimally invasive plate for a humeral shaft fracture, and surgical reduction using 2 Kirschner wires for an open, comminuted distal humerus fracture. Another 4 patients reported association with manipulation in the area (suture of a wound in the biceps; haematoma in the arm; blood donation, and venous puncture in the elbow flexure). The rest were associated with clinical symptoms of bicipital tendonitis (pain and limitation of elbow extension). An imaging study was performed in only one patient, at cervical level. Aetiological diagnosis was reached by the exclusion of other processes, through neurophysiological study and temporary association with the triggers reported by the patients. One patient was treated with rehabilitation (not specified in the clinical history), and no treatment was prescribed for the remaining patients. Three of the patients had a good clinical evolution, with improvement of the symptoms, all of them with moderate EMG involvement. Four of the patients had a poor clinical evolution, with persistence of sensory symptoms months later (3 of them with severe axonal involvement and one moderate). No information on evolution was available for the rest of the patients.
DiscussionIsolated involvement of the NCAL is a rare and probably under-diagnosed disorder. Symptoms may be confused or even overlap with plexopathies; radiculopathies; peripheral nerve compressions at different levels; epicondylitis; bicipital tendinitis or even other neurological conditions with which a differential diagnosis must be made.3 Less than 100 cases have been described in the literature.2,3 We present 11 cases objectified by EMG study in the last 20 years at the HGUCS in which only one was clinically suspected. Memon's group in the USA3 recently performed a retrospective review of 15 patients with isolated NCAL injury over 16 years. In most cases, the sensory alteration extended beyond the lateral portion of the forearm classically described in the literature, which probably influenced the difficulty of its recognition. This finding can be explained by a high prevalence of communications found between the NCAL nerve and the radial nerve. Variations have been described in which the NCAL, apart from innervating the territory of the superficial radial nerve, can even replace it. In anatomical studies, innervations of the back of the hand by the NCAL was observed in 39.8% of 93 cadavers and communications between both nerves in 71% of the forearms.4 In electrophysiological studies, this type of variation was found in 11% of the thumbs.5 The associated triggers in the cases observed in our hospital were mainly direct manipulations in the area, surgeries and bicipital tendonitis. Its close relationship with the cephalic vein and the bicipital tendon puts it at risk in these cases. These aetiologies have been described in the literature, along with others such as strenuous activity in the upper limbs, various throwing sports, tourniquet, reinsertion of the bicipital tendon, positioning during anaesthesia or even compression due to carrying heavy trays in waitresses.2,3,6,7
The patients described in the literature were treated in the acute phase with rest, non-steroidal anti-inflammatory drugs, local ice2 or pharmacological therapy for neuropathic pain.7 Steroid injections, ultrasound, transcutaneous electrical stimulation and even decompressive surgery for refractory cases have also been described.2 It is especially recommended to carry out adequate prevention of injuries by avoiding punctures in the lateral portion of the antecubital fossa, compressions with a blood pressure cuff and being careful with postures in the operating room. The American Society of Anaesthesiology recommends taking the patient's history to detect a predisposition to presenting with a peripheral nerve injury (diabetes, alcoholism, etc.), previously exploring the joint range and placing the limb in a neutral posture during surgery, with minimal shoulder extension, external rotation, abduction and slight flexion of the elbow with supination of the forearm and a neutral position of the wrist.8 Clinical evolution was favourable in most of our patients when the EMG showed moderate affectation, although all those with severe affectation had an unfavourable evolution, with persistence of symptoms months later.
ConclusionIsolated affectation of the NCAL is an uncommon and under-diagnosed alteration, probably due to the variability in the distribution of the sensory alteration reported by the patients and the similarity of the symptoms with other diseases. The diagnosis is clinical and it is important to consider it in patients with hypoaesthesia in the forearm, even in the radial border of the wrist or thumb, especially if it is related to manipulations around the elbow flexure or bicipital tendonitis. EMG is useful to confirm the diagnosis, rule out other differential diagnoses and predict the prognosis. Knowing the location of this nerve during manipulations, surgery on the arm and when placing patients in surgical positions can help to minimize cases.
Level of evidenceLevel of evidence iv.
Ethical considerationsThe study was conducted in accordance with the ethical standards recognized by the Declaration of Helsinki and resolution 008430 of 1993.
FundingThis research did not receive specific support from public sector agencies, commercial sector or non-profit entities.
Conflict of interestsThe authors have neither financial relationship nor conflict of interests to declare.