To describe a novel coronal osteotomy of the external facet of the patella, and to evaluate if the outcomes of the treatment of lateral knee compartment syndrome (LKCS) with this osteotomy, combined with the release of the external lateral retinaculum, are better than the isolated lateral retinacular release.
Material and methodsA prospective study with a 2 year follow up that included 70 patients diagnosed with LKCS, distributed into 2 groups. The first group included 50 patients on whom the lateral retinacular release combined with osteotomy was performed, and a second group on whom an isolated retinacular release was performed. Measurements were made using the Werner functional scale before the surgery and at 3, 12, and 24 months follow-up.
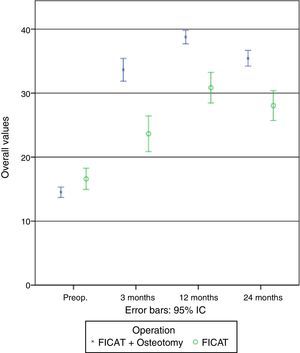
ResultsThere were significant differences in the overall functional state between the two groups after the surgery (better in the osteotomy group at all the intervals, P<.05). The improvement, which was progressive up to 12 months, was slightly less at 24 months, although the values were still better than the pre-surgical ones in both groups. Pain was the variable that showed most improvement. The patients with LKCS with degenerative signs showed a benefit in all cases.
ConclusionThe results demonstrate that the described patellar osteotomy technique, combined with lateral retinacular release, significantly improves the pain and the functional scale score of patients with LKCS after 2 years of follow-up, to a greater extent than isolated lateral retinacular release, including those in which there was evidence of degenerative signs.
Descripción de una nueva osteotomía coronal de la faceta externa de la rótula y valorar si los resultados del tratamiento del síndrome de compresión lateral de la rótula (SCLR) con nuestra osteotomía junto a la liberación del retináculo lateral externo son mejores que la liberación aislada del retináculo lateral.
Material y métodosEstudio prospectivo con 2 años de seguimiento, donde tratamos 70 pacientes diagnosticados de SCLR y distribuidos en 2 grupos: un primer grupo de 50 pacientes en los que se realizó la liberación del retináculo lateral asociada a osteotomía, y un segundo grupo de 20 pacientes en los que se realizó una liberación aislada del retináculo lateral. Se midió la escala funcional de Werner de forma preoperatoria y a los 3, 12 y 24 meses.
ResultadosExisten diferencias significativas en el estado funcional global postoperatorio entre grupos (mejor el grupo de osteotomía en todos los intervalos, p<0.05). La mejoría, que es progresiva hasta los 12 meses, experimenta un ligero retroceso a los 24, aunque los valores siguen siendo mejores que los preoperatorios en ambos grupos. Todas las variables muestran valores mejores en el grupo de la osteotomía. La variable con mayor mejoría es aparición del dolor. Los pacientes con SCLR con signos degenerativos presentaron un beneficio en todos los casos.
ConclusiónLos resultados muestran que la técnica de osteotomía rotuliana descrita asociado a la liberación del retináculo lateral mejora de forma significativa el dolor y la escala funcional de pacientes con SCLR a los 2 años de seguimiento, en mayor grado que lo hace la liberación aislada del retináculo lateral, incluso en aquellos en los que existe evidencia de signos degenerativos.
Merchant's1 classical classification of femoral and knee alterations includes lateral patella compression syndrome (LPCS). This is characterised clinically by pain in the anterior facet of the knee without episodes of true instability. Radiologically it is characterised by patella inclination, this being centred in the groove. Chronic alteration of the pressure in the medial facet and overload in the lateral facet give rise to arthrosic degeneration which when associated with lateral tension of the retinaculum may lead to a persistently painful retinaculum before signs of cartilage degeneration are noticed.
In LPCS the lateral retinaculum is too tense, giving rise to imbalance and patella inclination.2 Since Merchant and Mercer3 published the surgical technique they termed “lateral release of the patella” in 1974, this technique has become widespread, and its over-use has sometimes led to complication and poor results.4 Satisfactory results are reported in from 14% to 100%5–8 of cases. Nevertheless, it is hard to evaluate the results of releasing the lateral retinaculum and to compare the published results of this, due to the different evaluation systems used and patient selection, as many studies do not differentiate between those who mainly presented pain or instability.
This study presents a new surgical procedure which has the aim of improving the results obtained with release of the lateral retinaculum in patients with LPCS.
Although there is no certainty as to whether patella pain is directly caused by excessive pressure or if it is a part of a set of pathological phenomena which lead to degeneration of the subchondral bone, some authors have proposed the use of perforations of the bone to resolve excessive patella pressure, with different results: Almeida et al.,9 Schneider et al.10 or Miltner et al.11.
In patella osteotomies and regardless of the plane in which we perform them, we know that they will give rise to a reduction in intrabone pressures, and that this may be the main cause of the clinical improvement obtained in patients.
The aim of this study is to present the results of coronal osteotomy of the external facet of the patella in patients who suffer anterior knee pain due to LPCS after a follow-up of 2 years, comparing them to a control group and assuming that the venous decompression due to the osteotomy would improve the results of isolated release of the lateral retinaculum.
Material and methodsA comparative non-randomised prospective clinical study to evaluate the efficacy of coronal osteotomy of the external facet in association or not with freeing of the lateral retinaculum.
From January 2008 to December 2010 coronal osteotomy of the external facet of the patella associated with the release of the lateral retinaculum was performed in 50 patients. Simple release of the lateral retinaculum was performed in 20 patients who presented LPCS.
This is a prospective study that includes patients referred from external traumatology and rehabilitation departments with the diagnosis of lateral patella compression who fulfilled the inclusion criteria. They were treated using 2 different surgical procedures: the first group was treated using intraosseous patella decompression and release of the lateral retinaculum. The second and control group consisted of 20 patients who fulfilled the inclusion criteria and who were treated solely by release of the lateral retinaculum. In both groups a radiological protocol was followed prior to surgery with a series of simple anteroposterior, lateral and axial X-rays at 20° and 45°.
The patients included were diagnosed LPCS based on clinical and radiological criteria after conservative treatment during a period of at least 6 months had failed. From a clinical point-of-view they had to present pain in the anterior facet of the knee that increased with activities such as climbing or descending stairs or following long periods of time with the knees flexed. The patella compression test had to be positive, without episode of instability or signs of the same in the clinical examination. The radiographic criteria considered were unaltered patella height (Caton's index12 in lateral X-rays of the knee flexed at 30° from 0.6 to 1.3), an increase of Laurin's femoral-patella index13 above 1.6 (measured at 20° flexion) with normality of de Merchant's angle14 (less than 16°, measured at a 45° angle in flexion).
The exclusion criteria were an age below 18 years old or above 70 years old, patella subluxation, patients with mental or legal incapacity or who consumed drugs or refused to take part in the study, acceptance of which had to be expressed in the form of consent.
Conservative treatment prior to surgery consisted of restriction, as far as possible, of the activities which aggravate the pathology, together with analgesic-anti-inflammatory medication on patient demand and a 6-month long rehabilitation programme. The latter was based on lower limb mobilisation and elasticity work, with neuromotor control and muscular strengthening techniques. This treatment was undertaken by the Hospital Rehabilitation Unit. Daily sessions took place during the first 2 months (5 days a week) in the hospital gymnasium, while for the following 4 months each patient continued with exercises at home.
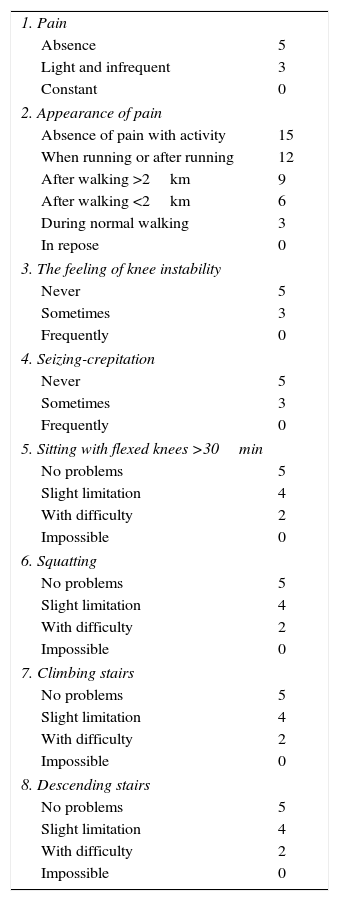
Patients with pain in the anterior facet of the knee were evaluated using a modification of Werner's functional scale15 prior to surgery and at 3, 12 and 24 months after the same. This scale contains 8 variables that score in such a way that the higher the score, the better the result. Zero is the lowest possible score and 50 is the highest (Table 1).
Modified Werner's functional scale for patients with pain in the anterior face of the knee.
| 1. Pain | |
| Absence | 5 |
| Light and infrequent | 3 |
| Constant | 0 |
| 2. Appearance of pain | |
| Absence of pain with activity | 15 |
| When running or after running | 12 |
| After walking >2km | 9 |
| After walking <2km | 6 |
| During normal walking | 3 |
| In repose | 0 |
| 3. The feeling of knee instability | |
| Never | 5 |
| Sometimes | 3 |
| Frequently | 0 |
| 4. Seizing-crepitation | |
| Never | 5 |
| Sometimes | 3 |
| Frequently | 0 |
| 5. Sitting with flexed knees >30min | |
| No problems | 5 |
| Slight limitation | 4 |
| With difficulty | 2 |
| Impossible | 0 |
| 6. Squatting | |
| No problems | 5 |
| Slight limitation | 4 |
| With difficulty | 2 |
| Impossible | 0 |
| 7. Climbing stairs | |
| No problems | 5 |
| Slight limitation | 4 |
| With difficulty | 2 |
| Impossible | 0 |
| 8. Descending stairs | |
| No problems | 5 |
| Slight limitation | 4 |
| With difficulty | 2 |
| Impossible | 0 |
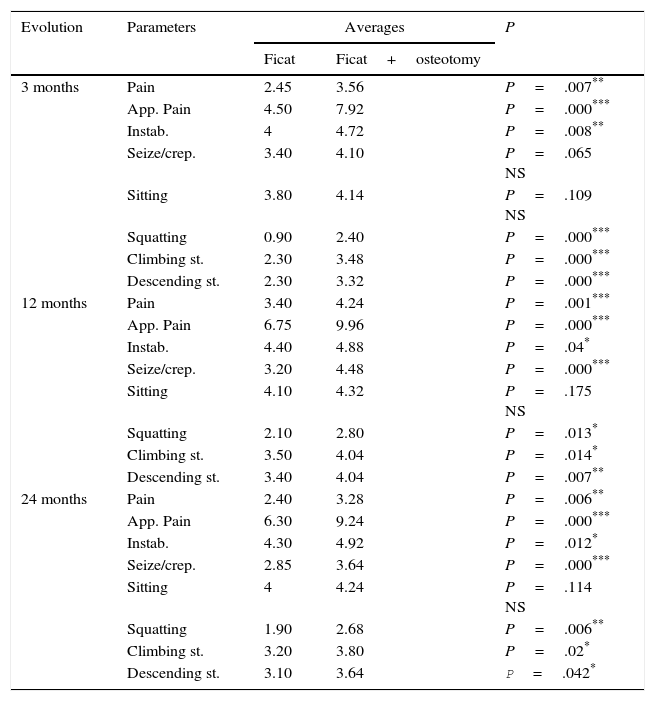
8 study variables are included in this analysis: pain, the appearance of pain, the feeling of knee instability, seizing-crepitation, sitting with flexed knees <30min., squatting, climbing and descending stairs (Table 2).
Results of analysis of Ficat's technique.
| Parameters | Averages | P | |||||
|---|---|---|---|---|---|---|---|
| Preop. | 3m | 12m | 24m | Preop.–3m | 3m–12m | 12m–24m | |
| Pain | 0.00 | 2.45 | 3.40 | 2.40 | P=.000*** | P=.017* | P=.010** |
| Appearance of pain | 2.25 | 4.50 | 6.75 | 6.30 | P=.002** | P=.001*** | P=.317 NS |
| Feeling of knee instability | 3.90 | 4 | 4.40 | 4.30 | P=.317 NS | P=.046* | P=.317 NS |
| Seizing-crepitation | 0.75 | 3.40 | 3.20 | 2.85 | P=.001*** | P=.860 NS | P=.102 NS |
| Sitting with knees flexed | 3.90 | 3.80 | 4.10 | 4.00 | P=.317 NS | P=.196 NS | P=.577 NS |
| Squatting | 1 | 0.90 | 2.10 | 1.90 | P=.317 NS | P=.001*** | P=.157 NS |
| Climbing stairs | 2.50 | 2.30 | 3.50 | 3.20 | P=.157 NS | P=.001*** | P=.083 NS |
| Descending stairs | 2.30 | 2.30 | 3.40 | 3.10 | P=1 NS | P=.001*** | P=.083 NS |
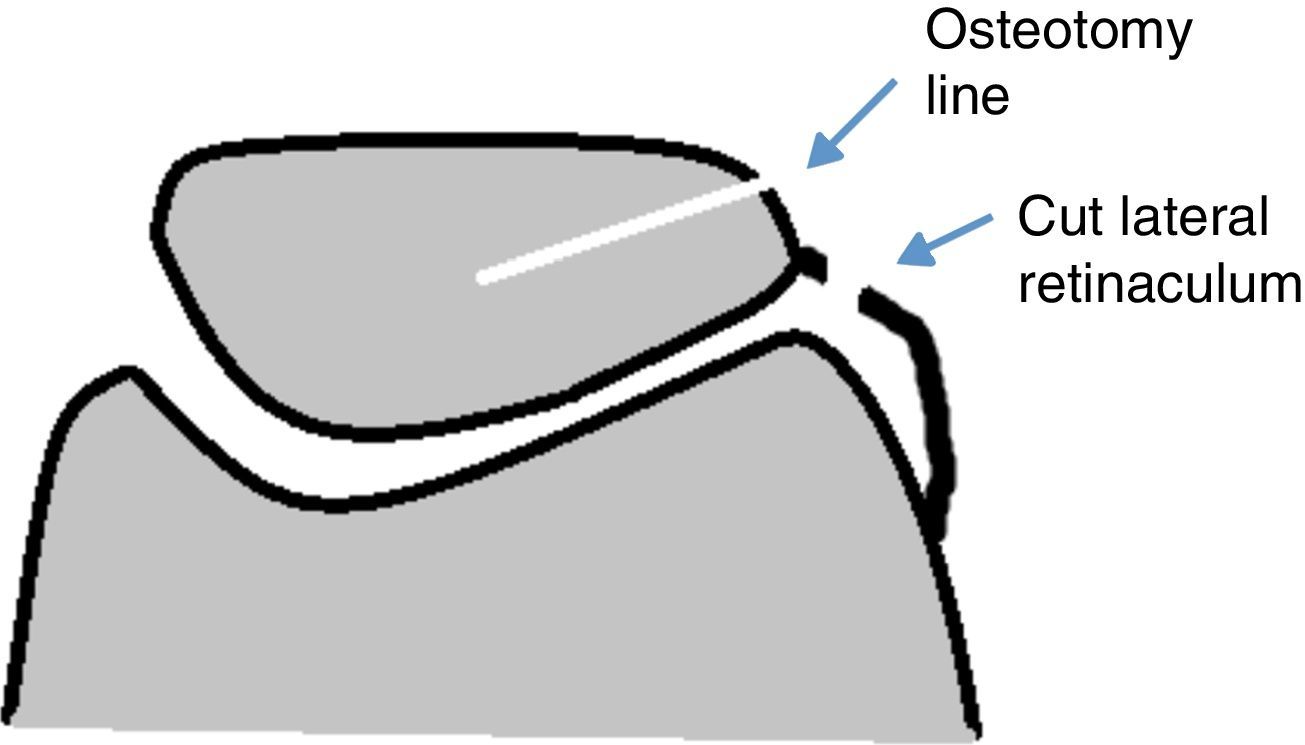
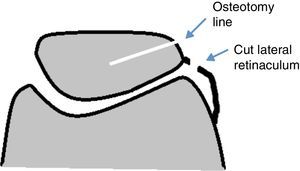
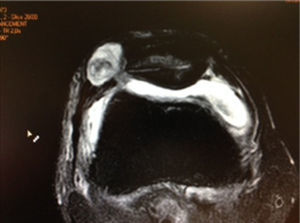
Surgery took place with the patient in supine decubitus, with ischaemia of the limb to be operated and spinal anaesthesia. 2 supports were used to ensure that the knee was comfortably in a position of 60° flexion without the need for an assistant to hold it. After making an incision of approx. 2cm in the external paralateral zone the lateral retinaculum was released outside the joint while avoiding an arthrotomy. In a second phase a coronal osteotomy was performed on the external edge of the patella using an oscillating saw, from its proximal edge to its distal edge and up to the mid-line of the patella (Figs. 1 and 2), with the aim of reducing bone pressure on the patella. The subcutaneous plane and skin was then closed. This procedure took an average time of 15min from start to finish.
24h after this procedure the patient started a rehabilitation programme with mobilisation from 0° to 60°, reaching 90° on the third day. The protocol followed was controlled by the Hospital Rehabilitation Unit.
All of the operations and the revisions of the same were carried out by the same surgeon. Overall analysis of the scale was used to analyse their progress over time, followed by detailed analysis of each section. Each patient was measured 4 times, which we identify by the time at which they took place: preoperative, after 3 months, 12 months and 24 months. The results of each measurement are shown as an average and standard deviation. To evaluate how the score of each variable varies before and after the operation we compared the preoperative values with the average of those in the 3 following measurements. Comparisons were established between the different time intervals using Student's t-test for groups of samples. The improvement was also evaluated by analysing the difference between the preoperative value of each scale heading and the average of the 3 postoperative values. P<.05 was considered significant.
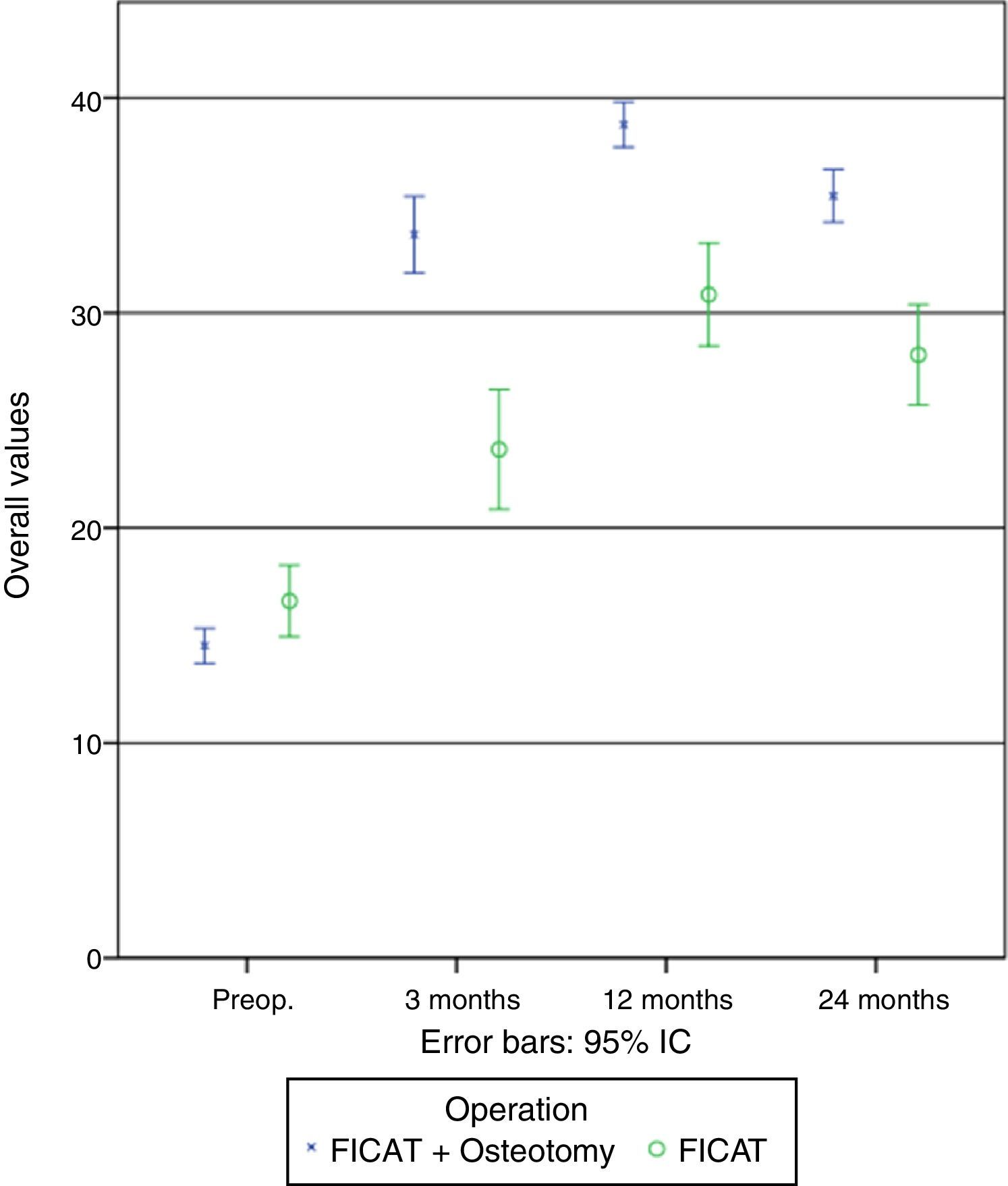
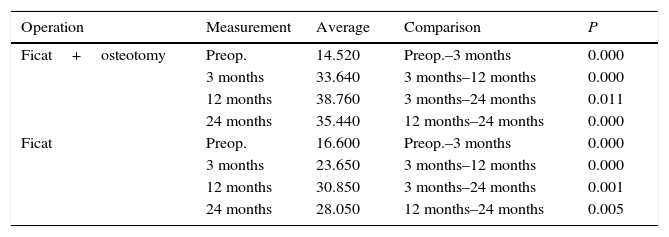
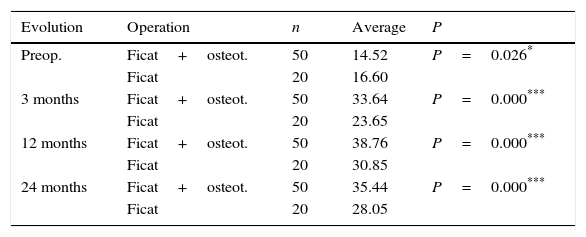
ResultsThe scores of different groups were compared at the different measurement intervals, as were those of each group at the different intervals (Fig. 3).
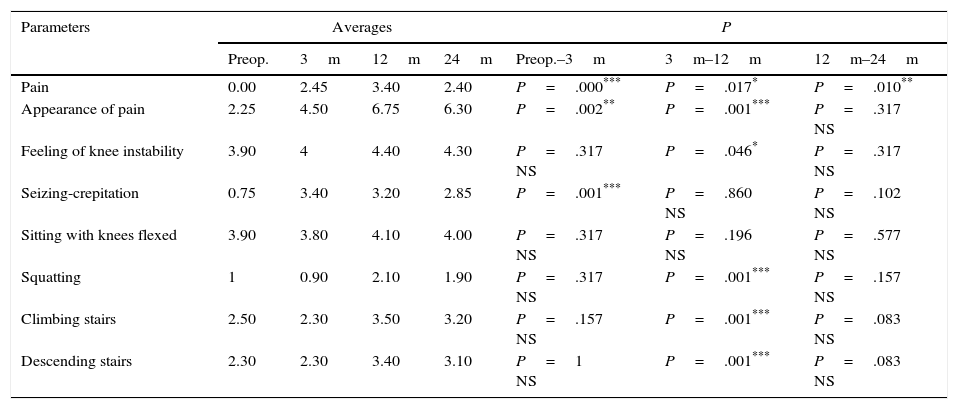
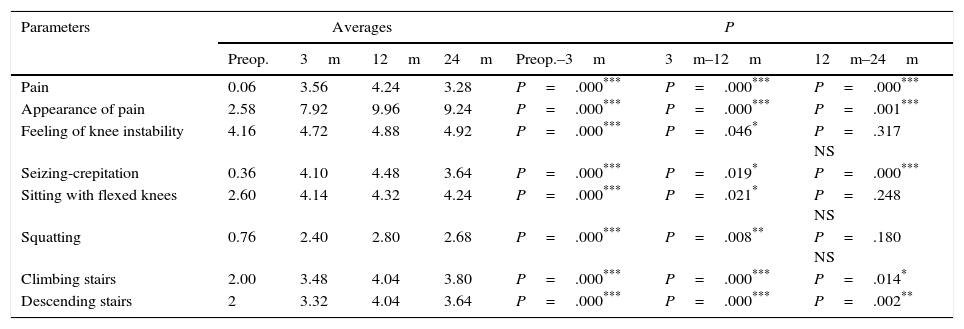
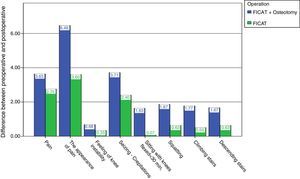
When each procedure was analysed separately, we found the following results (Tables 3 and 4 and Fig. 4):
- •
Release of the lateral retinaculum. After 3 months there is a significant improvement in the parameters for pain (P<.001), the appearance of pain (P<.01) and seizing/crepitation (P<.001), while no significant changes were found in any other parameter.
Results of analysis of Ficat's technique together with coronal osteotomy of the external facet.
| Parameters | Averages | P | |||||
|---|---|---|---|---|---|---|---|
| Preop. | 3m | 12m | 24m | Preop.–3m | 3m–12m | 12m–24m | |
| Pain | 0.06 | 3.56 | 4.24 | 3.28 | P=.000*** | P=.000*** | P=.000*** |
| Appearance of pain | 2.58 | 7.92 | 9.96 | 9.24 | P=.000*** | P=.000*** | P=.001*** |
| Feeling of knee instability | 4.16 | 4.72 | 4.88 | 4.92 | P=.000*** | P=.046* | P=.317 NS |
| Seizing-crepitation | 0.36 | 4.10 | 4.48 | 3.64 | P=.000*** | P=.019* | P=.000*** |
| Sitting with flexed knees | 2.60 | 4.14 | 4.32 | 4.24 | P=.000*** | P=.021* | P=.248 NS |
| Squatting | 0.76 | 2.40 | 2.80 | 2.68 | P=.000*** | P=.008** | P=.180 NS |
| Climbing stairs | 2.00 | 3.48 | 4.04 | 3.80 | P=.000*** | P=.000*** | P=.014* |
| Descending stairs | 2 | 3.32 | 4.04 | 3.64 | P=.000*** | P=.000*** | P=.002** |
Evolution of the general values with time for each one of the groups operated. The comparisons show the P value for each one of the comparisons made.
| Operation | Measurement | Average | Comparison | P |
|---|---|---|---|---|
| Ficat+osteotomy | Preop. | 14.520 | Preop.–3 months | 0.000 |
| 3 months | 33.640 | 3 months–12 months | 0.000 | |
| 12 months | 38.760 | 3 months–24 months | 0.011 | |
| 24 months | 35.440 | 12 months–24 months | 0.000 | |
| Ficat | Preop. | 16.600 | Preop.–3 months | 0.000 |
| 3 months | 23.650 | 3 months–12 months | 0.000 | |
| 12 months | 30.850 | 3 months–24 months | 0.001 | |
| 24 months | 28.050 | 12 months–24 months | 0.005 |
At 12 months there was a significant improvement in the parameters of pain (P<.05), the appearance of pain (P<.001), the feeling of knee instability (P<.05), squatting (P<.001) and climbing and descending stairs (P<.001) in comparison with 3 months’ evolution, while there were no changes in seizing and crepitation or sitting with the knees flexed.
At 24 months the pain parameter was significantly worse (P<.01), while the other parameters were at similar values to those found at 12 months.
- •
Osteotomy associated with release of the lateral retinaculum. At 3 months there was a highly significant improvement (P<.001) in comparison with the preoperative values for all of the parameters analysed.
At 12 months the values continued rising in comparison with those at 3 months, with changes that varied in significance in all of the parameters analysed: pain, the appearance of pain and climbing and descending stairs (P<.001), the feeling of instability in the knee and sitting with the knees flexed (P<.05), seizing and crepitation and squatting (P<.01).
At 24 months there was significant worsening compared with 12 months in pain, seizing and crepitation (P<.001), climbing and descending stairs (P<.05 and P<.01, respectively), although the resulting values are much better in patients with release of the lateral retinaculum. There were not changes in the other parameters.
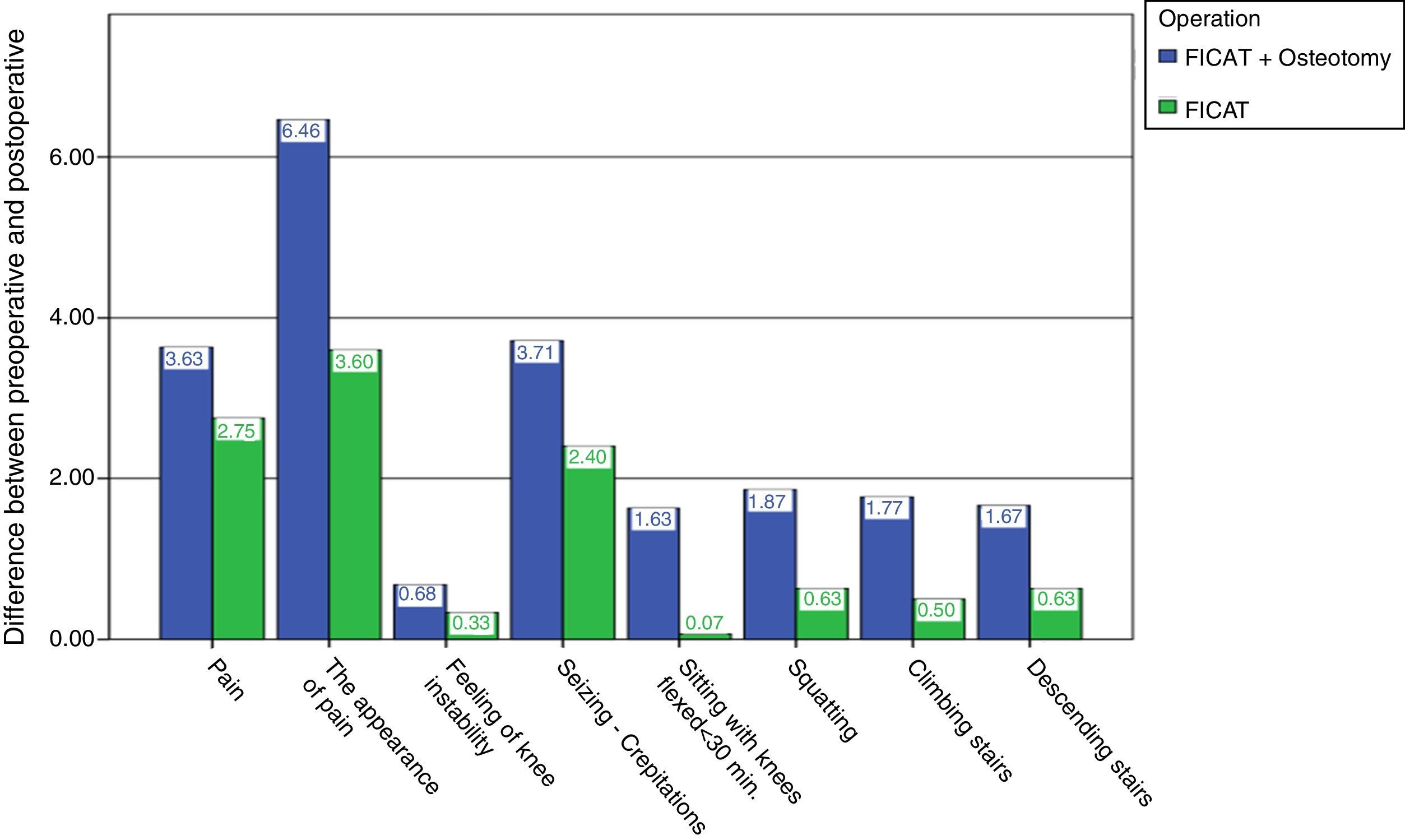
We found the following results when both groups were compared (Tables 5 and 6 and Fig. 5):
- •
When the results of both techniques are compared, we found that the values in patients with release of the retinaculum and osteotomy were better in all of the parameters analysed and at all of the time intervals than were the patients with release of the lateral retinaculum (Table 6).
- •
When the different parameters are analysed we find that at 3 months there is a highly significant increase (improvement) (P<.001) in pain, the appearance of pain, the feeling of an unstable knee, squatting and climbing and descending stairs in the Ficat group together with osteotomy in comparison with the patients in the solely Ficat group.
Comparison of both groups for the different parameters.
| Evolution | Parameters | Averages | P | |
|---|---|---|---|---|
| Ficat | Ficat+osteotomy | |||
| 3 months | Pain | 2.45 | 3.56 | P=.007** |
| App. Pain | 4.50 | 7.92 | P=.000*** | |
| Instab. | 4 | 4.72 | P=.008** | |
| Seize/crep. | 3.40 | 4.10 | P=.065 NS | |
| Sitting | 3.80 | 4.14 | P=.109 NS | |
| Squatting | 0.90 | 2.40 | P=.000*** | |
| Climbing st. | 2.30 | 3.48 | P=.000*** | |
| Descending st. | 2.30 | 3.32 | P=.000*** | |
| 12 months | Pain | 3.40 | 4.24 | P=.001*** |
| App. Pain | 6.75 | 9.96 | P=.000*** | |
| Instab. | 4.40 | 4.88 | P=.04* | |
| Seize/crep. | 3.20 | 4.48 | P=.000*** | |
| Sitting | 4.10 | 4.32 | P=.175 NS | |
| Squatting | 2.10 | 2.80 | P=.013* | |
| Climbing st. | 3.50 | 4.04 | P=.014* | |
| Descending st. | 3.40 | 4.04 | P=.007** | |
| 24 months | Pain | 2.40 | 3.28 | P=.006** |
| App. Pain | 6.30 | 9.24 | P=.000*** | |
| Instab. | 4.30 | 4.92 | P=.012* | |
| Seize/crep. | 2.85 | 3.64 | P=.000*** | |
| Sitting | 4 | 4.24 | P=.114 NS | |
| Squatting | 1.90 | 2.68 | P=.006** | |
| Climbing st. | 3.20 | 3.80 | P=.02* | |
| Descending st. | 3.10 | 3.64 | P=.042* | |
Comparison of both groups (total score).
At 12 months the increase is still significant for all of the parameters except for sitting with the knees flexed, and we found a clear improvement in the Ficat and osteotomy group patients.
At 24 months and spite of values being lower than they were at 12 months in both groups, they are still significantly higher in the group of patients with lateral retinaculum release and osteotomy.
Sitting with the knees flexed is the only parameter that presents no significant differences between the 2 techniques used at any of the time intervals analysed.
The greatest improvement in patients with lateral retinaculum release appears after 12 months evolution, while for patients with lateral retinaculum release together with osteotomy, at 3 months they already attain similar or even higher values than the patients with lateral retinaculum release at 12 months.
By comparing the preoperative values with the average values at the 3 time intervals after operating it is possible to see that the variable which improves the most is the appearance of pain, followed by crepitation. This is shown graphically in Fig. 5.
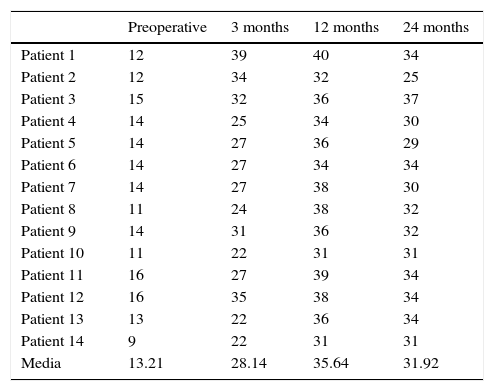
Study of the patients with LPCS and signs of advanced degeneration who were subjected to osteotomy together with release of the lateral retinaculum shows satisfactory results that are comparable with those of the group subjected to the complete operation (Table 7).
Evolution of the total score for Ficat+osteotomy in patients with degenerative signs (n=14).
| Preoperative | 3 months | 12 months | 24 months | |
|---|---|---|---|---|
| Patient 1 | 12 | 39 | 40 | 34 |
| Patient 2 | 12 | 34 | 32 | 25 |
| Patient 3 | 15 | 32 | 36 | 37 |
| Patient 4 | 14 | 25 | 34 | 30 |
| Patient 5 | 14 | 27 | 36 | 29 |
| Patient 6 | 14 | 27 | 34 | 34 |
| Patient 7 | 14 | 27 | 38 | 30 |
| Patient 8 | 11 | 24 | 38 | 32 |
| Patient 9 | 14 | 31 | 36 | 32 |
| Patient 10 | 11 | 22 | 31 | 31 |
| Patient 11 | 16 | 27 | 39 | 34 |
| Patient 12 | 16 | 35 | 38 | 34 |
| Patient 13 | 13 | 22 | 36 | 34 |
| Patient 14 | 9 | 22 | 31 | 31 |
| Media | 13.21 | 28.14 | 35.64 | 31.92 |
In this work the results show a significant improvement in pain and the functional scale in patients with LPCS after 2 years of follow-up after treatment with coronal osteotomy of the external facet and release of the lateral retinaculum, to a higher degree than was the case after simple release of the lateral retinaculum.
Merchant and Mercer3 published their description of the surgical procedure they termed “lateral release of the patella” in 1974. This procedure has now become widespread, and over-use of the same has sometimes given rise to complications and poor results. There seems to be agreement that the sine qua non to perform release of the lateral retinaculum is demonstration that it is under excessive tension,16 so that we should not perform this in situations when the patella is raised or when there is hyperelasticity or trochlear dysplasia.17 In LPCS the lateral retinaculum is too tense, giving rise to imbalance and inclination of the patella.2 The literature describes satisfactory results varying from 14% to 100%,7–9 although evaluation of the results of lateral retinaculum release and the comparison of published results are hindered by the different evaluation systems used, as well by patient selection. Many studies do not differentiate between patients who mainly presented pain or instability. This study presents an additional and new surgical procedure which improves on the results of isolated lateral release of the retinaculum in patients with LPCS.
In spite of the heterogeneous nature of these studies, some authors have recognised factors which correlate with less satisfactory results.18,19 These factors include female sex and those patients with established grade iii or grade iv changes in their joint cartilage, as well as those in whom patella instability instead of lateral oppression of the retinaculum is the main abnormality. On the contrary to what some authors state in the literature,20,21 in which they describe poor results in patients with grade iii or iv chondopathy after release of the lateral retinaculum, in our study all of the patients with radiological signs of advanced changes in the cartilage presented satisfactory results. The reduction of intrasseous pressure must therefore be considered to be a decisive factor in the final result of this group.
The effect of releasing the lateral retinaculum on patella biomechanics, as well as the different methods used, have been studied by several authors.22–26 We have restricted ourselves to cutting the most distal fibres in the proximal zone of the oblique lateral vastus, and distally at the level of the patella tendon.
The first osteotomies sought to reduce intraosseous pressure, to benefit from the effect of releasing the lateral retinaculum while also reducing the intraosseous pressure of the patella, trying to improve the results of solely releasing the lateral retinaculum.
Both of the groups operated were found to behave in the same way, given that in both the tendency seems to be a considerable improvement up to 3 months after the operation, another improvement up to 12 months and, finally, a slight worsening from 12 to 24 months. Even so, the final state at 24 months is better than it was at 3 months. After evaluating the results we can conclude that the differences observed between all of the time intervals described are statistically significant. They attain significantly higher values in all of the postoperative periods in the group with lateral release of the retinaculum and osteotomy than is the case in the group with only lateral release of the retinaculum. The differences between both groups are clear and significant at all levels.
For the group that only received release of the lateral retinaculum there is one variable (sitting with the knees flexed <30min) in which no significant difference is found. Therefore, in the light of the data, it does not seem to cause any change or affect this variable. The other variables can be divided into 2 groups. A first group consists of variables in which changes were observed after 3 months: pain, the appearance of pain and crepitation. A second group corresponds to those in which no significant differences were observed until 12 months, and this group includes the following variables: a feeling of instability in the knee, squatting, climbing and descending stairs. In this way we can see how the behaviour of each variable studied differs within this group.
For the group of retinaculum release together with osteotomy a clear improvement was observed in all of the variables at 3 months as well as at 12 months.
Although it cannot be known with absolute certainty whether patella pain is caused directly by excess pressure, or whether it is a part of the set of pathological phenomena that lead to degeneration of the subchondral bone, we can consider the patella to behave like a sealed compartment, unlike the epiphysis which is in contact with its diaphysis. In an attempt to resolve the pain caused by excess pressure, some authors have suggested the use of perforations of the patella bone. Almeida et al.9 showed, in their experimental study, that the said bone perforations did not lead to a reduction of pressure figures, regardless of whether or not there was a previous existing condition of excess pressure. Schneider et al.10 in 2000 and Miltner et al.11 in 2003 presented their cases which were satisfactory thanks to extra-articular bone perforations, with clinical improvement in anterior pain and a reduction in intraosseous pressure figures. Nevertheless, these are studies which have to be approached with caution, given both the measurement technique used and the selection of patients, as well as how their results are compared with those of the control group.
No perforations were made in this study, as the results obtained by the author in previous years withthese were not satisfactory. Nevertheless, a coronal osteotomy of the external facet was performed. The hypothesis is that the osteotomy we describe, coronal and solely of the external facet, is sufficient to achieve the said reduction in pressure, so that with minimum aggressiveness, an easy technique with swift recovery and which permits other techniques to be used as well, we are able to improve the results obtained with only releasing the lateral retinaculum, thereby leading to the benefit of the resulting fall in intraosseous pressure.
The varying score for each variable before and after the procedure can be seen in the results, when the preoperative values are compared to the average values at the 3 postoperative time intervals. An average increase was obtained in the scores for each one of the variables, giving us an idea of which variable improved the most, and allowing us to see that the variable which improved the most is that of pain, followed by crepitation.
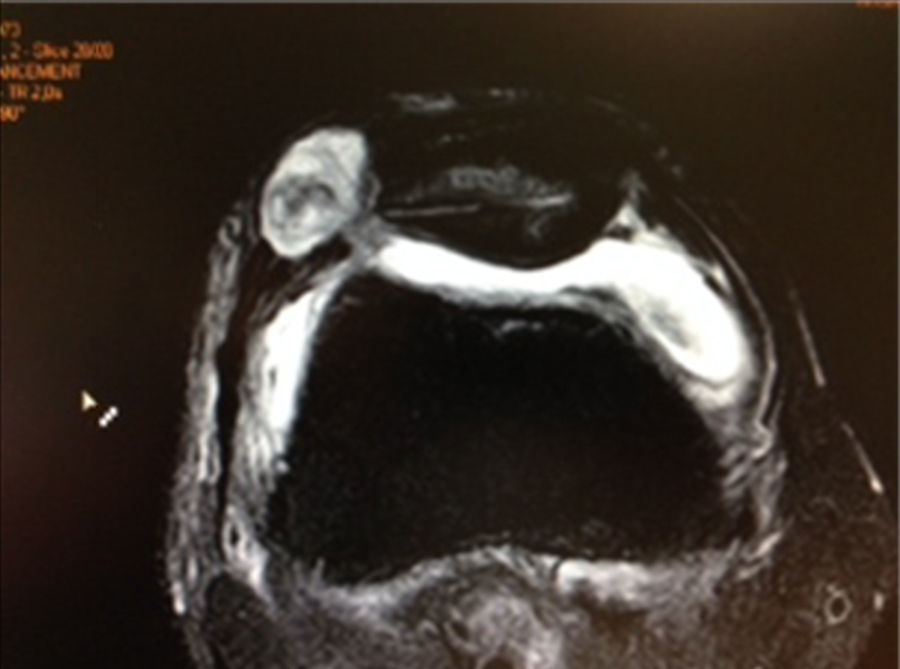
The most frequent complications27,28 which are described after the release of the lateral retinaculum include haematoma, weakness or atrophy of the quadriceps or medialisation of the patella.29–32 Only one complication arose in this study (Fig. 3) which we consider to be minor as it was resolved well. This complication was a fistula secondary to arthrotomy caused by releasing the lateral retinaculum. The said fistula was resolved satisfactorily within 3 weeks and altered neither the postoperative phase nor rehabilitation, so that the complications rate with the procedure of osteotomy associated with release of the retinaculum seems to be zero or very low.
The limitations of this study are the small size of its sample and its short follow-up period of 2 years, as well as its comparative non-randomised nature. Another limitation of our study is the functional scale that was used. Although this has been used in other studies, we are aware of the existence of more specific tests for the femoral-patella joint, such as Kujala's test.
This study was undertaken by a single surgeon who used the same surgical technique, with the same preoperative analysis and indications for this surgical treatment, as well as the same postoperative, rehabilitation and follow-up protocols.
We believe that the effect of bone decompression in association with release of the lateral retinaculum is a procedure that is hardly aggressive and which does not exclude subsequent surgery. It should be considered for LPCS within the therapeutic arsenal which is available to us.
ConclusionsThe results show that the patella osteotomy technique described is a new procedure that is not very aggressive and reproducible, and that when associated with release of the external patella retinaculum it significantly improves pain and the functional scale of patients with LPCS after 2 years of follow-up over the simple release of the lateral retinaculum.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that for this research no experiments took place with human beings or animals.
Data confidentialityThe authors declare that they followed the protocols of their centre of work for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rosales-Varo AP, Roda-Murillo O, Prados-Olleta N, García-Espona MA. La osteotomía patelar coronal de la faceta externa asociada a liberación del retináculo lateral mejora los resultados clínicos de la liberación lateral aislada en el síndrome de compresión lateral de rótula. Rev Esp Cir Ortop Traumatol. 2016;60:296–305.