The treatment of a chronic rupture of the Achilles tendon remains difficult. Different techniques such as augmentation or plasties are used for restoring the gap in these ruptures. The combination of Achilles tendon rupture with other tendon ruptures may increase the difficulty in their treatment. We present a rare combination of a delayed Achilles tendon rupture and a peroneus brevis tendon rupture and its management. The importance of the presented case is the combination of both ruptures that adds difficulty to the surgical technique. A thorough analysis should be made of the magnetic resonance findings when planning a tendon transposition. To our knowledge, there are no reports of a simultaneous combination of an Achilles tendon rupture and a peroneus brevis tendon rupture.
El manejo de una rotura crónica de tendón de Aquiles es un desafío. La mayoría de los cirujanos optan por técnicas de aumentación para prevenir nuevas roturas. La presencia de otras lesiones de forma simultánea a la rotura del tendón de Aquiles puede hacer más difícil su tratamiento. Presentamos el caso de un paciente afecto de una rotura crónica de tendón de Aquiles. Se planificó realizar una transposición del tendón peroneus brevis, observándose intraoperatoriamente una rotura concomitante de dicho tendón que obligó a modificar la técnica. Consideramos que la importancia del caso que se presenta es que la asociación de ambas roturas añade dificultad a la técnica de reconstrucción para el tratamiento del defecto del tendón de Aquiles. Al realizarse una planificación preoperatoria, debería llevarse a cabo un análisis exhaustivo de los hallazgos de la resonancia magnética para confirmar la integridad de los tendones a utilizar durante la técnica de reconstrucción. No se ha encontrado en la literatura consultada la asociación de rotura del tendón de Aquiles y del peroneus brevis.
For the majority of surgeons, treating chronic Achilles tendon rupture (ATR) is still a challenge. The literature contains different adjectives to describe this complaint: neglected, chronic, delayed, old and late ruptures.1 The question of when a rupture should be considered is chronic is also controversial, and 4 weeks is the criterion used the most often.1 Although direct suture is the best repair option, it is hard to perform this in chronic ruptures. Many techniques have been described to restore the length and strength of the tendon following this injury. The majority of surgeons use augmentatin techniques to prevent new ruptures: a free flap of gastrocnemius aponeurosis, a free semitendinosus graft, tendon transfer (flexor hallucis longus [FHL], flexor digitorum longus, peroneus brevis [PB], peroneus longus, thin plantar) and finally, allografts.1–4
The simultaneous presence of other lesions may hinder the treatment of ATR. We found at least 6 different associations with acute ATR in the published literature: peroneal melleolus, tibial malleolus, open ankle fracture, fracture of the talus neck, upper peroneal retinaculum lesion and avulsion of the calcaneofibular ligament.5–10
Nevertheless, no combination of chronic ATR with other lesions was found in the literature. This paper presents a combination of chronic ATR with PB rupture.
Clinical caseWe present the case of a 40 year-old male patient who suffered a sprained left ankle while walking up stairs. Relevant factors are that the patient was significantly obese and did not mention repeated sprains, and the ankle was normo-axed. He did not visit the doctor until 2 months after the accident due to persistent pain. The initial examination found pain in the Achilles tendon and a positive Thompson. Magnetic resonance (MR) imaging showed ATR with a separation between the ends of 5cm.
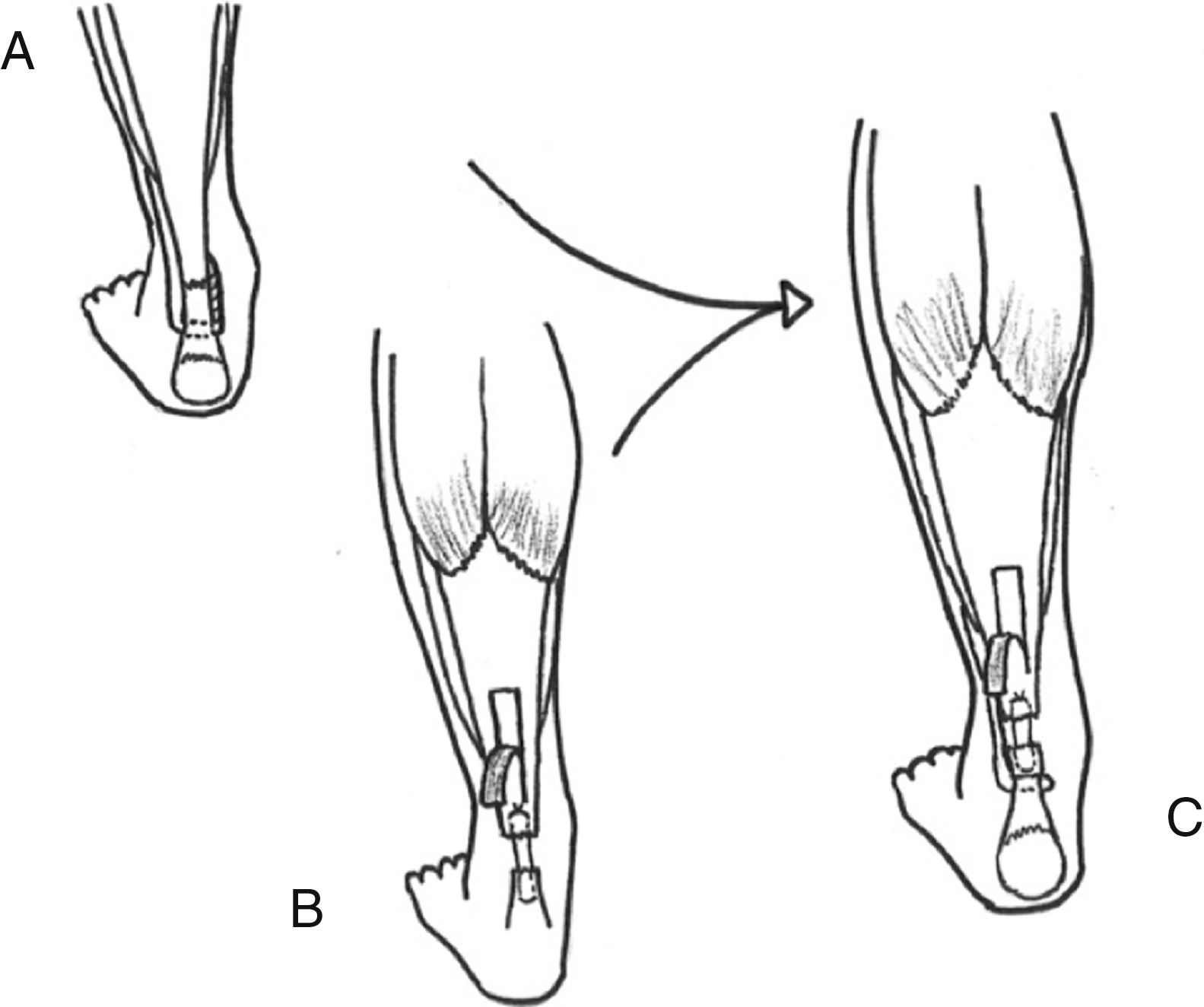
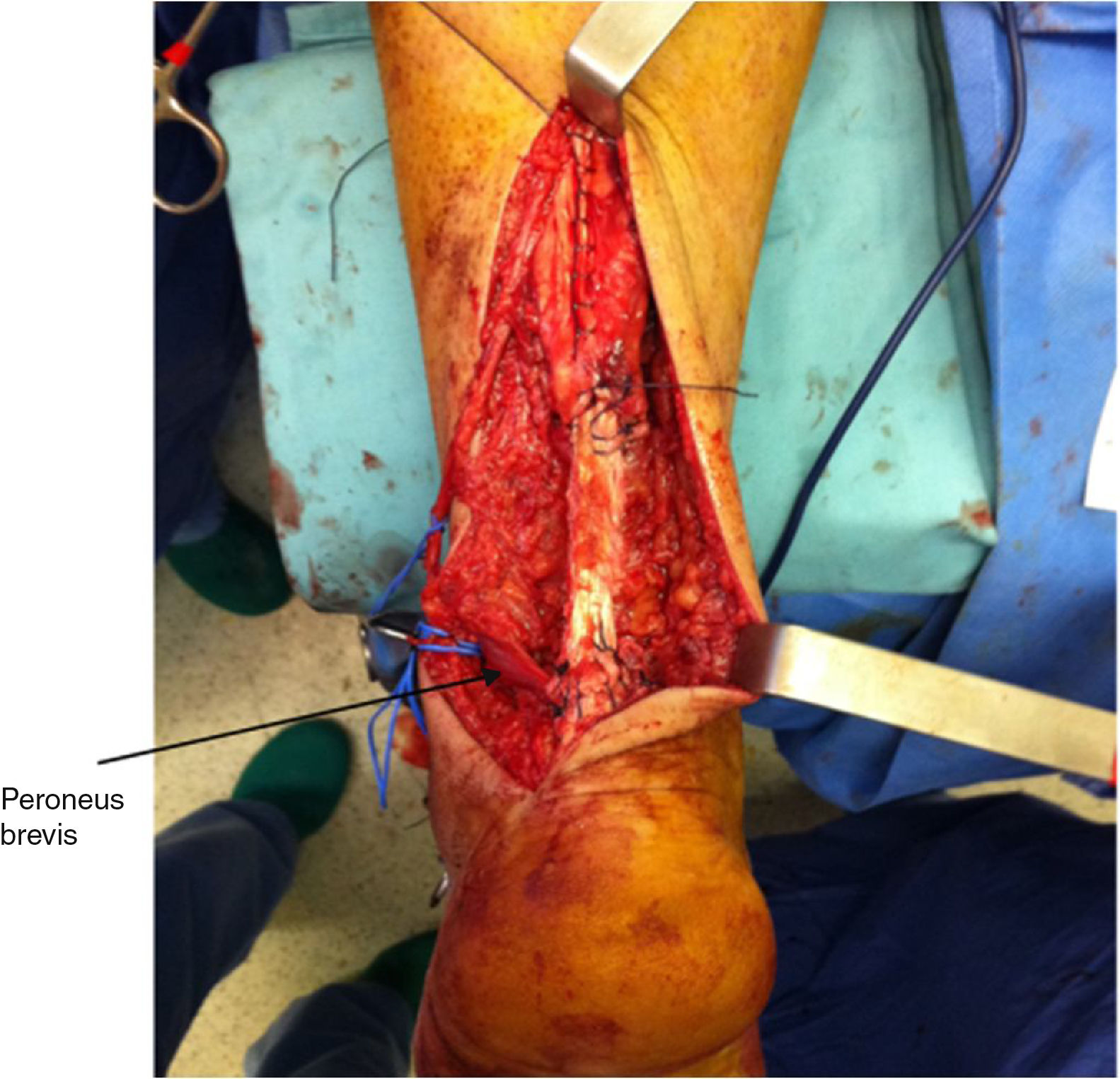
The decision was taken to use modified Turco and Spinella technique to transpose the PB (Fig. 1A).11 However, while seeking the PB tendon during surgery a rupture at 1cm from the base of the fifth metatarsal bone was detected, with the proximal end at the level of the inferior extensor retinaculum, indicating a PB rupture that had not been detected by the MR imaging technique.
The portion of PB obtained was too short to be used in the modified Turco and Spinella technique,11 so that the technique was modified and a rotation plasty was added (Figs. 1B, C and 2).
The MR image was reviewed after surgery and breakage of the PB was confirmed, this having gone undetected prior to the operation. The association between the ATR and PB rupture is not clear.
It is very important to analyse MR images in detail, not solely those showing the Achilles tendon and its rupture, but also the other important structures. These include the FHL, the PB and the peroneus longus, etc., especially in cases when a tendon transfer is considered.
ResultsPostoperative evolution was satisfactory. The patient commenced partial weight-bearing 6 months after surgery and complete weight-bearing after 10 weeks, using a walking boot for 12 weeks. 5 months after surgery he recommenced his work as a farmer.
MR imaging 12 months after surgery showed a heterogeneous Achilles tendon with anterior peritendinous fluid. Isokinetic dynometry showed a 75% recovery in plantar flexion, 83.1% recovery of dorsal flexion, 83.6% recovery of eversion and 84.4% recovery in inversion.
After 36 months of follow-up the patient was asymptomatic.
DiscussionThe treatment of chronic ATR is still controversial. When surgery is delayed it is difficult to restore the normal length of the tendon. This is why many surgeons use augmentation techniques or plasties with other tendons.1–4,12 Direct repair is possible for detects measuring less than 3cm after debridement, and it is possible to add a transposition of the FHL that adds to strength and vascularisation. When a defect measures from 1cm to 3cm13 or from 3cm to 5cm, according to authors, it is possible to make an advance flap in V-Y. For defects longer than 10cm the use of allografts has been described, although the results are restricted to case studies.14
The transposition of PB in the treatment of ATR was described by Pérez Teuffer in 1974, and it was subsequently modified by Turco and Spinella.11
This technique cannot be used in cases such as ours, where the PB is not untouched, so that a combination of techniques such as the one used may be performed, where PB plasty was combined with rotation plasty of the gastrocnemius. The literature consulted contained no combination of techniques like the one presented here, and we believe that it may be of use in cases where multiple lesions hinder the usual techniques.
In the 1995 work by Gallant et al.15 it was found that in patients with a transferred PB to treat rupture of the Achilles tendon, although there was an objective eversion deficit this deficit was not detected subjectively. Although we have used this PB transposition technique for several years, FHL transposition is now used routinely in cases like this one. Wapner et al.16 described the advantage of FHL transposition, of which they underline working in phase with the triceps surae and along the same axis as the same, as well as strength. It is easier to obtain due to its proximity.
Some conditions may weaken the tendons and thereby cause multiple tendon ruptures. These conditions may be medical (obesity, diabetes mellitus, hyperthyroidism, renal diseases, gout, arteriosclerosis, steroid use, syphilis and tuberculosis) or physical (desaxations or biomechanical alterations).17
We believe that this case is important due to the association of both ruptures, together with the difficulty of the reconstruction technique for treating the Achilles tendon defect.
An anatomical variation has recently been described in PB tendon insertion: instead of inserting in the base of the of the fifth metatarsal bone, it inserts in the calcaneous. This must be taken into consideration when planning PB transposition, although it is a rare variation (1%).18
In this case we were unable to ascertain whether the PB rupture was acute or chronic, or if it had occurred due to the weakness of the triceps. The sole risk factor for multiple tendon ruptures was obesity.
A previously unpublished association is presented of a chronic ATR with an undetected rupture of the PB. This case underlines the importance of a correct preoperative evaluation MR imaging and suitable physical examination to confirm the integrity of all the tendons to be used during surgery. A combination of surgical techniques may be a good alternative to a single surgical procedure.
Level of evidenceLevel of evidence v.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Catalán Amigo S, García Medina JR. Rotura crónica del tendón de Aquiles asociada a rotura del tendón peroneus brevis. Caso clínico. Rev Esp Cir Ortop Traumatol. 2019;63:376–379.