The aim of our study is to analyze the different techniques used in arthroscopic treatment of talus osteochondral lesions.
Material and methodWe retrospectively analyzed 73 patients who underwent surgery between 2000 and 2011. Patients were divided in two groups: group A (51 patients), those treated with osteochondral stimulation techniques, and group B (32 patients), that were treated by repair techniques. The mean age was 32.58 (19–73) years in group A and 36.50 (19–58) in group B. It is identified male predominance and medial lesions in both groups.
ResultsWere evaluated according to the AOFAS ankle scoring scale, it is observed a statistically significant clinical improvement (P<.001). Preoperative values were 48.77 (31–67) in group A and 58.08 (41–75) in group B. After surgery scores amounted to 85.19 (60–100) in group A and 93.60 (80–100) in group B.
ConclusionsAnkle arthroscopy is an excellent technique for the accurate staging of osteochondral lesions, and diagnosis and treatment of associated injuries. The arthroscopic treatment of lesions grade i, ii and sometimes iii, by stimulation techniques and chondral lesions grade iii and iv by replacement techniques, gives good results with few complications.
El objetivo de nuestro estudio es analizar las distintas técnicas artroscópicas empleadas en el tratamiento de las lesiones osteocondrales de astrágalo.
Material y métodoRealizamos un estudio retrospectivo de 73 casos, intervenidos entre los años 2000 y 2011. Los pacientes se dividieron en 2 grupos: grupo A (51 pacientes), aquellos tratados mediante técnicas de estimulación osteocondral; grupo B (32 pacientes), tratados mediante técnicas de reparación. La edad media fue de 32,58 años (19-73) en el grupo A, y 36,50 años (19-58) en el grupo B. Se identifica predominio del sexo masculino y de lesiones mediales en ambos grupos.
ResultadosSe evaluaron los resultados siguiendo la escala de la AOFAS de retropié, observando una mejoría clínica estadísticamente significativa (p<0,001). Los valores preoperatorios fueron 48,77 (31-67) en el grupo A, y 58,08 (41-75) en el grupo B. Después de la intervención quirúrgica las puntuaciones ascendieron a 85,19 (60-100) en el grupo A, y 93,60 (80-100) en el grupo B.
ConclusionesLa cirugía artroscópica es la técnica de elección en el tratamiento de las lesiones osteocondrales de tobillo, permite una correcta estadificación y tratamiento de las lesiones asociadas. El tratamiento artroscópico de las lesiones grado i, iiy, en ocasiones iii mediante técnicas de estimulación condral, y de lesiones grado iii y iv mediante técnicas de reparación ofrece buenos resultados con escasas complicaciones (11%).
Talus (or astragalus) osteochondral lesions are rare, affecting 0.041% of the population.1 Most lesions are located laterally and are associated with a history of trauma; however, only 60–80% of medial lesions are attributed to traumatic causes. Lesions in the lateral dome are caused by dorsiflexion associated to inversion, whilst medial lesions are caused by plantar flexion, inversion and external rotation.2
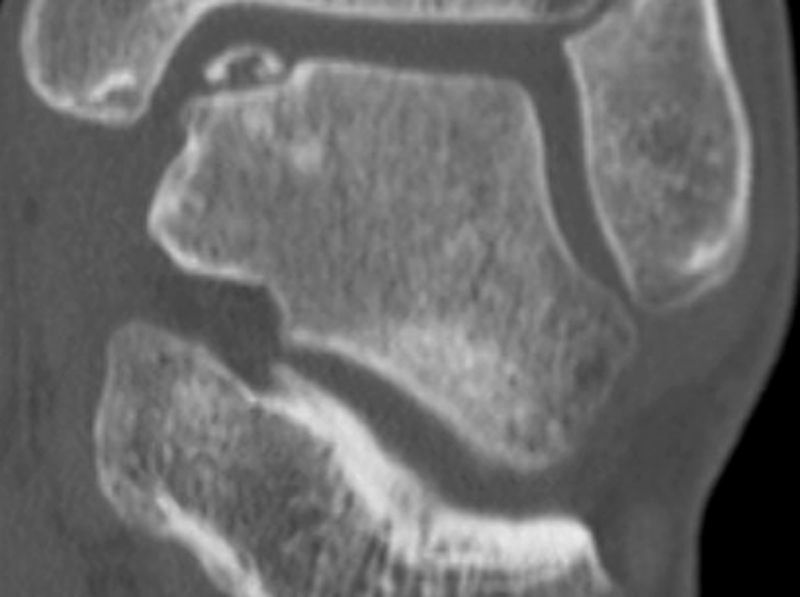
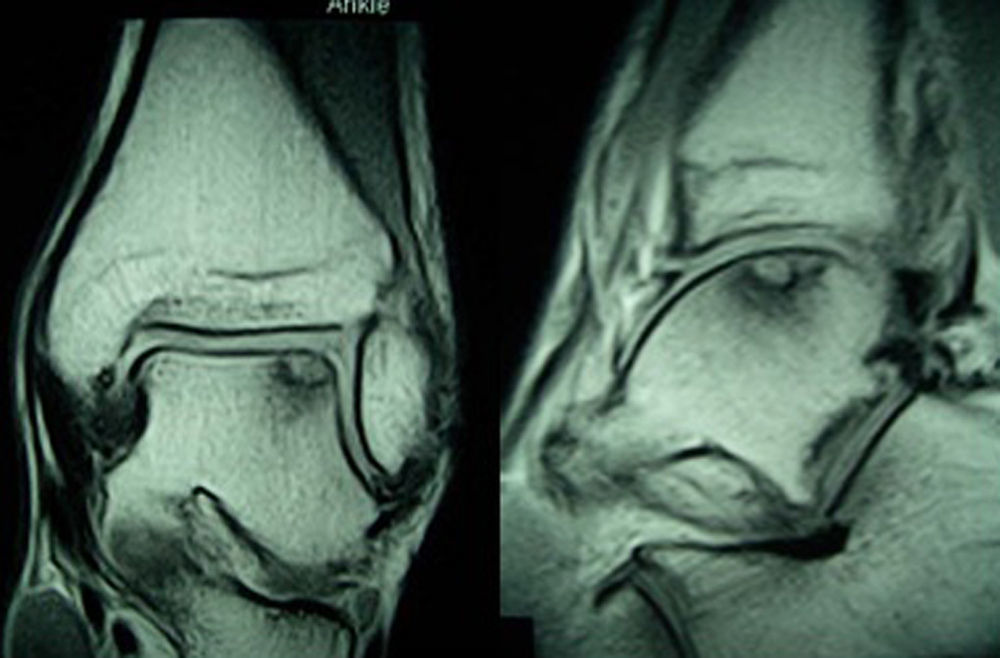
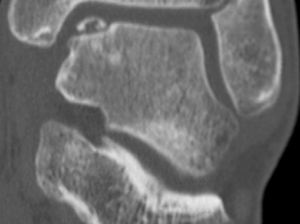
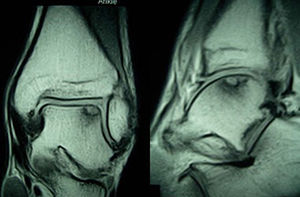
These lesions often go unnoticed initially and most of them evolve toward chronic ankle pain. Diagnosis should be based on symptoms and imaging tests. Some lesions can be detected by simple radiography, but most cases require a computed tomography (CT) scan to be performed. This technique offers the most accurate diagnosis and the best definition of the dimensions of the lesion. A magnetic resonance imaging (MRI) test may also be required. Although this test overestimates the area involved due to its ability to detect associated bone edema, it is very useful to identify associated lesions2 (Figs. 1 and 2).
The astragalus has limited reparative capacity because much of its surface is covered by articular cartilage, which limits vascular contribution.3
Pain does not come from the cartilage lesion; it is most likely caused by increased fluid pressure during walking, which stimulates the richly innervated subchondral bone. Preventing future degeneration depends on various factors, including the repair of the defect and a correct alignment of the ankle joint.4,5
If we consider that we only obtain 45–50% of satisfactory results in patients undergoing conservative treatment, it follows that in many cases we shall have to resort to surgical treatment.6 This can be performed through open techniques or arthroscopic techniques.
We can distinguish 2 approaches to treatment: on the one hand through osteochondral stimulation techniques, and on the other through chondral repair techniques. Osteochondral stimulation techniques include debridement and curettage with or without perforations. Repair techniques include autologous osteochondral transplantation, certain substitutive synthetic implants (TruFit® Angle, OBI) and autologous chondrocyte culture. The choice of technique to be employed should take into account the grade, size and depth of the lesion, as well as the age and functional demands of the patient.7
ObjectiveThe objective of our study is to evaluate the functional and clinical results using the AOFAS (American Orthopaedic Foot and Ankle Society) midfoot scale,8 as well as the complications of the different arthroscopic techniques used in the treatment of osteochondral talus lesions.
Arthroscopic techniquesOsteochondral stimulation- 1.
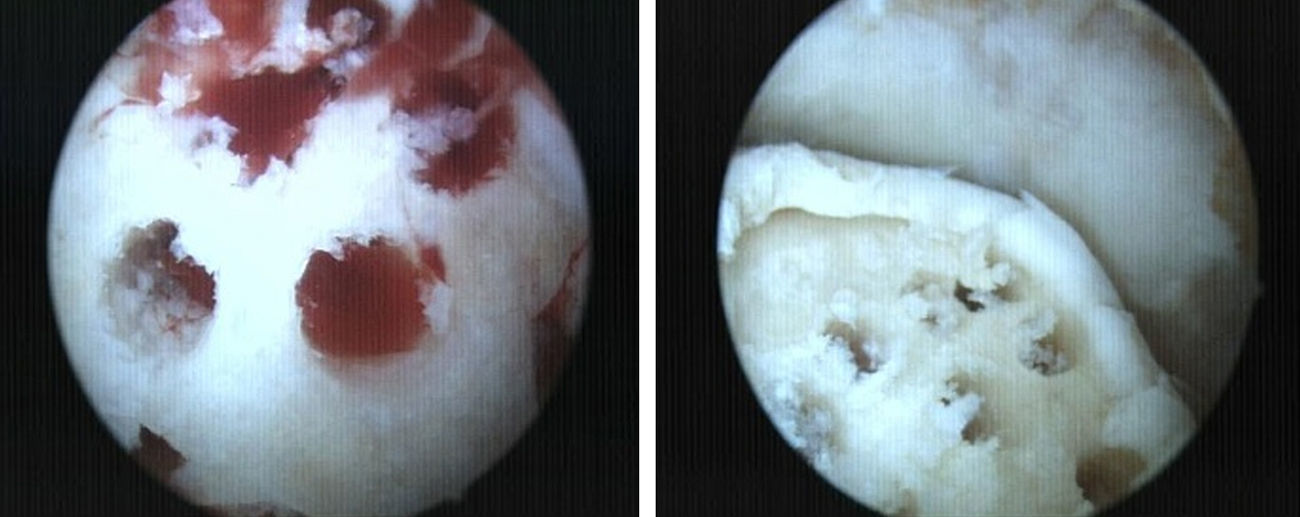
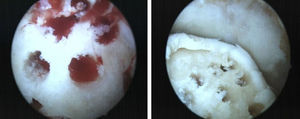
Debridement and curettage: the location of the lesion determined the use of classical anteromedial and anterolateral portals or posterior portals. We proceeded to the removal of the fragment, as well as any devitalized fibrous or cartilaginous debris, and curettage of the lesion surface with a synoviotome or fine arthroscopic mill, producing microfractures.
- 2.
Anterograde and retrograde perforations: the objective was to create vascular access channels to the subchondral bone with medullar elements which stimulated the formation of fibrocartilage which covered the defect.9,10 At present, it is possible to perform perforations through the usual portals or using guides which allow transmalleolar or retrograde perforations in those cases in which extensive areas of bone edema or subchondral bone cysts coexist (Fig. 3).
In cases presenting surface osteochondral defects which are less than 2cm2 in diameter (grade III–IV), we can consider covering the defect with a graft.
- 1.
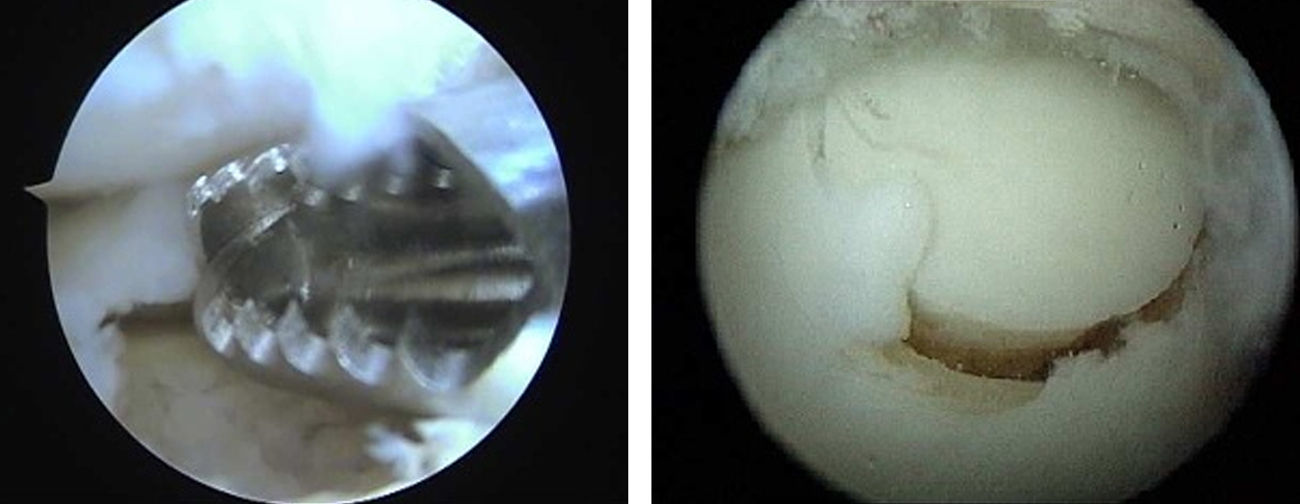
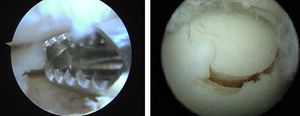
Mosaicplasty: this is indicated in patients younger than 50 years with osteochondral lesions under 2cm2 in diameter and over 5mm deep. It employs osteochondral plugs from non-load areas of the ipsilateral knee (external femoral side or intercondylar notch).11 Like other authors, due to the perpendicularity required by a correct placement of the osteochondral graft and to the axis of curvature of the talus, we favor the use of 2 plugs at most.12 Moreover, it is crucial to verify an absence of friction during dorsal or plantar flexion through arthroscopy (Fig. 4).
- 2.
Synthetic substitute (TruFit® Angle, OBI). OBI plugs are an osteochondral substitute made from a biodegradable and porous material composed of polyglycolic acid (PGA) fibers, calcium sulfate and a copolymer of lactic acid coglycolide. This technique shortens the surgical time and avoids morbidity at the donor site, albeit without offering the same properties as native cartilage.13 They have recently been recalled from the market.
Patients diagnosed with osteochondral talus lesions by imaging techniques, refractory to conservative treatment and intervened through arthroscopic ankle surgery.
We conducted a retrospective study of 73 patients diagnosed with osteochondral talus lesions, intervened using arthroscopic techniques between 2000 and 2011 at the Arthroscopy Unit of the Orthopedic Surgery and Traumatology Service of Doce de Octubre University Hospital in Madrid, Spain.
We identified 84 patients with a diagnosis of osteochondral talus lesion, of which 11 had to be ruled out because they had undergone open surgery. Of the 73 subjects included in the study, 50 patients underwent stimulation techniques (group A); platelet rich plasma (PRP) was used in 4 of them as an adjuvant treatment. Of the remaining 23 patients operated with repair techniques (group B), 20 underwent mosaicplasty and 3 of them underwent repair with a synthetic substitute graft.
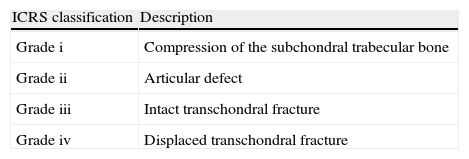
The lesions were classified during arthroscopic surgery, according to the classification of the International Cartilage Repair Society (ICRS),14 which divides osteochondral lesions into: grade I, compression of the subchondral trabecular bone; grade II, articular defect; grade III, intact transchondral fracture, and grade IV, displaced transchondral fracture. We found a small number of grade I lesions (5%), and more lesions of grade II (40%), grade III (25%) and grade IV (30%). Grade I, II and some grade III lesions underwent stimulation techniques, whilst repair techniques were reserved for grade III and IV lesions (Table 1).
Classification of osteochondral lesions according to the International Cartilage Repair Society (ICRS) scale.
| ICRS classification | Description |
| Grade i | Compression of the subchondral trabecular bone |
| Grade ii | Articular defect |
| Grade iii | Intact transchondral fracture |
| Grade iv | Displaced transchondral fracture |
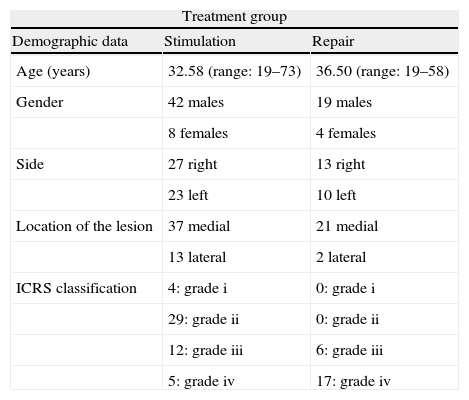
The mean age in group A was 32.58 years (range: 19–73 years), compared to 36.50 years (range: 19–58 years) in group B. We found a larger number of males in both groups (group A: 84.62%; group B: 83.3%). Regarding location, we observed a clear predominance of medial lesions (group A: 76.08%; group B: 91.67%). In terms of laterality, this was fairly similar in both groups, with 46.15% on the left side and 53.85% on the right side in group A and 41.67% on the left side and 58.33% on the right side in group B (Table 2). The demographic characteristics of the sample were statistically comparable. The mean follow-up period was 19.5 months, with a minimum of 11 months (range: 11–34 months).
Demographic data of patients and osteochondral lesions.
| Treatment group | ||
| Demographic data | Stimulation | Repair |
| Age (years) | 32.58 (range: 19–73) | 36.50 (range: 19–58) |
| Gender | 42 males | 19 males |
| 8 females | 4 females | |
| Side | 27 right | 13 right |
| 23 left | 10 left | |
| Location of the lesion | 37 medial | 21 medial |
| 13 lateral | 2 lateral | |
| ICRS classification | 4: grade i | 0: grade i |
| 29: grade ii | 0: grade ii | |
| 12: grade iii | 6: grade iii | |
| 5: grade iv | 17: grade iv | |
Patients were not immobilized postoperatively and began active ankle flexion and extension exercises and hydrotherapy from the time of discharge. In most cases, partial load was initiated after 3 weeks in patients undergoing stimulation techniques, and after 4 weeks in those undergoing repair techniques, with a full load at 8 weeks. Patients who underwent surgery during the initial years of the study followed a slower postoperative protocol, with partial load being delayed for 6–8 weeks.
ResultsClinical assessment was performed using the AOFAS midfoot scale (maximum value of 100 points), whilst associated injuries and complications were also recorded at the same time.
The statistical analysis was performed using the software package SPSS® v.17.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at a 95% confidence interval (P<.05).
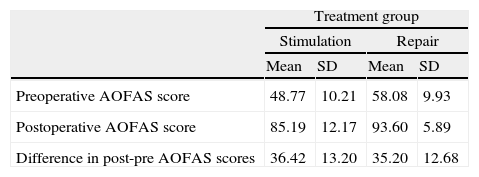
In group A, the assessment of preoperative AOFAS was 48.77 points (range: 31–67 points) compared to 85.19 points (range: 60–100 points) in the postoperative AOFAS. Group B experienced an improvement in the AOFAS score from 58.08 (range: 41–75 points) to 93.60 points (range: 80–100 points). The clinical improvement observed in both groups was statistically significant (P<.001). When comparing the clinical improvement obtained in each group we did not find statistically significant differences (P=.4471) (Table 3).
Comparison between improvement on the AOFAS scale in lesions treated with repair vs substitution.
| Treatment group | ||||
| Stimulation | Repair | |||
| Mean | SD | Mean | SD | |
| Preoperative AOFAS score | 48.77 | 10.21 | 58.08 | 9.93 |
| Postoperative AOFAS score | 85.19 | 12.17 | 93.60 | 5.89 |
| Difference in post-pre AOFAS scores | 36.42 | 13.20 | 35.20 | 12.68 |
SD: standard deviation. Chi-squared test. Difference in post-pre AOFAS: P=.4471.
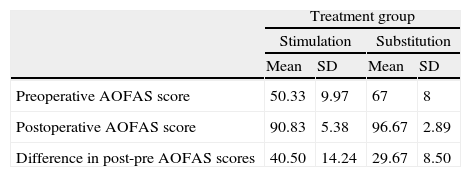
Next, we compared the difference between the results obtained for grade III lesions undergoing stimulation (12 patients) versus those undergoing repair (6 patients). These lesions were similar regarding depth, with a mean value of 7mm (range: 5–12mm). Regarding extension, the range in the stimulation group was 0.7–2.5cm2 in diameter with a mean value of 1.1cm2. In the substitution group, the range of lesions was 1.1–1.9cm2 in diameter, with a mean value of 1.5cm2. No statistically significant differences (P=.1213) in clinical improvement were appreciated in grade III lesions treated by stimulation (preoperative AOFAS: 50.33; postoperative AOFAS: 90.83) compared to those undergoing repair (preoperative AOFAS: 67; postoperative AOFAS: 96.67) (Table 4).
Comparison between improvement on the AOFAS scale in grade III osteochondral lesions treated through stimulation vs substitution.
| Treatment group | ||||
| Stimulation | Substitution | |||
| Mean | SD | Mean | SD | |
| Preoperative AOFAS score | 50.33 | 9.97 | 67 | 8 |
| Postoperative AOFAS score | 90.83 | 5.38 | 96.67 | 2.89 |
| Difference in post-pre AOFAS scores | 40.50 | 14.24 | 29.67 | 8.50 |
SD: standard deviation. Chi-squared test. Difference in post-pre AOFAS: P=.213.
Lastly, we compared patients treated with osteochondral stimulation techniques who were given PRP (preoperative AOFAS: 48.59; postoperative AOFAS: 85.14) versus those who were not given PRP (preoperative AOFAS: 49.75; postoperative AOFAS: 88.50) and found no statistically significant differences, although we must take into account the limitations of the series.
Associated lesions were found in 22% of patients, often after having gone unnoticed in imaging tests and being diagnosed during arthroscopy. In group A (14%) we found 2 cases of instability treated by thermal retensing, 3 lesions of the anterior talofibular ligament (ATL) treated with a peroneus brevis plasty in 2 cases and by arthroscopic homograft in the other, and 2 cases of impingement, 1 in the bone and 1 in soft tissue, which were treated by arthroscopic debridement and resection.
In group B (39%), we observed the following associated lesions: 2 cases of instability treated by thermal retensing and 2 ATL lesions treated with arthroscopic homograft. Moreover, we also found 4 cases of bony impingement and 1 case of soft tissue impingement, all treated by arthroscopic debridement and resection. In 1 patient the MRI led to a diagnosis of peroneal tendon injury, but the arthroscopy revealed peroneus cuartus, which was causing a space conflict that was resolved by tendoscopic debridement.
The rate of complications in our series was low (11%). We observed 4 cases of diffuse disuse osteoporosis: 3 patients in group A and 1 patient in group B. In addition, among patients undergoing chondral stimulation techniques, 2 patients continued to suffer ankle pain and another patient developed arthritis, requiring a total ankle arthroplasty. We only found 1 case of donor site morbidity, with mild pain in the knee of 1 year evolution.
DiscussionFollowing the completion of this study, we observed that both lines of treatment offered satisfactory short-term results with few complications. Therefore, the choice of one technique or the other should depend on the characteristics of the lesion: grade, size and depth, as well as the characteristics of the patient: age and functional demands. Performing an individualized approach and treatment is crucial.
Adequate treatment of talus osteochondral lesions remains a subject of controversy. Most authors15 recommend an initially conservative treatment for grade I and II lesions, and initial surgical treatment for grade III and IV lesions.2,3 As recommended by Zengerink et al.6 and Schuman et al.16 at our center we use conservative measures as the first treatment, despite obtaining poor results.
Zengerink et al.6 and Schuman et al.16 conducted a systematic review of 52 studies of treatment strategies for osteochondral lesions and concluded that arthroscopic excision, curettage and bone marrow stimulation was the preferred treatment for primary talus osteochondral lesions. This technique offers the following advantages: low cost, scarce morbidity, rapid recovery and high success rate.
In 2010, Qin-Wei et al.17 conducted a study seeking predictors of good results in arthroscopic treatment of osteochondral talus lesions through microfractures and found a strong correlation between the size of the lesion and the rate of satisfactory results. The best results were obtained in lesions smaller than 10mm. Considering results such as this, at our center we use substitution techniques in larger lesions. Gender, age, professional sports activities and the location of the lesion were not significantly correlated with the results.
Choi et al.18 conducted a cohort study in which they concluded that advanced age was not an independent risk factor for worse outcomes with arthroscopic perforations. Moreover, they found that, in older patients, traumatic history was less frequent and presented longer duration of symptoms and smaller osteochondral lesions. In our series of patients undergoing stimulation techniques, the mean age was 33.82 years, with a maximum of 73 years, since we did not consider advanced age as an exclusion criterion for stimulation techniques. However, we reserved replacement techniques for patients under 50 years.
In a different line, Hangody et al.19 reported good results using arthroscopic mosaicplasty, obtaining good or excellent final ankle function on the Hanover scale in 36 of 39 patients (94%), with scarce iatrogenic damage at the donor site at the end of a follow-up period of 2 to 7 years. This technique is typically indicated for lesions smaller than 2cm2 in patients younger than 50 years. Associated difficulties include the limited surface that can be covered, thus leaving a dead space between the grafts which must be filled by fibrocartilage. There may also be surface irregularity due to the difference in thickness of the transplanted cartilage.
Osteochondral substitute plugs can also be used as an alternative to osteochondral transplantation. This technique shortens the surgical time and eliminates damage at the donor site, albeit without offering the same properties as native cartilage.
At present, there are studies which associate platelet-rich plasma as a coadjuvant treatment for osteochondral transplantation,20 even employing repeated injections of hyaluronic acid or platelet-rich plasma as an isolated treatment with good results for at least 6 months.21 Due to the small number of patients in our study in whom we used platelet-rich plasma we could not extract significant conclusions.
Despite not being employed at our center, autologous chondrocyte culture has been used since the 90s for lesions greater than 1cm2. It is a costly technique which requires close collaboration with a tissue bank and which has the disadvantage of requiring surgery to be performed in 2 stages. Nevertheless, it has shown highly satisfactory results in recent years. Niemeyer et al.22 published a meta-analysis including 16 studies which concluded that, despite the promising results of the technique, further randomized and controlled trials were required to demonstrate its superiority or inferiority with respect to microperforations and transplants.
The study conducted at our center has limitations, as it was a retrospective study with a mean follow-up period shorter than 2 years. Satisfactory results were obtained in both treatment groups.
Our therapeutic algorithm for the treatment of osteochondral lesions was the following: osteochondral stimulation techniques for grade I–II–III lesions and replacement techniques for grade III–IV lesions, taking into account the characteristics of both patients and lesions, as well as the experience and preference of the surgeon. We opted for treating grade III lesions through repair techniques when the size of the lesion was less than 2cm2 and the depth was greater than 5mm, in patients younger than 50 years. Likewise, we can say that there were no statistically significant differences in clinical improvement observed with one technique over the other, in the same way that Gobbi et al.23 found no statistically significant differences in their prospective randomized study (level of evidence I) comparing chondroplasty, microfractures and osteochondral allografts.
We were able to achieve both diagnosis and treatment of associated injuries, often not diagnosed by CT or MRI scans. When we analyzed the scientific evidence published in the literature, we found a level of evidence B regarding the role of arthroscopic techniques in the treatment of osteochondral talus lesions.24,25 Further long-term, prospective, randomized studies with more cases would be required in order to evaluate the possible superiority of chondral stimulation versus chondral substitution techniques or vice versa.
ConclusionsWe consider arthroscopic ankle surgery as an excellent technique for the accurate staging of osteochondral talus lesions, which are occasionally difficult to differentiate through imaging techniques.
Both lines of treatment offered satisfactory results with few complications. The choice of one technique or another should depend on the characteristics of the lesion: grade, size and depth, as well as the characteristics of the patient: age and functional demands.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
FinancingThis study employed no sources of financing.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mellado-Romero M., et al. Tratamiento artroscópico de las lesiones osteocondrales de astrágalo: estudio de 73 casos. Rev Esp Cir Ortop Traumatol. 2013;57:224–30.