The purpose of this study is the evaluation of the patellofemoral arthroplasty (PFA) survival and clinical and radiological outcomes in our institution.
MethodsA retrospective evaluation of our institution patellofemoral arthroplasty cases from 2006 to 2018 was performed; the n sample after applying exclusion and inclusion criteria was 21. All patients excepting one were female with a median age of 63 (20–78). A Kaplan–Meier survival analysis at ten years was calculated. Informed consent was obtained from all patients prior being included in the study.
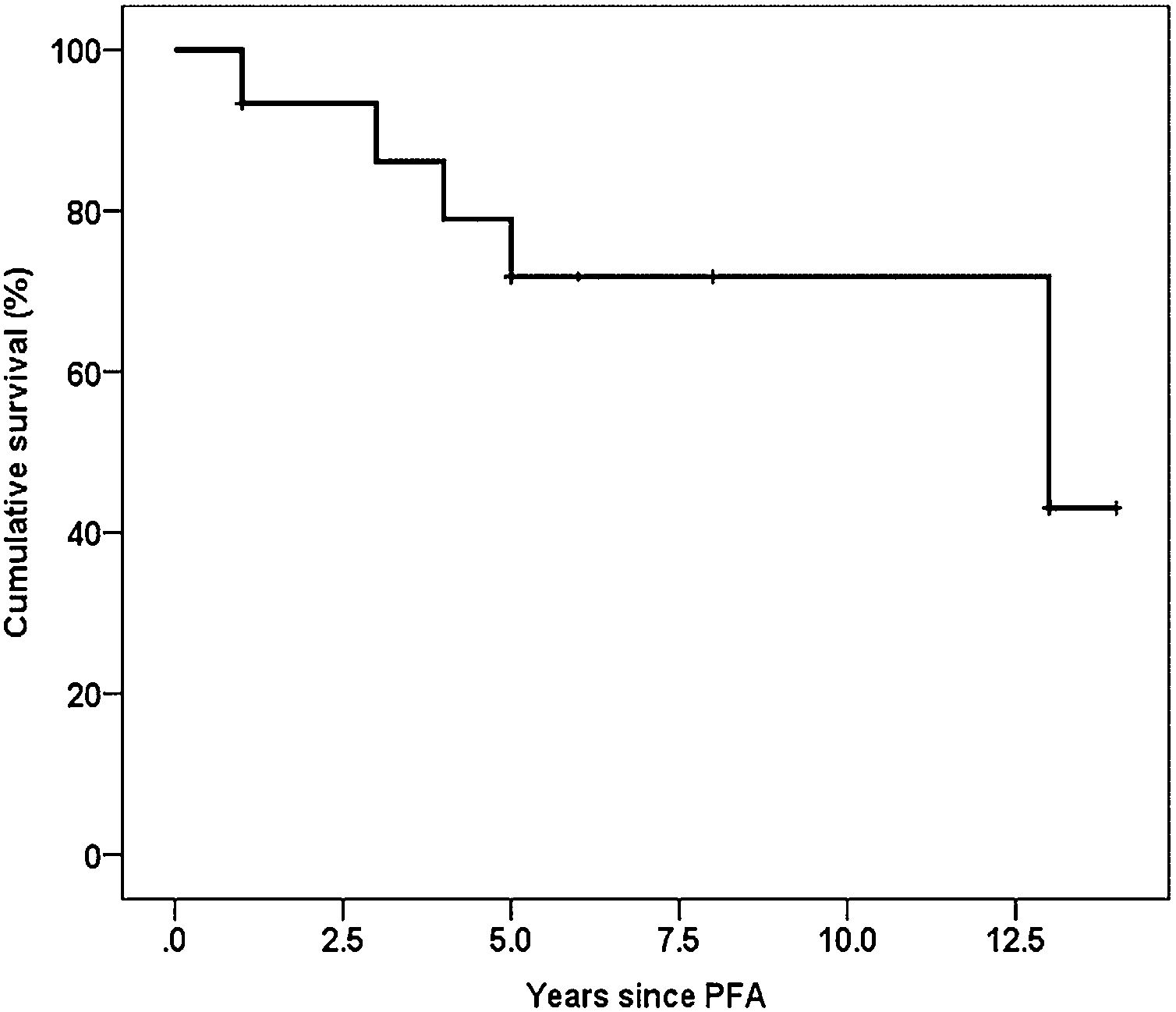
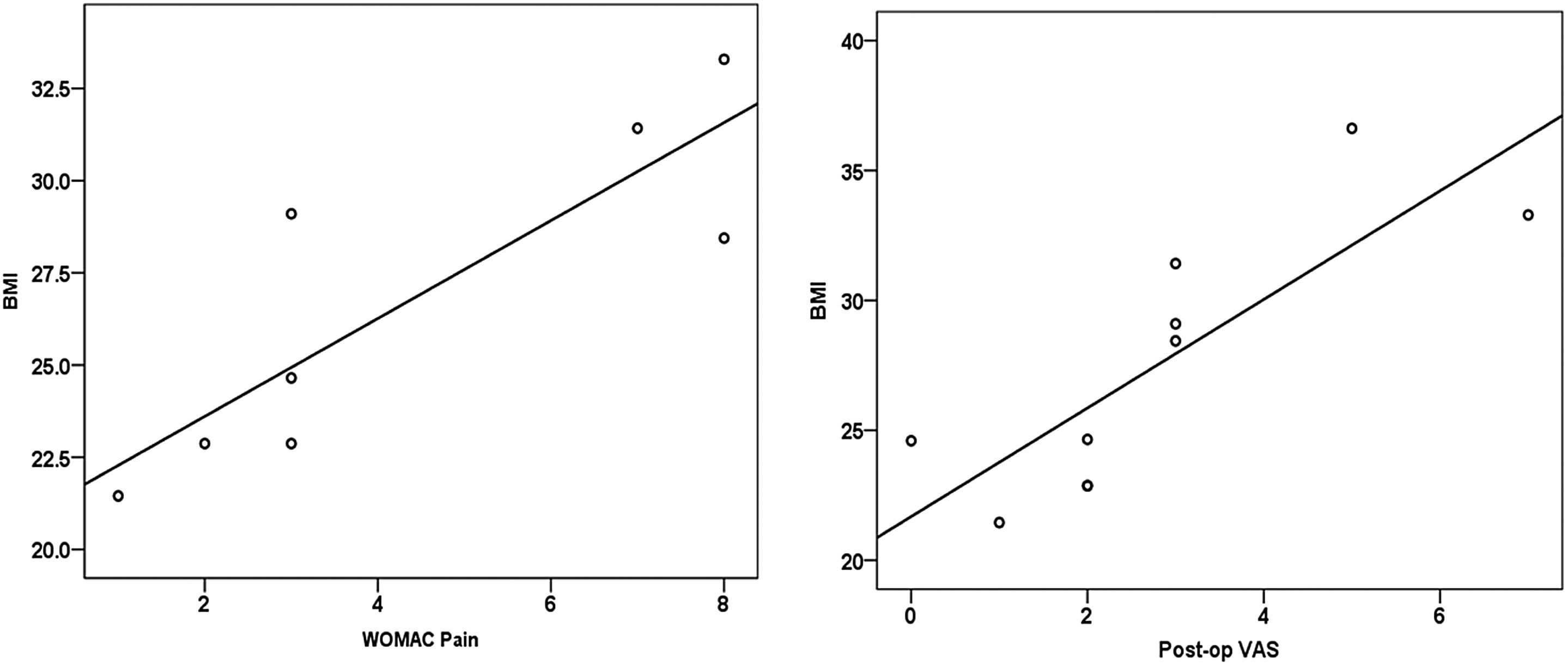
ResultsThe total revision rate was 6 out of 21 patients (28.57%). The progression of the osteoarthritis in the tibiofemoral compartment was the main cause (50% of revision surgeries). The degree of satisfaction with the PFA was high, with a mean Kujala score of 70.09 and a mean OKS of 35.45 points. The VAS score improved significantly (p<0.001) from a preoperative mean of 8.07 to a postoperative mean of 3.45, with an average improvement of 5 (2–8). Survival at 10 years, with revision for any reason as the endpoint, was 73.5%. A significant positive correlation between BMI and the WOMAC pain (r=0.72, p<0.01) and between BMI and the post-operative VAS (r=0.67, p<0.01) was observed.
ConclusionsThe results of the case series under consideration suggest that PFA could be a possibility in the joint preservation surgery on the isolated patellofemoral osteoarthritis. BMI >30 seems to be a negative predictor factor in relationship with the postoperative satisfaction, increasing the pain proportionally to this index and requiring more replacement surgery than patients with BMI <30. Meanwhile the radiologic parameters of the implant are not correlated with the clinical or functional outcomes.
El propósito de este estudio es la evaluación de la supervivencia de la prótesis femoropatelar y los resultados clínicos y radiológicos en nuestro centro.
MétodosEn el presente estudio se realiza una evaluación retrospectiva de los casos de prótesis femoropatelar en nuestro centro entre los años 2006 y 2018. El tamaño muestral, tras aplicar los criterios de inclusión y de exclusión, fue de 21 pacientes. Todos los pacientes excepto uno fueron mujeres, con una media de edad de 63 años (rango 20-78). Se calculó una gráfica de Kaplan-Meier de supervivencia en los primeros 10 años. El consentimiento informado de todos los pacientes fue obtenido previamente a la inclusión en este estudio.
ResultadosLa tasa de recambio a prótesis total fue 6 de 21 pacientes (28,57%). La progresión de la osteoartrosis en el compartimento tibiofemoral fue la causa principal (50% de las cirugías de revisión). El grado de satisfacción con la PFA fue alto, con una media en la escala de Kujala de 70,09 y una media de OKS de 35,45 puntos. La EVA mejoró significativamente (p<0,001), de una media preoperatoria de 8,07 a una media postoperatoria de 3,45, siendo la media de mejoría de 5 puntos (2 a 8 puntos). La supervivencia a los 10 años, con rescate de la prótesis debido a cualquier causa, fue del 73,5%. Se observó una correlación positiva ente el IMC y la escala WOMAC (r=0,72, p>0,01) y entre el IMC y la EVA postoperatoria (r=0,67 y p<0,01).
ConclusionesLos resultados de esta serie de casos mostraron que la prótesis femoropatelar puede ser una alternativa de tratamiento como cirugía de preservación de la osteoartritis femoropatelar aislada. El IMC>30 parece ser un factor predictor negativo en relación con la satisfacción postoperatoria, incrementando el dolor con una correlación positiva con este índice y requiriendo mayor cirugía de reemplazo que los pacientes con IMC<30. Por otra parte, los parámetros radiológicos relacionados con el implante no están correlacionados con los resultados clínicos ni funcionales.
Isolated patellofemoral (PF) osteoarthritis (OA) is a relative common pathology in our environment, appreciating an increasement of the prevalence in female patients over 50 years with rates of 24% comparing with 11% in males.1 The PF compartment is overloaded in daily activities such as climbing and descending stairs, standing up or sitting or in sports like trekking because of the knee flexion and quadriceps muscle contraction.
Treatment is conservative in early stages, using non steroid drugs, corticoid infiltrations, bracing, weight lost or rehabilitation. Surgical care must be required in advanced stages when conservative treatment has failed and the patient continues symptomatic. The surgical options available include replacement or non-replacement surgery (microfractures, chondroplasty, autologous cartilage implantation or anterior tibial tubercle osteotomy, etc.).
Replacement surgery is indicated when exists anterior pain or instability related to trochlear dysplasia or bone on bone contact between posterior facet of the patella and trochlear groove wearing the articular cartilage (posttraumatic or degenerative).2,3 There are two options of arthroplasty, total knee arthroplasty (TKA) and patellofemoral arthroplasty (PFA).
Traditionally is considered that PFA has lesser morbidity and mortality than TKA, a faster recovery of the patient and a better functionality4 with a higher bone stock in the knee, that will facilitate future revision surgeries if they are required.5
Most of studies report that the PFA revision to TKA is associated with worse outcomes than those patients whom are performed a primary TKA.6,7 Van Jonbergen et al.8 reported a negative effect on the results of a future TKA comparing 13 primary TKA and 13 PFA to TKA conversions; with similar outcomes in knee function scores and WOMAC, but with higher taxes of mobilization in patients who required a conversion to TKA.
The purpose of this study is the analysis of the patellofemoral arthroplasty (PFA) survival, clinical and radiological outcomes in our institution. The influence of BMI in the results and causes of PFA to TKA conversion are also considered.
Materials and methodsSubjectsFrom 2006 to 2018, 24 PFA were performed in Virgen del Rocío Hospital (Sevilla, Spain) by four different experienced knee surgeons.
Study inclusion criteria were a minimum of one-year follow-up, uni- or bilateral PFA, and availability to return to the hospital for exploration, personal interviewing and radiological assessments.
Study exclusion criteria were less than one-year follow-up of up, patients with an inflammatory/rheumatic disease affecting the knee and patients who were not living in the hospital area at the moment of the recruitment.
The indication of PFA surgery considered was painful isolated PF osteoarthritis with failure of conservative, excluding patients with treatment of inflammatory disease, medial or/and knee compartment OA, flexion patella instability or a fixed flexion deformity of the knee.5
For the radiological study, only 15 patients were available and informed consent was obtained for all of them. The rest of patients were not available to come to the hospital due to logistic problems because they lived in other cities or suffered multiple comorbidities that made difficult their transport. One patient refused the radiologist study.
The patients were evaluated retrospectively with a mean postoperative follow-up of 9.7 years (from 1 to 14 years).
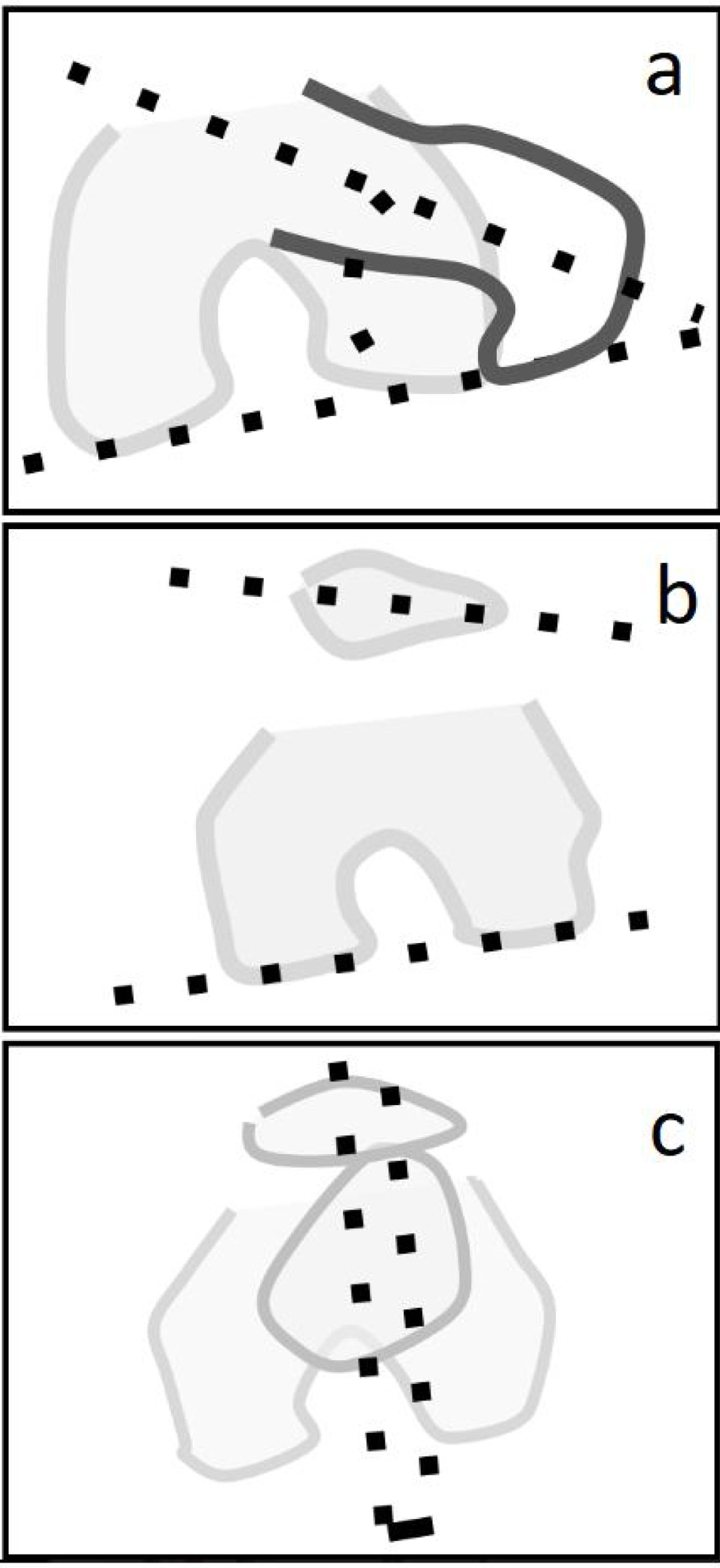
Surgical techniqueAll the patients received spinal anaesthesia and thigh ischaemia. Pre-operative antimicrobial prophylaxis with cephazolin was administrated to all patients. The approach was a medial parapatellar incision. The knee compartments, the menisci and the cruciate knee ligaments were inspected. Intramedullary guide was placed in the centre of the medullary canal and an anterior cut was made removing the minimal amount of bone from the trochlea. Trochleoplasty with rasp was made and the trial implant was placed. The next step was the patellar cut and after, the implantation of the final components (Fig. 1).
The two first implants were Avon PFA™ and the rest were Vanguard FP™. Both implants were on-lay. The bone cement was high viscosity polymethylmethacrylate mixed manually. No drains were used. Early mobilization and the immediate total wear bearing were authorized in the first 24h.
Measured outcomeClinical and functional assessment of all patients was carried out preoperatively using the visual analogue scale (VAS, 0 to 10 from no pain to worst possible pain) and postoperatively at twelve months using the VAS, the WOMAC scale (comprises 5 items for pain (0–20), 2 for stiffness (0–8), and 17 for functional limitation (0–68)),9 Oxford knee score (OKS, by which 0=worst possible score, 48=best possible score) assess function and pain after a TKA10 and Kujala score (ranged from 0 to 100, being 100 the full punctuation for life quality).11 The body mass index (BMI) and any complications were also recorded.
For the purpose of radiological assessment, immediate and during the follow-up, three radiographical projections (AP view, lateral view and patella axial view) were recorded.
In AP view, angle between anatomical axis and distal PFA axis was measured: a line through the mid-diaphyseal of femur is drawn and the other line crosses transversally the lower pole of the PFA. It is used to evaluate the femoral component coronal alignment with respect to the anatomical axis.12
In lateral view, Caton–Deschamps index was measured. This index is considered normal ranged 0.8–1.2. Patella alta is considered when the index is over 1.2 and patella baja is considered when the index is under 0.8.12
The measurement knee CT-scan are described down below:
Tibial tuberosity-trochlear groove distance (TTTG) measures the TTA lateralization, it was calculated to the nearest millimetre (mm) using cartilaginous-tendon landmarks described by Schöettle et al.13 (Fig. 2).
Femoral anteversion angle (FAVA) is the angle formed by a line anteriorly projecting from the femoral neck compared to the femoral shaft. To calculate this angle was necessary the measurement of the femoral neck horizontal angle (NHA) in the slice that reflects better this alignment and the posterior condyles horizontal angle (CHA) in the knee. If the CHA is in internal rotation (IR) this value must be added to the NHA. If the CHA is in external rotation (ER) the value must be rested to the NHA (Fig. 2).
Lateral patellar tilt angle (LPT angle) (Fig. 3): the angle is measured drawing a line through the mayor transverse axis of de PFA (trochlear component axis) and another line crossing the most posterior aspect of the femoral posterior condyles. This angle would indicate the rotation of the prothesis in relation with the posterior femoral condyles, so we can appreciate some of them in IR, others in ER and finally other PFA in neutral position.
Twist angle (Fig. 3): it is another angle to measure the implant rotation. The excessive internal rotation is described in the literature as proportional to the severity of the PF maltracking.14 To measure this angle we draw a line crossing the surgical epicondylar axis between medial and lateral epicondylar process and the other line crossing the major transverse axis of the prothesis. Negative values are internal rotation values and positive values correspond to external rotation.
PFA tilt with regard to patella (Fig. 3): two lines are drawn following respectively the transverse diameter of the PFA trochlear component and the transverse diameter of the patella. Rotation is also measured with this angle also corresponding positive values to external rotation and negative values to internal rotation.
‘IBM SPSS Statistics for Windows, version 29’ was used to perform the statistical analysis. Shapiro–Wilk test was chosen to study normality, owed to the small size of the sample (N<30). The results were described using central tendency measures; expressing the data as mean±standard deviation if the sample follows a normal distribution or median±interquartile range (IQR) if the sample non follows a normal distribution. Significance was set at p value <0.05.
Clinical improvement between the pre- and postoperative evaluation as described by the pre and post-operative VAS, OKS, WOMAC and Kujala was analyzed using a t-test for paired comparisons.
To calculate the statistical power, positive correlation between BMI and WOMAC pain (r=07.72, p>0.01) was considered. Pearson test was applied with a confidence level of 95% and a sample size of 21 obtaining a statistical power of 90.3%, with a 12.5% of loss.
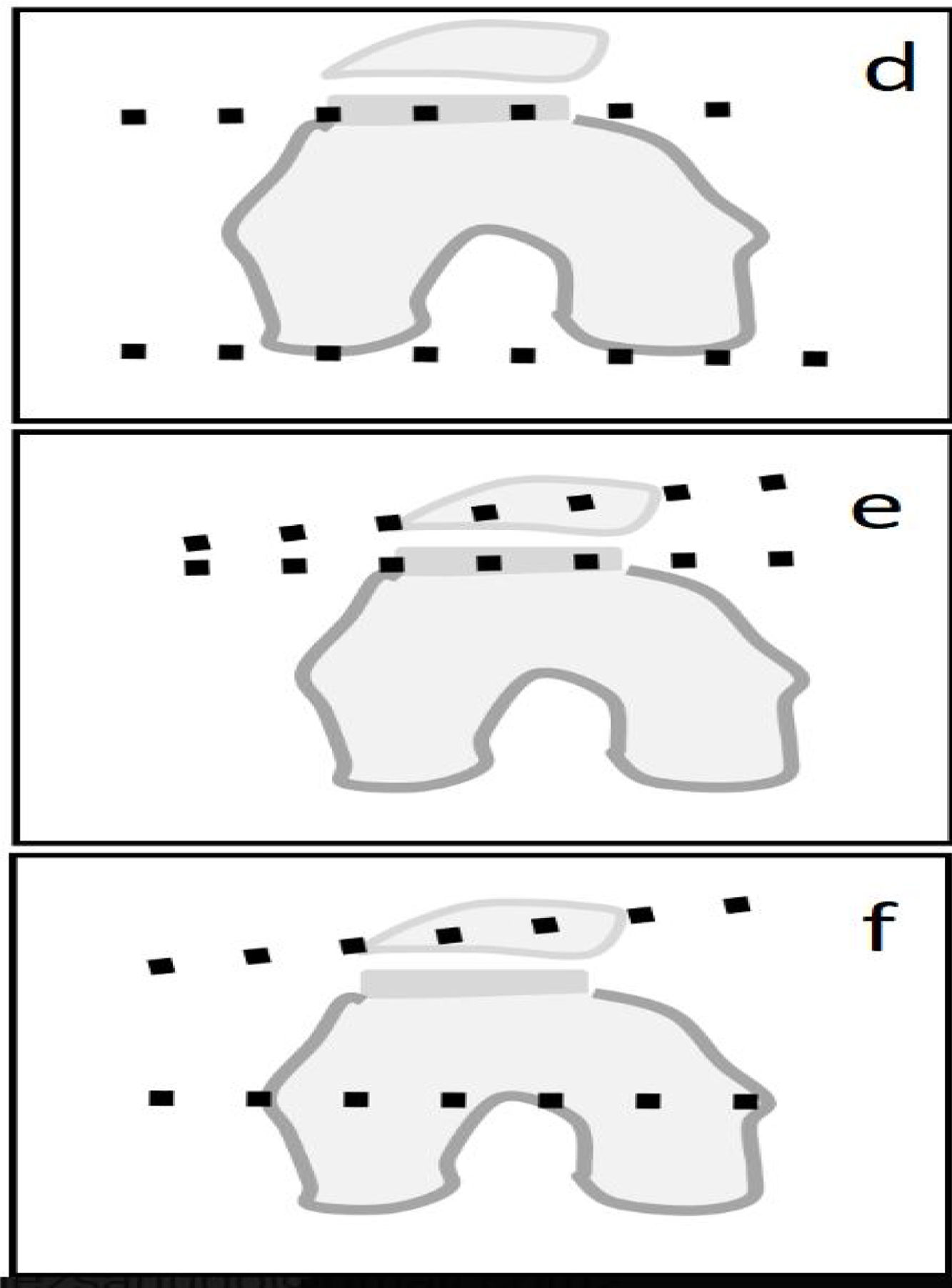
Kaplan–Meier survivorship analysis was performed, with implant revision as the endpoint.
The Pearson correlation coefficient was used to assess whether a correlation exists between the different parameters studied.
ResultsAfter applying inclusion and exclusion criteria, 21 patients aged between 20 and 79 years were selected. 12 were implanted in left knee and 9 in right knee. 2 patients had both knees affected. All the patients were female excepting one.
Exclusion criteria were applied for one patient because during the knee approach, a thickened synovial with ferrous colour and blood drain was found, pathologically corresponded with a villonodular synovitis. Two lost of follow-up were found; a man with a bilateral PFA and a woman with a unilateral PFA died during the follow-up due to causes beyond surgery.
Data was found to be normally distributed excepting age. The median age of surgery was 63 years (20–68). The mean of body mass index (BMI) was 26.65 points (from 21.43 to 36.62).
No intraoperative complications or deep vein thrombosis were observed.
The revision rate calculated about all the PFA implanted in our institution was 6 out of 21 patients (28.57%). Three knees (50% of replacements) were revised to a TKA because of disabling pain due to progression to osteoarthritis. Two patients (33.33%) were revised due to unexplainable disabling pain not related with OA progression. One patient (16.66%) was revised to TKA due to patella maltracking.
Kaplan–Meier survivorship analysis at 10 years, with revision for any reason as the endpoint, was 73.5% (Fig. 4). The survivorship mean time of the PFA that required revision was 8 years.
Clinical and functional assessmentThe mean Kujala score in this sample was 70.09 (45–100). OKS mean was 35.45 points (23–48). The VAS score improved significantly (p<0.001) from a preoperative mean of 8.07 (6–9) to a postoperative mean of 3.45 (0–7), with an average improvement of 5 (2–8) (Fig. 5).
Regarding the WOMAC stiffness section, 81.8% did not present any stiffness. 9.3% scored 1 point and other 9.3% 3 points. WOMAC physical functionality had a mean of 24.36±12.93 points. The mean of WOMAC pain was 4.38±2.82 points.
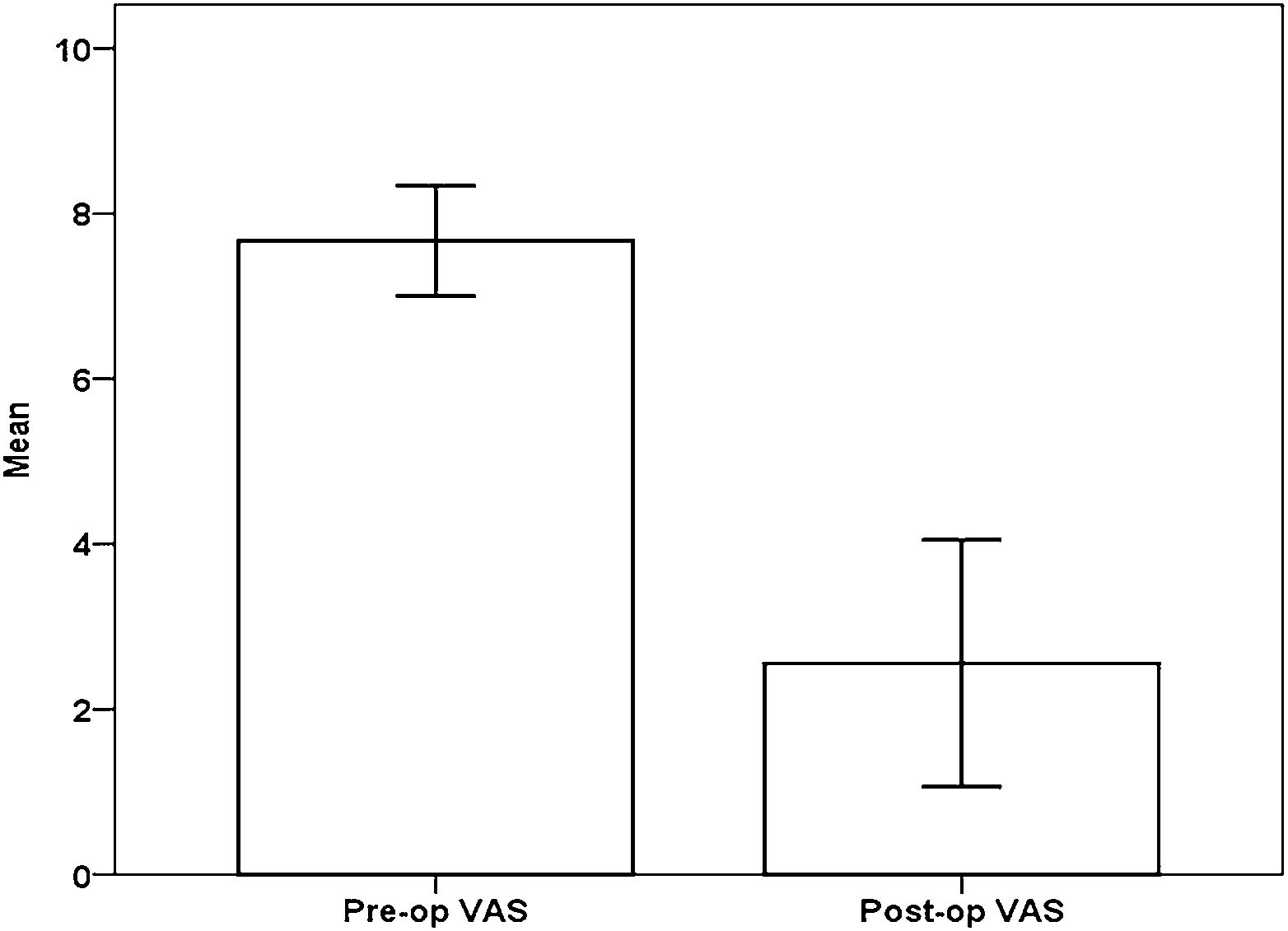
Correlations between BMI and the WOMAC pain subscale are described in Fig. 6.
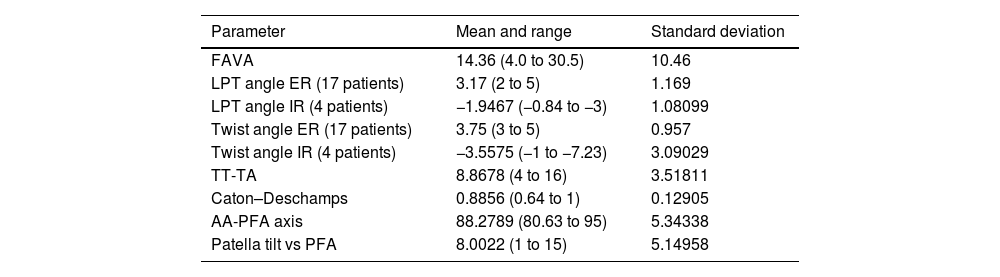
Radiological assessmentAn experimented musculoskeletal radiologist measured both, radiographies and CT-scans. Radiological measurements are reflected in Table 1.
Radiological measurements summarizing mean, ranges and standard deviations.
| Parameter | Mean and range | Standard deviation |
|---|---|---|
| FAVA | 14.36 (4.0 to 30.5) | 10.46 |
| LPT angle ER (17 patients) | 3.17 (2 to 5) | 1.169 |
| LPT angle IR (4 patients) | −1.9467 (−0.84 to −3) | 1.08099 |
| Twist angle ER (17 patients) | 3.75 (3 to 5) | 0.957 |
| Twist angle IR (4 patients) | −3.5575 (−1 to −7.23) | 3.09029 |
| TT-TA | 8.8678 (4 to 16) | 3.51811 |
| Caton–Deschamps | 0.8856 (0.64 to 1) | 0.12905 |
| AA-PFA axis | 88.2789 (80.63 to 95) | 5.34338 |
| Patella tilt vs PFA | 8.0022 (1 to 15) | 5.14958 |
FAVA: femoropatelar anteversion angle; LPT: lateral patellar tilt angle; ER: external rotation; IR: internal rotation; TTTG: tibial tuberosity–trochlear groove distance; AA-PFA axis: anatomical axis-patellofemoral arthroplasty.
No significant correlation was observed between the radiological measurements and postoperative OKS, pre- and postoperative VAS, VAS improvement, WOMAC or Kujala.
The main finding of this study is the result in midterm outcomes in 10 years of follow-up, describing a survivorship of 73.5% with a revision rate of 27.27% with a mean of 8 years of survivorship in the PFA before revision to TKA. These results are in line with other articles in the literature,15–18 but with inferior results as Konan et al.,16 96.1% of survival Ackroyd et al.17 95.8% with 5 years of follow-up or Odumenya et al.18 100% in 5 years, but all of them the follow-up was lower than this study (7 years in Konan and 5 years in Ackroyd and Odumenya) that can explain their results.
There is a lot of controversy in the literature about the PFA failure rate vs TKA. Meanwhile some studies describe more failure rate in PFA (18.9%) than in TKA (3.4%) a 2011 meta-analysis of 28 studies showed no significant differences in reoperation, revision, pain, or mechanical complications between second-generation PFA and TKA.19 There is a substantial difference in the age of surgery comparing PFA (58 years of mean) and TKA (70 years).1 In our study, the median age was 63 (20 to 78 years).
Early failures in recent studies were attributed to pain (31%), while late failures were a result of OA progression.6,20,21 According to Strickland et al., a 25% of revision surgery were performed in the first year, this was attributed to mechanical failure, infections or pain. Late failures are due to the osteoarthritis advance to the other compartments in our series.6
The most part of PFA replacement in periods over than a year are caused by the progression of osteoarthritis to tibiofemoral compartment causing tibiofemoral osteoarthritis (over 38% in some series). Other causes are pain (16%), septic looseness (14%) or patella maltracking (46%).22 More recent studies pointed at pain as the main cause or arthroplasty replacement to TKA with a percentage of 31% in PFA operated more than a year ago.22
In our series, three knees (50%) were revised to a TKA because of disabling pain due to progression to osteoarthritis. No septic replacement was described in our series. One patient who was unsatisfied with PFA because of unexplainable pain and with major psychiatric problems was rescued with TKA without any improvement on her knee pain. Only one patient (16.66%) was revised to TKA due to patella maltracking. Patella maltracking seems to be in relation with the rotation of the implant according to Hernigou et al.14; the excessive internal rotation of the implant was proportional to the severity of the PF maltracking14 meanwhile no correlation was found between knee injury and osteoarthritis outcome score (KOOS) scores and the amount of external rotation.7
Implant loosening is a rare complication (less than 0.5% at seven years in some series).23 No evidence of component loosening or radiolucencies were observed in our study.
Patellofemoral osteoarthritis is a common knee pathology in our environment with higher prevalence in women as previously has been described in literature1 and agree with our results. This data could be due to the higher incidence of PF malalignment and trochlear dysplasia in women in our series.24
Other important finding of the study is positive correlations found between BMI and the WOMAC, highlining the importance of obesity in relation with the satisfaction with the implant, also in consonancy with the previous literature.25 Even though in literature is clearly described the influence of the BMI in the osteoarthritis evolution; no study has demonstrated if the BMI affects the arthroplasty survival. Some previous studies defended that BMI is not in relationship with the arthroplasty results; meanwhile other recent studies indicated than BMI over 30 (this value categorizes obesity) is in close relation with a worse patient satisfaction with inferior functionality results.25 In our series, 5 of 13 patients with BMI >30 required replacement surgery (38.46%) meanwhile only in 1 of 9 patients (11.11%) with BMI <30 a rescue surgery was performed. A significant positive correlation between BMI and the WOMAC pain (r=0.72, p<0.01) and between BMI and the post-operative VAS (r=0.67, p<0.01) was observed (Fig. 3).
There is also controversy about the influence of the femoral component rotation in the incidence of severity of the patellofemoral complications or pain. Despite no significant correlation was observed between the radiological measurements and postoperative OKS, pre- and postoperative VAS, VAS improvement, WOMAC or Kujala, with 17 implants in external rotation and 4 in internal rotation, Hernigou et al.26 described that increasing amounts of excessive internal rotational malalignment resulted in more severe patellofemoral complications, but they only analyzed the twist angle to study the rotation.
LimitationsThe main limitation of this study is the small n of the sample. This is a retrospective study which only can analyze the OKS, WOMAC, Kujala and EVA pre and post operative interviewing the patients at the moment of the recruitment without control group.
ConclusionsThe results of the case series under consideration suggest that PFA could be an optimal treatment in the joint preservation surgery on the isolated patellofemoral osteoarthritis. This study is limited because of the small size of the sample. BMI >30 seems to be a negative predictor factor in relationship with the postoperative satisfaction, increasing the pain proportionally to this index and requiring more replacement surgery than patients with BMI <30. Meanwhile the radiologic position of the implant is not correlated significantly with the functionality or pain outcomes.
Level of evidenceLevel of evidence III.
FinanciaciónLos autores declaran que no han recibido financiación para la realización de la presente investigación, la preparación del artículo, ni su publicación.
Conflicts of interestThe authors declare that they have no conflict of interest.
Derecho a la privacidad y consentimiento informadoLos autores han obtenido el consentimiento informado de los pacientes y/o sujetos referidos en el artículo. Este documento obra en poder del autor de correspondencia.