To evaluate midterm functional outcome after pyrolytic carbon prosthesis (PyroDisk) implantation in the treatment of rhizarthrosis of the thumb, comparing outcomes with those of ligamentous resection/suspension/reconstruction.
Material and methodsA cross-sectional study retrospectively comparing two patient groups aged between 40 and 65 years with rhizarthrosis of the thumb. Thirty-two patients operated between 2009 and 2013 were distributed between group i (interposition arthroplasty with PyroDisk implant) and group ii (ligamentous resection/suspension/reconstruction arthroplasty). Data on pain, functionality (Quick-Dash questionnaire) and articular movement were collected in 2015. In addition, a radiological study was undertaken using radiographs and CT.
ResultsThirty-two patients, 16 in each group with a mean follow-up of 35 months (23–47). Pain at the end of follow-up was greater in the group with the pyrolytic carbon prosthesis (p=0.000). According to the QuickDash questionnaire, the patients in group i achieved a mean functionality of 31.14 (0–70) points compared to 15.81 (8–24) points for group ii (p=0.027). No differences were found in the degree of mobility at the end of follow-up (p=0.46). The prosthesis had to be removed in six cases.
DiscussionThe pyrolytic carbon prosthesis has been presented as an alternative treatment for rhizarthrosis of the thumb. The papers published to date highlight the discrepancies in midterm functional outcomes.
ConclusionsPyrolytic carbon prostheses have shown inferior functional outcomes, compared with resection/suspension/reconstruction arthroplasties.
Evaluar el resultado funcional a medio plazo de la utilización del implante de carbón pirolítico (PyroDisk) en el tratamiento de la rizartrosis del pulgar, comparando sus resultados con la artroplastia de resección-suspensión-reconstrucción ligamentosa.
Material y métodoEstudio transversal que compara de forma retrospectiva 2grupos de pacientes entre 40 y 65 años con rizartrosis del pulgar. Los 32 pacientes intervenidos entre 2009 y 2013 se distribuyeron entre el grupo i (artroplastia de interposición con el implante PyroDisk y el grupo ii (artroplastia de resección-suspensión-reconstrucción ligamentosa). En 2015 se recogieron el dolor, la funcionalidad (cuestionario Quick-Dash) y el balance articular. Además, se realizó un estudio radiológico con radiografías y TC.
ResultadosSe siguió a 32 pacientes, 16 en cada grupo, con un seguimiento medio de 35 meses (23–47). El dolor al final del seguimiento fue mayor en el grupo intervenido con la prótesis de carbón pirolítico (p=0,000). En la funcionalidad según el test de QuickDash, los pacientes del grupo i obtuvieron una media de 31,14 (0–70) puntos frente a 15,81 (8–24) puntos del grupo ii (p=0,027). No se encontraron diferencias en el grado de movilidad al final del seguimiento (p=0,46). En 6 casos fue necesario retirar la prótesis.
DiscusiónLa prótesis de carbón pirolítico se ha presentado como alternativa para el tratamiendo de la rizartrosis del pulgar. En los trabajos publicados hasta el momento destaca la discrepancia en los resultados funcionales a medio plazo.
ConclusionesLa prótesis de carbón pirolítico ha mostrado resultados funcionales inferiores a medio plazo comparada con la artroplastia de resección-suspensión-reconstrucción ligamentosa.
The trapeziometacarpal joint has a wide range of movement due to it being a bioconcave saddle-shaped joint.1 However, this wide movement predisposes the appearance of early joint degeneration. In fact, in 21% of adults over 40 years of age, trapeziometacarpal arthrosis may be observed in radiological changes and in women of postmenopausal age this prevalence rises to 25%.2,3 Joint erosion leads to pain at the base of the thumb which is associated with limited movement and a loss of strength, affecting not just everyday activities, but also the activities of actively employed patients. Despite its high frequency and copious amounts of literature on the subject, the latest reviews indicate that no single surgical technique leads to a better functional outcome than any other.4–9
The use of pyrolytic carbon prostheses as an alternative in rhizarthrosis surgery has increased during the last decade. In studies published to date, the discrepancy in mid-term functional results is outstanding. Some authors state highly favourable outcomes whilst others are totally bleak.10–13 One reason for this could be the radiological changes observed, such as the subluxations of the implants. It would be of interest to determine the reasons for these complications and analyse the differences in clinical outcome.
The purpose of this study was to assess the midterm functional outcome of the use of the pyrolytic carbon implant (PyroDisk) in the treatment of rhizarthrosis, comparing its results with those of the technique described by Burton–Pellegrini (ligamentous resection/suspension/reconstruction arthroplasty) as benchmark. The hypothesis of the study was that pyrolytic carbon prostheses led to better functional outcomes than the standard technique.
Material and methodA cross-sectional study was designed which retrospectively compared two groups of patients aged between 40 and 65. All the patients had been diagnosed with Eaton and Glickel grade II and grade III rhizarthrosis14 and conservative treatment had failed (splinting, infiltrations and physiotherapy). The patients underwent surgery with the Burton–Pellegrini technique or pyrolytic carbon prostheses (PyroDisk, Integra Life Sciences, Plainsboro NJ) between 2009 and 2013. Patients with previous operations in trapeziometacarpal joints were excluded, as were those with radiological evidence of scaphoid trapezium trapezoidal arthrosis, concomitant injuries which required associated surgical approaches (DeQuervain disease, instability or metacarpophalangeal arthrosis) and those with the inability to complete the questionnaires due to cognitive/linguistic difficulties. The patients were operated on by specialist surgeons from the Hand unit of the Orthopaedic Service of a single hospital. Each of the patients was included on the waiting list for surgery and received verbal information regarding treatment. Informed consent was obtained. The selected patients were randomly assigned to a treatment group. The study was accepted by the hospital Ethics Committee.
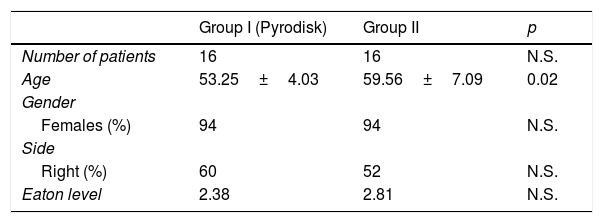
The 32 patients were distributed into two groups according to the surgical technique applied. Group i comprised 16 patients operated on using interposition arthroplasty with the pyrolytic carbon prostheses (PyroDisk). Group iicomprised 16 patients operated on using ligamentous resection/suspension/reconstruction arthroplasty described by Burton–Pellegrini. The patients were assessed throughout 2015. Sociodemographic data were collected, and the degree of preoperative arthrosis was classified in accordance with the Eaton Glickel scale14 (Table 1).
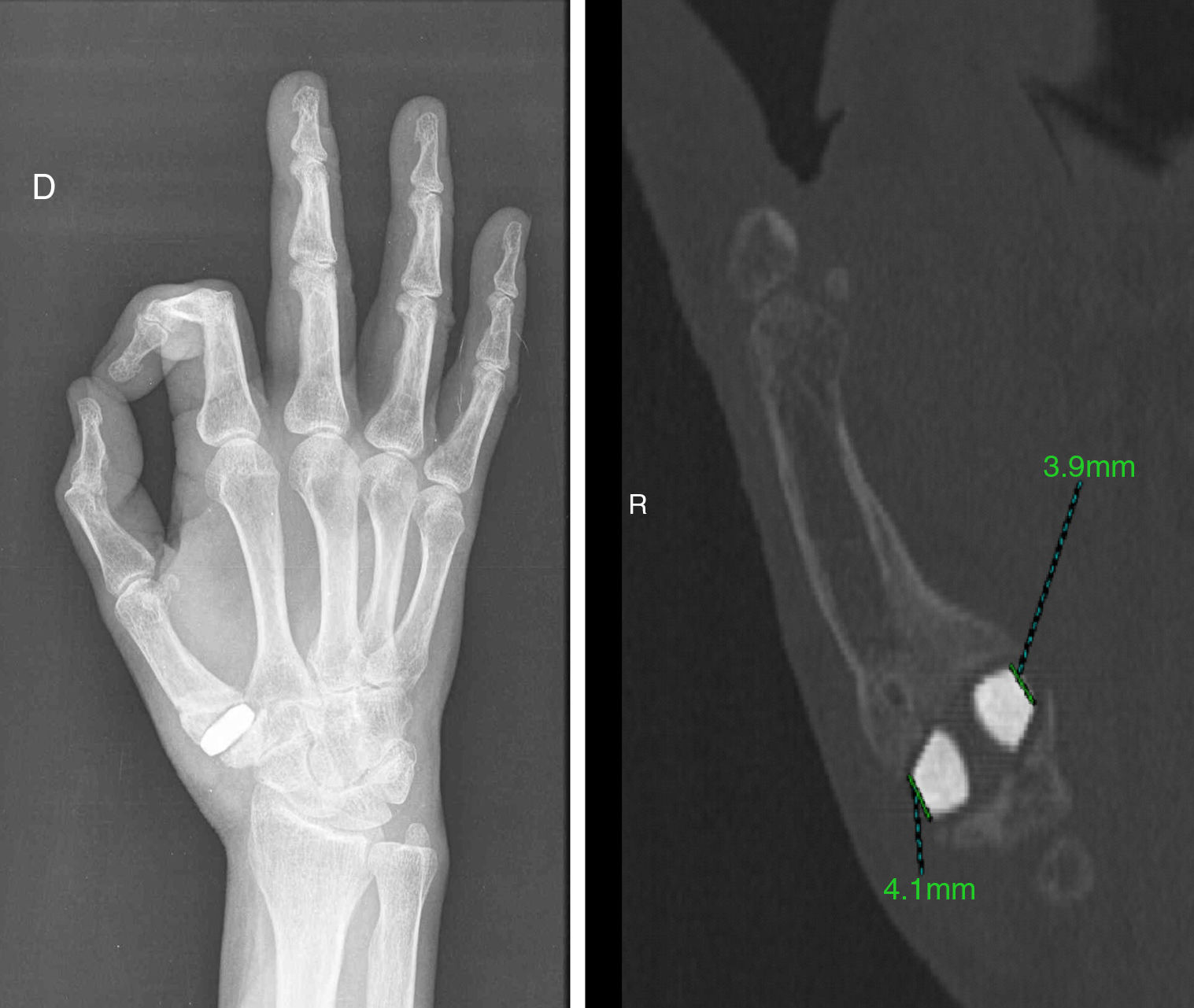
Postoperatively, pain was assessed with the visual analogue scale (VAS), where 0 stood for pain-free and 10 the maximum pain possible. Functionability was assessed with the Quick-Dash questionnaire (with scores between 0 in the absence of disability and 100 the highest disability)10 and joint balance of the thumb by Kapandji scale.15 Patients from group i (PyroDisk) were submitted to a radiological study with anteroposterior, oblique radiographies and a CT scan. The longitudinal axis of the trapeziometacarpal joint was measured for analysis of accurate positioning of the implant and its dimensions, as shown by Barrera-Ochoa et al.11 Furthermore, possible bone reactions around the implant were collected, with a radiolucency line of under 1mm around the implant regarded as normal.16,17 All data were collected by an independent third-party observer: an orthopaedic surgeon in training.
Surgical TechniqueWe used a dorsolateral approach, capsulotomy and hemi-trapeziectomy with oscillating saw on group I patients who received the pyrolytic carbon prostheses. The trapezium and the base of the first metacarpal were tunnelled with a 3.2mm drill. The metacarpal base drill was made 1.5cm distal to the joint surface, from the dorsoradial region to the joint surface. In the trapezium, the oblique tunnel extended from the centre of the scaphoid and trapezium joint to the centre of the trapezium metacarpal joint. The implant was selected from six sizes, avoiding the overlap. Intraoperative fluoroscopy was used in some cases to confirm the appropriate size.
Hemi-plasty of the flexor carpi radialis tendon was performed passing it through the trapezium, the implant hole and recovering it finally through the metacarpal tunnel. The plasty was sutured to itself, with special care taken to avoid too much tension.
The patients in group iiunderwent ligamentous resection/suspension/reconstruction arthroplasty through the flexor carpi radialis hemi-tendon using the Burton–Pellegrini18 technique. A dorsolateral approach was used, and complete trapeziectomy was performed.
Postoperative rehabilitation protocol was the same for the two groups. This consisted of a soft ante-brachial bandage for 2 weeks with free movement of the thumb, but with restriction of digital pincer activities (writing, sewing, cooking, opening doors, etc.) for up to 6 weeks.
Statistical analysisStatistical analysis was performed using the SPSS version 15.0 (SPSS Inc., Chicago, IL, USA) software. Continuous variables are presented as means or standard deviation ranges. Categorical variables were presented as percentages. Parametric data such as the functional tests between groups were analysed using the Student's t-test. A statistical significance level was established at p<0.05.
ResultsThe 32 patients of the sample were split into two groups, 16 patients in each group. The minimum follow-up time was 16 months and the mean follow-up time for the whole sample was 35 months (23–47 months).
With regard to the level of preoperative impact for the group operated on with PyroDisk, a mean of 2.37 points was obtained on the Eaton scale, whilst for the group operated on with the Burton–Pellegrini technique this was 2.81, and no differences were found between them (p=0.16). With regard to age, we found there was a lower mean age in patients for whom the pyrolytic carbon prostheses were indicated (53.25 years) than in those operated on with the Burton–Pellegrini technique (59.56) (p<0.05) (Fig. 1).
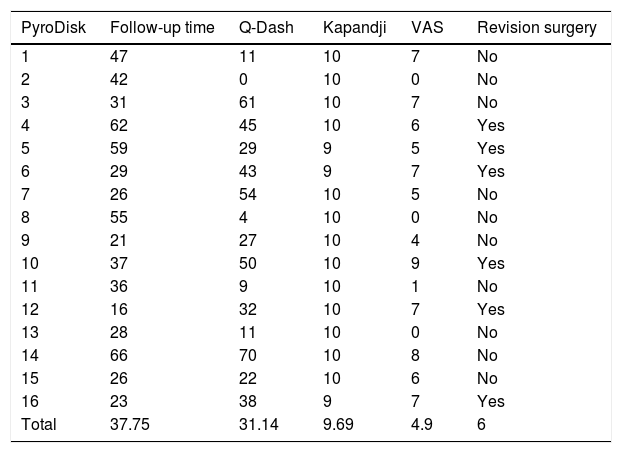
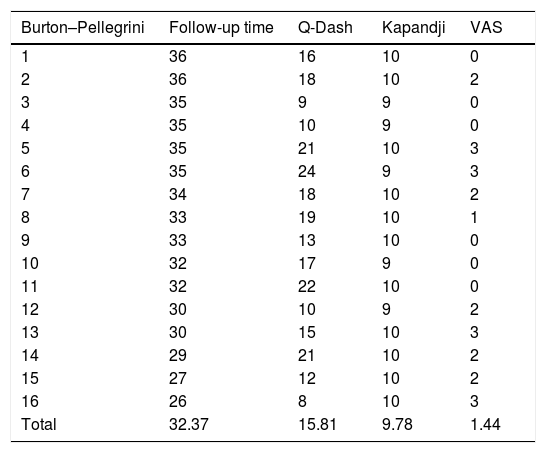
Postoperatively, the pain at the end of follow-up was greater in the group operated on with pyrolytic carbon prostheses with a mean pain score of 4.9 (0–9) on the VAS compared with a mean pain score of 1.43 (0–3) in the Burton–Pellegrini group (p=0.000). With regard to usability from the QuickDashtest, the patients of group I obtained a mean of 31.14 points (0–70) compared with 15.81 (8–24) for group ii, with statistically significant differences (p=0.027). There were no differences in mobility according to Kapandji at the end of follow-up (p=0.46) (Tables 2 and 3).
Functional outcome of pyrolytic carbon prosthesis.
| PyroDisk | Follow-up time | Q-Dash | Kapandji | VAS | Revision surgery |
|---|---|---|---|---|---|
| 1 | 47 | 11 | 10 | 7 | No |
| 2 | 42 | 0 | 10 | 0 | No |
| 3 | 31 | 61 | 10 | 7 | No |
| 4 | 62 | 45 | 10 | 6 | Yes |
| 5 | 59 | 29 | 9 | 5 | Yes |
| 6 | 29 | 43 | 9 | 7 | Yes |
| 7 | 26 | 54 | 10 | 5 | No |
| 8 | 55 | 4 | 10 | 0 | No |
| 9 | 21 | 27 | 10 | 4 | No |
| 10 | 37 | 50 | 10 | 9 | Yes |
| 11 | 36 | 9 | 10 | 1 | No |
| 12 | 16 | 32 | 10 | 7 | Yes |
| 13 | 28 | 11 | 10 | 0 | No |
| 14 | 66 | 70 | 10 | 8 | No |
| 15 | 26 | 22 | 10 | 6 | No |
| 16 | 23 | 38 | 9 | 7 | Yes |
| Total | 37.75 | 31.14 | 9.69 | 4.9 | 6 |
Functional outcome of the Burton–Pellegrini technique.
| Burton–Pellegrini | Follow-up time | Q-Dash | Kapandji | VAS |
|---|---|---|---|---|
| 1 | 36 | 16 | 10 | 0 |
| 2 | 36 | 18 | 10 | 2 |
| 3 | 35 | 9 | 9 | 0 |
| 4 | 35 | 10 | 9 | 0 |
| 5 | 35 | 21 | 10 | 3 |
| 6 | 35 | 24 | 9 | 3 |
| 7 | 34 | 18 | 10 | 2 |
| 8 | 33 | 19 | 10 | 1 |
| 9 | 33 | 13 | 10 | 0 |
| 10 | 32 | 17 | 9 | 0 |
| 11 | 32 | 22 | 10 | 0 |
| 12 | 30 | 10 | 9 | 2 |
| 13 | 30 | 15 | 10 | 3 |
| 14 | 29 | 21 | 10 | 2 |
| 15 | 27 | 12 | 10 | 2 |
| 16 | 26 | 8 | 10 | 3 |
| Total | 32.37 | 15.81 | 9.78 | 1.44 |
In the radiological study, of the 16 cases operated on with prostheses, 11 presented with an accurate implantation and alignment, whilst in five cases the prostheses was subluxated. Reintervention was necessary to remove the implant and perform complete trapeziectomy in six cases, all of which were due to poor pain control and functional limitations. Only three prostheses of the patients who were operated on again were subluxated. No relationship was observed between the radiological alignment of the prosthesis and functional outcome. There were no signs of implant loosening (Fig. 2).
DiscussionPyrolytic carbon prostheses were proved to have poorer midterm functional results compared with the Burton–Pellegrini technique and the initial hypothesis of this study was therefore rejected.
In 2005, PyroDisk pyrolytic carbon prostheses were developed. This is a biconvex implant with a central orifice through which a hemi-plasty of the flexor carpi radialis tendon was passed to provide joint stability and to replace the complex anatomy of the trapeziometacarpal joint (PyroDisk, Integra Life Sciences, Plainsboro, NJ). Initially this had advantages over the other techniques, such as the preservation of the thumb length as minimum bony resection was required, its duration, the low amount of friction of the material, due to similar elasticity as the bone, the disappearance of problems such as metalosis and wear and tear of polyethylene observed in other models.19–24 However, these advantages were not able to be shown in our study.
Regarding postoperative pain, we observed disparity in the results published to date: both Barrera-Ochoa et al. and Mariconda et al. referred to a VAS of 1.7 and 0.5 points on termination of their follow-up periods.11,25 Furthermore, Maru et al. referred to a mean VAS on termination of follow-up of 5.6, even higher than that of this study.26 In this study, the mean VAS on termination of follow-up was 4.9, with a high variation of between 0 and 9 in the patients. On the contrary, the patients who underwent the technique described by Burton–Pellegrini presented a VAS of 1.43 (0–3), with these results being more homogeneous and in keeping with the literature.9
With regard to functionability, according to the QuickDash test, the obtained outcomes with pyrolytic carbon prostheses showed high disability scores, with a mean of 31.14 points. Moreover, a higher variation of results was also observed in patients intervened with PyroDisk, with patients who referred to zero disability (0 points) and patients with a score on the QuickDash test of 70 points, which made the results much more unpredictable. Along the same lines, Maru et al. published a series of 18 cases with pyrolytic carbon prostheses (Pi2) with a mean QuickDash of 35 points after mean follow-up of 20 months.26 Furthermore, Barrera-Ochoa et al. published a series of 19 cases comparable with those of this study with a follow-up of 5 years in which they reported 90% satisfaction results, with a VAS mean of 1.7 points. However, mean disability of the limb according to the QuickDash test was 20.2 points.11
The rate of reoperations in our series was 37.5% of the total prostheses implanted, after a minimum follow-up of 10 months. A high rate of reoperations has already been reported by several authors: Maru et al. with 33% with the model Pi2, Colegate-Stone et al. with 21% reoperations with the same model and Martínez de Aragón et al. with 29% reoperations with the NuGrip hemi-arthroplasty which is also pyrolytic.25–28 Barrera-Ochoa et al., however, report only 10% revisions surgery in their PyroDisk type prostheses with a mean follow-up of 5years.11
It has not been possible to demonstrate the link between subluxation of the implant and the rate of reoperations, since only three of the prostheses requiring reoperations presented with malposition. In their series, Barrera-Ochoa et al. also presented four of their cases with a radiological subluxation during follow-up11: reoperation was necessary in just two cases.
The radiological diagnosis of loosening described by some series of pyrolytic carbon prostheses should be analysed. The radiolucency line (<1mm) around the implant is a normal radiological finding in pyrolytic carbon prostheses. The implant is composed of a nucleus of radiopaque graphite, covered by pyrolytic carbon which is radiotransparent. The lucency is the radiotransparent coating layer and a thin fibrous membrane which forms the adaptation of the bone to the implant.16,17 We would only consider that the implant had become loose in the case of a radiolucency above 1mm, which in our series was not observed in any cases.
There are several limitations to this study. Firstly, it is a retrospective study with a small sample size. Secondly, this is a new surgical technique and the cases presented may be considered part of a learning curve of prosthesis implantation.
To conclude, in this study, pyrolytic carbon prostheses presented poor functional outcomes and high midterm pain scores. The fact that these results are worse than those of the standard technique and that rescue is technically demanding should be taken into account when choosing the type of technique to treat rhizarthrosis. Randomised long-term studies are probably needed to demonstrate whether one technique is superior to another.
Level of evidenceLevel of evidence III.
Ethical liabilitiesProtection of people and animalsThe authors declare that the procedures followed comply with the ethical standards of the Committee responsible for human experimentation, the World Medial Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have adhered to the protocols of their centre of work on patient data publication.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe first signatory author of the manuscript declares in his name and on behalf of all the signatories that there is no potential conflict of interests with this article.
Please cite this article as: Cuenca-Llavall M, Lizano-Díez X, Cruz-Sánchez M, Cebamanos-Celma J, Pidemunt-Moli G. Análisis funcional comparativo entre la prótesis de carbón pirolítico y la artroplastia de suspensión-reconstrucción ligamentosa para el tratamiento de la rizartrosis del pulgar. Rev Esp Cir Ortop Traumatol. 2018;62:373–379.