A high percentage of knee osteoarthritis finally needs a knee replacement. Previous treatments used including viscosupplementation with hyaluronic acid can delay the knee replacement. The objective of this study was to estimate the economic impact in the short, medium and long term of the knee replacement delay, by conducting a budget impact analysis of the incorporation of viscosupplementation to the treatment of knee osteoarthritis.
From the data of patients treated at a specialised Knee Osteoarthritis Unit we built a discrete event simulation model that reproduced the progress of patients, as it could represent changes in the health status of an individual and their interaction with the system. The model allowed the number of prostheses and replacements performed each year to be calculated in a population including 1000 patients each year according to the use of viscosupplementation. The budget impact analysis was estimated for 10 years by adding the cost of each treatment.
A total of 224 patient candidates to receive a knee replacement were studied. The viscosupplementation use delayed the need to perform the knee replacement by 2.67 years The budgetary impact would lead to net savings during the 10 years. However, it is much greater in the earlier years. The sum of the savings in the first three years would be 36 million Euros.
The study concludes that the use of viscosupplementation reduced the economic burden of knee osteoarthritis in the health system as a result of delayed knee replacement. The simulation model enabled the economic impact in both the short and long term to be analysed.
Una gran parte de los pacientes con artrosis de rodilla acaban siendo intervenidos de una prótesis. Los tratamientos previos utilizados entre ellos la viscosuplementación con Ácido Hialurónico pueden permitir retrasar esta evolución lo que conlleva un impacto económico a corto, medio y largo plazo. El objetivo de este estudio fue estimar el análisis del impacto presupuestario de la incorporación de la viscosuplementación.
A partir de un estudio retrospectivo de pacientes tratados con viscosuplementación se construyó un modelo de simulación de eventos discretos que reprodujo la evolución de los pacientes ya que permite representar cambios en el estado de salud de un individuo y su interacción con el sistema. El modelo permitió, calcular el número de prótesis y recambios efectuados cada año en una población que cada año incorpora 1000 pacientes. Añadiendo los costes de cada uno de los tratamientos aplicados se estimó el análisis del impacto presupuestario.
Se estudiaron 224 pacientes. El uso de viscosuplementación retrasó 2,67 años la necesidad de implantación de la prótesis. Al analizar el impacto presupuestario se estimó un ahorro continuado a lo largo del tiempo que es mucho mayor en los primeros años. Los ahorros de los primeros tres años fueron de 36 de millones de euros.
El uso de la viscosuplementación redujo la carga económica de la artrosis de rodilla en el sistema sanitario como consecuencia del retraso de la implantación de la prótesis. El modelo simulación permitió analizar conjuntamente el impacto económico a corto y largo plazo.
Knee osteoarthritis (KO) is a debilitating disease with a high prevalence in all populations, including Spain.1,2 Its burden for patients is not limited to pain and reduced quality of life, as it also leads to high costs, both within the hospital and outside.3,4 There are 2 different stages in the natural history of KO, depending on the treatment applied. The first is characterised by the use of alternative medical treatment based on several criteria such as the severity of symptoms and clinical response.5,6 Clinical practice guidelines accept several treatment options with the primary intention of controlling KO symptoms.5,7 These treatments include non-steroidal anti-inflammatory drugs (NSAIDs), viscosupplementation (VS) through intra-articular injections of hyaluronic acid and other treatment options such as SYSADOAS (Symptomatic Slow Acting Drugs in Osteo-Arthritis), paracetamol and opioids among others. VS provides the added benefit of delaying progression towards a knee prosthesis.6 The use of treatments such as VS is a decision to consider at the initial stage, since they involve more short-term costs, but represent savings in the medium and long term by delaying surgery. The second therapeutic stage, consisting in the surgical implantation of a prosthesis,7 is considered when the level of pain is so severe that it hinders daily activity.
The cost criterion is important when selecting medical treatments during the first phase, since they all improve symptoms without a clear superiority of any option in terms of effectiveness.5 However, the economic assessment of the treatment is complex because it must take into account both short-term costs due to the drug itself and long-term costs as a result of lengthening the time until prosthesis implantation. The methodology recommended by experts in order to analyse clinical decisions which have consequences in the short and long term evolution of patients is the representation of the natural history of the disease by mathematical models.8 Although there are few examples in the literature of studies using mathematical models applied to orthopaedic treatments, their application is conducted in the same way as any other pharmacoeconomic study, since they measure a change in the consumption of healthcare resources caused by KO according to the use or not of a treatment such as VS.9
Although various methods are used in the economic evaluation of new medical treatments, the most common is cost-effectiveness.10 One of the complaints that have been expressed is the difficulty of translating the findings to the context of a healthcare management system focused on budget. In response to these criticisms, a complementary tool known as budget impact analysis (BIA) has been used for years. This is aimed at estimating the impact of introducing a new drug on the budgets of coming years. According to Mauskopf, BIA measures the impact of a new treatment on the annual cost, the annual benefit on health and other outcomes of interest in the years following its introduction into a national healthcare system or private healthcare plan.11 There is scarce experience with BIA in the scientific literature since the format employed has generally been simple models based on assumptions from the literature and often on expert opinions. In recent years, several authors have proposed guidelines with more stringent requirements for the use of BIA and have thus endowed it with a better scientific standing.11–13
The objective of this study is the economic evaluation of the use of VS as a modifier of the natural history of KO in terms of impact on budget.
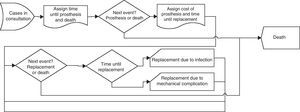
MethodsThe method used was the mathematical representation of the natural history of KO from the moment when patients reached a level of osteoarthritis which made them candidates for surgery. To do this, a discrete event simulation (DES) model was constructed,14–16 which reproduced the evaluation until the death of patients with KO and without VS, and which allowed us to measure costs in the short and long term. In biomedical research, DES models have been employed mainly to optimise the use of resources and the management of waiting lists, but their flexibility to represent different stages of a disease has made them increasingly present in the economic evaluation of new treatments.8 This flexible modelling approach is characterised by its capacity to represent the internal and external events affecting the entities and populations represented. For example, in healthcare, this means that it is possible to represent both the transitions in the health state of an individual and the way in which that individual interacts with other individuals or with the system. This flexibility allows the model to be used for a wide range of problems. DES was originally developed in the 60s, in the fields of industrial engineering and operational research, to represent industrial and business processes. Its first healthcare applications took place in the 80s and since then it has been employed in various fields, especially in pharmacoeconomics.
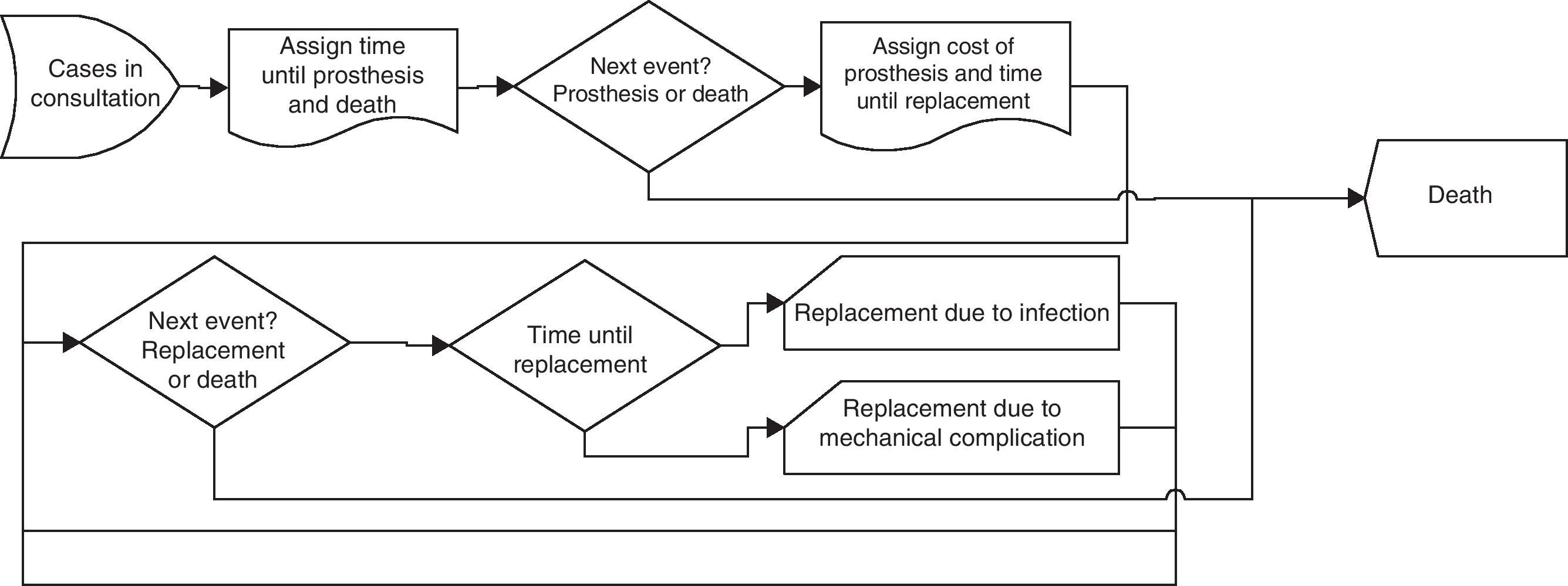
Conceptual modelIn order to evaluate the alternative treatment of KO with VS and without VS we used a conceptual model (Fig. 1) consisting of the following stages: KO, waitlist for initial prosthesis, status with operated knee, prosthesis replacement, status with replaced prosthesis and death. Due to their high cost, the model took into account both the prostheses and their replacements. In order to convert the conceptual model into an operational model we carried out a naturalistic retrospective study,17 which analysed data from the database of the Specialist Knee Osteoarthritis Consultation of Jaén Hospital (CMAR). This consultation serves patients who are candidates for implantation of a knee prosthesis with an alternative approach involving intraarticular viscosupplementation (NASHA hyaluronic acid: Durolane®) according to the protocol of the traumatology and orthopaedic surgery service of the centre. Durolane® is stabilised hyaluronic acid (NASHA), causing it to degrade more slowly and remain within the joint for up to 8 weeks.18 This enables it to be applied in a single administration per treatment cycle, unlike traditional hyaluronic acid compounds which require multiple injections per treatment cycle. As a control group, we analysed patients with KO treated conventionally (without VS) in traumatology consultation, who were included in the surgery waitlist once the prosthesis was indicated. In both groups, the intervention criterion was based on the quality of life of each patient according to the judgement of the physician. Since both treatment alternatives served the same population with KO, we considered measuring the cost of the process according to the approach used in order to test the hypothesis that VS lengthens the time until knee prosthesis implantation, and that the surgical interventions thus avoided offset the costs of VS.6 In the CMAR consultation, patients were asked about their clinical status. If they had remained stable or had improved after viscosupplementation then the treatment was maintained, but when patients had worsened they were referred back to the surgical waitlist for knee prosthesis. The decision by the researcher regarding the most appropriate care or treatment for each patient was not interfered with under any circumstances. The variables studied in both groups were: age, gender, height, weight, activity, occupation, date of first consultation, date of inclusion in waiting list for prosthesis, date of prosthetic intervention, condition on current date, date of death, number of VS sessions, severity of osteoarthritis according to the classification of Kellgren & Lawrence19 and medical treatments received. The statistical analysis of differences in sociodemographic characteristics between the 2 groups was performed using the Chi-square test, whereas the Fisher exact test was applied in the case of binary variables. We used the Student t test for comparison of means or the Wilcoxon nonparametric test when normality was not followed. We used the Kolmogorov–Smirnov test in order to verify the normal distribution of variables. We used this same method in the comparison of means between groups. The statistical analyses were performed using the software package SPSS® v.19.0 for Windows.
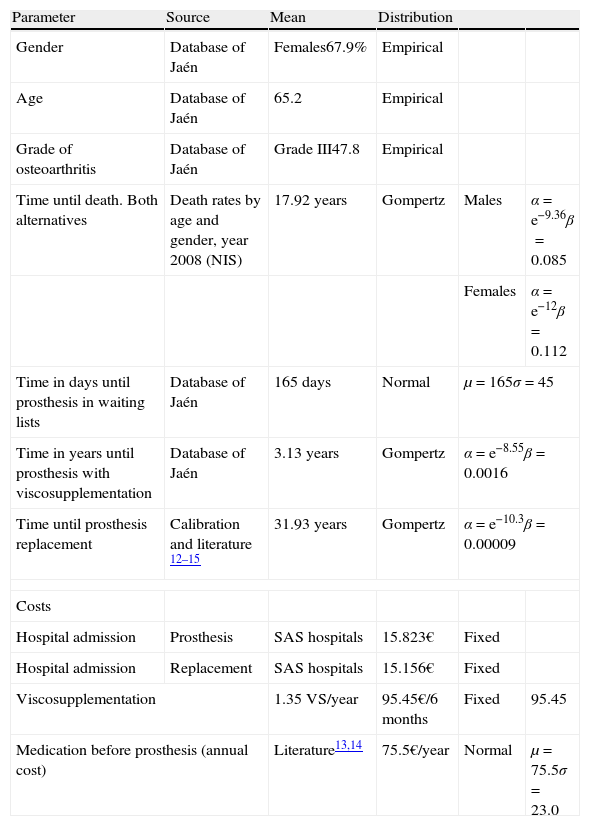
Mathematical simulation modelThe parameters of the model are shown in Table 1. It represents the competitive or concurrent risks that are relevant in these patients.8 On the one hand there is the risk of death corresponding to their age and gender, which is notable because these were middle-aged patients, and on the other hand is the risk of undergoing knee prosthesis surgery. Finally, the model incorporates the possibility of patients suffering complications and requiring another operation to replace the initial prosthesis. The working hypothesis of the study is that improvement in patient outcomes due to VS will delay the need for a prosthesis. The risks of death, prosthesis and replacement compete with each other so that, upon delaying the prosthesis, some individuals will die before the initial intervention or replacement. The consequence is that there will be a reduction in the number of surgical interventions without affecting the quality of life of patients. The model enables us to quantify the interaction between these elements in a joint manner and, therefore, to measure the number of interventions, the different times and, finally, the costs involved.
Parameters of the model.
| Parameter | Source | Mean | Distribution | ||
| Gender | Database of Jaén | Females67.9% | Empirical | ||
| Age | Database of Jaén | 65.2 | Empirical | ||
| Grade of osteoarthritis | Database of Jaén | Grade III47.8 | Empirical | ||
| Time until death. Both alternatives | Death rates by age and gender, year 2008 (NIS) | 17.92 years | Gompertz | Males | α=e−9.36β=0.085 |
| Females | α=e−12β=0.112 | ||||
| Time in days until prosthesis in waiting lists | Database of Jaén | 165 days | Normal | μ=165σ=45 | |
| Time in years until prosthesis with viscosupplementation | Database of Jaén | 3.13 years | Gompertz | α=e−8.55β=0.0016 | |
| Time until prosthesis replacement | Calibration and literature 12–15 | 31.93 years | Gompertz | α=e−10.3β=0.00009 | |
| Costs | |||||
| Hospital admission | Prosthesis | SAS hospitals | 15.823€ | Fixed | |
| Hospital admission | Replacement | SAS hospitals | 15.156€ | Fixed | |
| Viscosupplementation | 1.35 VS/year | 95.45€/6 months | Fixed | 95.45 | |
| Medication before prosthesis (annual cost) | Literature13,14 | 75.5€/year | Normal | μ=75.5σ=23.0 | |
NIS: National Institute of Statistics; SAS: Andalusian Health Service; VS: viscosupplementation.
The data required for the model were obtained directly from the Jaén CMAR or from the literature, and are presented in Table 1. The ages, genders and severity of the condition of patients in the cohort were those registered by the Jaén CMAR. The parameters of the Gompertz function which reproduces life expectancy by age and gender were calculated through mortality rates of the Spanish population in 2008 obtained from the National Statistics Institute.20 In the model, the mean life expectancy until the death of patients was of 17.92 years, which corresponded well with the mean age of 65.72 years upon entry into the model.
We used a Gompertz function to assign the time until prosthesis of patients with viscosupplementation. The function parameters were obtained by analysis of survival of the Jaén CMAR database. The use of survival analysis was due to the right-censored nature of data at the Jaén consultation. Parametric models were used to calculate an absolute value of survival for a given risk profile. Each model had a different risk profile and statistical tests enabled us to select the model that fits best. In order to extrapolate the time until prosthesis we tentatively used survival parametric models to calculate the baseline risk function. In the analysis, the baseline risk was modelled using the most common exponential distributions, Weibull and Gompertz,9 and the best fit of the models analysed was obtained with the Gompertz function. The time until prosthesis in the control group was assigned by a normal distribution whose parameters were calculated from the data of the waiting list of the same hospital in Jaén.
The parameters of the Gompertz distribution for time until prosthesis complication were calculated from the literature. The characteristic of this function was that risk increased with time. The distribution applied by type of complication was 50% by infection and 50% by loosening. The main references were not only the technical report and articles on the cost-effectiveness of hip replacement models by Briggs et al.,9,21,22 but also publications on the survival of knee prostheses derived from prosthesis records, which indicated a mean annual risk of 1.26%.23,24 This mean annual risk meant that, for each year of life, 1.26 patients out of every 100 would require a replacement.
Although some publications give results in the form of constant risk,22,25 in accordance with the analysis of risk of replacement in hip prostheses by Briggs, we believe that the risk increases with duration and that it reaches a final maximum point as a result of material fatigue.9 This assessment is also supported by all existing literature on the effect of wear particles on the aetiology of osteolysis linked to prosthesis loosening.26,27 The median time until replacement was 31.93 years. This meant that, at that point in time, the risk of replacement was 50% if no other risks were taken into account. Evidently, in reality less than 50% of knee prostheses are replaced because individuals suffer from other competing risks, such as death.
The model incorporated an annual cohort of 1000 patients for 10 years and estimated the following results year after year for the 2 alternatives: duration of each stage (osteoarthritis and prostheses), cost of each stage, life expectancy of patients, number of prosthetic implants and number of replacements conducted.
Costs of the modelAs cost of VS we included only the cost of the medication, which was 140€ for each infiltration. Since each patient received a mean 1.35 injections per year, the cost was 95.45€ per semester. We assumed that the healthcare process included the same consultations before and after the prosthesis in the 2 alternatives, so, therefore, the cost of consultation was the same for both. The hospital cost of the initial prosthesis (15,823€) and the replacement (15,156€) were obtained from the rates of the Andalusian Health Service. The cost of medical treatments before the prosthesis with and without VS was obtained from the literature. Two works published by Spanish authors give almost equal figures of 75.5 and 77€ per year.28,29
Economic assessmentThe methodology used in the economic evaluation was BIA.10,30 The analysis assumed that the 2 treatment alternatives being evaluated were equally effective. Accordingly, the objective of the study was to identify the option associated with lower costs. The starting point of the study was that the natural history of KO requires patients to be treated medically for as long as possible, and, after this stage, to implant a prosthesis. The problem is that prostheses have a limited survival and, therefore, one clinical goal is to delay their implantation whenever possible. While in the control group the intervention took place as soon as the waiting list allowed it, in the alternative with VS therapy that period of time was lengthened for as long as the clinical condition of each patient was favourable. However, the intervention criterion remained the same as in the conventional approach, that is, patients were operated once their loss in quality of life required it, when analgesics and NSAIDs were no longer able to control the pain. Whenever VS treatment did not improve the condition of patients, they were automatically incorporated into the surgical procedure. Consequently, the 2 alternatives provided the same effectiveness, as the criteria to start surgical treatment were the same.
The simulation was repeated 100 times and the mean results were analysed. BIA required incorporating successive annual cohorts into the model. In our case, these cohorts always included 1000 patients with a time horizon of 10 years. This was considered without any adjustments, since the data for each year were presented separately and, therefore, did not require any changes.30
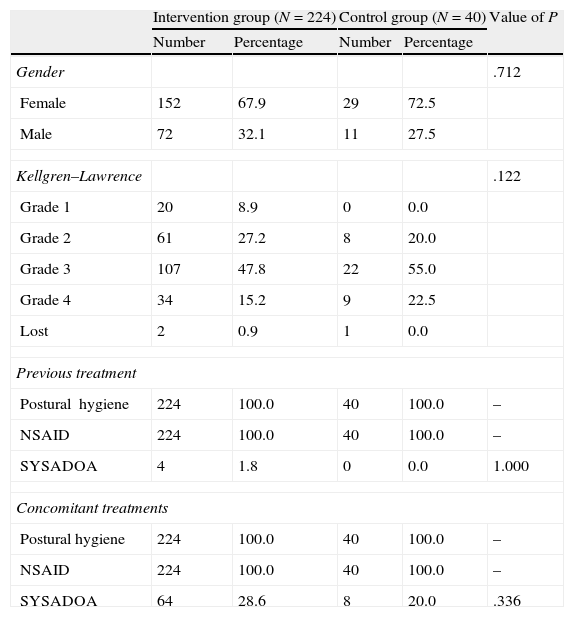
ResultsWe collected data from 224 patients treated consecutively at the CMAR consultation from April 5th, 2006 to April 29th, 2009. The characteristics of the sample and the 40 patients in the control group who were referred directly to surgery are shown in Table 2. Patients were mostly female (67.9% of the total) and with osteoarthritis of grade III in the Kellgren & Lawrence classification (47.8% of the total). The only statistically significant differences were found in age, which was higher in the control group. The characteristics of the sample were also comparable with the epidemiological data of the Spanish population diagnosed with KO.2 The mean follow-up period was 408 days, the mean number of VS administrations was 1.52 and the mean number of total consultations was 2.45.
Characteristics of patients in the sample attended in the knee osteoarthritis monographic consultation and in the control group.
| Intervention group (N=224) | Control group (N=40) | Value of P | |||
| Number | Percentage | Number | Percentage | ||
| Gender | .712 | ||||
| Female | 152 | 67.9 | 29 | 72.5 | |
| Male | 72 | 32.1 | 11 | 27.5 | |
| Kellgren–Lawrence | .122 | ||||
| Grade 1 | 20 | 8.9 | 0 | 0.0 | |
| Grade 2 | 61 | 27.2 | 8 | 20.0 | |
| Grade 3 | 107 | 47.8 | 22 | 55.0 | |
| Grade 4 | 34 | 15.2 | 9 | 22.5 | |
| Lost | 2 | 0.9 | 1 | 0.0 | |
| Previous treatment | |||||
| Postural hygiene | 224 | 100.0 | 40 | 100.0 | – |
| NSAID | 224 | 100.0 | 40 | 100.0 | – |
| SYSADOA | 4 | 1.8 | 0 | 0.0 | 1.000 |
| Concomitant treatments | |||||
| Postural hygiene | 224 | 100.0 | 40 | 100.0 | – |
| NSAID | 224 | 100.0 | 40 | 100.0 | – |
| SYSADOA | 64 | 28.6 | 8 | 20.0 | .336 |
| Mean | Standard deviation | Mean | Standard deviation | ||
| Age (years) | 65.72 | 10.22 | 68.87 | 7.04 | 0.027 |
NSAID: non-steroidal anti-inflammatory drugs; SYSADOA: Symptomatic Slow Acting Drugs in Osteo-Arthritis.
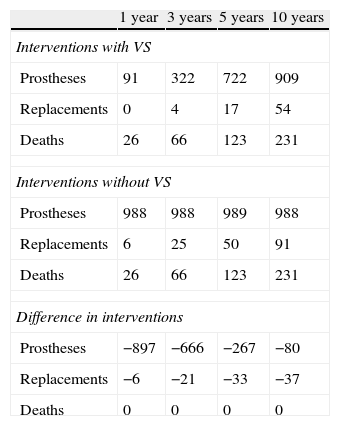
In the BIA characterised by incorporating a cohort of patients with KO each year, the number of arthroplasties decreased considerably in the initial years. With 1000 new patients entering the process each year, only 91 prostheses were operated during the first year, 322 during the second and third, 722 during the fourth and fifth and the figure became stabilised at 909 after the sixth year (Table 3). These results are shown in annual figures, both for the number of operations and the costs.
Analysis of the impact on healthcare of the introduction of VS with hyaluronic acid.
| 1 year | 3 years | 5 years | 10 years | |
| Interventions with VS | ||||
| Prostheses | 91 | 322 | 722 | 909 |
| Replacements | 0 | 4 | 17 | 54 |
| Deaths | 26 | 66 | 123 | 231 |
| Interventions without VS | ||||
| Prostheses | 988 | 988 | 989 | 988 |
| Replacements | 6 | 25 | 50 | 91 |
| Deaths | 26 | 66 | 123 | 231 |
| Difference in interventions | ||||
| Prostheses | −897 | −666 | −267 | −80 |
| Replacements | −6 | −21 | −33 | −37 |
| Deaths | 0 | 0 | 0 | 0 |
The results are the mean of 100 simulations incorporating a cohort of 1000 patients each year.
VS: viscosupplementation.
Patient monitoring showed that the use of viscosupplementation delayed the need for implantation of knee prostheses by a mean 2.67 years.
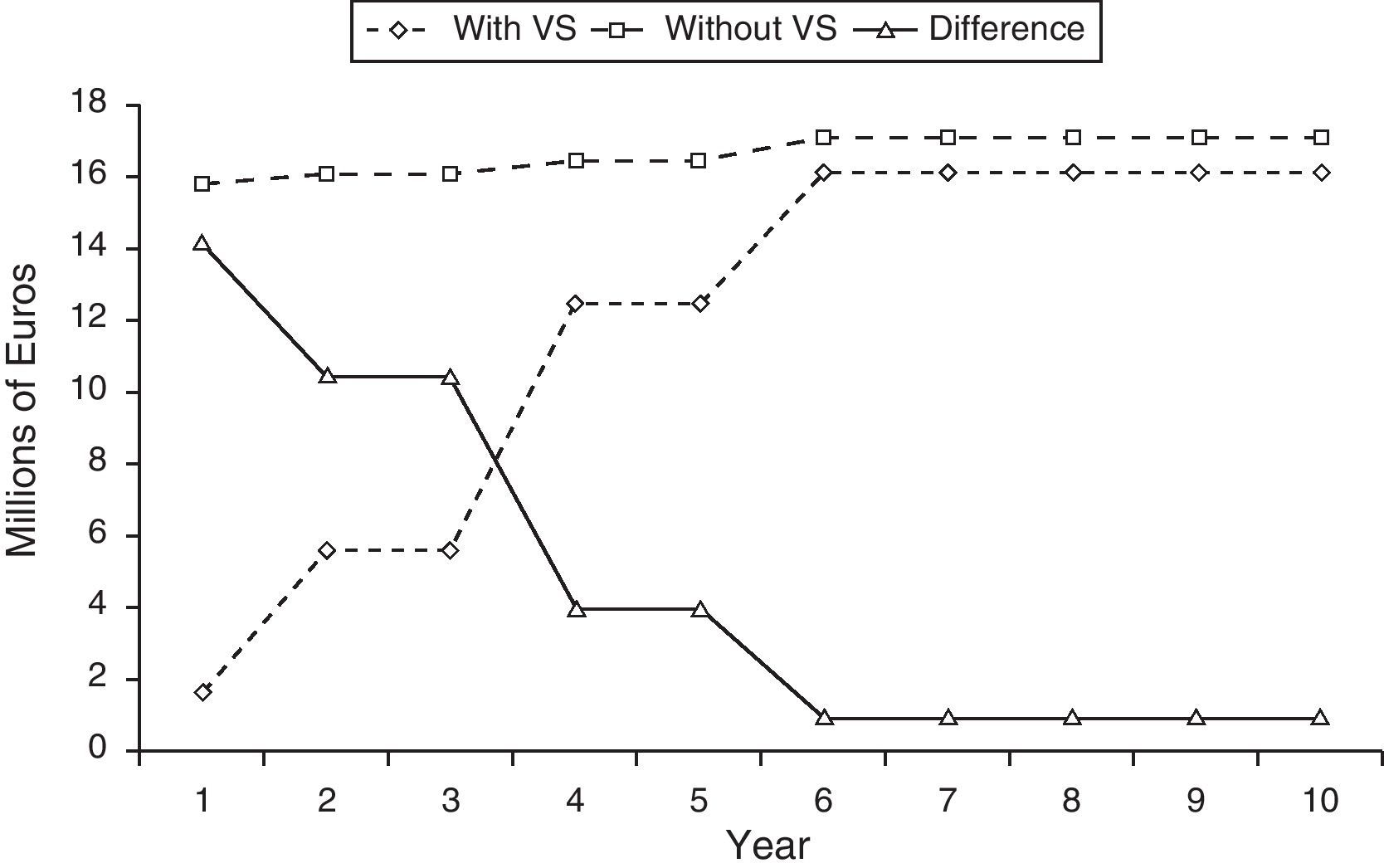
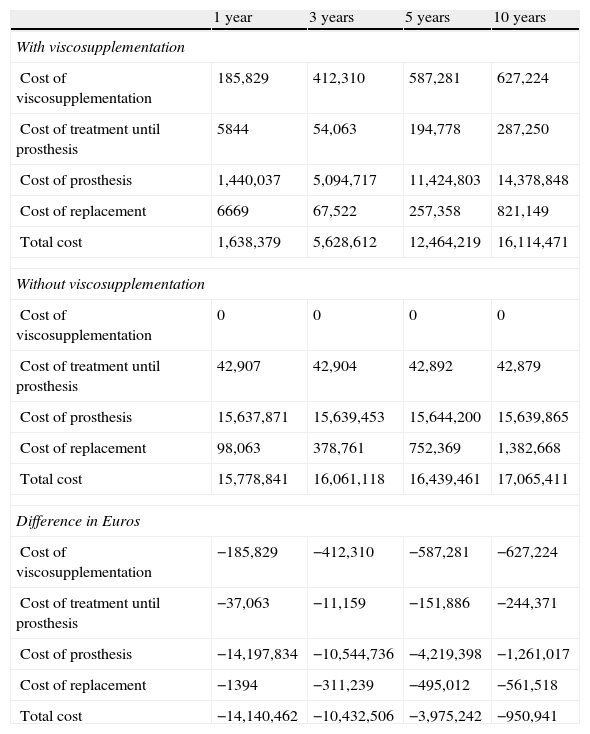
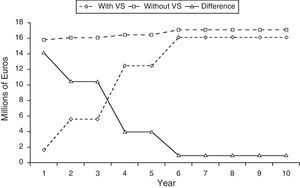
The BIA (Table 4) showed that the corresponding savings ranged from 14 million Euros in the first year to 1 million Euros in the sixth year. Between the second and fifth years, savings were between those figures in proportion to the number of surgical procedures avoided (Table 4 and Fig. 2). Thus, for a population generating an incidence of 1000 candidates for knee prostheses each year, we noted that the sum of the savings of the first 3 years amounted to 36 million Euros. These savings were still maintained once the process became stabilised, albeit to a lesser extent. Bearing in mind the reality of a hospital with 100 patients candidates for knee prostheses annually, this treatment would generate savings of 1.4 million Euros during the first year and an aggregate of 3.6 million Euros at 3 years.
Analysis of the impact on budget in Euros of the introduction of viscosupplementation with hyaluronic acid.
| 1 year | 3 years | 5 years | 10 years | |
| With viscosupplementation | ||||
| Cost of viscosupplementation | 185,829 | 412,310 | 587,281 | 627,224 |
| Cost of treatment until prosthesis | 5844 | 54,063 | 194,778 | 287,250 |
| Cost of prosthesis | 1,440,037 | 5,094,717 | 11,424,803 | 14,378,848 |
| Cost of replacement | 6669 | 67,522 | 257,358 | 821,149 |
| Total cost | 1,638,379 | 5,628,612 | 12,464,219 | 16,114,471 |
| Without viscosupplementation | ||||
| Cost of viscosupplementation | 0 | 0 | 0 | 0 |
| Cost of treatment until prosthesis | 42,907 | 42,904 | 42,892 | 42,879 |
| Cost of prosthesis | 15,637,871 | 15,639,453 | 15,644,200 | 15,639,865 |
| Cost of replacement | 98,063 | 378,761 | 752,369 | 1,382,668 |
| Total cost | 15,778,841 | 16,061,118 | 16,439,461 | 17,065,411 |
| Difference in Euros | ||||
| Cost of viscosupplementation | −185,829 | −412,310 | −587,281 | −627,224 |
| Cost of treatment until prosthesis | −37,063 | −11,159 | −151,886 | −244,371 |
| Cost of prosthesis | −14,197,834 | −10,544,736 | −4,219,398 | −1,261,017 |
| Cost of replacement | −1394 | −311,239 | −495,012 | −561,518 |
| Total cost | −14,140,462 | −10,432,506 | −3,975,242 | −950,941 |
The results are the mean of 100 simulations incorporating a cohort of 1000 patients each year.
The first conclusion of this study was that the use of VS represented a saving when taking into account the short, medium and long term consequences. The reason was that the cost of prostheses and reviews saved exceeded the cost of VS. In this sense, the simulation model served to elaborate a joint analysis over time of both the cost of the new treatment and its consequences in surgical interventions, and to make this analysis available to those responsible for making medical decisions. The BIA showed the result of a model which reproduced real events within an area of healthcare where a specific number of osteoarthritis patients were considered for surgery continuously each year. The considerable savings obtained in the initial years were due to the delay in the need for surgery. We should note that the economic balance was always positive, since although the number of prostheses implanted increased over time, the final number was 10% lower than the conventional alternative.
In order to understand the results, it is important to analyse the 2 competing risks for a patient undergoing prosthesis surgery. On one side is the risk of death and on the other is the risk of replacement. The latter only occurs when it is less than that of death. In the model, each individual is assigned both times according to certain mathematical functions that reproduce epidemiological reality through probabilistic mathematical methods. The probabilistic feature of the functions means that each individual is randomly assigned both times and it is only chance that determines which one takes place sooner. The use of sophisticated simulation methods such as DES allows rigorous documentation of the methods employed and is the key to validating the results.16
The BIA informed us about the behaviour of the balance between new costs incurred by VS treatment and savings generated through a reduced use of prosthetics and replacements.11 The result of the BIA was that the greatest savings occurred in the initial years, since this was the period when a greater number of prostheses were delayed through the benefit of VS treatment. The result in the long term was still positive, but less so, since the patients in the initial cohort were operated, although to a lesser extent as a result of competition with other sources of disease and death.
The reliability of the results of a simulation model depends on its robustness in terms of fidelity to the natural history of the disease being reproduced and the validity of the parameters entered into it. The structure of our model reproduced that of models used in other studies carried out by Markov models and was, therefore, well documented in the literature.9,21,22 We believe that the use of DES constituted a more natural representation of the risks associated with arthroplasty and, therefore, reinforced the validity of the model.16
The 2 key parameters of the model were the time until prosthesis with VS and the risk of review of the prosthesis. Regarding the former, we relied on parametric survival analysis of the patients studied. Regarding the latter, we used a function with an increasing risk of review. The annual rate of review remained between 1% and 1.5% in the first 10 years, increasing to levels between 1.5% and 2% in the second decade and between 2% and 3% in the third decade. The result was a prosthesis survival of 87.2% at 10 years, 71.5% at 20 years and 63.1% at 25 years. This was a key parameter in the final results, since an increasing survival led to a decreasing number of replacements because patients would die before requiring them and, therefore, VS would offer no benefit. In order to apply this function, we considered the work by Labek et al. studying the cumulative results of worldwide knee prosthesis records.23 The data covered approximately 10 years and the annual rate of review was 1.26%. We applied an increasing risk, following the cited article by Briggs et al. and the existing literature on the particular disease associated with the materials used.20–22 Follow-up periods of 20 years giving figures of 76% prosthesis survival have been published for hip prostheses.31 Thus, we believe that the model was properly validated. One limitation of our model was that we projected a risk of replacement greater than the follow-up time published by prosthesis records.23 However, limiting the time horizon to 10 years cancelled its impact on the results.
In conclusion, we can say that our results demonstrate that the use of a treatment such as VS, aimed at improving quality of life for patients and postponing the implantation of knee prostheses, is economically viable and reduces the economic burden of KO for the health system.
Two limitations of the study were that its design was not that of a clinical trial, but rather a naturalistic study with a non-randomised control group, and that we did not use a quality of life questionnaire, such as the WOMAC or the SF-36, to indicate surgery. Given that the cost savings achieved by the use of VS were due to delaying total prosthesis implantation, it could be argued that the study itself functioned as a mechanism of administrative delay. In this case, the intervention criterion was established by the physician depending on radiographic severity and the symptoms of each patient. In the analysis of the 2 groups we did not find any differences regarding radiological classification or any other characteristic, except for age. Regarding the use of a quality of life questionnaire, since this was a naturalistic study we followed the same procedure as in routine clinical practice, which does not include a systematic measurement of quality of life.17,31 We believe that the delay of 3.13 years would never have been possible without a real effect of VS, although it is possibly true that a small portion of that time period could be explained by the mere fact of indicating a treatment prior to surgery and waiting to observe its effect. Using a naturalistic design involved reproducing the usual process of consultation and increased the external validity of the results obtained.32
Level of evidenceLevel of evidence II.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have received a fee from Zambon Spain for their participation in this study.
Please cite this article as: Mar J, et al. Análisis de costes del tratamiento con viscosuplementación con ácido hialurónico estabilizado en pacientes con artrosis de rodilla candidatos a implantación de prótesis. Rev Esp Cir Ortop Traumatol. 2013;57:6–14.