Systematic review and meta-analysis.
ObjectiveTo compare early (<24h) versus late (>24h) spinal cord decompression on neurological recovery in patients with acute spinal cord injury.
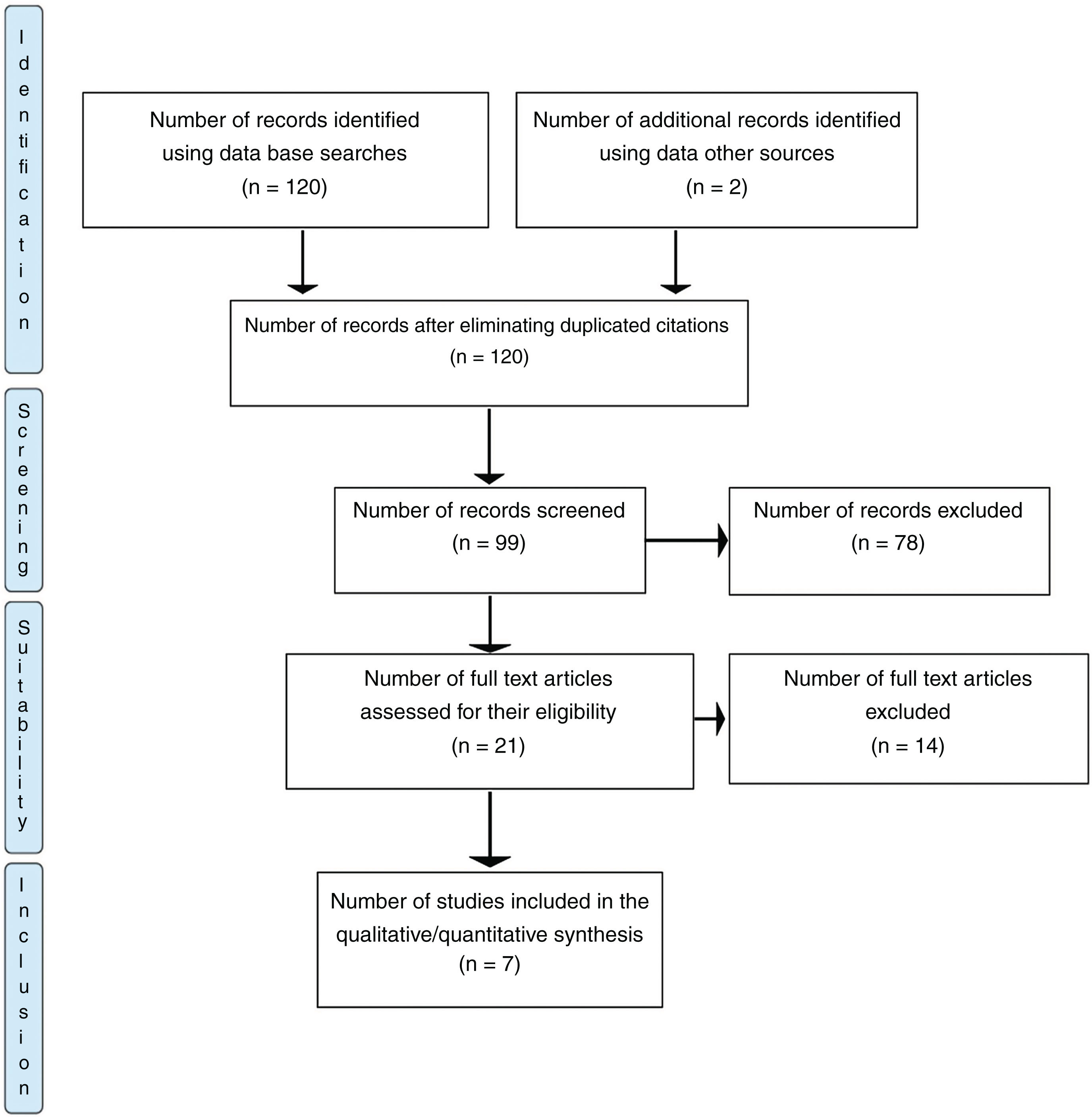
MethodsA systematic review was performed according to the PRISMA protocol to identify studies published up to December 2022.
Prospective cohort studies and controlled trials comparing early versus delayed decompression on neurological recovery were included. Variables included number of patients, level of injury, treatment time, ASIA grade, neurological recovery, use of corticosteroids, and complications. For the meta-analysis, the “forest plot” graph was developed. The risk of bias of the included studies was assessed using the ROBINS-I22 and Rob223 tools.
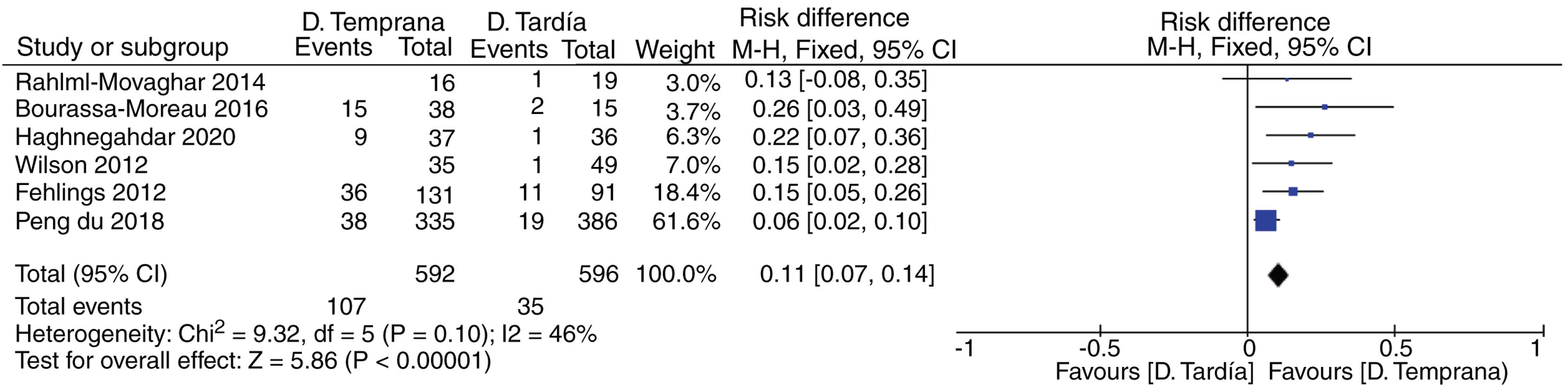
ResultsSix of the seven studies selected for our review were included in the meta-analysis, with a total of 1188 patients (592 patients in the early decompression group and 596 in the delayed decompression group), the mean follow-up was 8 months, in 5 studies used methylprednisolone, the most reported complications were thromboembolic cardiopulmonary events.
Five studies showed significant differences in favour of early decompression (risk difference 0.10, 95% confidence interval 0.07–0.14, heterogeneity 46%). The benefit was greatest in cervical and incomplete injuries.
ConclusionThere is scientific evidence to recommend early decompression in the first 24h after traumatic spinal cord injury, as it improves final neurological recovery, and it should be recommended whenever the patient and hospital conditions allow it to be safely done.
Revisión sistemática y metaanálisis.
ObjetivoComparar descompresión medular precoz (<24h) versus tardía (>24h) en la recuperación neurológica de pacientes con lesión medular aguda.
MétodosSe realizó una revisión sistemática según el protocolo de PRISMA para identificar estudios publicados hasta diciembre de 2022.
Se incluyeron solo estudios de cohorte prospectivos y ensayos controlados que comparan la descompresión precoz versus tardía en la recuperación neurológica. Como variables se incluyeron el número de pacientes, el nivel lesionado, el tiempo de tratamiento, el grado de ASIA, la recuperación neurológica, el uso de corticoesteroides y las complicaciones. Para el metaanálisis se desarrolló el gráfico «forest plot». El riesgo de sesgo de los estudios incluidos se evaluó utilizando la herramienta ROBINS-I22 y Rob223.
ResultadosSeis de los 7 estudios seleccionados para nuestra revisión fueron incluidos en el metaanálisis, con un total de 1.188 pacientes (592 pacientes en el grupo de descompresión precoz y 596 en el grupo de descompresión tardía), el promedio de seguimiento fue de 8 meses, en 5 estudios utilizaron metilprednisolona, las complicaciones mayormente reportadas fueron los eventos cardiopulmonares tromboembólicos.
Cinco estudios mostraron diferencias significativas a favor de la descompresión precoz (diferencia de riesgo: 0,10; intervalo de confianza del 95%: 0,07-0,14 y heterogeneidad: 46%). El beneficio fue mayor en las lesiones cervicales e incompletas.
ConclusionesExiste evidencia científica para recomendar la descompresión precoz en las primeras 24h tras la lesión medular traumática al mejorar la recuperación neurológica final, y debe recomendarse siempre que las condiciones del paciente y el hospital permitan hacerlo con seguridad.
The rate of traumatic spinal cord injury in developed countries has remained stable during the last decade at 26.5 cases per 1,000,000 inhabitants.1
In Spain traffic accidents are the most common cause, with significant increase in cervical spinal cord injuries caused by minimal trauma in advanced aged patients. Men continue to be the most affected and account for 75% of total patients.2
There is increasing tendency to perform early decompression and stabilisation of the spine and spinal cord, since this is a safe procedure which reduces mortality, spinal cord-associated complications and days of hospital admission.3 Despite this, in Spain, only 28% of patients undergo surgery during the first 24h after injury, with major variability between services and hospitals.2
Controversy exists as to whether early decompression is associated with a neurological improvement. Some studies suggest that early decompression would be more effective in terms of neurological recovery. However, this is also impacted by the affected region (cervical, thoracic) and by the level of injury (incomplete, complete).4 Due to ethical and legal problems, it is very difficult to conduct quality randomised studies on the emergency or non-emergency treatment of these injuries. The few, existing, well-designed studies, and those conducted with animals, suggest that early decompression is associated with an improvement in the neurological result.5
In general, and by consensus, “early decompression” has been defined as that which takes place during the first 24h after a spinal cord injury,6 although some authors speak of greater effectiveness in “ultra early” decompression within the first 8h. However, this is very difficult to achieve in standard clinical practice.7,8
The aim of our study was to assess the efficacy of early spinal cord decompression (under 24h) versus late decompression (over 24h) in the neurological recovery of adult patients with acute traumatic spinal cord injury.
MethodsA systematic review of the medical literature was performed according to the PRISMA protocol, with a search of the Medline (Pubmed), EMBASE, Cochrane library and Google Scholar databases to identify studies on the subject, published up until December 2022.
The following terms were used for the search: “spinal cord injury” combined with others such as “early surgery”, “late surgery”, “American spinal injury association impairment”, with synonyms and filters in the previous mentioned search engines (see additional material).
The PICO (population, intervention, comparison, outcome) acronym was used to structure the systematic search:
- -
Population: Adults with complete and incomplete traumatic spinal cord injury at any level (cervical, thoracic and/or lumbar).
- -
Intervention: early decompression surgery (under 24h).
- -
Comparison: late decompression surgery (over 24h).
Neurological outcomes according to the American Spinal Injury Association (ASIA) scale.9
Studies published in any language, in humans, with an abstract and full text were considered for inclusion. Only prospective cohort and randomised studies which compared early versus late decompression were sought and included in the review.
Retrospective, case studies, control studies, case series and case reports were excluded.
Studies which used surgical methods for decompression of the spinal cord and which presented efficacy or effectiveness outcomes in final neurological recovery using the ASIA9 scale were sought.
The parameter of a clinically significant improvement in the neurological outcome was improvement of 2 grades or more on this scale between the outset and final situation, as suggested by several authors.10,11
Study selectionThe literature review was performed by 2 medical researchers (JG and GCW). After the initial search and filter selection, the final articles were selected by a group of doctors with experience in the treatment of patients with spinal cord injury (AB, LR and MP) following the quality article selection protocols,12–14 reading and analysing the full articles of the relevant studies according to the chosen inclusion criteria. The final decision regarding the inclusion of the works was resolved through discussion among the entire group of authors of this study.
Statistical analysisData from the included studies were saved and summarised through the Review Manager (RevMan) programme, version 5.4.1, Cochrane collaboration 2020. Statistical heterogeneity was evaluated with the I,2 with the fixed-effect model. The forest plot was used for the studies included in the meta-analysis, and visual inspection of the symmetry of the funnel plot, together with the Egger test, were used to assess publication bias. The Egger test was performed using the “metafor” package of the R computer programme.
ResultsWith our search strategy, 120 references were located. Ninety-nine were excluded based on their title and/or abstract and 21 were selected for full text reading. After excluding previous systematic reviews, there were 7 final articles that met the inclusion criteria (Fig. 1), 5 of them being prospective cohort studies15–19 and 2 controlled trials.20,21
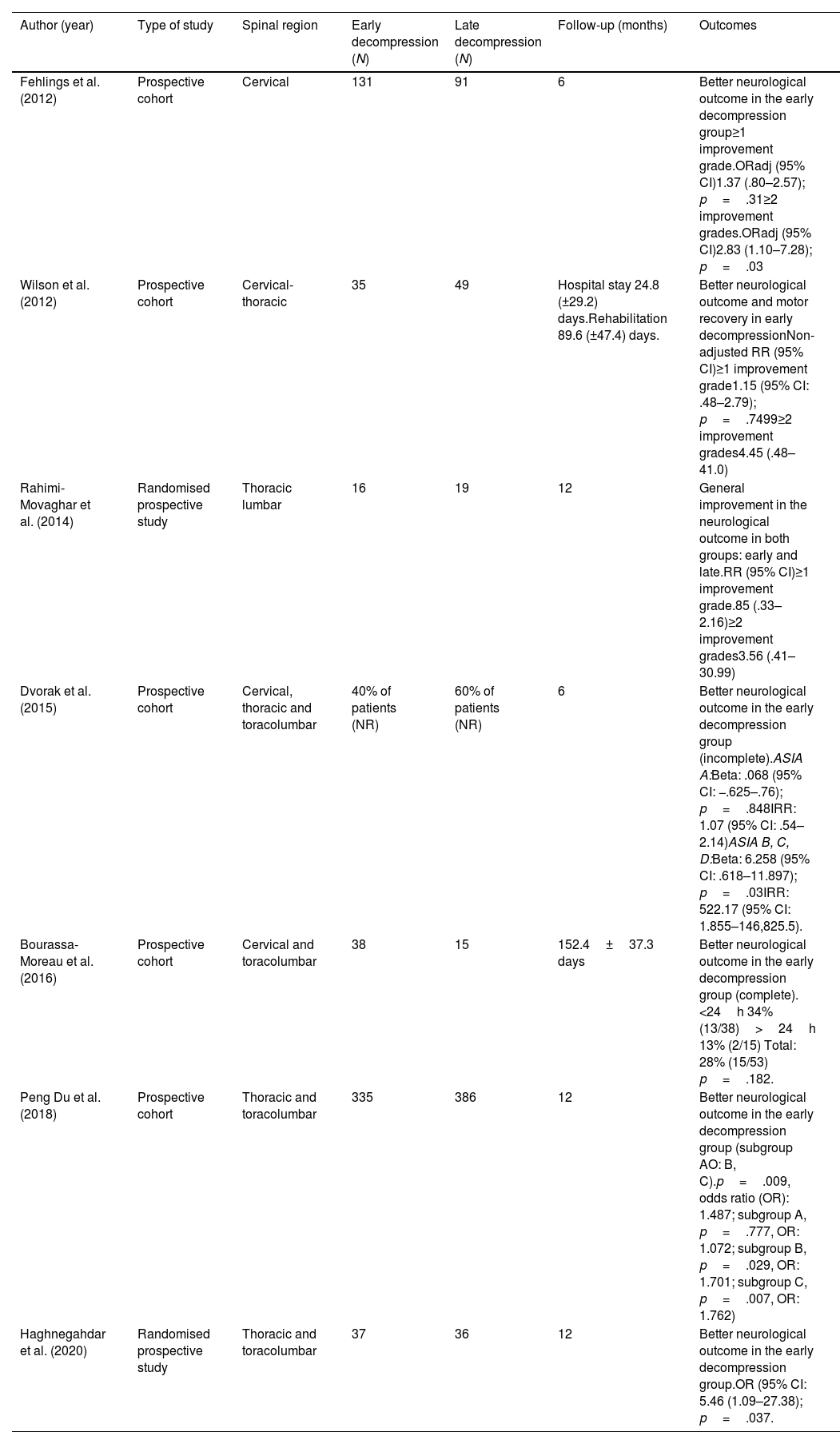
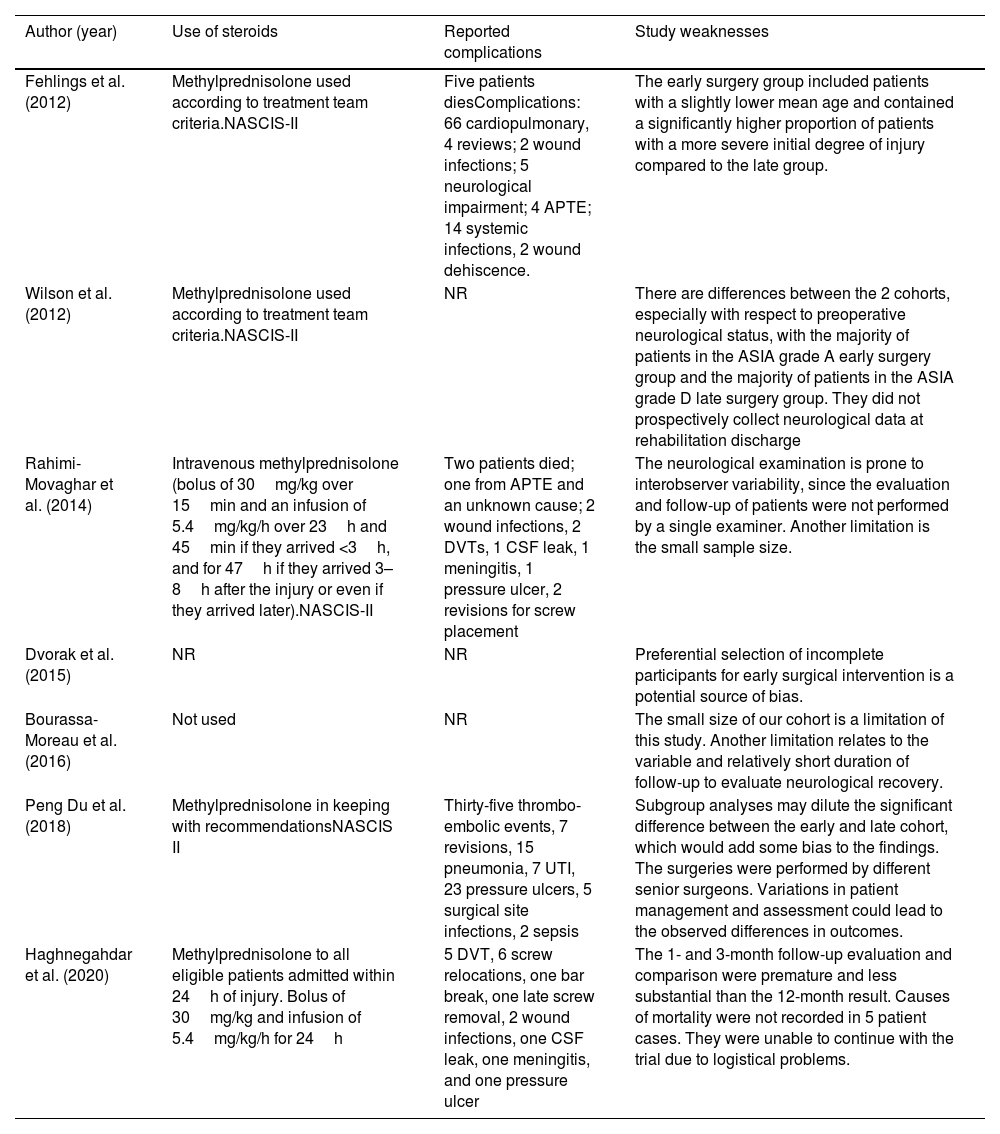
From the 7 included studies, data were extracted on the total number of patients; the injury level; the number of patients undergoing early decompression; the number of patients undergoing late decompression; the number of patients according to pre- and postoperative ASIA subgroups; the percentage of neurological recovery (primary objective); follow-up time; steroid regimen received or not, and complications (Tables 1 and 2).
Statistical analysis of studies included.
| Author (year) | Type of study | Spinal region | Early decompression (N) | Late decompression (N) | Follow-up (months) | Outcomes |
|---|---|---|---|---|---|---|
| Fehlings et al. (2012) | Prospective cohort | Cervical | 131 | 91 | 6 | Better neurological outcome in the early decompression group≥1 improvement grade.ORadj (95% CI)1.37 (.80–2.57); p=.31≥2 improvement grades.ORadj (95% CI)2.83 (1.10–7.28); p=.03 |
| Wilson et al. (2012) | Prospective cohort | Cervical-thoracic | 35 | 49 | Hospital stay 24.8 (±29.2) days.Rehabilitation 89.6 (±47.4) days. | Better neurological outcome and motor recovery in early decompressionNon-adjusted RR (95% CI)≥1 improvement grade1.15 (95% CI: .48–2.79); p=.7499≥2 improvement grades4.45 (.48–41.0) |
| Rahimi-Movaghar et al. (2014) | Randomised prospective study | Thoracic lumbar | 16 | 19 | 12 | General improvement in the neurological outcome in both groups: early and late.RR (95% CI)≥1 improvement grade.85 (.33–2.16)≥2 improvement grades3.56 (.41–30.99) |
| Dvorak et al. (2015) | Prospective cohort | Cervical, thoracic and toracolumbar | 40% of patients (NR) | 60% of patients (NR) | 6 | Better neurological outcome in the early decompression group (incomplete).ASIA A:Beta: .068 (95% CI: −.625–.76); p=.848IRR: 1.07 (95% CI: .54–2.14)ASIA B, C, D:Beta: 6.258 (95% CI: .618–11.897); p=.03IRR: 522.17 (95% CI: 1.855–146,825.5). |
| Bourassa-Moreau et al. (2016) | Prospective cohort | Cervical and toracolumbar | 38 | 15 | 152.4±37.3 days | Better neurological outcome in the early decompression group (complete).<24h 34% (13/38)>24h 13% (2/15) Total: 28% (15/53) p=.182. |
| Peng Du et al. (2018) | Prospective cohort | Thoracic and toracolumbar | 335 | 386 | 12 | Better neurological outcome in the early decompression group (subgroup AO: B, C).p=.009, odds ratio (OR): 1.487; subgroup A, p=.777, OR: 1.072; subgroup B, p=.029, OR: 1.701; subgroup C, p=.007, OR: 1.762) |
| Haghnegahdar et al. (2020) | Randomised prospective study | Thoracic and toracolumbar | 37 | 36 | 12 | Better neurological outcome in the early decompression group.OR (95% CI: 5.46 (1.09–27.38); p=.037. |
NR: not reported.
Use of steroids and complications reported in the studies in addition to their respective weaknesses.
| Author (year) | Use of steroids | Reported complications | Study weaknesses |
|---|---|---|---|
| Fehlings et al. (2012) | Methylprednisolone used according to treatment team criteria.NASCIS-II | Five patients diesComplications: 66 cardiopulmonary, 4 reviews; 2 wound infections; 5 neurological impairment; 4 APTE; 14 systemic infections, 2 wound dehiscence. | The early surgery group included patients with a slightly lower mean age and contained a significantly higher proportion of patients with a more severe initial degree of injury compared to the late group. |
| Wilson et al. (2012) | Methylprednisolone used according to treatment team criteria.NASCIS-II | NR | There are differences between the 2 cohorts, especially with respect to preoperative neurological status, with the majority of patients in the ASIA grade A early surgery group and the majority of patients in the ASIA grade D late surgery group. They did not prospectively collect neurological data at rehabilitation discharge |
| Rahimi-Movaghar et al. (2014) | Intravenous methylprednisolone (bolus of 30mg/kg over 15min and an infusion of 5.4mg/kg/h over 23h and 45min if they arrived <3h, and for 47h if they arrived 3–8h after the injury or even if they arrived later).NASCIS-II | Two patients died; one from APTE and an unknown cause; 2 wound infections, 2 DVTs, 1 CSF leak, 1 meningitis, 1 pressure ulcer, 2 revisions for screw placement | The neurological examination is prone to interobserver variability, since the evaluation and follow-up of patients were not performed by a single examiner. Another limitation is the small sample size. |
| Dvorak et al. (2015) | NR | NR | Preferential selection of incomplete participants for early surgical intervention is a potential source of bias. |
| Bourassa-Moreau et al. (2016) | Not used | NR | The small size of our cohort is a limitation of this study. Another limitation relates to the variable and relatively short duration of follow-up to evaluate neurological recovery. |
| Peng Du et al. (2018) | Methylprednisolone in keeping with recommendationsNASCIS II | Thirty-five thrombo-embolic events, 7 revisions, 15 pneumonia, 7 UTI, 23 pressure ulcers, 5 surgical site infections, 2 sepsis | Subgroup analyses may dilute the significant difference between the early and late cohort, which would add some bias to the findings. The surgeries were performed by different senior surgeons. Variations in patient management and assessment could lead to the observed differences in outcomes. |
| Haghnegahdar et al. (2020) | Methylprednisolone to all eligible patients admitted within 24h of injury. Bolus of 30mg/kg and infusion of 5.4mg/kg/h for 24h | 5 DVT, 6 screw relocations, one bar break, one late screw removal, 2 wound infections, one CSF leak, one meningitis, and one pressure ulcer | The 1- and 3-month follow-up evaluation and comparison were premature and less substantial than the 12-month result. Causes of mortality were not recorded in 5 patient cases. They were unable to continue with the trial due to logistical problems. |
CSF: cerebrospinal fluid; DVT: deep vein thrombosis; NR: not reported; UTI: urinary tract infection.
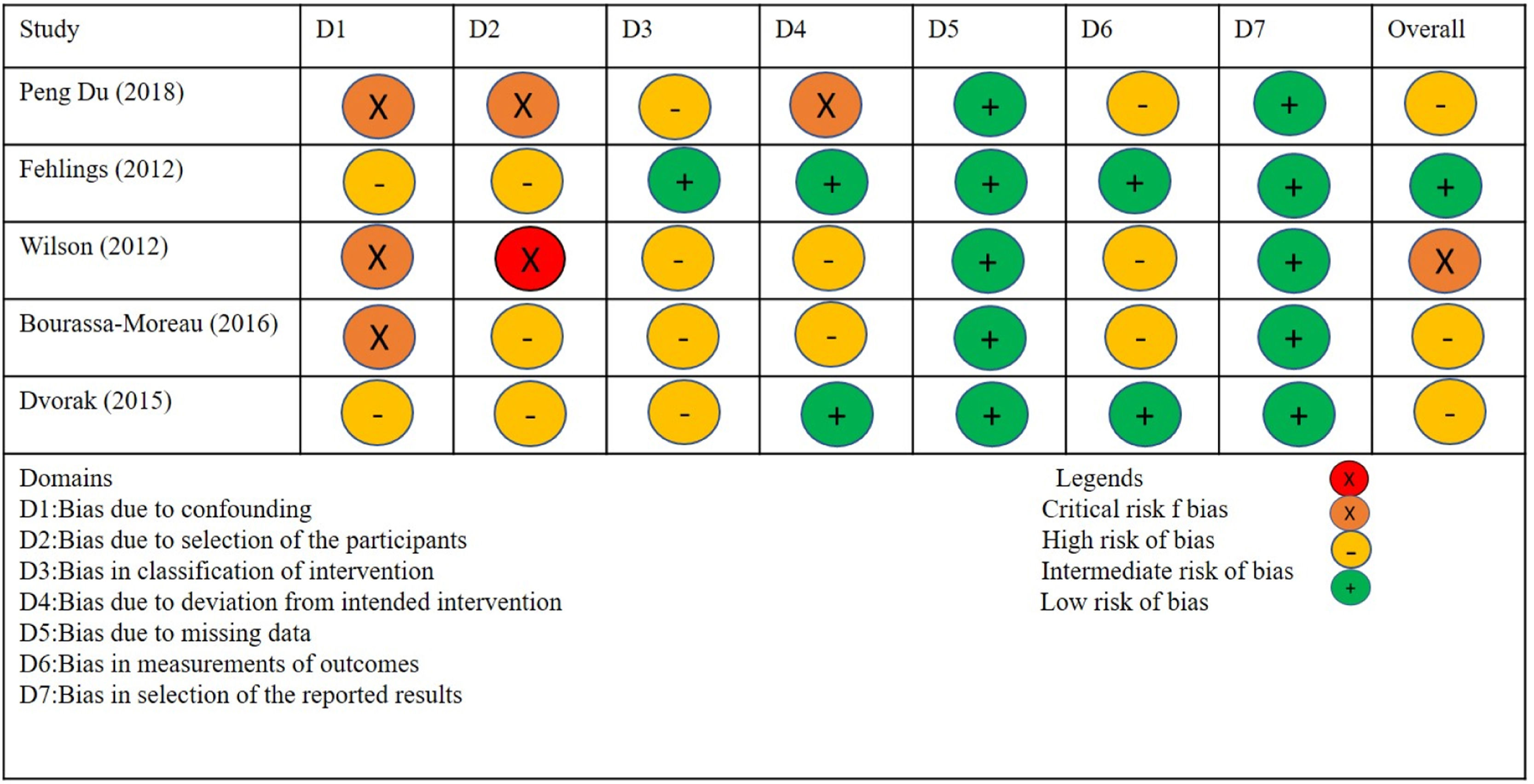
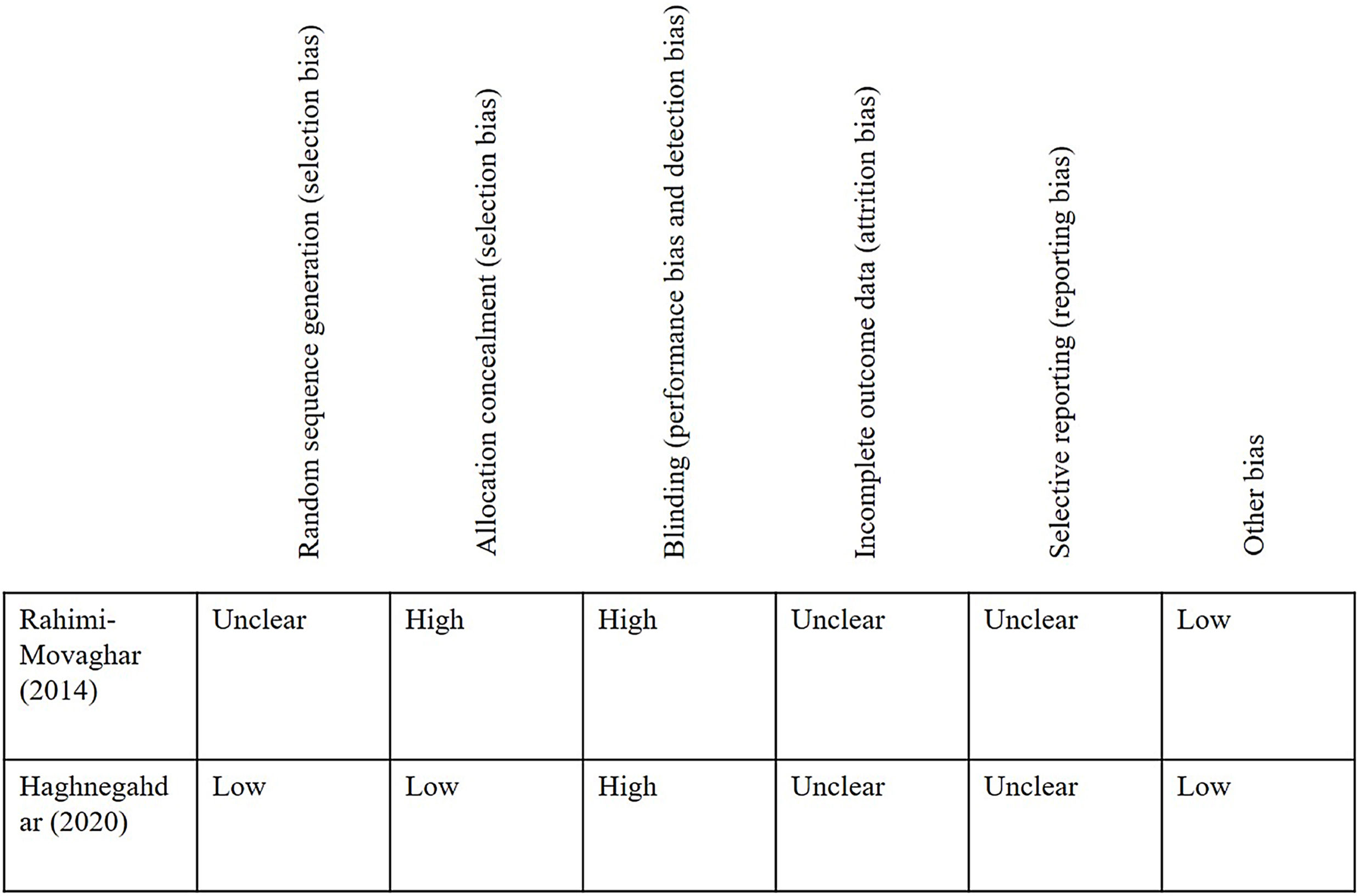
All articles were critically assessed, also including their levels of evidence and risk of bias with the tool known as Risk Of Bias In Non-Randomised Studies – of Interventions (ROBINS-I)22 for observational studies and Rob223 (version 2 of Cochrane risk-of-bias tool for randomised trials) for controlled clinical trials. We included two studies with level of evidence type II,18,21 the remaining five studies with level of evidence type III.
Of the 6 studies included in the meta-analysis, 5 studies showed significant differences in favour of early decompression. The benefit was greater in cervical and incomplete injuries.
Steroid usageIn 5 studies, steroids were used within 24h after the injury according to the NASCIS-II protocol (Table 2). Three of these studies used it systematically,16,20,21 2 used it according to the criteria of the treating team,18,19 one study did not use it15 and one study did not include this criterion.19
Follow-upOnly 3 of the selected studies had a follow-up of at least 12 months.16,20,21 One of the studies reported follow-up dividing into average hospital duration and average rehabilitation duration with no differences between early and late surgery groups17 and one study did not report long-term or final neurological follow-up, arguing that the objective of the work was to study improvement of acute and sub-acute motor activity produced between time of injury and 6 months after the injury.19
Sample sizes varied among the 7 studies, with the smallest being 35 patients20 and the largest 888 patients.19
The seven selected studies assessed the neurological function using the ASIA scale. All, except one16 included both complete and incomplete spinal cord injuries.
Injury level outcome analysisOf the studies included, one provided data on the cervical spinal cord,18 one on the cervical and toracolumbar injury15 2 on thoracic-toracolumbar injuries,16,21 one on the toracolumbar segment20 and 2 on injuries of the 3 cervical, thoracic and lumbar segments.17,19
Cervical spinal cord injuryWe found one study,18 where initially 313 patients were recruited, leaving the final sample at 222 patients available 6 months after the injury. One hundred and thirty-one patients underwent early decompression surgery, and 91 late decompression surgery.
In the preoperative neurological evaluation, there was a predominance of injuries with ASIA grade A in the early decompression group and ASIA grade D in the late decompression group. In the postoperative neurological evaluation, there was a predominance of patients with ASIA grade D in both the patient groups with early and late decompression surgery. According to this information, 74 patients (56.5%) in the early group and 45 patients (49.5%) in the late group experienced at least 1 grade improvement and 26 patients (19.8%) in the early group and 8 patients (8.8%) in the late group experienced an improvement of at least 2 grades.
The study had a 6-month follow-up. Methylprednisolone was used by the treatment team, as recommended by the NASCIS-II study. A total of 194 patients (62%) received steroids when admitted to hospital, with a significantly greater proportion of administration in the early group compared with the late one.
Five patients died and 86 were lost to follow-up. Cardiopulmonary complications were the most prominent of complications and were present in 66 cases.
In the multivariate analysis, adjusted for preoperative neurological status and steroid administration, the odds of an ASIA improvement of at least 2 grades were 2.8 times higher among those who underwent early surgery compared with those who underwent late surgery (OR: 2.83, 95% CI: 1.10–7.28; p=.03).
Cervical and toracolumbar spinal cord injuryThe 2016 study by Bourassa-Moreau et al.15 that only included patients with complete spinal cord injury suggests that surgical decompression and stabilisation within 24h may improve neurological recovery, particularly for those with cervical injuries. No steroids were used and complications were not described.
A greater proportion of patients operated on in the first 24h after traumatic injury had some neurological improvement upon discharge from rehabilitation, compared to patients operated on later.
Finally, this study concludes that some may consider complete spinal cord injury with fatalism because it carries a poor neurological prognosis. However, neurological improvement has been shown to be possible in this population.
The findings of this study suggest that early surgical intervention within 24h after a traumatic complete spinal cord injury can promote neurological recovery, especially for those with injuries at the cervical level. Thus, they recommend keeping the surgical time at least less than 24h to promote neurological recovery.
Thoracic and toracolumbar spinal cord injuryThe 2020 prospective randomised study by Haghnegahdar A et al.,21 with a sample size of 73 patients, of whom 37 were surgically decompressed early and 36 late, indicates a significant difference in favour of early surgery versus late surgery, for a conversion of ASIA>2 degrees at 12-month follow-up. This study used methylprednisolone in all eligible patients admitted within 24h after injury, and the most common complication was deep vein thrombosis.
In the study, 17 patients (45.9%) in the early surgery group and 12 (33.3%) in the late surgery group had an improvement of ≥1 grade in ASIA at 12 months. Additionally, 9 patients (24.3%) in the early surgery group and 2 (5.6%) in the late surgery group were reported to have grade ≥2 improvement at 12 months. With these results, the authors conclude that early decompression is associated with a greater probability of neurological improvement, especially in injuries of the thoracic spine below T8.
Du JP et al.16 conducted a prospective cohort study in patients with thoracic injury. Their sample of 721 patients were divided into an early decompression group (<24h, n=335) and a late decompression group (24–72h, n=386). Each group was divided into subgroups A, B and C according to the AO Spinal Injury Classification System (AOSICS).24 Analysis of the effect of time from injury to surgery on ASIA grade conversion showed that early surgical decompression did not lead to a significant improvement in AOSICS24 type A classification, but did improve conversion into AOSICS type B and type C. The authors concluded that patients classified as AOSICS type A with complete spinal cord injury do not need to undergo aggressive early operations. However, patients with type B and type C lesions must undergo early intervention to achieve better clinical results).24
This study used methylprednisolone in all patients according to the NASCIS-II protocol, and the most frequent complications were thromboembolic events (35 patients) and pressure ulcers (23 patients).
Toracolumbar spinal cord injuryIn a study a of 35 patients, Rahimi-Movaghar V et al.20 evaluated the effect of early surgical decompression in spinal cord injuries with a level between T1 and L1. They observed improvements of 2 ASIA grades in 3 of 16 patients with early surgery and 1 of 19 in patients with late surgery RR: 3.56, 95% CI: .41–30.99, with no statistical significance being reached. Regarding complete spinal cord injury, no improvement was found in the motor activity score in any of the groups.
They administered intravenous methylprednisolone (bolus of 30mg/kg over 15min and an infusion of 5.4mg/kg/h over 23h and 45min if they arrived <3h, and for 47h if they arrived 3–8h after injury or even if they arrived later) based on NASCIS-II recommendations. The complications described were varied: deep vein thrombosis, surgical wound infection and cerebrospinal fluid fistula, among others.
Cervical-thoracic-toracolumbar spinal cord injuryTwo Canadian prospective cohort studies evaluated the three injured segments.
In one of them, Wilson JR et al.17 found no differences in the mean improvements in motor scores between the early and late decompression groups at the time of discharge (p=.18). However, at the time of discharge from rehabilitation (mean 90 days), patients who received early decompression showed additional motor improvement compared with those who received late decompression (mean improvements not reported for either group). Similarly, a greater percentage of patients in the early surgery group experienced an ASIA improvement of ≥2 grades (27.2%) than in the late surgery group (3%) when they were discharged from inpatient rehabilitation (non-adjusted RR: 8.9, 95% CI: 1.12–70.64; p=.0154). The strength of evidence for all of these results was very low.
Methylprednisolone was used at the discretion of the treatment team and following the NASCIS-II recommendations. No complications were reported.
In the study with the largest number of patients, by Dvorak MF et al.19 (888 patients), no significant differences were found in the improvement of motor score between the early and late surgery groups in patients with ASIA grade A.
Patients with ASIA grades B, C or D spinal cord injury treated early improved an average of 6 additional motor points compared to those who were decompressed late. The confidence interval for the regression coefficient was large and indicated substantial variability. They did not report the time period for improvement or follow-up, nor were use of steroids and complications described.
Meta-analysis on neurological recovery of the studies includedSix of the 7 selected studies were included for our meta-analysis. We excluded the study by Dvorak MF et al.19 due to the lack of certainty regarding its number of patients in the early and late decompression groups.
Based on the results, a significant improvement was observed in favour of early decompression over late decompression with a heterogeneity of 46%, which, according to the fixed effect model25 (Fig. 2), was considered moderate.
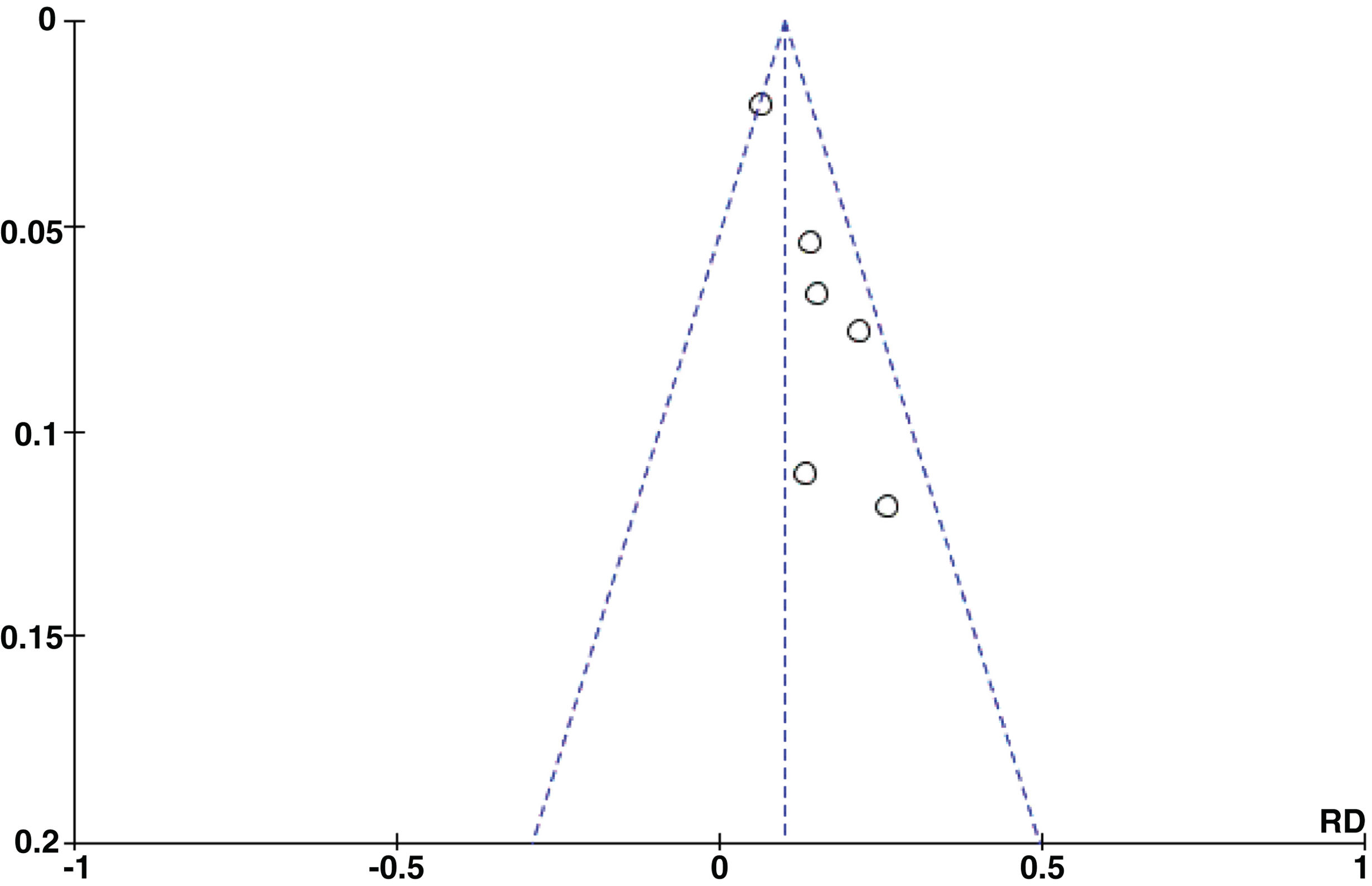
A possible significant publication bias was found from inspection of the funnel plots (Fig. 3) and Egger's test (p=.0053). This may be because the number of publications included in our study was very small. In these cases, the Funnel plot and the statistical tests are reduced in power.
Risk of bias of the included studiesFigs. 4 and 5 show the risks of bias for prospective cohort studies and for controlled trials, respectively. The bias was considered low for the study by Fehlings et al., moderate for the studies by Peng Du et al., Moreau et al. and Dvorak et al., and high for the study by Wilson et al. For the controlled trials, the risk of bias was considered moderate for both studies.
DiscussionIn our review we found evidence in favour of early decompression over late decompression in 6 studies,15,21 and benefits in both groups in one study.20 Regarding general neurological recovery, this difference was evident in injuries at the cervical level and in incomplete injuries, but was unclear in injuries to the thoracic and thoracolumbar region, and in complete ASIA grade A injuries.
In other previous systematic reviews, such as that of Hsieh YL et al.26 which included 26 studies, they reported that the cut-off time in early decompression was a significant moderator of the effect, and that if performed before 8–12h after spinal cord injury, it was associated with greater benefits. However, they concluded that quality evidence was lacking.
In another review by Yousefifard M. et al.27 they found that surgical decompression performed within 24h after injury was associated with significantly lower rates of postoperative complications. However, unlike our review (exclusive of prospective studies), they included case series and retrospective studies (12 of the 24 included studies) and there was also non-uniformity regarding the definition of early decompression.
The combined analysis of individual patient data, derived from 4 prospective and independent multicentre sources by Badhiwala J et al.28 is also noteworthy. This analysis reports that patients who underwent early surgical decompression experienced greater recovery than patients who underwent delayed decompression surgery one year after spinal cord injury, and conclude that the first 24–36h after injury appear to represent a crucial time window to achieve optimal neurological recovery with decompression surgery after an acute spinal cord injury.
Surgical treatment in patients with traumatic spinal cord injury in whom spinal cord compression persists, aims to reduce the extension of the secondary spinal cord injury that appears after the primary spinal cord injury associated with spinal cord trauma. It would therefore form part of neuroprotection strategies after spinal cord injury.2,29
In injuries with complete spinal cord section, early decompression may not make sense, but it must be taken into account that the majority of spinal cord injuries are due to compression and are cervically located (51% in our environment) with possible disability as severe as a tetraplegia as a sequela.2 Therefore, any effort to mitigate the ultimate neurological damage in these patients must be considered and analysed.
Several factors determine the severity of spinal cord damage during spinal trauma. Among them, the magnitude of the initial damage, known as “primary damage” that influences the severity of the injury and the extent of neurological compromise. The greater the energy of the initial trauma, the greater the spinal inflammatory process and the disruption of the microvasculature, which leads to greater oedema and release of pro-apoptotic cytokines.30
After this initial damage, there is a “secondary injury”, determined by a subsequent inflammatory response, which can lead to definitive neurological damage. The objective of surgical treatment in acute spinal cord injury is to attenuate the cascade of secondary damage, with the aim of allowing an improvement in the neurological condition.31
Thus, since the results obtained by the STASCIS18 study were reported, where it was shown that patients undergoing early decompression had better neurological recovery compared to patients with late decompression 6 months after treatment, multiple studies added evidence to this recommendation.17,32–35 Ter Vengel PV et al.4 analysed neurological recovery after early and late decompression in patients with complete and incomplete cervical injury and observed greater improvement in patients with incomplete injury than in patients with complete injury.
However, other studies have shown similar results between early and late decompression.20 In a randomised study, neurological improvement was observed in both groups, without significant differences. This study is limited by a relatively low number of patients with 16 in the early decompression group and 19 in the late decompression group. Similar results were observed by Ter Vengel PV et al.4 in patients with thoracic injury undergoing early versus late decompression.
Weaknesses of the included studiesAs weaknesses of the study by Fehlings MG et al.18 we observed that the early surgery group included patients with a slightly lower mean age and contained a significantly higher proportion of patients with a more severe initial degree of injury compared to the late group. Additionally, the non-random nature of the sample suggested possible selection bias.
Regarding the study by Bourassa-Moreau E et al.,15 the small cohort size constitutes a study limitation (53 patients). Another limitation is related to the variable and relatively short duration of follow-up to evaluate neurological recovery (152.4±37.3 days).
A weakness in the work of Du JP et al.,16 was that randomisation and double-blind methods were not used, so some potential biases could not be avoided. Subgroup analyses may dilute the significant difference between the early and late cohort, which would add some bias to the findings. The interventions were performed by different senior surgeons. Variations in patient management and assessment could lead to the observed differences in outcomes.
In the study by Rahimi-Movaghar V et al.20 the number of complications was high (11 patients) in relation to their short series.
As weaknesses of the study by Wilson JR et al.,17 the authors expressed that there were differences between the 2 cohorts, especially with respect to preoperative neurological status, with the majority of patients in the ASIA grade A early surgery group and the majority of patients in the ASIA grade D late surgery group. Also, they did not prospectively collect neurological level data at rehabilitation discharge.
One possible bias in the study by Dvorak MF et al.19 was attributing the improvement in the recovery of the motor score to the surgical intervention when it could simply be due to the natural course of the incomplete spinal cord injury. Another potential source of bias in this study was the preferential selection of participants with incomplete spinal cord injury for early surgery.
The overall strength of the evidence that early surgical decompression results in clinically meaningful improvements in neurological status (≥2 ASIA grade improvement) at any follow-up period was ‘low’ to ‘very low’.
Similarly to Fehlings MG et al.,32 we believe that there are many limitations in the current scientific evidence. These include heterogeneity between studies (population, severity and level of injury); relatively low number of patients in some studies; a lack of consistency of findings due to single studies, and the inability to detect differences in complication rates in surgical cohorts due to lack of statistical power. These data should be taken into account for planning future research on the topic. In this practical guideline,32 the authors suggest that early surgery be offered as an option for adult patients with acute spinal cord injury, regardless of the “low” level of recommendation.
Another important element that impacts patient selection is transportation time from the time of injury to the appropriate level hospital for resolution of the condition, associated with all the nuances involved in performing “emergency” decompression surgery (both logistics and surgical materials to be used for stabilisation). To this end, Spain needs to create an appropriate health organisation (similar to the National Transplant Organisation or the Stroke Codes, which have demonstrated such good results) to enable rapid transfer of these patients from the accident site to a tertiary hospital where the initial assessment and decompression surgery can be performed in the shortest time possible.
LimitationsOur study has limitations and strengths. The limitations of this review are directly related to the limitations of the individual studies included, which were previously discussed and to the number of patients; possible treatment selection bias (higher proportion of young patients in the early decompression group); the use of corticosteroids, and the heterogeneity of follow-up. We would also like to report that we did not register the review protocol in PROSPERO, and there may be similarity with other reviews. However, we consider that our review is the most up-to-date on the topic in question. Furthermore, we found possible publication bias, demonstrated by the Egger test (p=.0053), which could be due to the low number of studies included in the meta-analysis.
Study strengths include the quality of the studies included in our review, with 2 prospective randomised studies, and the remainder prospective cohort studies. As review quality is directly related to the quality of the included studies, we consider that this systematic review meets the quality criteria for its results to be sustained.
Finally, although the references are primarily English-language publications, to our knowledge, this is the first systematic review and meta-analysis on this topic carried out in Spanish.
ConclusionsThere is scientific evidence to recommend early decompression in the first 24h after traumatic spinal cord injury, as it improves final neurological recovery. These results are more evident in cervical and incomplete injuries, while the effectiveness in thoracolumbar and complete injuries is unclear.
Although there is a patient selection bias in most of the included studies, in general terms, current evidence suggests a beneficial effect of early over late surgical decompression, which should be recommended whenever the patient and hospital conditions allow it to be safely performed.
Level of evidenceLevel of evidence i.
Conflict of interestsThe authors have no conflict of interests to declare.