Acetabular revision surgery is a challenge due to the appearance of bone defects that make primary fixation of implants difficult when extracting loosened components. Reinforcement rings, such as Burch-Schneider (BS), have been shown to be allies in moderate or severe bone defects. The objective of the study is to evaluate the results and survival of these types of implants in acetabular revision surgery in the medium follow-up.
Material and methodsRetrospective study on a cohort of 64 patients (67 replacements) with BS rings associated with morselized bone allografts in a 2 years minimum follow-up. Data were collected regarding clinical outcomes, graft incorporation, implant mobilization, survival and complications.
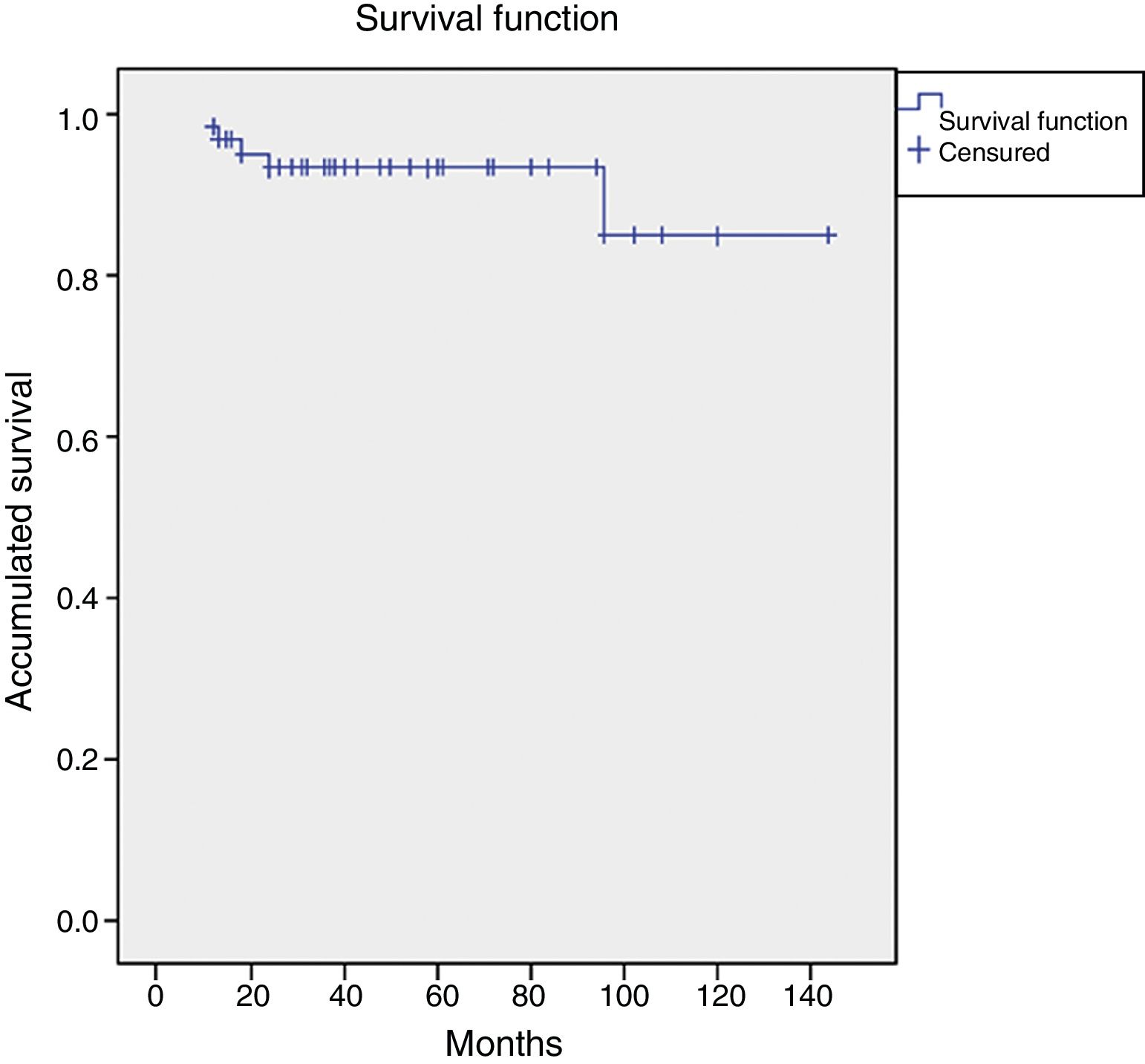
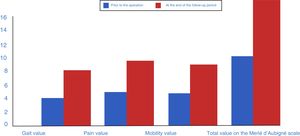
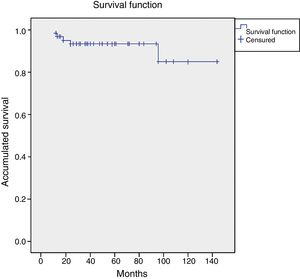
ResultsThe mean follow-up was 5.06 years (R=2.2–12). The Merle scale improved from 8 points to 15 points at the end of follow-up (p<.0001) with 76.11% of good or excellent results. Reproduction of the anatomical centre of rotation was associated with a better result (p<.05). There was total or subtotal incorporation of the bone allograft in 97% of the patients, although this did not prevent a significant migration of the ring according to Gill criteria in 6 cases. We observed an overall survival of the implant for any cause of 93.4% at 5 years, and 84.6% at 10 years.
ConclusionsThe BS reinforcement ring shows good results in the medium and long term enabling anatomical reconstruction in revision surgery as well as replacement of the bone stock. These results are also comparable and are a vast improvement on other rings.
La cirugía de revisión acetabular supone un reto por la aparición de defectos óseos que dificultan la fijación primaria de los implantes al extraer los componentes aflojados. Los anillos antiprotrusivos, como el de Burch-Schneider (BS) se han mostrado como aliados en defectos moderados o severos. El objetivo del estudio es evaluar resultados y supervivencia de este tipo de implantes en recambios acetabulares a medio plazo.
Material y métodosEstudio retrospectivo sobre una cohorte de 64 pacientes (67 recambios) con anillo de BS asociado a injerto triturado con un seguimiento mínimo de 2 años. Se recogen los datos relativos a resultados clínicos, incorporación de injertos, movilización de los implantes, supervivencia y complicaciones.
ResultadosEl seguimiento medio fue de 5,06 años (R=2,2-12). La escala de Merlé pasó de una mediana de 8 puntos a una mediana de 15 puntos al final del seguimiento (p<0,0001), con un 76,11% de resultados buenos o excelentes. La reproducción del centro de rotación anatómico se asoció con un mejor resultado (p<0,05). Se produjo incorporación total o subtotal de los injertos en el 97% de los pacientes, aunque esto no impidió una migración significativa del anillo según criterios de Gill en 6 casos. Se constató una supervivencia global del implante para cualquier causa del 93,4% a 5 años y del 84,6% a 10 años.
ConclusionesEl anillo de BS presenta buenos resultados a medio y largo plazo permitiendo una reconstrucción anatómica en cirugía de revisión, además de permitir una reposición del stock óseo, estos resultados además son comparables y mejoran ampliamente a otros anillos.
The increase in the population's life expectancy is bringing about a rise in the number of prosthetic exchanges and a gradual increase is foreseen.1 In most cases the failure of primary surgeries is due to an aseptic loosening of the components, with mobilization due to infectious processes, instability or peri-prosthetic fractures being less common.2 Revision surgery for hip arthroplasties implies an increase in the complexity of the surgery if we take into account the associated bone defect, particularly at the acetabular level and the low quality of the remaining pelvic bone in generally elderly patients.
Numerous methods have been described for handling major and massive bone defects. Some include materials to supplement the lack of bone reserve in acetabular revision surgery. Thus we can find cases of giant or oblong cups, impacted bone grafts, massive structural allografts, trabecular metal (TM) or acetabular reconstruction rings.3–5 The degree of bone deficiency and the degree of contact between the host bone and the implant is the fundamental principle for assessing the technical to be applied and will ensure a good outcome for the revision surgery.6
Reinforcement rings have emerged in an attempt to improve biomechanical stability in acetabular review surgery on a deficient bed.7,8 These implants have a protective effect on bone grafts by improving their incorporation through diminishing the tension to which they are subjected, and distributing the loads towards the periphery.9 They are considered to be essential when the graft surface is greater than 50% of the support area for the implants. In these cases, it is necessary to use rings presenting iliac anchorage, using a hook or even screwing them in place. The Burch-Schneider ring (BS), initially described by Burch and modified by Schneider, is currently made of titanium and has two anchorage areas, one for the ilium, to which it is attached by screws, and a hook that is placed intraischiatically. Although their use has reduced somewhat, very good outcomes have been described with the use of these implants in long-term series.10–12 The purpose of this study is to evaluate the outcomes and the medium- and long-term survival of acetabular review surgery with the use of an anti-protrusive BS ring associated with a morselized and impacted graft.
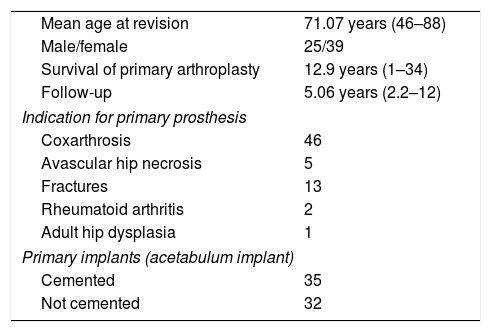
Material and methodsLongitudinal retrospective study of a series of patients subjected to hip revision surgery between March, 1999, and December, 2012. Out of a total of 239 acetabular revision surgery cases, those who met the criteria for inclusion, revision with anti-protrusive ring, addition of morselized and impacted bone allografts, and a minimum of 2 years’ clinical and radiological follow-up were included. Out of the total sample, these criteria were met by 67 hips in 64 patients. Of the 64 patients in this series, we found 25 males (39.60%) and 39 women (60.40%) with a mean age of 71.07 years (46–88) at the time of surgery. The mean follow-up period was 5.06 years (2.2–12).
The initial diagnosis determining primary arthroplasty was coxarthrosis in 46 cases, fractures in 13 cases, avascular necrosis in 5 hips, 2 cases of rheumatoid arthritis and a single case due to dysplasia of the hip as a sequela of childhood polio. The indication for revision surgery was aseptic loosening in 58 hips, septic loosening in 2 cases and recurrent dislocation in 7 cases. The mean survival of the primary implant was 12.9 years (1–34). There was great variability in the implants used (Table 1).
Summary of the sample's demographic details.
| Mean age at revision | 71.07 years (46–88) |
| Male/female | 25/39 |
| Survival of primary arthroplasty | 12.9 years (1–34) |
| Follow-up | 5.06 years (2.2–12) |
| Indication for primary prosthesis | |
| Coxarthrosis | 46 |
| Avascular hip necrosis | 5 |
| Fractures | 13 |
| Rheumatoid arthritis | 2 |
| Adult hip dysplasia | 1 |
| Primary implants (acetabulum implant) | |
| Cemented | 35 |
| Not cemented | 32 |
Preoperative images and intraoperative findings were used to evaluate and classify acetabular bone defects. As per our experience, we used the classification by Paprosky et al.6 As is well known, this is based on an anterior–posterior X-ray of the hip generating four criteria that determine the degree of bone defect present in the acetabulum.
All of the revision surgeries were performed by 2 surgeons (FS and JA) more frequently using the Watson-Jones route (73.13%), followed by the amended Hardinge-Bauer route (23.8%); the Kocher-Langenbeck posterior-lateral route was used in one case. A BS-type implant (Zimmer, USA) was used with 2 ring sizes: small (44), 86.5% and large (50), 13.5%, with a median of 4 screws (3–7) to the ilium. The hook was positioned intraischiatically in 89.4% of the case (61 cases). For the infill of the bone defects, compacted morselized bone allografts were used. The mean graft used was 95cm3 (30–180cm3). Until 2005, we used grafts from the hospital's own bone bank with intra-operative shaping; since that year, we used to spongy grafts from the blood and tissue bank of Aragon, in both cases with prior washing and freezing; the size of the shaping was not altered and direct impacting was performed. An “allpoli” Muller-type implant (Biomed®, USA) was cemented on the ring in 60 cases, along with 2 Exeter-type (Stryker®, the Netherlands) and 5 Trident-type constrained rings (Stryker®, the Netherlands). Antibiotic cement was used in all cases. The friction torque was polyethylene metal in all cases. In 17 cases, it was also necessary to perform a replacement of the femoral rod at the same time; for this revision surgery, a Modular Plus implant (Smith & Nephew®, Switzerland), was used in 14 cases, with porous diaphyseal anchorage and a long, cemented Exeter-type implant (Stryker®, the Netherlands) in 3 cases.
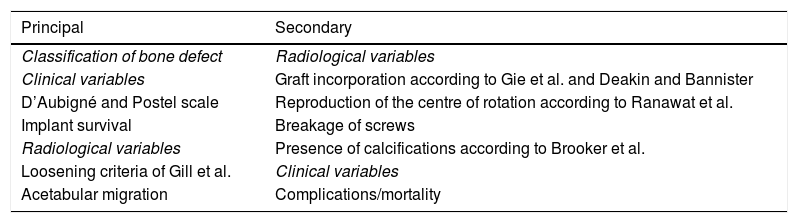
Clinical and radiological evaluationAn assessment was made at each visit using the d’Aubigné and Postel hip scale13 and radiological observations and measurements were taken. A summary of the variables can be seen in Table 2. A score of 18 points on the clinical scale was considered excellent, between 17 and 14 points was a good outcome, between 13 and 11 points was so-so and less than 11 points was considered a poor outcome.
Scheme of primary or principal and secondary variables studied.
| Principal | Secondary |
|---|---|
| Classification of bone defect | Radiological variables |
| Clinical variables | Graft incorporation according to Gie et al. and Deakin and Bannister |
| D’Aubigné and Postel scale | Reproduction of the centre of rotation according to Ranawat et al. |
| Implant survival | Breakage of screws |
| Radiological variables | Presence of calcifications according to Brooker et al. |
| Loosening criteria of Gill et al. | Clinical variables |
| Acetabular migration | Complications/mortality |
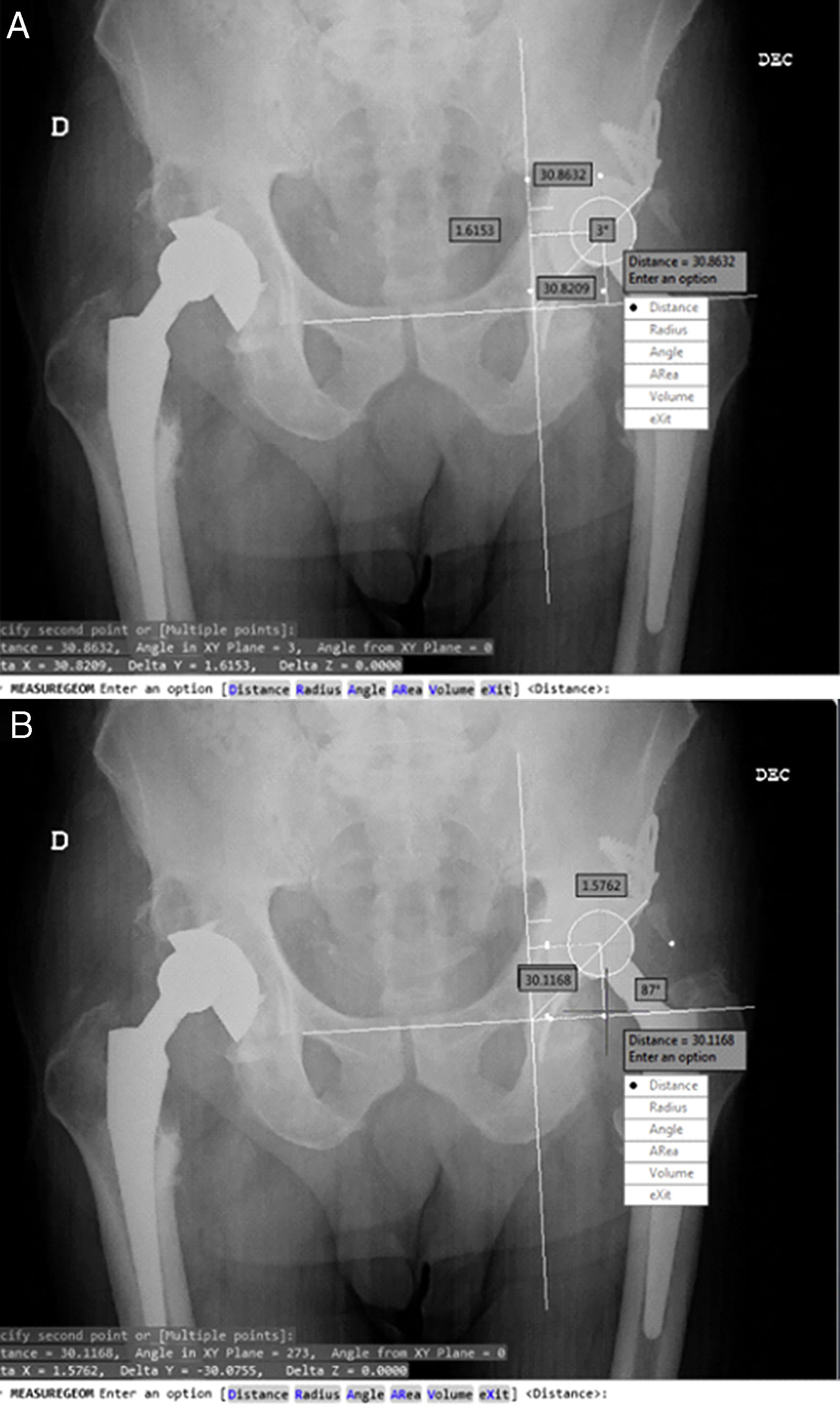
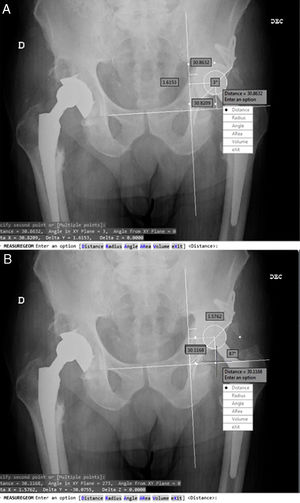
The reproduction of the rotation centre and the migration of the acetabular component were determined using post-operative measurements after 6 months, 1 year and at the end of the follow-up period using AP X-rays focused on the pelvis. The method of Ranawat et al.14 was used to determine the theoretical centre of rotation. For the evaluation of acetabular migration, we used the system described by Peters et al.,7 which takes as its reference the horizontal line connecting the lower margin of the teardrop and its distance to the centre of the head of the prosthesis (vertical distance) and the vertical line passing through the medial edge of the teardrop and its distance to the centre of the head of the prosthesis (horizontal distance). The system also allows measurements of the acetabular angle (Fig. 1). Measurements were taken using the automatic dumping of the images into the Autodesk® AutoCAD® 2013 system, with resampling of the images through the known size of the femoral head.
Furthermore, the degree of incorporation of the bone allografts was evaluated using the system described by Deakin and Bannister15 and by Gie et al.16 in a simple X-ray after 6 months, 1 year and at the end of the follow-up period, with the appearance of trabeculae crossing the graft area being interpreted as the complete incorporation of the graft. Osteolysis of the acetabular component was evaluated in the areas described by DeLee and Charnley17 and the presence of heterotopic calcifications was assessed using the system of Brooker et al.18
At the end of the follow-up period, the X-rays were compared with the X-rays immediately after the operation, and consideration was given to migration by the component of more than 5mm in the vertical or horizontal planes, the presence of continuous radiolucency, a change of more than 5° in the acetabular inclination or the presence of breakage in the ring's screws or hook determined the failure of the implant in accordance with the criteria of Gill et al.19
Statistical analysisWe used the SPSS® v.15.0 software package (SPPS, Chicago, IL, USA) for statistical analysis. Student's t-test was used to analyze the means in the clinical tests, and variables were also categorized and analyzed using the Chi-squared test with respect to the clinical outcome for graft incorporation parameters. The general level for significance was 5%. Survival curves were drawn up using Kaplan–Meier. The performance of revision surgery was considered to be a failure due to any mechanical failure in the surgery, infection or recurrent dislocation.
ResultsOf our 67 hips, according to the classification of Paprosky et al.,6 3 were cavitation defects (type I), 9 presented greater bone loss (presented a loss of the upper ring (type IIB), 19 presented loss of the medial wall and teardrop with the integrity of the columns (type IIC), 18 patients had a type IIIA defect (lysis in excess of 3cm with Köhler's line intact or inflated, lysis of less than 15mm in the ischium and partial destruction of the teardrop) and only 2 patients presented a major type IIIB defect.
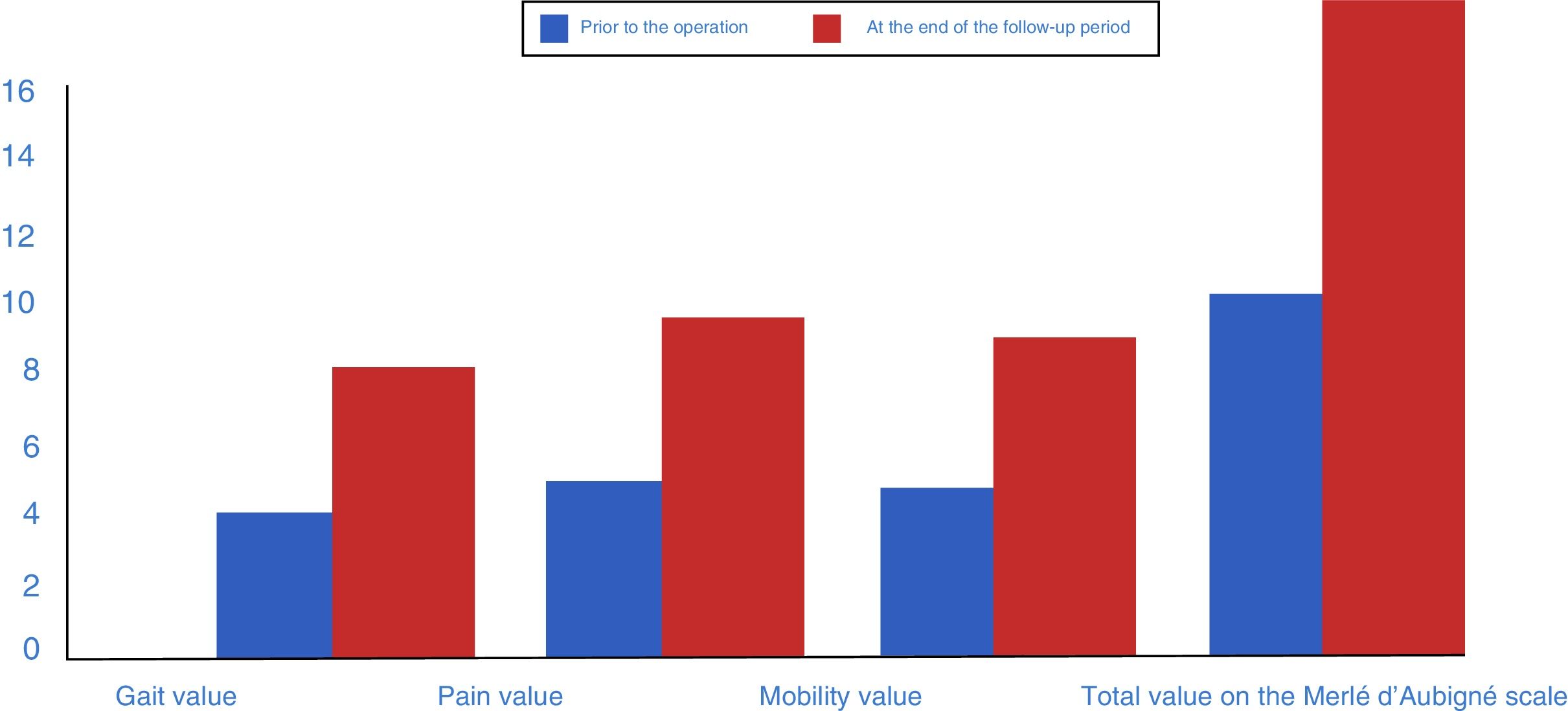
Radiological and clinical outcomes and complicationsFrom a clinical perspective, we observed a significant improvement in post-operative values compared to pre-operative values using the d’Aubigné scale. These went from 8.43 (R=5–15; median: 8) to 14.29 (7–18; median: 15) at the end of the follow-up period, p<.0001. Quantitatively speaking, the gait scale increased by a median of 2 points, pain by a median of 3 points and mobility by a median of 2 points. All of the above implied a statistically significant difference between the pre- and post-operative functional values with p<.001. In 11 patients, the outcome was considered excellent, in 40 cases it was good, the result was so-so in 12 cases and 4 had poor outcomes (Fig. 2). The initial bone defect did not have any impact on the clinical outcome at the end of the follow-up period (p=.303). No surgery-associated vascular or nerve lesions were noted.
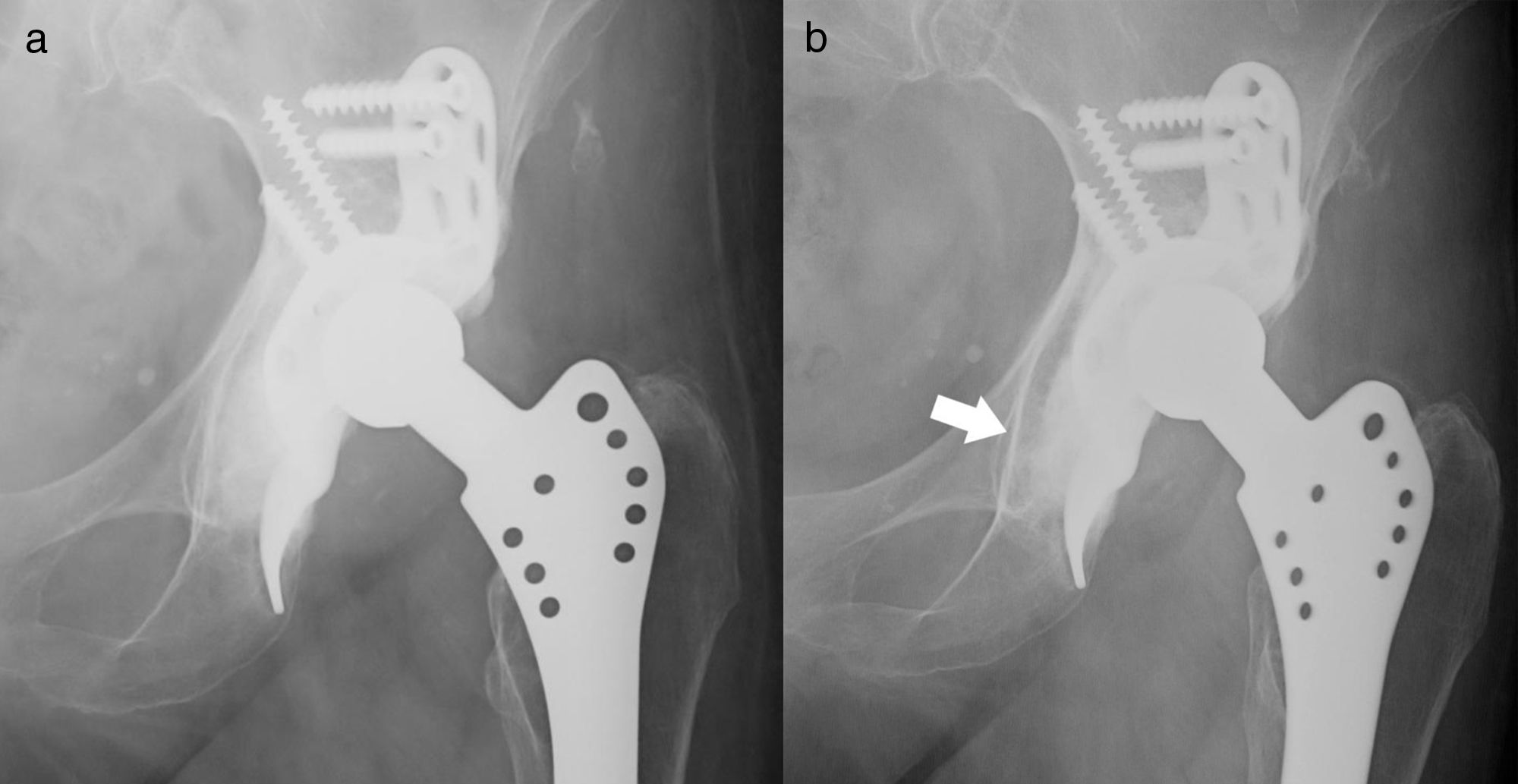
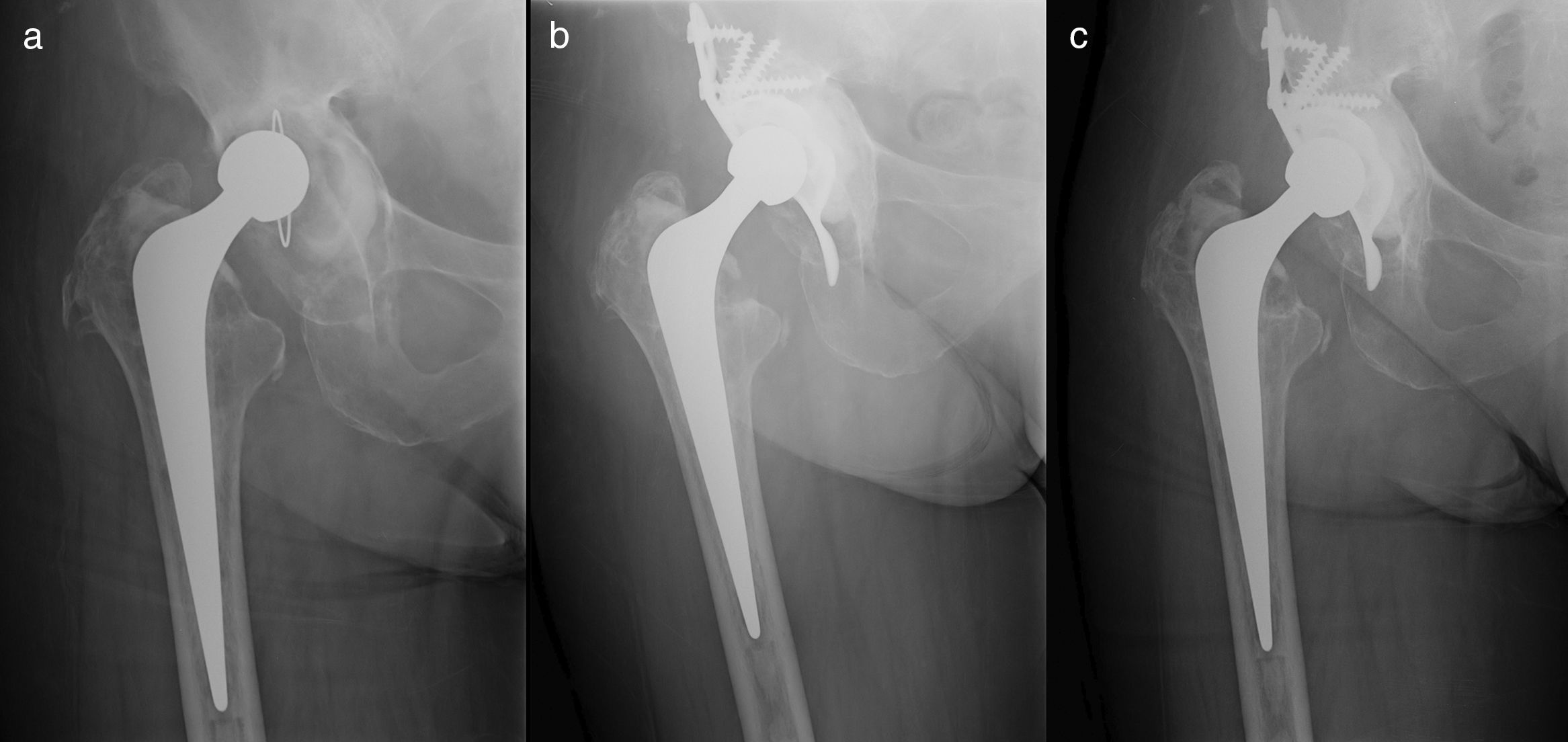
With respect to the integration of the graft 6 months after surgery, we observed total or sub-total apposition (grades II or III of Gie et al.) in 64 hips (34 grade II, 30 grade III) with absence of changes in 3 patients. One year after surgery, total or sub-total apposition was seen in 65 hips (8 grade II, 57 grade III) with only 2 patients not presenting any differences with respect to the initial X-ray (Fig. 3). Applying the theory of Deakin and Bannister, the outcomes are similar, with observation after one year of partial reabsorption of the graft in 2 patients with complete trabeculation in the remaining 65 hips (Fig. 3). The volume of the graft did not influence its incorporation (p=.582). The presence of graft incorporation did not reflect any differences with regard to the implant's survival (p=.211).
After applying the method of Ranawat et al., we observed that it had been possible to restore the hip's anatomical centre of rotation in 61.19% of patients (41 cases). The largest percentage of those who did not achieve this was due to raising the centre of rotation significantly (more than 5mm); only in 3.2% was the centre of rotation considered to be lateralized with respect to its theoretical anatomical centre. The reproduction of the centre of rotation achieved a significantly higher number of good and excellent outcomes versus not achieving it (p=.047). The reproduction of the centre of rotation was not influenced by the initial bone defect (p=.477). Migration of the ring was measured in the X-ray after the operation and at the end of the follow-up period. Following the scheme proposed by Peters et al., a mean migration of 1.5mm was observed in the horizontal plane (from 3.30 medial to 3.41 lateral), 2.28mm in the vertical plane (from 8.18mm cranial to 7.41mm caudal) and 1° of inclination in the ring. The degree of graft incorporation, the number of screws associated with the ring or the presence of breakage in the screws did not significantly change the degree of mobilization of the implants (p>.05).
At the end of the follow-up period, it was seen that 41.8% (28/67) of the patients presented Brooker grade I, 36.7% (21/67) grade II, 13 patients (19.4%) presented major grade III ossifications, 2 patients presented intermediate grades (2/3 and 3/4), one patient (1.5%) apparently presented grade IV ossification with ankylosis of the hip. With regard to the complications during the follow-up, we observed a peri-prosthetic fracture of the femur, 4 dislocations, 3 infections of the surgical wound, one mobilization of the femoral rod. One patient suffered a deep infection that did not clear up despite lavage, change mobile components and suppression of antibiotics. Of the dislocations, 2 remained recurrent and had to be changed again. 17.1% of patients (11/64) died during follow-up for reasons unrelated to the revision.
Analysis of failures and survivalsDuring follow-up, there were 5 acetabular revisions, 2 due to mechanical failure of the implant, 2 due to relapsing dislocations, and one due to deep infection. If we apply purely radiological criteria, according to those of Gill et al., 6 cases were considered to be mobilized, 2 of them with breakage of screws and 4 presented radiolucency at the level of the ring hook and were considered potentially loosened. However, only 2 patients presented compatible clinical symptoms for a change to be carried out. The rest of the series did not present radiological changes (Fig. 4). According to Paprosky et al., the initial defect (p=.062) and the degree of graft incorporation (p=.14) did not significantly change the survival of the implants.
In the analysis of the Kaplan–Meier curve for the revision of implants for any reason, the accumulated survival after 5 years was identified as 93.4%. Ten years after surgery, the survival would be 84.6% with an upper limit of 144 months, a lower limit of 123 months, and a confidence interval of 95% (Fig. 5).
DiscussionDealing with the failure of acetabular implants has been one of the warhorses of orthopaedic surgery and its difficulty lies in that we have to replace the bone loss arising prior to revision surgery. The type of bone defect associated is going to determine the type of revision and its survival.12 Our study shows good functional outcomes and a high level of survival for implants of this type associated with impacted grafts regardless of the type of initial bone defect.
According to our data, the d’Aubigné and Postel scale went from a median of 8 points preoperatively to a median of 15 at the end of the follow-up period, with 77% of good or excellent outcomes in our series. Coscujuela et al. reported a shift from 8.8 to 15.1 points on average at the end of the follow-up.11 Symeonides et al.20 had an improvement from 9.7 to 15.5 in the post-operative period. In addition, as in our series, the parameter that most improved was pain which went from 2.6 to 5.1 (in our case from 3.1 to 5.43) and the one with the least improvement was mobility which went from 3.5 to 4.8 (in our case from 2.9 to 4.8). In 2001, Perka et al. presented a series with somewhat inferior outcomes and a d’Aubigné and Postel categorized as excellent or good in 63.3% of cases, satisfactory in 28.8% and poor in the rest.21 As in our series, other authors have found that the reproduction of the anatomical centre of the hip improves functional results and might definitively affect the survival of the implants in both primary arthroplasty and in revision surgery.22,23 This would be due to a fall in the stresses in the implant by reproducing the mechanics of the native hip.22
The association of an impacted graft with the ring has improved the outcomes of the revision surgery with rings.12 Graft incorporation was complete in 97% of our patients, although this figure varies between 80 and 100% in the published series.8,9,24,25
The evaluation of early migration of the ring may give is an idea of the initial stability of the implants, and has even been identified as a prognostic value in replacement surgery. A greater incidence of migration has been described in revision surgery. Ilchmann et al.26 described significant migration in 10% of their sample, more than 3mm, and complete mobilization in 7% of their sample. They presented breakage of screws in 20% of cases, with significant impact on survival in that group compared to those with no breakage. They concluded that the early migration of implants is a determining factor for migration, breakage of screws and revision of implants. Van der Linde27 and had already described significant migration in 5 there are 42 patients, concluding that this migration slows down after 2 years following surgery. The series of Pieringer et al.28 presents a trend similar to ours. Of their 66 patients, 20.3% presented migration in excess of 1mm and in 5 cases they considered the migration to be significant at more than 5mm. In the study of our 64 patients (67 replacements), we found only one revision due to aseptic loosening after 5 years. At the end of the follow-up period, in addition to another revision due to loosening, 6 cases presented mobilization according to the criteria of Gill et al. without meeting clinical criteria for replacement. The migration of the ring may occur in any direction. This generates a paradox because the most logical result would be for migration to be exclusively medial and cranial due to the forces applied to the implant. However, lateral migration had already been described by Ilchmann et al.26 In the case of caudal migration, as they themselves discuss, there is no reason and it is probably due to a failure in the interpretation of the X-ray or in its performance.29 According to our results, we believe that there is an initial migration of implants that might reach significance or might stop with respect to multifactorial aspects (integration, mechanical stability, type of defect, etc.) hence the heterogeneity of the outcomes and their lack of significance.
Survival with this type of implant has been compared to other techniques. Thus, Böhm and Banzha30 compared outcomes with the BS, Müller and Harris Galante rings, finding a greater survival in BS, in cases of loosening, compared to the other rings, with a survival of 94% after 11 years in BS, 89% after 13 years in Müller rings and 73% after 8 years in Harris rings. Jones et al. report survival after 9 years of 95.5% in their series of 29 patients.31 Coscujuela-Mañá et al., however, presented survival indices of 92.4% after 13 years with only 3 loosenings in their series of 91 patients with anti-protrusive rings.11 In terms of major defects, the outcomes can be affected as described by Marx et al. With 88% survival after average follow-up of 4.5 years.32 Despite these figures, new techniques and materials are coming to the fore and the first comparative studies between anti-protrusive rings and TM have begun to appear. A meta-analysis by Beckman et al.33 concludes that the biomechanics of TM favours their integration by reducing their loosening rate. These authors highlight the appearance of statistically significant differences in the survival of TM implants versus anti-protrusive rings. Nonetheless, when conducting an in-depth analysis, this meta-analysis is based on observational studies with a short follow-up and must be confirmed in future by studies with greater validity. In our opinion, the decline in the use of anti-protrusive rings is fundamentally due to the technical difficulty, the need for extensive approaches, and the appearance of new implants that might simplify revision.
This study has certain limitations that we should like to highlight: (1) The cohort is not very extensive and some have been lost during follow-up; (2) The follow-up period prevents powerful conclusions being drawn particularly with regard to the loosening of implants; (3) The systematic use of X-rays may give rise to biases since, despite the assistance of software, it is difficult to evaluate millimetric migrations and predict implant failure; and (4) There is no control group in which other techniques been used.
Despite these limitations, in view of our outcomes with a significant improvement in function and survival of 84.6% after 10 years, we can conclude that the use of the BS anti-protrusive ring associated with grafts is a reproducible technique with a high survival rate and a very low complications rate. Long-term follow-up will be required to confirm these outcomes.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments have been conducted for this research in human beings nor in animals.
Data confidentialityThe authors declare that no patient data are contained in this article.
Right to privacy and informed consentThe authors declare that no patient data are contained in this article.
Conflict of interestThe authors present no conflict of interest with the results of this study.
Please cite this article as: Torres-Campos A, Albareda Albareda J, Seral García B, Blanco Rubio N, Gómez Vallejo J, Ezquerra Herrando L. Anillo de Burch-Schneider asociado a injerto óseo triturado, supervivencia y resultados clínicos en revisión acetabular. Rev Esp Cir Ortop Traumatol. 2018;62:428–435.