This study aimed to analyze factors of comorbidity in older patients with acetabular fracture to know the role of disease in the treatment of this population.
MethodsDesign: retrospective cohort study.
SettingSingle Level 2 Trauma Center.
Patient selection criteriaA prospective database of acetabular fractures in patients over 55 years between January 2011 and January 2021 was studied. The exclusion criteria were age, pathological fracture, associated pelvic or hip fracture, follow-up of less than one year, and not having a computed tomography.
Outcome measures and comparisonsPatients were categorised as low (0–2), intermediate (3–4) or high (≥5) risk according to the age-adjusted Charlson comorbidity index (ACCI). The primary outcomes were risk of complications, number of complications and mortality at one year according to the ACCI scale. The difference between the pre-fracture Clinical Frailty Scale (CFS) and the one-year follow-up was also analysed. Descriptive and multivariable regression analyses were performed and ROC curves were constructed.
ResultsA total of 119 patients with acetabular fracture were collected. Ninety-eight out of those met inclusion criteria for our study. In regard to ACCI groups, 22% were low-risk, 26% were intermediate-risk, and 52% were high-risk. Statistically significant differences were found according to age, sex, mechanism of injury, treatment type, surgical treatment type, Clinical Frailty Scale (CFS) score, readmissions, complications, and mortality. ROC curves showed an association between ACCI and CFS in terms of complications and mortality, with the exception of unadjusted Charlson comorbidity index. On the multivariable regression analysis, associations were found between ACCI and presence of complications (OR 1.37, 95% CI 1.06–1.77, p=0.015) and mortality (OR 1.32, 95% CI 1.04–1.67, p=0.025) and between CFS and complications (OR 2.01, 95% CI 1.30–3.11, p=0.001) and mortality (OR 1.59, 95% CI 1.08–2.35, p=0.019). No statistical correlation was established between ASA and complications or mortality.
ConclusionPresurgical ACCI and CFS scales may serve as a risk assessment method in treatment decision-making for patients with acetabular fracture. An association is observed between patients with a pre-fracture ACCI score ≥5 (high-risk) and a pre-fracture CFS score >4 (mild frailty) and mortality and complications at one year.
Analizar los factores de comorbilidad en pacientes con fractura acetabular y edad superior a 55 años. Estudiar su influencia en la decisión terapéutica de esta población.
MetodologíaSe ha realizado un estudio retrospectivo de una base de datos prospectiva sobre fracturas acetabulares en pacientes de más de 55 años entre enero 2011 y enero 2021. Los criterios de exclusión fueron la edad, las fracturas patológicas, las fracturas asociadas con afectación de pelvis y cadera, pérdida de seguimiento y no tener realizada una tomografía computadorizada en el ingreso. Se clasificaron según el Índice de Comorbilidad de Charlson ajustado a Edad (age-adjusted Charlson comorbidity index (ACCI) en grupo de bajo riesgo (0-2), riesgo intermedio (3-4) y alto riesgo (≥5). Se evaluaron la tasa de complicaciones y la mortalidad en el primer año según cada grupo de riesgo y el detrimento funcional en cada grupo según el estado previo a la fractura (Clinical Frailty Scale pre fractura, CFS) y tras 1 año de seguimiento. Se realizó un análisis descriptivo, un análisis de regresión multivariable y se elaboraron curvas ROC.
ResultadosDe un total de 119 pacientes con fractura acetabular y edad superior a 55 años, 98 cumplieron criterio de inclusión. Los grupos obtenidos eran un 22% de bajo riesgo, un 26% de riesgo intermedio y un 52% de alto riesgo. Se observaron diferencias estadísticamente significativas en relación a la edad, sexo, mecanismo de lesión, tipo de tratamiento, tipo de técnica quirúrgica, Clinical Frailty Scale prequirúrgico, reingresos, complicaciones y mortalidad. Las curvas ROC muestran una asociación entre ACCI y CFS en términos de complicaciones y mortalidad, sin observar una correlación con el índice de Charlson no ajustado a edad. En el análisis de regresión multivariable, se encontró una asociación entre ACCI y la presencia de complicaciones (OR 1.37, 95%CI 1.06-1.77, p=0.015) y mortalidad (OR 1.32, 95%CI 1.04-1.67, p=0.025). También se encontró una asociación entre CFS y las compliaciones (OR 2.01, 95%CI 1.30-3.11, p=0.002) y mortalidad (OR 1.59, 95%CI 1.08-2.35, p=0.019). No se observó una relación estadística entre ASA y complicaciones/mortalidad.
ConclusiónLas escalas prequirúrgicas ACCI y CFS pueden servir como una herramienta que permita la toma de decisions en el tratamiento de pacientes con fractura acetabular y edad avanzada. Una asociación es observada entre pacientes con un valor de ACCI ≥5 (alto riesgo) y un estado functional previo a la caída (CFS prefracrura) >4 (fragilidad moderada) respecto a complicaciones y mortalidad al año.
Acetabular fractures in older adults are increasing worldwide due to, among other reasons, population aging; this increase has spurred research on them.1–3 This injury is more severe in older adults than in younger ones, due to associated comorbidities and fracture pattern.4 There is no clear consensus5 or clinical guidelines on the best treatment for each patient. Similarly, the influence of comorbidity on decision-making in these patients has not been investigated.
The definition of an older adult varies widely in the literature. A chronological definition is generally used, but it ranges from 50 to 80 years of age.4–7 Considering these discrepancies, establishing an age threshold for defining an older adult is not sufficient and other variables such as comorbidity should be weighed as well.
There are many scales for stratifying comorbidity.8,9 The Charlson comorbidity index (CCI)10 is universally accepted and establishes life expectancy at one month, three months, one year, and ten years based on the patient's comorbidity. The CCI consists of 19 items whose sum determines a survival score. It has been successfully used in studies on cancer,11 elective surgery,12 fractures,10 and more recently on arthroplasty.13 Charlson et al.,14 upon revising their scale, observed an increase in the risk of mortality with each additional decade of life. This led to a modification by some other authors: the age-adjusted Charlson comorbidity index (ACCI), which yields better predictions than the CCI.10,15,16
Frailty is described as an increase in individual vulnerability, mortality or dependency when exposed to a stressor. Therefore, assessment of frailty is necessary for all patients, especially the most vulnerable. At present, use of the Clinical Frailty Scale (CFS)17–19 to evaluate frailty in older adults is becoming more common. It not only analyzes comorbidity, but also physical disability and cognitive impairment. The CFS evaluate specific disciplines to generate a frailty score ranging from 1 (very fit) to 9 (terminally ill). This scale has demonstrated excellent predictive results on mortality and institutionalization, and was more useful than the frailty index, another instrument for measuring frailty, according to the Canadian Study of Health and Aging (CSHA).18
In previous studies some authors have not observed a relationship between comorbidity prior to a fracture, complications, and mortality1,20,21 whereas others describe complications and the mortality rate without analyzing prior comorbidity.22–25 There are no studies which examine comorbidity as a method of treatment stratification in acetabular fracture in older adults. This paper aims to assess whether the ACCI would allow for establishing risk groups in older adult patients with acetabular fracture. This research analyses the relation of comorbidity in patients over 55 years of age with acetabular fracture. In addition, it evaluates the risk of complications and mortality at one year follow-up according to the ACCI and CFS scales.
Materials and methodsThis study was conducted based on a database which included patients attended between January 2011 and January 2021. The project was approved by the Ethics Committee and Research Unit of our Institution on the 29th of September of 2022. The study was conducted according to the Declaration of Helsinki and STROBE cohort guidelines. Patients were identified by means of the International Classification of Diseases (ICD) 9–10 diagnoses of pelvic fracture (ICD 9: 808/ICD 10: S32.8) and acetabular fracture (ICD 9: 808.0/ICD 10: S32.4). Data were collected using the HP Doctor® program (Hewlett Packard, Palo Alto, CA, USA, 2010). Images were viewed through the PACS (Picture Archiving and Communication System) Carestream (Health Spain, S.A. 2016) system.
The inclusion criteria included diagnosis of acetabular fracture, age ≥55 years, and a minimum follow-up time of one year. The exclusion criteria were age <55 years, pathological fracture, associated pelvic or hip fracture, follow-up of less than one year, and not having a computed tomography (CT) scan prior to the decision regarding treatment. The age cut-off point was established following the literature,5,21,26 with 55 years being the lowest age recorded. Treatment decisions were based on health status and an evaluation by the Orthopaedic Trauma, Anesthesiology, and Internal Medicine Departments.3
Non-operative treatment consisted of 8 weeks of non-weight bearing on the injured side with active-passive assisted range of motion exercises, followed by partial weight bearing with assistance and physiotherapy for 4–6 weeks. Variability in surgical technique depended on injury factors such as fracture pattern and associated injuries and treatment factor such as treatment timing and surgeon preference. The ilioinguinal approach was used for wall and anterior column fractures. The Kocher–Langenbeck approach was used for wall or posterior column fracture. If both columns were involved, a combined approach was used.
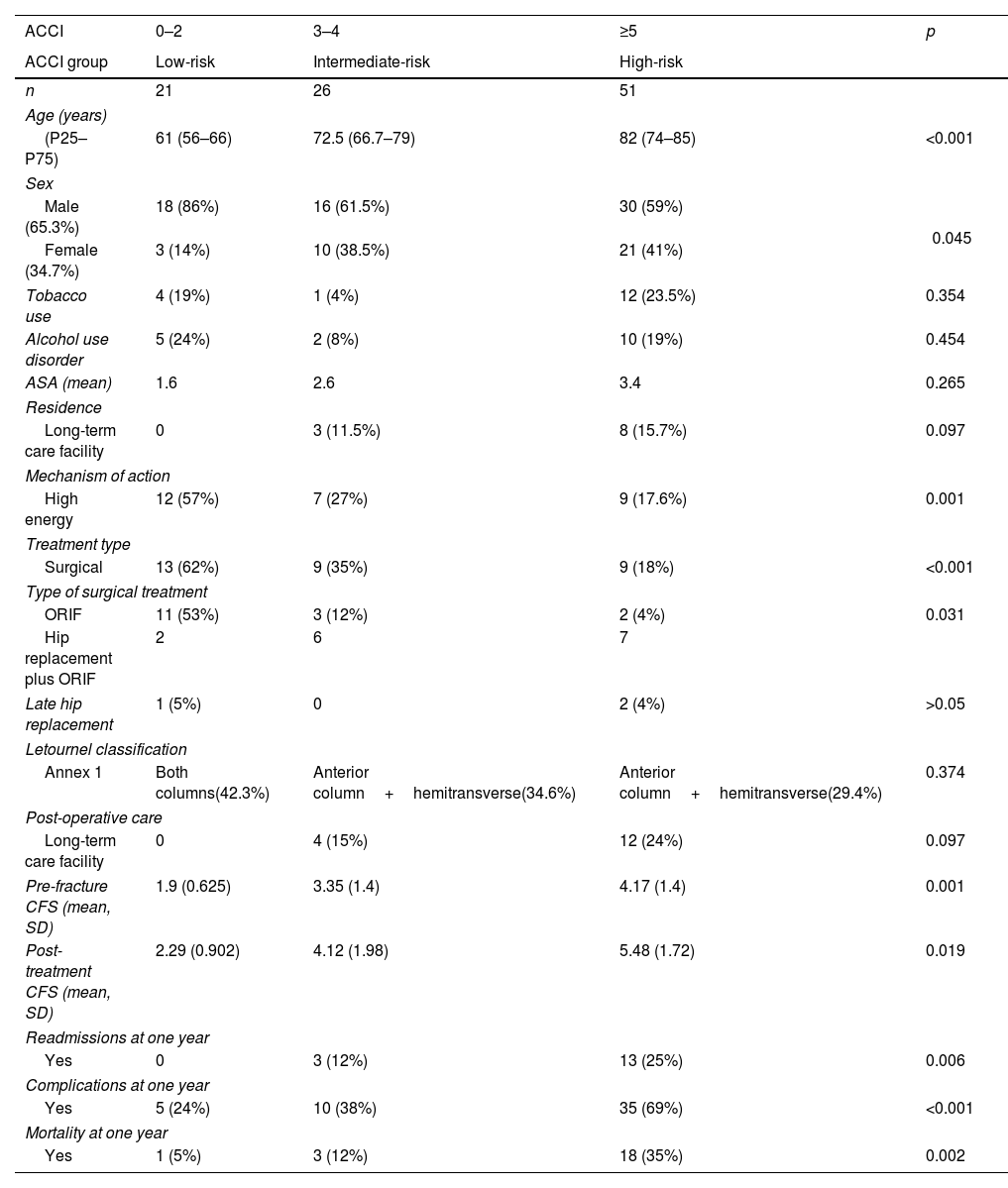
The variables analyzed were age, sex, tobacco use, alcohol use, American Society of Anesthesiologists’ Physical (ASA), adjusted Charlson comorbidity index (ACCI), Clinical Frailty Scale (CFS), residence (home, long-term care facility), mechanism of action (low or high energy), treatment type (surgical or non-operative), surgical treatment (open reduction and internal fixation (ORIF), ORIF plus hip replacement) and post-operative care (home, long-term care facility, acute care hospital). Fractures were classified by the operating surgeons according to Letournel–Judet classification. Clinical endpoints at 1 year were early or late complications and the need for secondary reconstructive procedures. Information on complications was detailed in terms of emergency or readmission episodes. These variables are shown in Table 1 and supplemental file. The supplementary file contains the Letournel classification stratified according to ACCI groups, the number and type of complications per year according to ACCI groups.
Sociodemographic and clinical variables according to risk groups. The percentages of categorical variables have been calculated according to the different groups of ACCI.
| ACCI | 0–2 | 3–4 | ≥5 | p |
|---|---|---|---|---|
| ACCI group | Low-risk | Intermediate-risk | High-risk | |
| n | 21 | 26 | 51 | |
| Age (years) | ||||
| (P25–P75) | 61 (56–66) | 72.5 (66.7–79) | 82 (74–85) | <0.001 |
| Sex | ||||
| Male (65.3%) | 18 (86%) | 16 (61.5%) | 30 (59%) | 0.045 |
| Female (34.7%) | 3 (14%) | 10 (38.5%) | 21 (41%) | |
| Tobacco use | 4 (19%) | 1 (4%) | 12 (23.5%) | 0.354 |
| Alcohol use disorder | 5 (24%) | 2 (8%) | 10 (19%) | 0.454 |
| ASA (mean) | 1.6 | 2.6 | 3.4 | 0.265 |
| Residence | ||||
| Long-term care facility | 0 | 3 (11.5%) | 8 (15.7%) | 0.097 |
| Mechanism of action | ||||
| High energy | 12 (57%) | 7 (27%) | 9 (17.6%) | 0.001 |
| Treatment type | ||||
| Surgical | 13 (62%) | 9 (35%) | 9 (18%) | <0.001 |
| Type of surgical treatment | ||||
| ORIF | 11 (53%) | 3 (12%) | 2 (4%) | 0.031 |
| Hip replacement plus ORIF | 2 | 6 | 7 | |
| Late hip replacement | 1 (5%) | 0 | 2 (4%) | >0.05 |
| Letournel classification | ||||
| Annex 1 | Both columns(42.3%) | Anterior column+hemitransverse(34.6%) | Anterior column+hemitransverse(29.4%) | 0.374 |
| Post-operative care | ||||
| Long-term care facility | 0 | 4 (15%) | 12 (24%) | 0.097 |
| Pre-fracture CFS (mean, SD) | 1.9 (0.625) | 3.35 (1.4) | 4.17 (1.4) | 0.001 |
| Post-treatment CFS (mean, SD) | 2.29 (0.902) | 4.12 (1.98) | 5.48 (1.72) | 0.019 |
| Readmissions at one year | ||||
| Yes | 0 | 3 (12%) | 13 (25%) | 0.006 |
| Complications at one year | ||||
| Yes | 5 (24%) | 10 (38%) | 35 (69%) | <0.001 |
| Mortality at one year | ||||
| Yes | 1 (5%) | 3 (12%) | 18 (35%) | 0.002 |
ACCI: age-adjusted Charlson comorbidity index; CFS: Clinical Frailty Scale; SD: standard deviation; ORIF: open reduction and internal fixation.
The ACCI, ASA and CFS were calculated according to medical records. Patients were grouped according to ACCI score as low-risk (0–2), intermediate-risk (3–4), and high-risk (≥5).11,13 The CFS was measured after the fracture and at a follow-up of one year.
The statistical analysis was conducted using the SPSS® program (IBM® v 28). ACCI groups (low, intermediate, or high-risk) were compared using the chi-square test for linear trends for qualitative variables and the Kruskal–Wallis test for quantitative variables. A general linear model was used to evaluate the patient's CFS before the fracture and at one year of follow-up after the fracture according to the three ACCI groups. Receiver operating characteristic (ROC) curves were calculated to evaluate the prognostic performance of CFS and ACCI regarding the presence of complications and annual mortality as well as the area under the ROC curve (AUROC). Goodness-of-fit was determined using the Hosmer–Lemeshow test and Nagelkerke's R2. Simple logistic regression models were built with the aforementioned variables, selecting independent variables adjusted in the equation through a forward stepwise regression method. The odds ratio (OR) and 95% confidence intervals were calculated. A multivariate regression model was created by selecting significant variables. Statistical significance was defined as p<0.05.
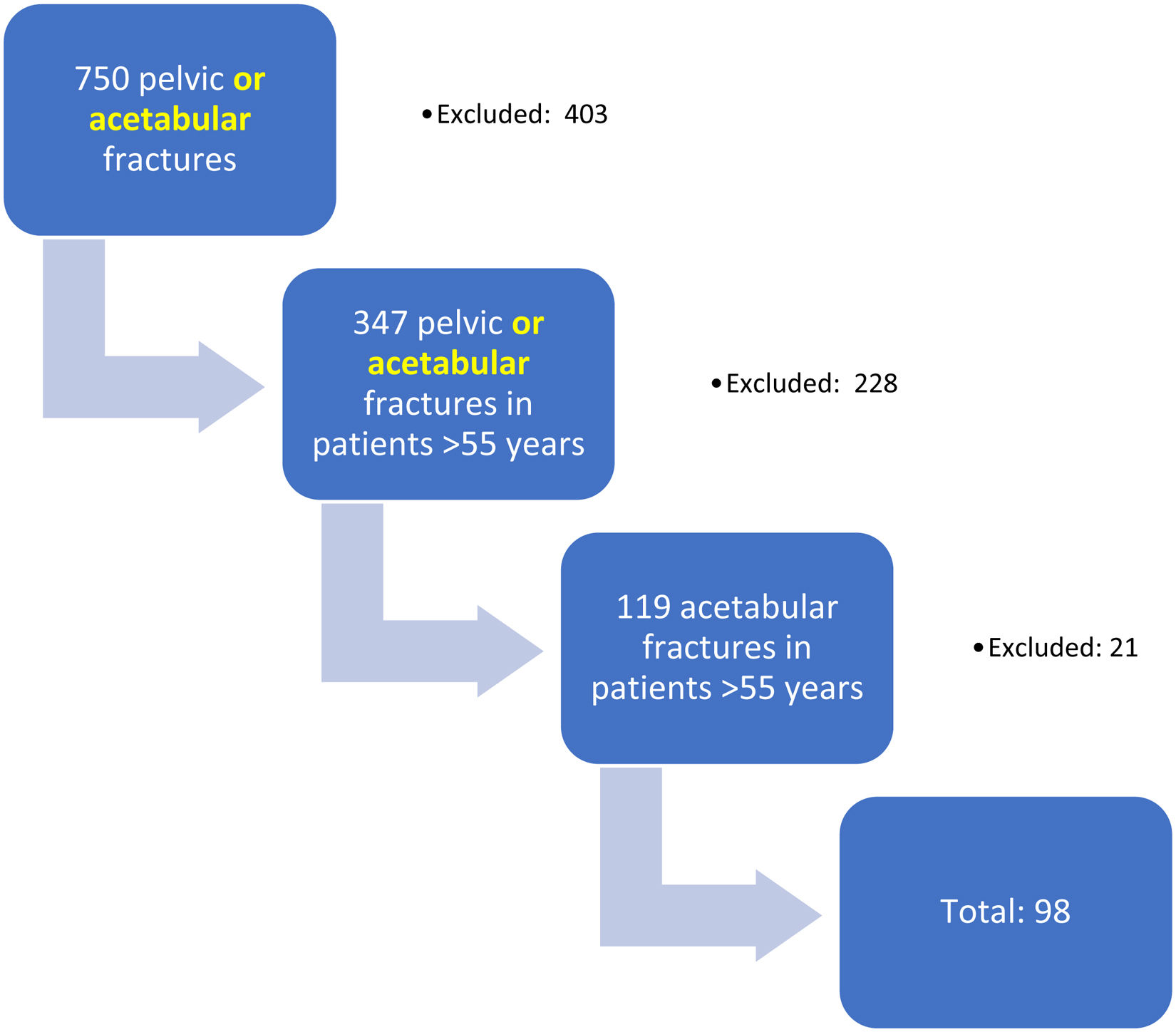
ResultsA total of 750 pelvic and acetabular fractures were recorded during the study period. Out of them, there were 119 acetabular fractures in patients older than 55 years without an associated pelvic fracture. Twenty-one (17%) patients out of these 119 with acetabular fractures were excluded: four for not having a CT scan available and 17 due to loss of follow-up. Ninety-eight patients were finally included in the study (Fig. 1). The variables and their results are shown in Table 1 and supplemental file.
The majority of the patients were male (65.3%) and age is already included as one of the ACCI variables. ASA value increased by risk group. Residence in a long-term care facility was more common in the high-risk group (15.7%). The high-energy mechanism of action was higher in the low-risk group. Low-risk group was treated with ORIF (82%), whereas intermediate and high-risk groups were managed non-operatively (62%). Intermediate and high-risk group managed surgically, the technique was ORIF plus hip replacement. In intermediate and high-risk groups, anterior column plus posterior hemitransverse fracture made up the majority of all fractures (34% and 29%, respectively). In low-risk group, both column was significantly more frequent (42%). The rates of complications, readmissions and mortality were higher in the high-risk group.
The three ACCI risk groups were found to have statistically significant differences in age (p<0.001), sex (p=0.045), mechanism of injury (p=0.001), conservative or surgical treatment (p<0.001), type of surgical treatment (p=0.031), CFS (p=0.001), readmission (p=0.006), complications (p<0.001), and mortality (p=0.002) (Table 1).
After one year of follow-up, three patients (3.1%, one with ACCI 0–2 and two with ACCI >5) treated non-operatively required a total hip arthroplasty. There were no reinterventions in patients treated surgically with ORIF, as they were in the younger age group (p=0.031). Twenty-two patients (22%) died within one year of follow-up (Table 1).
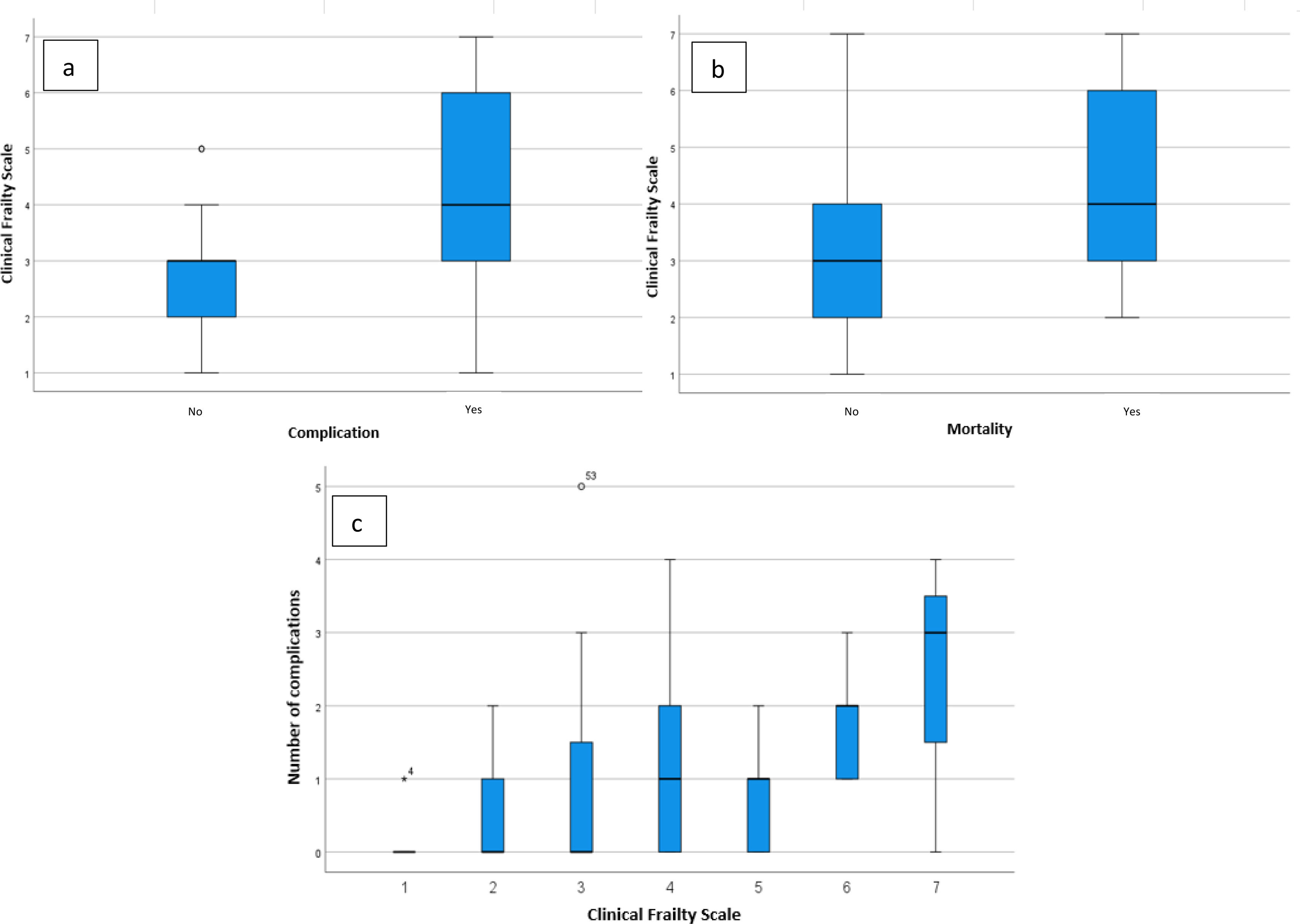
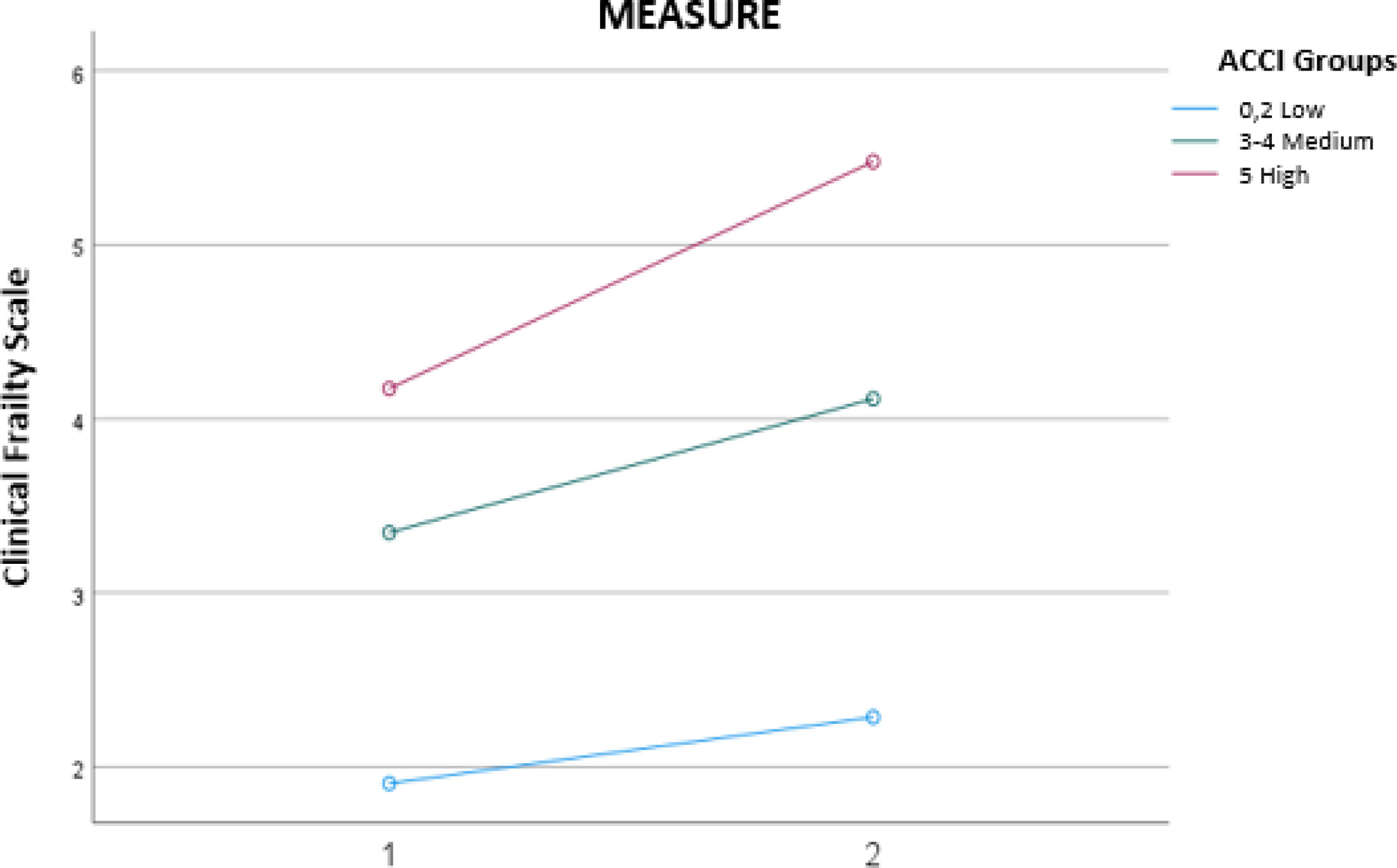
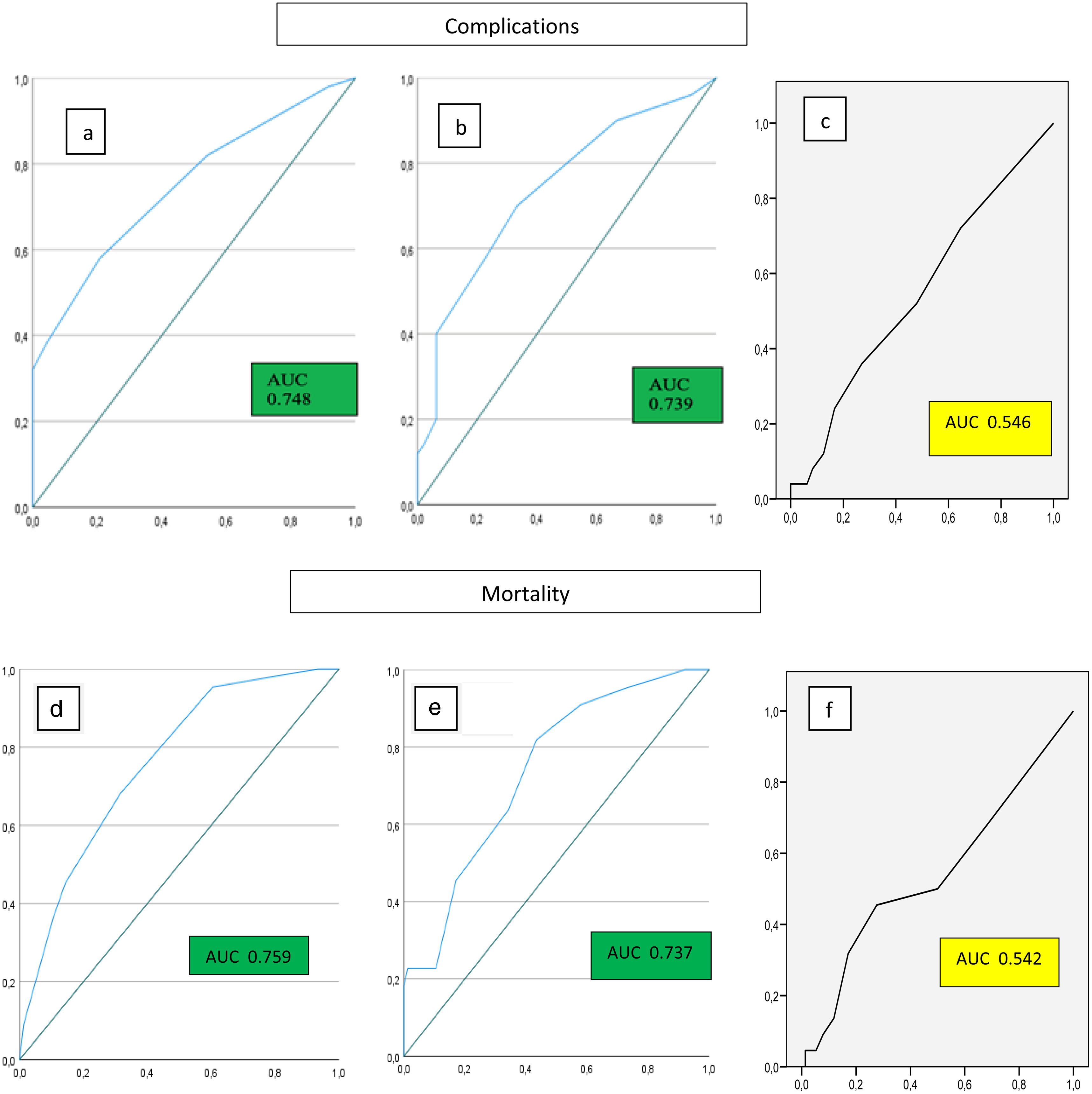
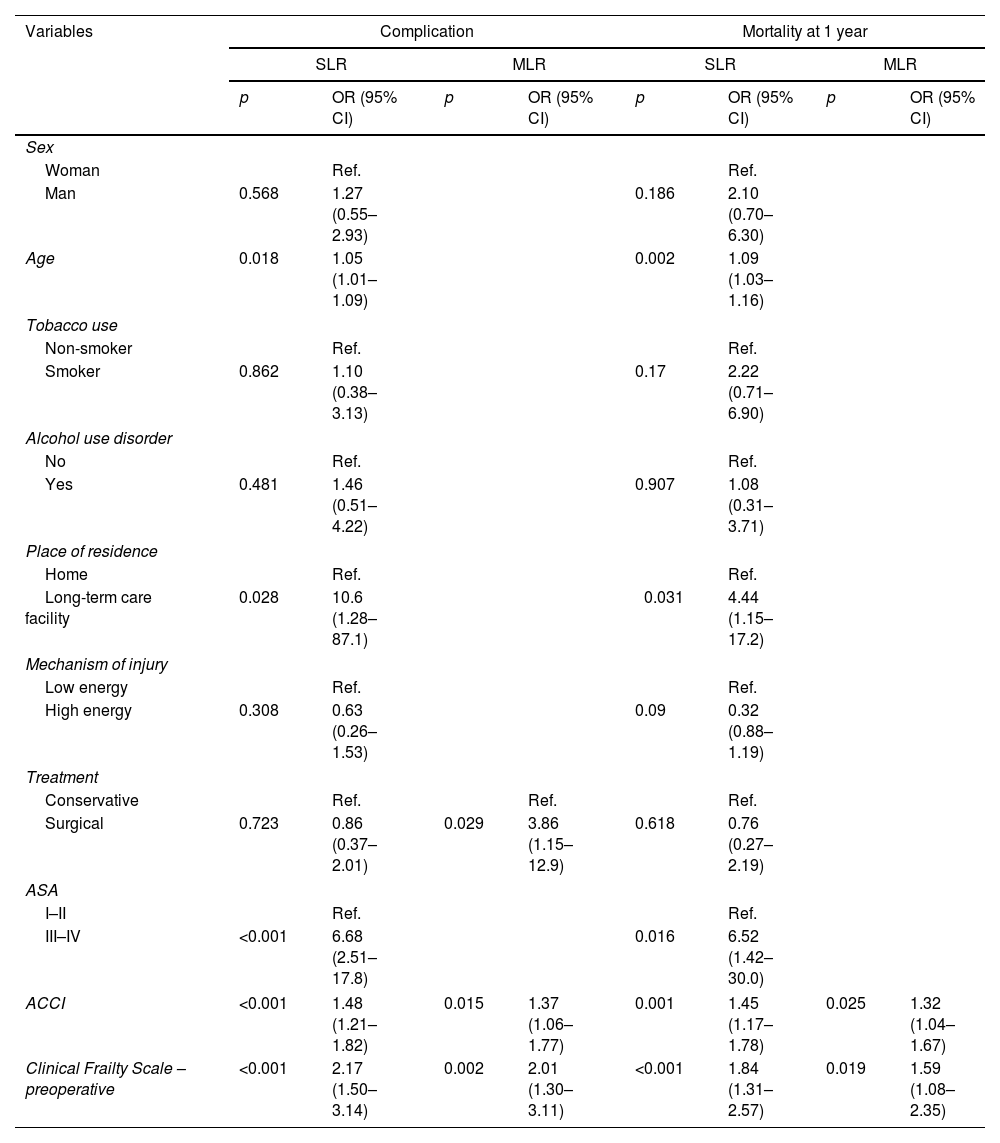
A one-point increase in the pre-fracture ACCI entailed an increase in the risk of complications by OR 1.37 (95% CI 1.06–1.77, p=0.015) and an increase in the risk of mortality by OR 1.32 (95% CI 1.04–1.67, p=0.025) (Table 2). Regarding CFS, a one-level increase entailed a greater risk of complications with an OR of 2.01 (95% CI 1.3–3.11, p<0.001) and a greater risk of mortality with an OR of 1.59 (95% CI 1.08–2.35, p=0.019) (Table 2). The CFS cut-off point for complications was 4 (mildly frail) (Fig. 2a–c). Likewise, there were differences in the mean CFS before the fracture (p=0.001) and at one year of follow-up (p=0.019), with outcomes becoming worse as the ACCI risk group increased (Fig. 3). On the ROC curve analysis, a correlation was observed between ACCI and CFS with complications and mortality (AUC >0.7), apart from unadjusted Charlson comorbidity index (Fig. 4).
Crude and multivariable logistic regression with outcome variables of complications and mortality at one year.
| Variables | Complication | Mortality at 1 year | ||||||
|---|---|---|---|---|---|---|---|---|
| SLR | MLR | SLR | MLR | |||||
| p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | |
| Sex | ||||||||
| Woman | Ref. | Ref. | ||||||
| Man | 0.568 | 1.27 (0.55–2.93) | 0.186 | 2.10 (0.70–6.30) | ||||
| Age | 0.018 | 1.05 (1.01–1.09) | 0.002 | 1.09 (1.03–1.16) | ||||
| Tobacco use | ||||||||
| Non-smoker | Ref. | Ref. | ||||||
| Smoker | 0.862 | 1.10 (0.38–3.13) | 0.17 | 2.22 (0.71–6.90) | ||||
| Alcohol use disorder | ||||||||
| No | Ref. | Ref. | ||||||
| Yes | 0.481 | 1.46 (0.51–4.22) | 0.907 | 1.08 (0.31–3.71) | ||||
| Place of residence | ||||||||
| Home | Ref. | Ref. | ||||||
| Long-term care facility | 0.028 | 10.6 (1.28–87.1) | 0.031 | 4.44 (1.15–17.2) | ||||
| Mechanism of injury | ||||||||
| Low energy | Ref. | Ref. | ||||||
| High energy | 0.308 | 0.63 (0.26–1.53) | 0.09 | 0.32 (0.88–1.19) | ||||
| Treatment | ||||||||
| Conservative | Ref. | Ref. | Ref. | |||||
| Surgical | 0.723 | 0.86 (0.37–2.01) | 0.029 | 3.86 (1.15–12.9) | 0.618 | 0.76 (0.27–2.19) | ||
| ASA | ||||||||
| I–II | Ref. | Ref. | ||||||
| III–IV | <0.001 | 6.68 (2.51–17.8) | 0.016 | 6.52 (1.42–30.0) | ||||
| ACCI | <0.001 | 1.48 (1.21–1.82) | 0.015 | 1.37 (1.06–1.77) | 0.001 | 1.45 (1.17–1.78) | 0.025 | 1.32 (1.04–1.67) |
| Clinical Frailty Scale – preoperative | <0.001 | 2.17 (1.50–3.14) | 0.002 | 2.01 (1.30–3.11) | <0.001 | 1.84 (1.31–2.57) | 0.019 | 1.59 (1.08–2.35) |
SLR: simple logistic regression; MLR: multivariable logistic regression; ASA: American Society of Anesthesiologists; ACCI: age-adjusted Charlson comorbidity index.
ROC curves of the prognostic performance for complications (a and b), according to ACCI (a), CFS (b) and unadjusted Charlson comorbidity index (c). And ROC curves performance for mortality, according to ACCI (d), CFS (e) and unadjusted Charlson comorbidity index (f). ACCI: age-adjusted Charlson comorbidity index; CFS: Clinical Frailty Scale.
Although significant differences were observed in several mortality and complications variables on the simple logistic regression (crude analysis), on the adjusted multiple logistic regression analysis, only ACCI and CFS showed a significant association. The Hosmer–Lemeshow test (0.441) and Nagelkerke's R2 (0.29) indicate an acceptable calibration and goodness-of-fit. Age is already included as one of the ACCI variables. There was no significant association with either residing in a long-term care facility or ASA scores (Table 2). Surgical treatment entails a greater risk of complications with an OR of 3.86 (95% CI 1.15–12.9, p=0.029). However, this should be subject to criticism as there are statistically significant differences between the groups in terms of the type of treatment.
DiscussionAge, functional status prior to the fracture, and comorbidity are factors that must be taken into account when deciding on individualized treatment in patients older than 55 years with an acetabular fracture.2,3,5,27–30 Given that there is no consensus5 or clinical guidelines that establish the best individualized treatment for patients with fractures, new researches that stratifies them into risk groups are needed.
In this study, significant differences were observed between ACCI risk groups14 and the effectiveness of ACCI and CFS as risk classification methods for complications and mortality, represented on the ROC curve (AUC >7). Neuhaus et al.10 obtained similar results to those shown in our paper but in patients with hip fractures. They concluded that ACCI is a predictor of mortality, though it should be evaluated together with concomitant injuries. Harrison et al.,31 studying older patients sustaining pelvic or acetabular fractures, observed statistically significant differences between mortality and CCI, prior mobility status, and age.
The CFS allows for evaluating mobility and dependency, which are variables related to frailty. Church et al.19 describe the widespread use of the CFS in the literature and the association between the CFS and clinical outcomes in the care of older adult patients. In this regard, Romero-Ortuno et al.32 used this scale as a method for selecting older adult patients with various diagnoses who require greater care. In our study, a significant association was observed between preoperative CFS and the presence of complications and mortality at one year follow-up (Fig. 2). Likewise, a greater absolute increase in CFS score calculated before the fracture and after treatment was found in the high-risk ACCI group (Fig. 3).
Ernstberger et al.33 determined that the most frequent fractures in older adults, namely anterior column plus posterior hemitransverse fracture, tend to present little displacement, which makes them more likely to be treated non-operatively. We have found that patients in the low-risk group (ACCI 0–2) most commonly presented with a fracture of the two columns compared to the medium- and high-risk groups (ACCI >2), which generally presented with an anterior column plus posterior hemitransverse fracture and were also predominantly treated non-operatively. Nonetheless, some authors currently include them for surgical treatment.34 In this regard, the multivariable analysis conducted in our study showed a higher risk of complications in patients treated surgically. However, no conclusions can be drawn from these results because the type of treatment was different in each risk group. Surgical treatment was more frequent in the low-risk group (62%) and less frequent in the intermediate- and high-risk groups (35% and 18%, respectively), and this difference was statistically significant p<0.001. Therefore, further research is needed to analyze the type of treatment by risk group.
Despite the fact that the ASA classification is cited in nearly all publications,2,5,26–28,35 it was originally designed to evaluate anesthetic risk prior to surgery; indeed, frailty scoring systems are more precise in regard to complications and mortality.36 Kim et al.37 observed a lower degree of precision in the prediction of annual mortality using the ASA classification compared to a frailty evaluation system (multidimensional frailty score model). We found that the ASA classification had no statistical association with complications and mortality at one year follow-up on a multiple regression model (Table 2).
Surprisingly, no significant differences were found in the literature regarding how early the surgical intervention was performed (48–72h),20,29 unlike what has been described in proximal and distal femur fractures.38 In our research we have observed surgeries were performed after 72h.
In regard to the mechanism of injury, except for Gary et al.,29 who found that a high-energy mechanism of injury in older adults was a predictive factor of mortality, other authors20,39 have not observed differences between a low or high-energy mechanism. Furthermore, Kehoe et al.40 described that in older adult patients with acetabular fracture, those between 50 and 70 years of age with a fall of less than <2m tended to be categorized as having major trauma (injury severity score >15). Heimke et al.39 observed that younger patients within this age group (60–65 years) with a high-energy mechanism of injury who were treated with internal fixation, had better functional outcomes at one year, but they did not observe differences in complications or mortality compared to older patients (>70 years). In our study, we have observed that a high-energy mechanism of injury was more frequent in the low-risk group (ACCI 0–2) and a low energy mechanism in the rest (ACCI >2), findings which were statistically significant. Nonetheless, the mechanism of injury was not found to be a predictive factor of either complications or mortality (Table 2).
A medical history of smoking or alcohol abuse disorders tends to lead to an increase in comorbidity.39,41 However, the paucity of results in the literature and the heterogeneity of these findings may be due to a lack of stratification of the variables. We have found that smoking or alcohol abuse disorders were more prevalent in the high-risk group, though not statistically significant (Table 1).
It has been published that residing in a long-term care facility has been associated with increased mortality among older adults with hip fracture,42 though this factor has not been widely studied in acetabular fracture. In our study, more patients in the high-risk group lived in long-term care facilities, though this finding was not statistically significant (Table 1).
Our study has several limitations. This study is retrospective in nature and sample size of each group should have exceeded 30 patients in order to have the statistical power for a comparative study between risk groups. However, statistically significant associations were found between comorbidity scales and complications and mortality. Although a larger sample size would be desirable, this single-center registry had a loss to follow-up of just 14% (17 patients) and, unlike large registries, recorded specific data on comorbidity.1 Secondly, patients’ baseline nutritional status or sarcopenia status were not included.30 Thirdly, although preoperative and post-operative ambulation status has been recorded, other functional outcomes were not described either.
ConclusionsThe use of the preoperative ACCI score to stratify older adult patients with acetabular fracture into risk groups could serve as a risk assessment method for therapeutic decision-making, as it shows a direct correlation with complications/mortality. In addition, the previous functional status (CFS) of these patients showed a statistically significant association with complications and mortality. No association was observed between ASA classification and complications and mortality, questioning the usefulness of ASA in classifying comorbidities in older adult patients with acetabular fractures. A pre-fracture ACCI score ≥5 (high-risk) and a pre-fracture CFS score >4 (low fragility) imply an exponential increase in risk that should be taken into account when making therapeutic decisions. Determining which type of treatment is most appropriate for each comorbidity requires future research.
Level of evidencePrognostic. Level III. Retrospective cohort study.
FundingThe author(s) received no financial or material support for the research, authorship, and/or publication of this article.
Conflicts of interestNone declared.