Primary hip and knee arthroplasties are some of the most frequent surgical procedures in the Spanish Healthcare System. This study was carried out with the aim of identifying the current clinical practices held in the territory for such processes, as well as future trends.
Material and methodsIn May 2017 a set of 40 questions regarding the practices, indicators, coordination, concerns and tendencies were sent to 289 Heads of Orthopaedic Services from all over Spain.
ResultsResponses were received from 141 hospitals. The mean length of stay varied from 2,6 to 126 days. Mobilization is initiated from the first post-operative hours in 4% of hospitals, until 48 h after surgery in 16% of hospitals. There is no unique standard for the use of drains, urinary catheter or fasting time. In addition, different surgical approaches, implant types, analgesia and blood management protocols can coexist within the same hospital.
In 87% of cases, there are no formal channel paths for interdisciplinary coordination.
Fast-track surgery has been incorporated into the practice of 36% of hospitals, while 66% of hospitals consider that by applying it they could achieve an earlier patient recovery.
In 56% of those surveyed, surgeon concerns are focused on infection management and its prevention, which is expected to have a high impact in the future of arthroplasties, together with pain management.
ConclusionThe study shows a high variability in practices among centers in processes, clini-cal protocols and interdisciplinary coordination, which have an effect on results and process indicators.
Las artroplastias de rodilla y cadera son de los procedimientos quirúrgicos más frecuentes en el Sistema Sanitario español. El estudio pretende conocer la práctica clínica actual y las tendencias de estos procesos en los hospitales españoles.
Material y métodosEn mayo del 2017 se envió un cuestionario a 289 Jefes de Servicio de Cirugía Ortopédica y Traumatología. Constaba de 40 preguntas sobre prácticas, indicadores, coordinación, preocupaciones y tendencias.
ResultadosSe recibieron 141 respuestas. La estancia se sitúa entre 2,6 y 12,6 días, la primera movilización se produce desde las primeras horas post-quirúrgicas en el 4% de los centros, hasta pasadas las 48 horas en el 16%. No existe un único patrón en el uso de drenaje, catéter urinario o restablecimiento de la ingesta. Asimismo, en un mismo hospital pueden coincidir varios tipos de abordajes, implantes, protocolos de analgesia y gestión de sangre.
En el 87% de los casos, no se establecen canales formales de comunicación interdisciplinar.
El 36% de hospitales aplica prácticas de la cirugía fast-track, y el 66% considera que con ellas podría adelantar la recuperación del paciente.
Las preocupaciones del 56% de los cirujanos se centran en el manejo y prevención de las infecciones que se prevé tendrán un impacto en el futuro de las artroplastias, junto con el tratamiento del dolor.
ConclusionesEl estudio muestra una variabilidad en las prácticas entre centros tanto a nivel de procesos como de protocolos clínicos y comunicación interdisciplinar, lo que se traduce en diferencias en resultados e indicadores de proceso.
In 2015, 40,000 primary total knee (TKA) and 35,000 total hip (THA) arthroscopies1 were performed, generating almost half a million hospital stays, which made these the first and fourth most frequent surgical procedures undertaken in the Spanish health system. An ageing population, improved medical and technical skills, as well as greater demands on lifestyle have led to a significant increase in the indications for this surgery in recent years.
TKA and THA are effective surgical procedures that improve patients’ quality of life, increase their functional capacity and reduce pain, and are currently considered among the most successful procedures in medicine.2
Together with the technology used in arthroplasties, patient care processes have improved significantly over the past few decades. Clinical pathways focussed on quality and efficiency, clinical guidelines on surgery, anaesthesia and pain management have been developed, that aim to identify good practice in these procedures.
Given the importance of arthroplasties in the surgical activity of hospitals, in some countries national registers have been developed to obtain systematic information to study the quality of care of arthroplasty interventions and improve the evolution and use of joint prostheses.
The objective of these registers is principally to evaluate the results of the prosthesis in terms of survival, in order to help health professionals in deciding the type of implants to be used. However, they do not assess the care practices surrounding the surgical process.
Furthermore, fast-track surgery3,4 for TKA and THA has become widespread in some European countries. This approach is based on a multi-modal intervention in peri-operative care to reduce postoperative organic dysfunction, possible associated morbidity and recovery time.
Bearing these antecedents in mind, the aim of this study was to establish actual clinical practice, and the characteristics and trends of TKA and THA procedures in Spanish hospitals.
Material and methodsFrom the catalogue of hospitals in Spain,5 the centres with orthopaedic activity and available e-mail addresses of heads of orthopaedic surgery and trauma (OST) departments were selected, mainly through the database of the Spanish Society of Orthopaedic Surgery and Trauma (SECOT). A total of 289 contacts were made of OST department heads: 198 from public hospitals (69%) and 91 from private hospitals (31%).
Information was obtained by sending an online questionnaire to the selected population between May, July 2017. The questionnaire was designed by the authors, reviewed by two orthopaedic surgeons from outside the project. It consisted of 40, questions of different types: closed, multiple choice, open, with an estimated response time of 30 min. It included questions relating to the pre-operative, intraoperative, post-operative preparation phases. It also included questions on practices associated with fast-track surgery, on internal, multidisciplinary coordination, concerns, expected trends in TKA, THA. The data were requested for the year 2016, had to reflect the routine practice of the entire OST department.
In order to ensure data protection and confidentiality of responses, an external consultancy was commissioned to manage the survey and subsequent data analysis.
The variables analysed were mean hospital stay, practices followed in preparing the patient during admission and surgery (analgesia and anaesthesia, use of drains, ischaemia, blood management, urinary catheter, type of approach, implant, stabilisation and fixation) and on discharge (discharge criteria, mobilisation and rehabilitation guidelines). The possible impact of some of these practices on hospital stay was also studied. Finally, the intra- and interdepartmental coordination mechanisms and the advances and trends expected by the OST departments were analysed.
Excel (2016, Microsoft, USA) was used for the analysis using the descriptive statistical function to obtain averages and percentages in the main variables, and the determination coefficient R2 to study the correlation between variables.
ResultsResponses were received from 141 hospitals, a return of close to 50%, which showed a representative sample of practices carried out in Spain, with a margin of error of 5.9% and a 95% confidence level.
The participating hospitals were 124 public hospitals (88%) and 17 private hospitals (12%). In terms of care level, 35% were level 3, 44% level 2 and 21% level 1. Centres from all Spain’s Autonomous Regions participated, except Ceuta and Melilla, from which no contact data were obtained.
Based on the number of responses received, the care practice for around 23,010 TKA and 12,262 THA were analysed.
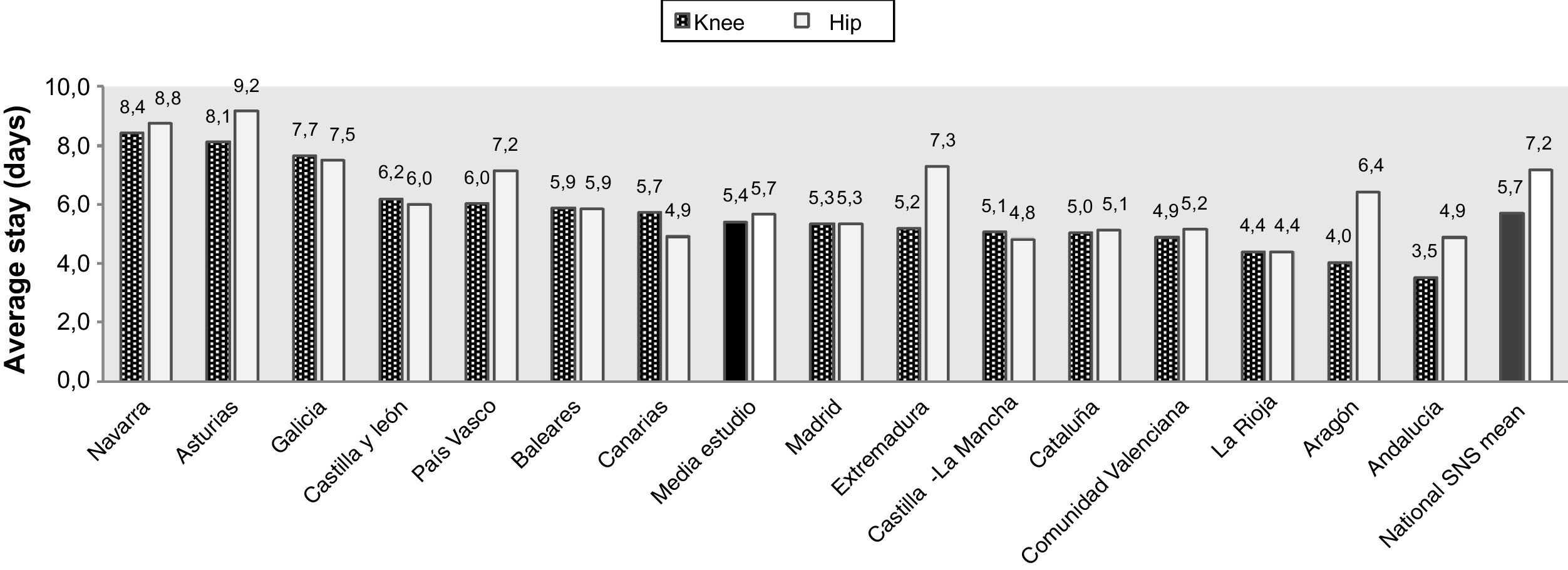
Hospital stayThe mean stay found in the study is similar to that reported by the SNS in 20151 for TKA (5.4 days is the mean stay for the hospitals of the study, compared to 5.7 days in the SNS). For THA, the mean stay of the hospitals participating in the study was 1.5 days less than the average for the SNS (5.7 days in the study compared to 7.2 days in the SNS).
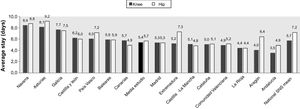
There is variability in the length of stay between the Autonomous Regions (Fig. 1), with a difference of up to 5 days between them. The difference reaches 10 days if the means of all the centres are compared globally, and limit values of mean stay are found of 2.6 and 12. 6 days; this suggests a diversity of clinical practice for these two procedures.
Thirty-six percent of hospital s in Spain indicate that practices are used that are typical of fast-track surgery, such as early mobilisation and rehabilitation, exchange of some activities for others based on evidence, and patient education, although not always for all patients.
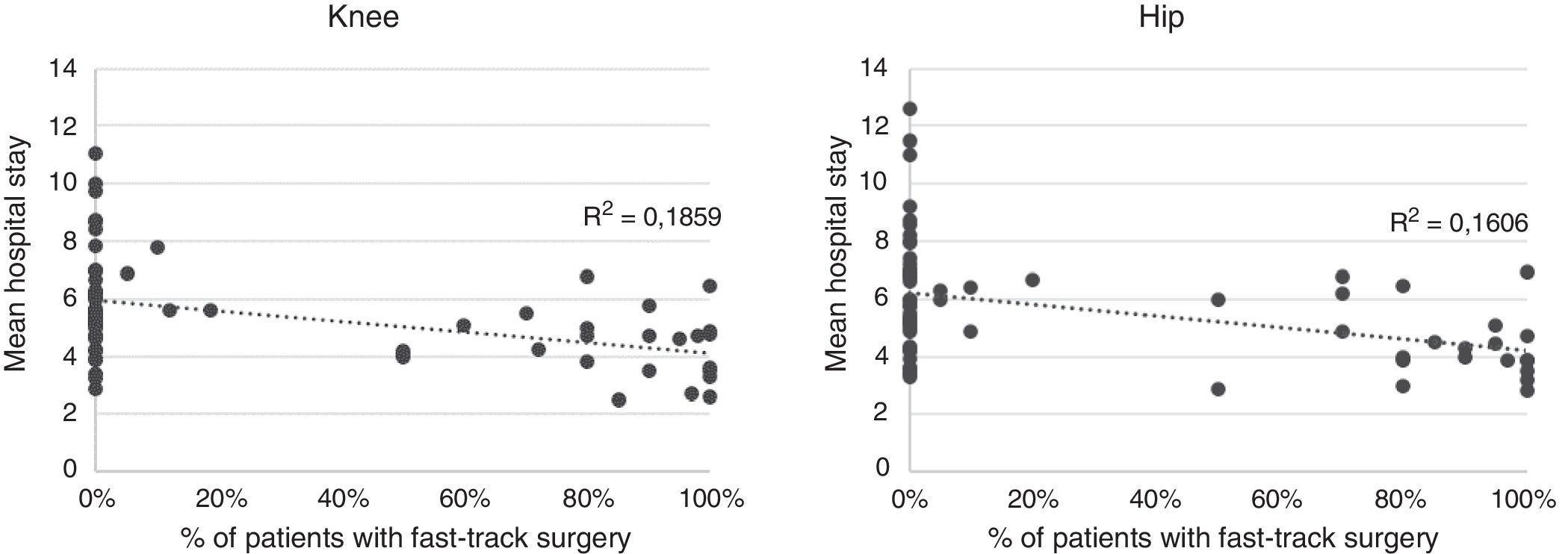
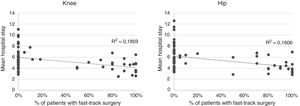
Comparing the data on hospital stay between centres that do and do not use fast-track surgery (Fig.2) a significant correlation can be observed with appreciable magnitude between implementing fast-track surgery and reduction in hospital stay (R2 = 0.1859, p < .05 in TKA; R2 = 0.1606, p < .05 in THA). The difference in hospital stay between the two groups is more moderate than that reported in the literature, which shows a decrease in hospital stay of around 50%.6
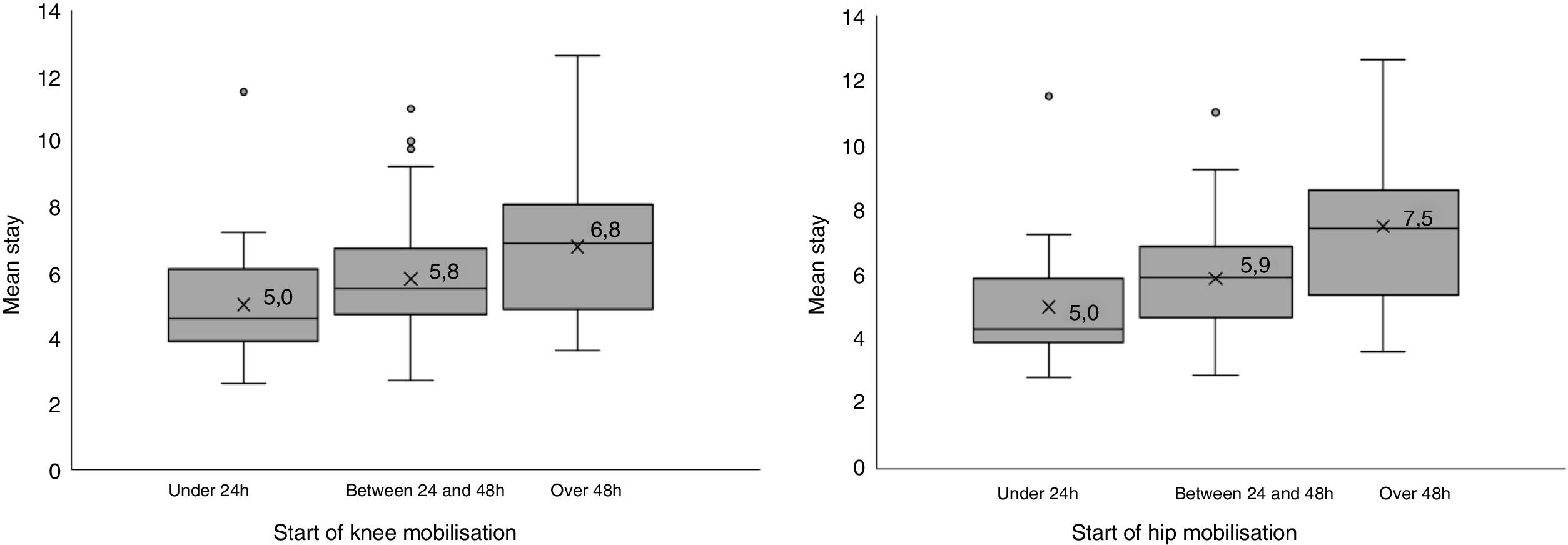
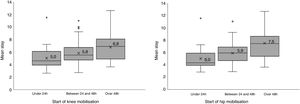
Another factor that was correlated with length of hospital stay was the start of ambulation. Recovery is anticipated in line with mobilisation (p < .05), and hospital stay is shortened by one day whenever ambulation is brought forward by one day (Fig. 3). Thus, the difference between average stay when mobilisation takes place later than 48 h and when it occurs in less 24 h is 2 days.
ProcessesOf the participating hospitals, 73% have a defined clinical pathway for TKA and THA, in most cases developed in a multidisciplinary manner together with nursing, anaesthesia and/or rehabilitation and physiotherapy areas or services.
All the hospitals provide verbal or written information to patients in the surgeon’s clinic on the surgery that they are to undergo. Twenty-five percent of them organise additional specific education sessions for their patients and 14% include in their clinical pathway a session with a physiotherapist to demonstrate and practice rehabilitation exercises before the surgery.
In 60% of the hospitals, the patient’s social situation is analysed prior to admission, and in 50% of them, functionality and quality of life are assessed prior to surgery. Thirty percent of the centres have a pre-admission nursing clinic.
Patients scheduled for knee or hip arthroplasty surgery are admitted for surgery on the same day as the operation in 57% of hospitals, while 38% admit their patients the evening or night before, and 5% the morning of the day before surgery.
Discharge criteria are only agreed by the OST department in 50% of the hospitals, and in 27% of centres the multidisciplinary team attending the patients also participates in defining these criteria. In the remaining 23% of the hospitals they are not protocolised, and therefore depend on the judgement of each surgeon.
Furthermore, 33% of the hospitals carry out specific questionnaires to evaluate functionality and quality of life before and after surgery.
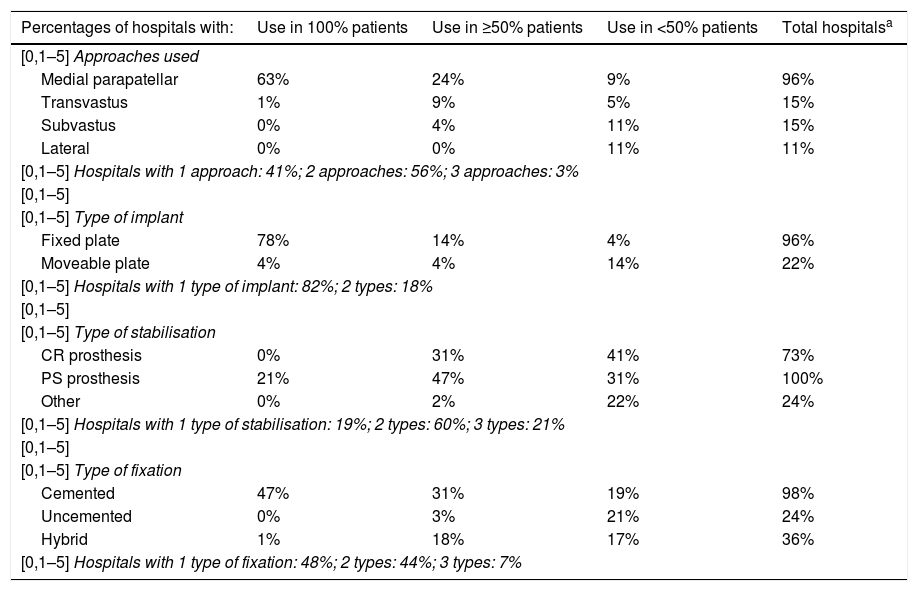
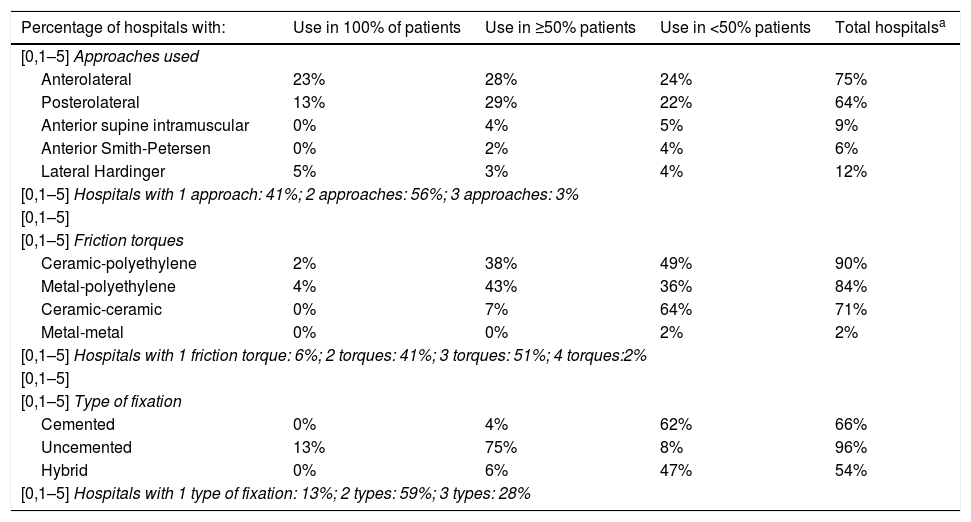
SurgeryTables 1 and 2 show the characteristics of TKA and THA in terms of type of approach, implant, stabilisation and fixation.
Aspects of knee arthroplasty surgery (percentage of hospitals according to the volume of patients in which it is used).
| Percentages of hospitals with: | Use in 100% patients | Use in ≥50% patients | Use in <50% patients | Total hospitalsa |
|---|---|---|---|---|
| [0,1–5] Approaches used | ||||
| Medial parapatellar | 63% | 24% | 9% | 96% |
| Transvastus | 1% | 9% | 5% | 15% |
| Subvastus | 0% | 4% | 11% | 15% |
| Lateral | 0% | 0% | 11% | 11% |
| [0,1–5] Hospitals with 1 approach: 41%; 2 approaches: 56%; 3 approaches: 3% | ||||
| [0,1–5] | ||||
| [0,1–5] Type of implant | ||||
| Fixed plate | 78% | 14% | 4% | 96% |
| Moveable plate | 4% | 4% | 14% | 22% |
| [0,1–5] Hospitals with 1 type of implant: 82%; 2 types: 18% | ||||
| [0,1–5] | ||||
| [0,1–5] Type of stabilisation | ||||
| CR prosthesis | 0% | 31% | 41% | 73% |
| PS prosthesis | 21% | 47% | 31% | 100% |
| Other | 0% | 2% | 22% | 24% |
| [0,1–5] Hospitals with 1 type of stabilisation: 19%; 2 types: 60%; 3 types: 21% | ||||
| [0,1–5] | ||||
| [0,1–5] Type of fixation | ||||
| Cemented | 47% | 31% | 19% | 98% |
| Uncemented | 0% | 3% | 21% | 24% |
| Hybrid | 1% | 18% | 17% | 36% |
| [0,1–5] Hospitals with 1 type of fixation: 48%; 2 types: 44%; 3 types: 7% | ||||
Aspects of hip arthroplasty surgery (percentage of hospitals according to the volume of patients in whom it is used).
| Percentage of hospitals with: | Use in 100% of patients | Use in ≥50% patients | Use in <50% patients | Total hospitalsa |
|---|---|---|---|---|
| [0,1–5] Approaches used | ||||
| Anterolateral | 23% | 28% | 24% | 75% |
| Posterolateral | 13% | 29% | 22% | 64% |
| Anterior supine intramuscular | 0% | 4% | 5% | 9% |
| Anterior Smith-Petersen | 0% | 2% | 4% | 6% |
| Lateral Hardinger | 5% | 3% | 4% | 12% |
| [0,1–5] Hospitals with 1 approach: 41%; 2 approaches: 56%; 3 approaches: 3% | ||||
| [0,1–5] | ||||
| [0,1–5] Friction torques | ||||
| Ceramic-polyethylene | 2% | 38% | 49% | 90% |
| Metal-polyethylene | 4% | 43% | 36% | 84% |
| Ceramic-ceramic | 0% | 7% | 64% | 71% |
| Metal-metal | 0% | 0% | 2% | 2% |
| [0,1–5] Hospitals with 1 friction torque: 6%; 2 torques: 41%; 3 torques: 51%; 4 torques:2% | ||||
| [0,1–5] | ||||
| [0,1–5] Type of fixation | ||||
| Cemented | 0% | 4% | 62% | 66% |
| Uncemented | 13% | 75% | 8% | 96% |
| Hybrid | 0% | 6% | 47% | 54% |
| [0,1–5] Hospitals with 1 type of fixation: 13%; 2 types: 59%; 3 types: 28% | ||||
Use of the tourniquet for TKA is very widespread in Spanish centres; according to the results, 9 out of 10 centres operate on knees using tourniquet- induced ischaemia. In half the tourniquet is maintained throughout the surgery, while 44% remove it following placement of the implants. Four percent of the hospitals do not use the tourniquet, and a further 4% only use it occasionally.
Similarly, 76% of the participating hospitals leave a drain after surgery, a suction drain in 80% of the cases. Drainage is maintained for 24 h (47% of the centres) or for 48 h following the surgery (51%). Of the hospitals, 14% do not use drains and the remaining 10% do not use them routinely.
Of the hospitals, 41% systematically use a urinary catheter, which is maintained in most cases from 24 to 48 h. Forty-eight percent of the hospitals no longer use a catheter during or after surgery.
Fluid intake is started 4 h, and intake of solids 6h following the surgery in 75% of the hospitals, whereas 4% start intake of fluids immediately after the operation.
Pain and blood managementRegional anaesthesia, especially spinal anaesthesia is the most popular in knee and hip arthroplasties in Spain, and it is the main anaesthetic technique or technique of choice in 65% of the hospitals. Thirty-five percent choose epidural anaesthesia as the first option, 8% a combination of techniques and less than 1% use general anaesthesia.
There is no single protocol in most centres (59%) on the analgesic technique to be used for arthroplasty patients, but this depends on the anaesthetist responsible for the patient in each case, even though 61% of the hospitals have an acute pain unit.
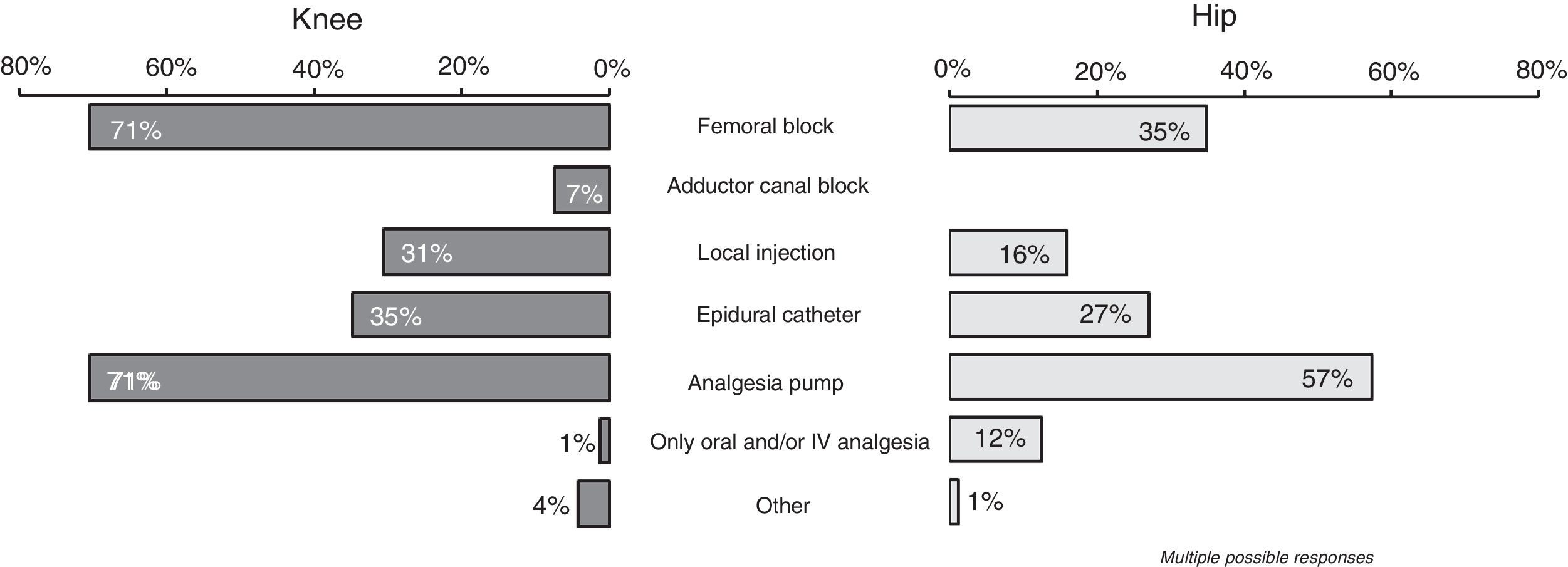
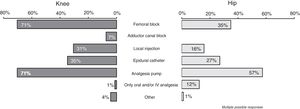
In any case, femoral block and the analgesia pump are the most frequent post-operative analgesic techniques (Fig. 4) used in knee surgery in 7 out of every 10 centres, whereas techniques such as local injection are used in 30% of the centres for the knee and 16% for the hip.
With regard to the drugs used for postoperative analgesia, the combination of paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs) and opiates is the most frequent pattern, used in more than 80 of the hospitals. COX-2 inhibitors are also used in 20% of the centres.
For the first 24 h the most usual administration route is intravenous, although some of the centres (2%) start the oral route as soon as the patient arrives on the ward.
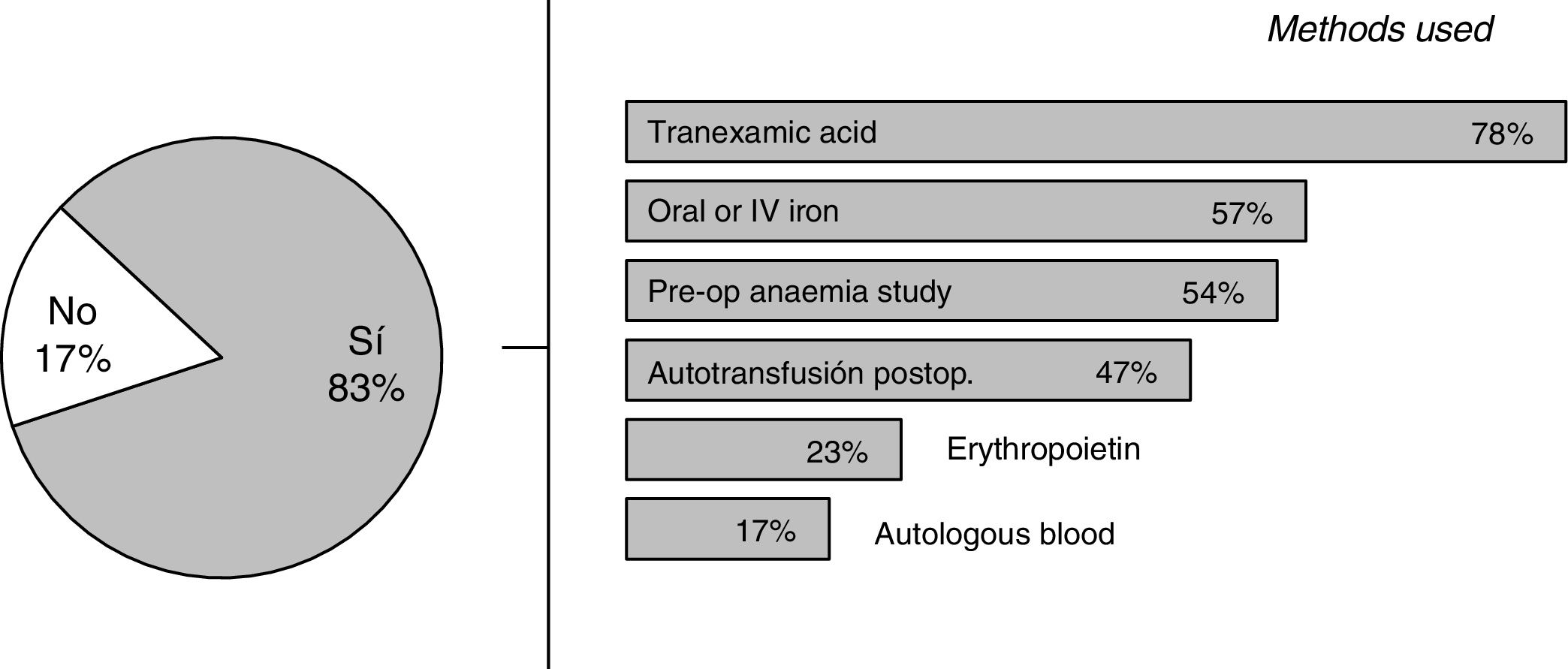
Transfusions are currently performed in 14% of TKA patients and in 16% of THA patients.
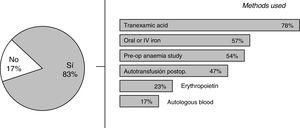
Tranexamic acid is the most commonly used alternative for bleeding control (Fig. 5), and although there seems to be consensus on its use, there is some variability with regard to administration route and regimen.
Mobilisation and rehabilitationTwenty percent of the hospitals start active mobilisation and weight bearing during the first 24 h, 4% manage this in the first 6 h, but in most of the hospitals ambulation is started between 24 h and 48 h following surgery (64%). In 16% of the hospitals it is started 2 days following the surgery.
Of the hospitals, 82% have a physiotherapy service at least from Monday to Friday in the morning. This service is also available during the weekend in 20%.
Thirteen percent of the hospitals following knee surgery and 37% following hip surgery do not prescribe hospital rehabilitation sessions for any of their patients.
After discharge from hospital, during the recovery phase after hip arthroplasty, restriction of movement is common for several weeks to minimise the risk of dislocation. Seventy-six percent of the hospitals recommend avoiding movements such as crossing legs, sitting in low places or flexion greater than 90 degrees.
Communication and coordinationThe OST departments generally respond that there is fairly or very good coordination with the rest of the services and areas involved in the patient care process.
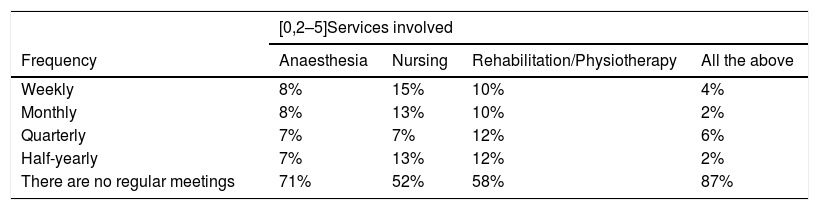
In any case, regular multidisciplinary communication through formal channels established together with all the services involved is not common practice in 87% of the centres (Table 3).
Meetings agreed between the orthopaedic and trauma department and other services involved in arthroplasty procedures.
| [0,2–5]Services involved | ||||
|---|---|---|---|---|
| Frequency | Anaesthesia | Nursing | Rehabilitation/Physiotherapy | All the above |
| Weekly | 8% | 15% | 10% | 4% |
| Monthly | 8% | 13% | 10% | 2% |
| Quarterly | 7% | 7% | 12% | 6% |
| Half-yearly | 7% | 13% | 12% | 2% |
| There are no regular meetings | 71% | 52% | 58% | 87% |
Only a few hospitals and OST departments – between 6% and 15%, depending on frequency and the services involved – hold periodic formal meetings to discuss issues relating to knee or hip arthroplasty procedures with other areas or services.
Challenges and trendsThe concerns of the Spanish OST departments focus primarily on surgery and its clinical outcomes. Infections come first, and are a priority issue for 56% of the hospitals. After infections, clinical outcomes, such as the quality and survival of the implant and patient safety, are the issues of most concern for 20% of the participants. Aspects relating to variability, procedure management and patient management are of less weight, at around 10%.
Along with advances in pain management, the diagnosis and treatment of infections are again expected to have the greatest impact on the future of arthroplasties, and thus the major concern of the OST departments. Also noteworthy in the area of procedures and management are aspects relating to data treatment and sharing, the responsibility of the clinician in managing and measuring the experience of patients.
Along the same lines, the advances expected over the next 5–10 years relate to the personalisation of surgery, prevention of infection, and improvement of implants and the surgical procedure.
DiscussionThis study was based on a voluntary survey where the majority of respondents were from public hospitals; therefore the results obtained principally reflect these types of hospitals. Nevertheless, given the number of responses, it provides an approximate indication of the reality of some essential aspects of the daily care of TKA and THA about which there has been no aggregated knowledge to date at a national level.
The results obtained show the variability that exits in many practices throughout the care process among Spanish hospitals, in terms of the preoperative preparation of patients, development of the surgery or postoperative treatment, and also within the same centre, where, for example, there are various approaches to pain management. The consequence of this variability in the process is high dispersion in one of its main outcome indicators: average hospital stay, which differs by up to 10 days between centres.
Although a greater consensus is observed in some aspects, such as the use of tourniquet-induced ischaemia for knee surgery, postoperative drains or starting mobilisation after 24 h, these practices do not currently always seem to be supported by a sufficient level of evidence to justify their continuity. In relation to these practices, it is worth asking: Are rest, fasting and limitation of movement necessary after surgery when seeking patient recovery? Are drains, urinary catheters and analgesia pumps necessary? Are we not principally looking at the passing on of traditions7–9 between generations of surgeons?
Recent evidence also shows that rapid mobilisation of patients following total joint replacement can be performed safely and improves postoperative recovery.10,11 This fact is also demonstrated in this study (Fig. 3). However, to be able to start mobilisation early, several factors must come together simultaneously, such as anaesthesia and analgesia with minimal side effects, organisation of work that includes patient ambulation among the activities to be carried out immediately postoperatively, a coordinated multidisciplinary team and informed and involved patients.12
Unlike some European countries,6 these practices specific to fast-track surgery are not the majority in Spain. At the moment, only a third or hospitals indicate using all or some of them, while others (11%) are working towards starting to apply them. However, two thirds of the professionals participating in the study state that their patients’ recovery time could be reduced by using this methodology.
A priori, arthroplasty surgery would meet the conditions to become a standardised procedure; it is an elective and scheduled procedure, high volume, that affects a certain population profile and whose activities have been tested and contrasted.
Implementing clinical pathways that have been defined and coordinated in a multidisciplinary manner and based on the latest evidence could help to standardise and coordinate care, incorporate proven best practice into the hospital environment, improve patient outcomes and safety, and thus provide efficient and satisfactory care.13,14
ConclusionAfter the analysis, variability was seen in practices implemented between the Spanish hospitals, principally the public hospitals, both at the level of process and clinical procedure and interdisciplinary communication, which translates into differences in the results of mean hospital stay and other indicators of the process, such as starting mobilisation of patients. Based on the study, and bearing in mind that the results refer to 2016, it is expected that the information obtained on the situation of TKA and THA in Spanish hospitals will help to encourage reflection on current healthcare practices and thus favour the ongoing improvement of one of the most important surgical procedures in the Spanish healthcare system.
LimitationsThere was limited access to the contact details of department heads of all hospitals in Spain. Since there is no global and updated database with hospitals, OST department heads and emails, it was necessary to consider contacts available and identified as department heads on the database of SECOT members, to which was added the identification and verification of a limited number of additional contacts on an individual basis. As a result, there was not full access: a number of hospitals did not receive the survey and did not have the opportunity to participate.
The second limitation concerns the possible subjectivity of the responses. The responses were based on the view of the respondent, so they depended on the respondent’s access to the information requested at the time of responding to the survey, with the possibility in some cases that their answers did not fully reflect all of their department’s practices and outcomes.
Finally, in order to create a simple questionnaire that did not require too much time to complete, not all the aspects of healthcare practice were included, a series of questions or aspects that might also have been of interest for the study were removed.
Level of evidenceLevel of evidence III.
FinancingThe study was financed by Zimmer Biomet S.L.U., who commissioned SDSEUROGROUP S.L to manage the survey and subsequent data analysis.
Conflict of interestsThe authors have no conflict of interests to declare.
We thank the Spanish Society of Orthopaedic Surgery and Trauma (SECOT) for their support of the project, as well as all the respondents to the questionnaire who contributed to the success of the study
Please cite this article as: Molko S, et al. El proceso de atención de las artroplastias primarias totales de rodilla y cadera en Espa˜na: un estudio a nivel nacional. Rev Esp Cir Ortop Traumatol. 2019;63:408–415.