The treatment of calcaneal fractures with joint involvement continues to be a challenge for the traumatologist. The inconsistent clinical results and frequent complications of open reduction have made it difficult to standardize surgical management of these injuries. The new percutaneous construction techniques appear to have a future due to a lower complication rate and better technical accessibility.
El tratamiento de las fracturas de calcáneo con afectación articular sigue constituyendo un reto para el traumatólogo. Los inconsistentes resultados clínicos y frecuentes complicaciones de la reducción abierta han dificultado la generalización del manejo quirúrgico de estas lesiones. Las nuevas técnicas de reconstrucción percutánea parecen ser el futuro gracias a la menor tasa de complicaciones y mayor accesibilidad técnica.
The latest advances in orthopaedics and in surgical techniques have led to a consensus as to the best treatment for calcaneal fractures, which have always been the subject of controversy.
Even today, however, when faced with evaluating, classifying, and treating a calcaneal fracture, expert orthopaedic surgeons are still in doubt because, for any given injury, there may be several, widely differing criteria and solutions. Both short- and long-term complications are common with these fractures and with their treatment, posing a major challenge for the traumatologist.
Most calcaneal fractures—between 70% and 90%—involve the subtalar joint and result from high-energy trauma. The typical patient is a working-age male who has been the victim of a work accident. Consequently, this is an injury that has major socio-economic repercussions, and it is well worth the effort to ensure the fastest and most complete functional recovery possible for our patients.
Anatomy and biomechanics of calcaneal fracturesMost intra-articular fractures result from direct, high-energy trauma, with the vector of force moving vertically from plantar and crushing the calcaneus against the talus—a much denser bone that acts as a wedge or battering ram on the subtalar joint. The calcaneus shatters, with its articular facet collapsing, the greater tuberosity rising, and its walls widening—especially the lateral because it is the weakest wall.
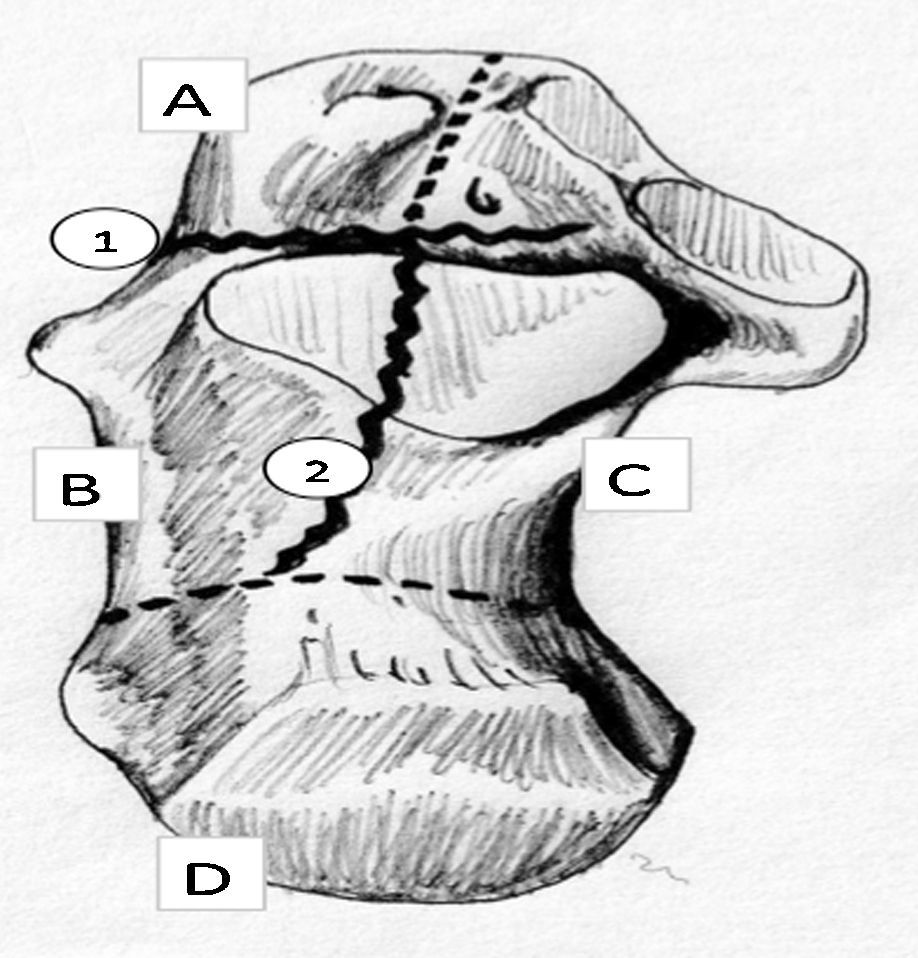
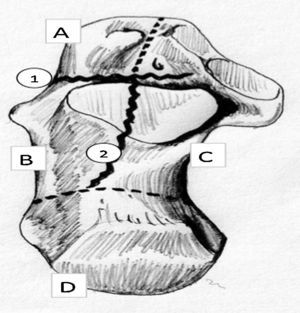
These displacements can be discovered by measuring the Böhler angle on the lateral x-ray, and several characteristic fracture fragments may be identified on CAT scan: (1) anterolateral fragment, which includes the lateral cortex and anterior process; (2) superomedial or sustentacular fragment, which includes the medial cortex, the sustentaculum tali, and a variable portion of the posterior subtalar facet; (3) superolateral fragment or fragments, which include the collapsed or displaced articular facet and its lateral cortical portion; and (4) posterior fragment, which includes the greater tuberosity of the calcaneus (Fig. 1).
The first 2 fragments are the most stable while the last are the most unstable and displaced. These concepts are important in terms of proposing a reduction and fixation of the fracture—whether open or closed.
In our experience, the integrity of the inferior cortex of the calcaneus is a major anatomical influence on the surgical management of these fractures. In cases where it remains intact after the fracture, bone length is preserved, and all we have to do is restore the height and width. When the inferior cortex is ruptured, there will be further displacements and the calcaneus will be shortened, which complicates the reduction because this shortening means more severe varus or valgus deformities.
There are 2 important aspects of calcaneal biomechanics that may be altered with fractures. First, this bone acts as tensor for the Achilles-calcaneus-plantar system. In fractures that heal with a loss of bone length and an elevation of the greater tuberosity, this very important system will lose power, leading to atrophy of the triceps surae and gait changes.
Radiographic assessmentCalcaneal fracture is usually diagnosed on x-rays taken of the entire traumatized foot in the routine antero-posterior, lateral, and oblique views. An axial view of the heel completes the radiographic assessment.1
On the lateral x-ray—the most useful view—we should evaluate the following points: joint involvement; displacement and collapse of the fracture fragments; Böhler angle; angle of Gissane; number of fragments; comminution; and relationship with neighbouring bones.
On the axial x-ray, we will see varus or valgus displacement of the greater tuberosity; axial fracture lines; and the state of the external cortex and peroneal canal.
The radiographic assessment may be completed with oblique views, such as Broden's projection; these days, however, a CAT scan is absolutely necessary to characterize and classify calcaneal fractures as well as to determine a therapeutic approach.
These studies should include plantar and coronal slices. Fascinating, three-dimensional reconstructions for surgical planning can be obtained with a helical CAT scan.
Magnetic resonance imaging has not proven to be useful in evaluating calcaneal fractures.
ClassificationThe Sanders classification2 is currently the most popular; it is based on frontal plane CAT scan images, looking for the one with the greatest joint displacement. It has shown only moderate interobserver reliability.3–7 It divides the calcaneal body into 4 columns with lines correlating to the most common fracture lines. Because this classification does not take the other CAT scan slices into consideration, it may fail to detect other fracture lines. It also does not take into consideration the degree of fracture displacement, complexity of the fracture line, osteochondral collapse, the entrapment of canaliculi, or the status of soft tissues affected by the trauma energy. Thus, we may find fractures that can be classified as grade II and yet are high-energy injuries with significant displacement as well as cartilage and soft tissue involvement.
In any case, and as Fitzgibbons et al. point out,8 any given fracture should always be assessed with both simple x-rays and CAT scan because these are complementary diagnostic tools and never mutually exclusive.
Approaches to treatmentWith calcaneal fractures, decisions will depend on various factors besides the type of fracture. The patient's age, where the accident occurred, intercurrent diseases, and whether there are associated injuries or multiple traumas are important aspects to be taken into account, for they will have a major influence on the outcome.
Type of fracture: in current protocols, conservative treatment is reserved exclusively for non-displaced or Sanders I fractures. For type II and type III displaced fractures, the treatment indicated is open reduction and internal fixation; primary arthrodesis is indicated for type IV fractures.
Patient's age: surgical treatment is not contraindicated in the elderly, although osteoporosis does complicate it. Plate fixation is less effective, and less invasive procedures are recommended.
Where the accident occurred: calcaneal fractures may result from any accident, but they are much more common in the work environment. In these cases, the existence of financial compensation influences the outcome. Thornes et al.9 showed that, in working patients, this factor made no difference between functional and surgical treatments in terms of outcome.
The presence of associated injuries or multiple trauma is another key factor to bear in mind. Aktuglu and Aydogan10 pointed out that the course of a calcaneal fracture is worse in multiple trauma patients than in cases of isolated fracture. On many occasions, this fracture is disregarded and treated later as a sequela.
Intercurrent diseases: diabetes, vascular insufficiency, smoking, and other pathologies dramatically increase the incidence of complications with open surgical treatment. In many of these cases, minimally invasive surgery or even conservative treatment is preferable.
Surgeon's experience: this is an important factor to keep in mind. As Sanders himself has pointed out,2 a poor reconstruction of the calcaneus is even worse than doing nothing. An extended approach involving open reduction and internal fixation, which we will describe below, is a complex surgical procedure that has a great number of possible complications, some of which are quite serious; therefore, it is best left to expert surgical teams to whom these injuries should be referred. In the event that it is not possible to refer the patient, the recommendation is to opt for minimally invasive procedures that, when correctly performed, achieve clinical results close to those of open surgery done by experts.11
Conservative treatmentIt seems clear that surgical treatment of serious calcaneal fractures, when properly indicated and performed, offers significant advantages for patients over functional treatment.2,12–16 However, up to half of the traumatologists in Spain opt not to do surgery and resign themselves to the sequelae of displaced intra-articular fractures.17 This same study shows that, in the medium to long term, almost 60% of these patients will require surgery to treat these sequelae, which usually involves a secondary subtalar arthrodesis, with or without deformity correction. Another study done in Holland18 shows that a high percentage of traumatologists (39%) in that country still prefer conservative treatment.
The reasons for this trend are not given, but analysing the daily patient care situation may reveal several of them. On the one hand, in multiple trauma patients where other systemic and musculoskeletal injuries have priority, a serious calcaneal fracture is often disregarded.19 In cases where it is an isolated injury, the team's lack of training in complicated surgical reconstruction of the calcaneus tips the balance toward a conservative approach, which is supported by the inherent morbidity burden and the inconsistency of clinical results with these procedures—open osteosynthesis, in particular.
Numerous authors20 have published good results with traditional, non-surgical treatment. This consists of an initial phase of rest with elevation of the foot and application of ice, non-steroidal anti-inflammatories, and antithrombotic prophylaxis. When the inflammation is better, very early rehabilitation is started to improve mobility and reduce oedema, with the support of proper nutrition. The non-weight-bearing phase depends on the fracture and varies from 6 to 8 weeks. Immobilizations are not used these days, for there is scientific evidence that the results are worse. Insoles are usually required for better distribution of the load. The advantages of this minimalist treatment are a low incidence of complications and the fact that any orthopaedic surgeon can manage it. Joint incongruence and deformities are accepted, and normally they are better tolerated than one might expect.
Closed reduction and plaster immobilizationBöhler21 developed a system of compression and closed manipulation for calcaneal fractures, aimed at minimizing deformities. Other authors like Omoto22 have published modifications of the closed reduction method. Problems with this method are the risk of cutaneous necrosis, acute compartment syndrome, and recurrence of the deformity; for these reasons, it has seen a great decline in popularity. These days, it is only in cases of gross deformity with marked lateral compromise that conservatives would definitely recommend it.
Closed reduction and percutaneous fixationWhile the first percutaneous surgical procedure for calcaneal fractures was described by Westhues, it was Essex-Lopresti who defined the indications for this method. It is currently used by many surgeons23 and is the procedure most recommended for those with little experience in open reduction. Kirschner wires, Steinman pins, external fixators, and cannulated screws may be used to reduce fracture fragments and fix them temporarily while healing takes place. The philosophy behind this method is that intervention on the fragments be done percutaneously to restore the length and height of the greater tuberosity and to reduce the subtalar joint; for this reason, it is especially indicated for tongue-type fractures (Sanders type IIC) where quite satisfactory reductions may be achieved.The first step in the technique is to force the heel into varus to free up the fragments. The wire(s) is/are inserted through the heel to the talus, which is then immediately pried toward plantar while the forefoot is put into equinus. After the reduction is confirmed on x-ray, the wires are advanced with the foot in valgus and fixed to the talus (Westhues) or to the anterior tuberosity of the calcaneus (Essex-Lopresti). It is immobilized for 4 weeks with a plaster cast; the wires are removed in 6 or 8 weeks; and weight-bearing is permitted at 10 weeks. Wee and Wong24 have recently demonstrated a way to shorten the non-weight-bearing period and to ensure the result by injecting tricalcium phosphate cement after the reduction and percutaneous fixation. The morbidity associated with the extended approach for open reduction and internal plate fixation in articular calcaneal fractures has fostered numerous attempts to treat these lesions through minimally invasive surgery and percutaneous fixation, with results as good as open reduction.25–28
Because these procedures are neither well defined nor standardized, however, every author advocates a different method. The use of wires, pins, cannulated screws, and external fixators has been so highly variable that it is difficult to accept any of these as standard procedure.
Some authors have suggested that external fixators be used for comminuted fractures.29 These external fixation systems would enable alignment of the fractured calcaneus to be maintained until healing takes place. There is a minimally invasive reduction and synthesis of the articular surface. Results with this technique have been inconsistent, but it may be an option in the most serious open fractures.
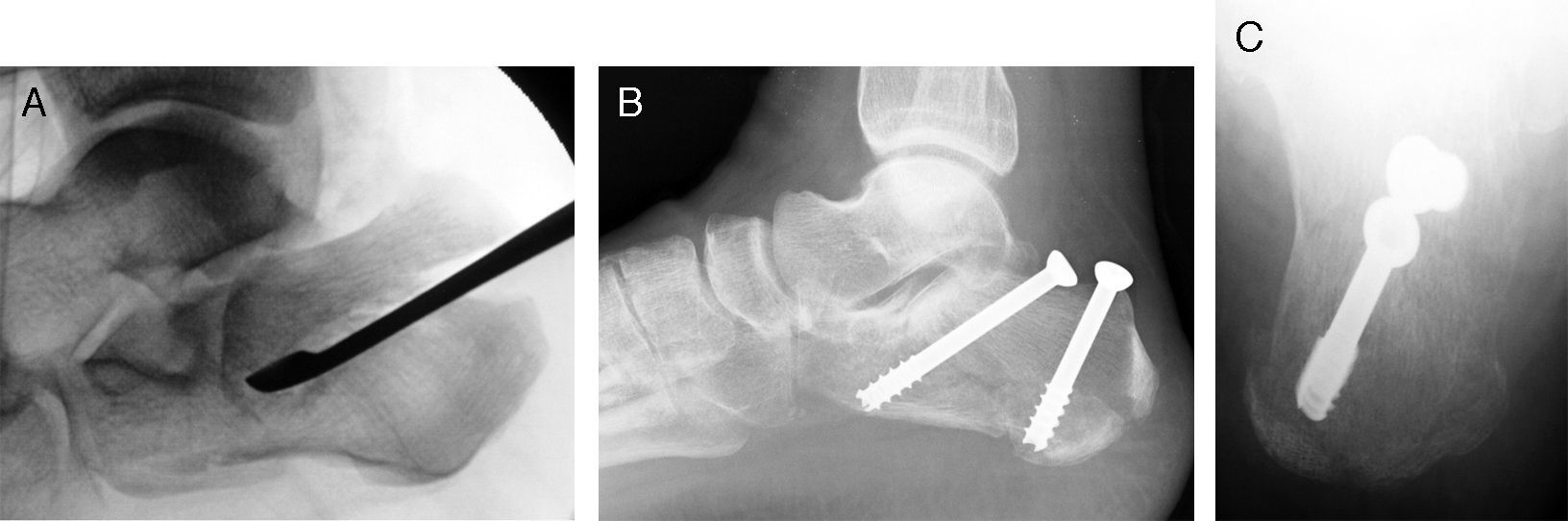
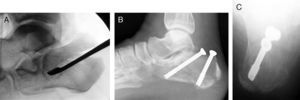
In our experience, osteosynthesis with cannulated screws is preferable because it circumvents the problems usually associated with the use of percutaneous wires, such as loosening, infection, and skin problems. We routinely use a small, 5-mm, lateral incision under the peroneals, through which we insert a forceps, wedge, or fine periostotome to reach the tongue-type fragment. By applying pressure in a proximal direction and flexing the ankle, a good reduction of the subtalar joint is easily achieved. The assistant is prepared to fix the reduction achieved with 2 Kirschner wires, over which we will place the 5-mm or even 6.5-mm cannulated screws. The first screw is inserted in an anterolateral direction from the internal aspect of the Achilles tendon and runs under the subtalar joint to the anterior process of the calcaneus. It supports the anterolateral and anteromedial fragments, thereby keeping the tongue-type fragment from collapsing. The second screw is placed in a posteromedial direction from the external aspect of the Achilles in an attempt to stabilize the superolateral tongue-type fragment with the posterior fragment. Post-operative immobilization generally is not required, and progressive weight-bearing is permitted from the fourth week (Fig. 2).
Tongue-type fracture treated with closed reduction and percutaneous fixation. (A) Percutaneous reduction through a very small lateral incision for using a wedge to raise the tongue-type fragment. (B) Follow-up lateral x-ray showing the reduction achieved and fixation with 2 6.5-mm cannulated screws in anterolateral and posteromedial orientation. (C) Axial view of the same case.
There is consensus in the literature regarding the indications for surgical treatment. As with any other displaced, intra-articular fracture, reconstruction with stable osteosynthesis is the most desirable of the surgical solutions. A majority of authors recommend it for Sanders grade II and III fractures, reserving reconstruction and primary arthrodesis for grade IV fractures.
Modern surgical treatment of fractures aims to meet the following objectives: reduction of the bone fragments, joint congruency, and a stable fixation that permits early mobility. In calcaneal fractures, the principles of osteosynthesis are perfectly applicable; historically, however, the results have been controversial.30
These poor results are due to the extreme technical difficulty, the post-operative morbidity, and the long-term outcome, which is not so different from that of functional treatment. It has been shown that an imperfect osteosynthesis is far worse than functional treatment,31 for added to the low efficacy is a higher incidence of complications. Transient or permanent damage to the sural nerve following open surgery is seen in 50% of cases, even in expert hands.32 The incidence of post-operative infection is quite high at 3%–5%.33
It has been shown32 that open surgery should never be performed during the acute phase of the fracture because this increases the incidence of complications. It is better to wait 7–10 days until the oedema has diminished.
The objectives of surgical treatment: (1) restore joint congruency; (2) restore heel height (Böhler angle); (3) reduce the width of the calcaneus; (4) decompress the medial and lateral canals; and (5) achieve good axial alignment.
This may be accomplished through 3 different surgical approaches: lateral, internal, or combined.
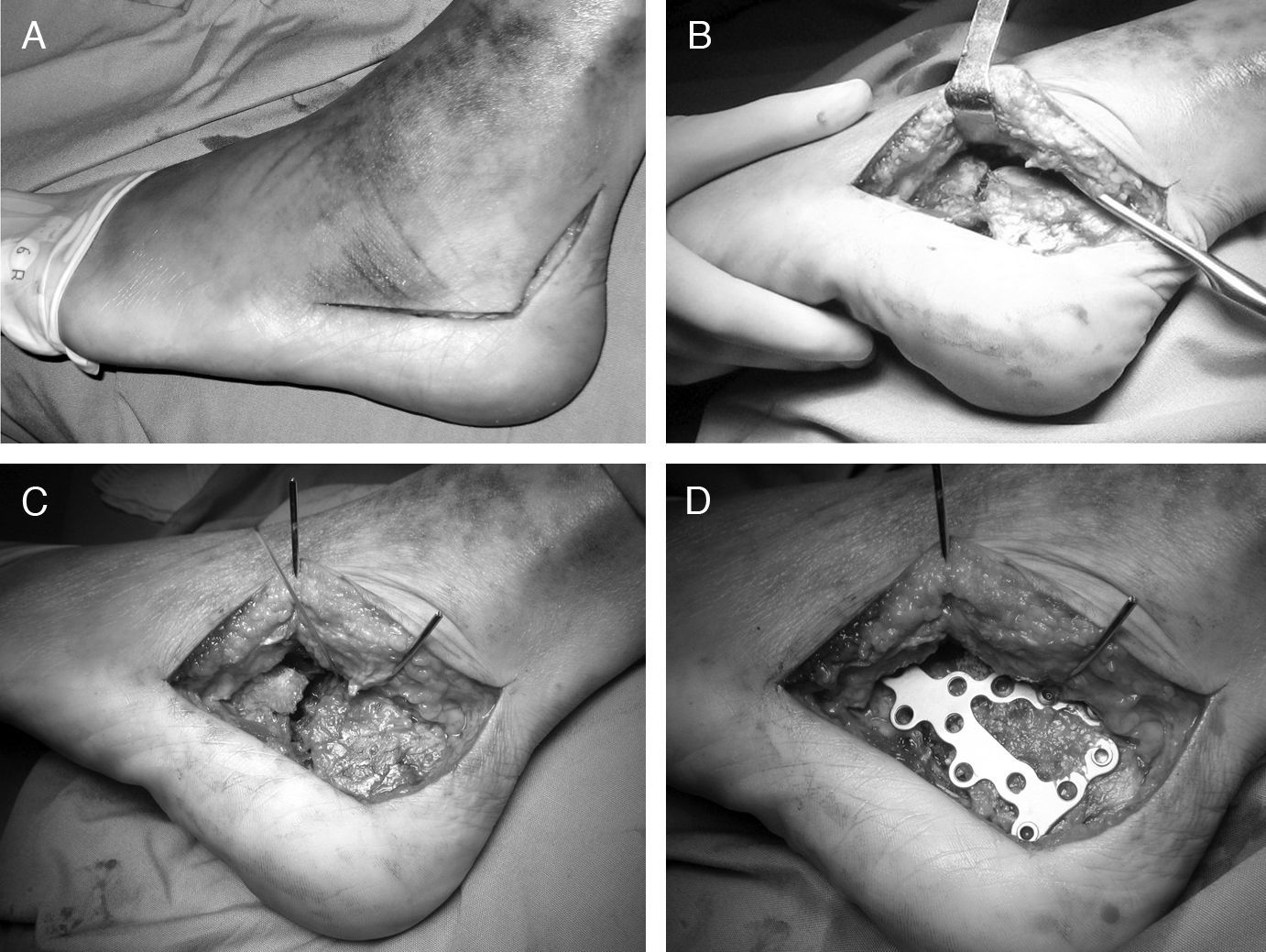
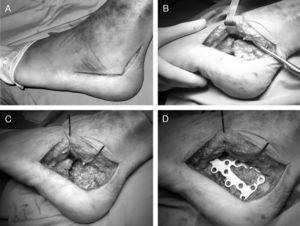
Lateral approachThe lateral approach most recommended is the Sangeorzan and Benirschke extended approach.16 This is done through an L-shaped skin incision, which permits visualization and reduction of the subtalar and calcaneal-cuboid joints and the greater tuberosity (Fig. 3).
Open reduction and internal fixation with an angular-stable screw-plate system in intra-articular calcaneal fractures. (A) Skin incision. (B) Creation of the fasciocutaneous flap, which includes periosteum and peroneal tendons in their sheath. (C) Exposure of the fracture through the lateral wall of the calcaneus. (D) Fixation with specially designed plate.
The position of the foot during the surgical procedure is very important to prevent reconstructions in varus, which are subsequently quite incapacitating. The foot is always placed in lateral decubitus position with a soft support under the heel to correct its natural tendency toward varus.
The key to preventing a high incidence of wound problems is to start the incision just lateral to the Achilles tendon and include the sural nerve and the peroneal sheath in the flap.1 The incision should go all the way down to the bone, thereby preventing dissection of the flap, and a scalpel is used to lift it directly off the periosteum. The flap should be handled with extreme care, and this is why it is preferable to separate it with Kirschner wires inserted into the malleolus, talus, and anterior tuberosity and folded back on themselves. It must be carefully sutured, and the stitches must remain in place for a minimum of 3 weeks.
Once the fracture is exposed, we should be very analytical about it. A thorough assessment of the x-rays and CAT scan will enable us to plan the surgery in advance. In simple fractures, with very little rise or shortening of the greater tuberosity and moderate collapse of the talus, it will be relatively easy to restore the condition of the subtalar joint and then support the fragments with a plate. In addition to the plate, temporary wires and loose screws often have to be used.
Plates specially designed for the calcaneus, like the Sanders or other similar plates, are highly recommended for their versatility. These plates have evolved toward implants, with angular stability screws, extremely low profiles, and different sizes and shapes.
Once the external wall of the calcaneus is exposed, we can pull it down or even remove it from the field to access the primary fracture lines. Using a periostotome or wedge, we disimpact the posterior fragment to restore the length and height of the calcaneus by reconstructing the Böhler angle. A Steinman pin in the greater tuberosity enables us to exert more force for the reduction.
Then we will reconstruct the posterior subtalar joint surface. We may find a great variety of fracture patterns in this area. We will disimpact the collapsed fragments and try to achieve a good reduction of the joint. On occasion, it is necessary to use an osteotome to pry the fragments free and move them to their area. Thus, we create a bony defect that we will subsequently fill with a substitute or bone graft. The joint now reduced is held with temporary Kirschner wires, and the larger fragments are reduced. In fractures where the inferior cortex is ruptured and the tuberosity has risen greatly, this can be a costly manoeuvre. After the reduction and its temporary maintenance with wires, we put the lateral cortex of the bone in its place and, over it, the specially designed calcaneal plate. It may be appropriate to fix the joint beforehand with a 3.5-mm screw in subchondral position oriented from lateral to the sustentaculum tali. It is difficult to synthesize the sustentaculum using an angular-stable screw-plate system, so we should use screws independent of the plate.
Once the plate has been modelled for adaptation to the calcaneus, we can keep it in position with wires, and we begin by placing the talar screws, then the anterior tuberosity screws, and finally the posterior tuberosity screws. An intra-operative Broden's projection will tell us whether the subtalar joint reduction is satisfactory. Rammelt et al.34 have suggested using the arthroscope during open reduction to confirm joint congruency.
Our personal preference is a screw-plate system without angular stability, for it has a much lower profile, is more versatile, and enables the screws to be oriented at one's discretion; in addition, it corrects bone widening by applying compression against the plate as the screws are tightened.
Insertion of a bone graft or substitute is usually required in fractures with extensive collapse, although Longino et al.35 found no evidence that bone substitutes improve either clinical or radiographic evolution.
More complex fractures are a real challenge to any surgeon, and perfect reconstruction quite often proves to be impossible. One should bear in mind that, with lengthier and more complex surgery, the risk of complications and a poor outcome increases exponentially.36
Therefore, to avoid problems, it is essential that the fracture characteristics and the surgical team's technical capabilities be properly evaluated.
The internal approach was introduced by McReynolds37 and is not used very much because of its poor access to the subtalar and the presence of the neurovascular bundle. It is indicated for fractures of the sustentaculum tali and little involvement of the lateral wall.
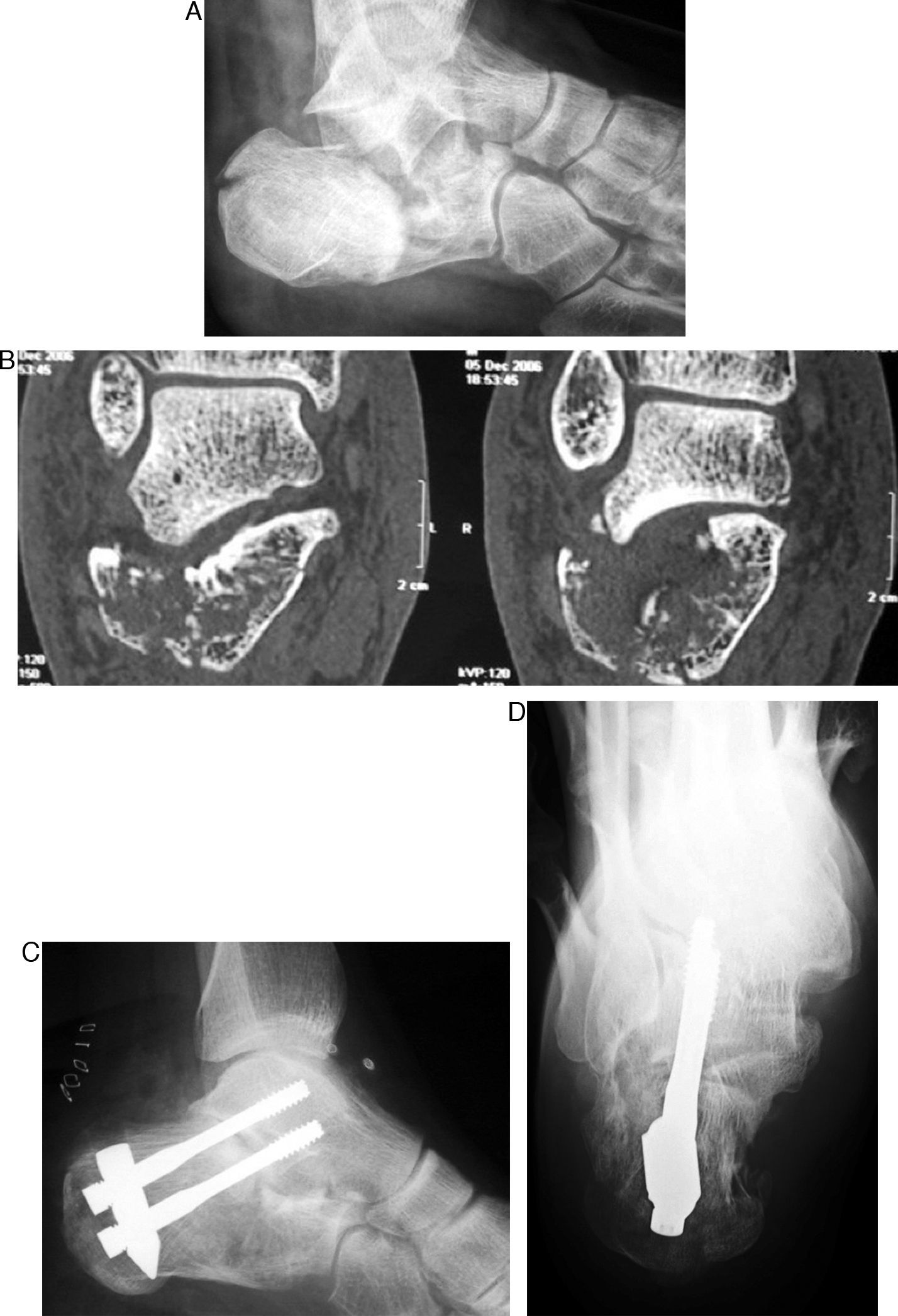
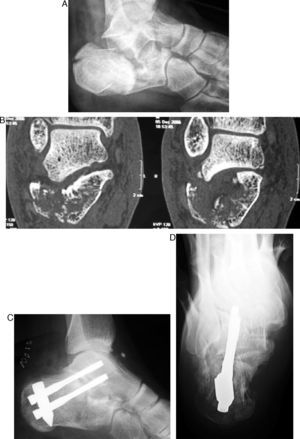
Reconstruction and primary subtalar arthrodesisQuite often, the fracture is so comminuted that surgical reconstruction is impossible or the patient presents with local or general problems that significantly increase the risk. In these cases, we could adopt a conservative approach and treat the sequelae later, or we could attempt to pre-empt them by reconstructing the calcaneal shape and performing a primary arthrodesis on the subtalar joint. This procedure has been shown to be effective in minimizing long-term complications and shortening convalescence38; it has been endorsed by numerous authors over a long period of time, since Stulz et al.,39 and should be standardized in routine treatment protocols.40Primary arthrodesis may be performed, per tradition, via either a conventional lateral approach or percutaneously by inserting a graft through a very small incision. It is recommended that stable osteosynthesis be enhanced using 6.5-mm cancellous screws inserted via the heel through the joint and anchored in the talar body. We recommend 2 screws that are crossed, as opposed to parallel, to prevent collapse of the greater tuberosity (Fig. 4). As an option for surgical treatment of calcaneal fractures, primary arthrodesis has gotten a major boost recently with the development of the Vira system.41–45
This system enables the shape of the fractured bone to be reconstructed—restoring functionality to the calcaneus-Achilles-plantar system—and simultaneously fixes it to the talar body to achieve arthrodesis of the subtalar joint.
In concept, it is minimally invasive surgery that, in a majority of fractures, does not require harvesting a graft because bone obtained from reaming for the implant placement is used for the arthrodesis.
The system consists of an implant and a guide, and the implant consists of 3 pieces: a nail that is inserted into the greater tuberosity, which usually retains good residual structure in these fractures, and 2 double-threaded, cannulated screws that support the nail with the talar body where they are inserted by passing through the posterior subtalar joint.
The Vira guide enables the length and height of the calcaneus to be recovered, which normalizes the Böhler angle and permits secure placement of the implant.
The Vira system is technically simple and safe, especially in more serious fractures, regardless of the surgeon's ability or experience. It is also indicated in treatment of the sequelae of calcaneal fractures, such as subtalar osteoarthritis or malunion.
The Vira implant is designed to withstand the tremendous load borne by the heel with normal gait, so in all cases—even bilateral cases—ambulation may be permitted 2 weeks after surgery, as tolerated by the patient. This shortens the rehabilitation process considerably.
Open fracturesOpen calcaneal fractures must be treated with extreme caution because of the high incidence of complications, which may even lead to amputation of the limb.
We recommend following the Thornton et al. algorithm46 in evaluating and making decisions about these injuries. The risk of complications depends on the size and position of the trauma wound. Wounds of the outer aspect are rare and frequently involve complications. Wounds of less than 4cm on the inner aspect may be treated by open reduction and internal fixation, if the wound can be closed and stabilized using antibiotic therapy. Wounds of more than 4cm or wounds that are unstable should not be treated with open reduction and internal fixation, but they may be reduced and kept in alignment using percutaneous wires.
ComplicationsAn important area of research in calcaneal fractures is the complications that may appear not only in the acute phase, hampering treatment and prolonging convalescence, but also long-term, casting a shadow over the prognosis for these injuries. Describing these complications and defining their proper management is beyond the scope of this article, but we can highlight some of the major concepts.
Almost all the complications described result from intra-articular fractures, most commonly when they present as high-energy injuries and with comminution.47 Most late complications are due to a malunion of intra-articular fractures. The following are the typical clinical sequelae in patients who suffer this injury: atrophy of the triceps surae; widening of and loss of height in the heel; bony prominences; and limited mobility of the subtalar joint.
This circumstance is usually well tolerated by the majority of patients, who manage it through adaptation of their footwear and varying degrees of permanent sports-work limitation, depending on the case. A pseudarthrosis would be unusual.
The most common complication of calcaneal fractures is symptomatic subtalar osteoarthritis, which frequently requires late surgical intervention for arthrodesis. Ball et al.48 have recently shown that there is a significant decline in the viability of articular cartilage following calcaneal fractures, which may be the cause of its post-traumatic degeneration in the medium and long term.
According to Allmacher et al.,49 the very long term outcome of treatment in calcaneal fractures basically hinges on the degree of osteoarthritis in the subtalar joint. When there is no significant axial deformity, arthrodesis in situ is the most widely accepted treatment, although the results with prostheses developed for this joint have not yet been confirmed because they are young patients in whom joint replacement does not work in the long term. In cases where there is marked collapse, the recommendation is to perform a secondary subtalar distraction bone block arthrodesis, preferably via a posterior approach,50 to partially restore the Böhler angle. When the patient has a deformity, the subtalar arthrodesis must be combined with a corrective osteotomy of the calcaneus.
Without question, however, the most-feared complication of calcaneal fractures—post-operative or not—is chronic infectious osteitis.51 The therapeutic approach is the one routinely used in bone infections—curettage, laying open, and covering52—but the results may not be good and the infection may be prolonged indefinitely. Some authors have even advocated total calcanectomy as definitive treatment for this problem and have published acceptable results.53
ConclusionsRecent advances in the management of intra-articular calcaneal fractures have expanded the therapeutic arsenal, putting solutions for these fractures within reach of traumatologists who have limited experience and reducing the risk of complications. As in other situations, minimally invasive approaches are the future in surgical treatment of trauma to the foot.
Evidence levelEvidence Level II.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of DataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestDr. F. López-Oliva maintains a patent release agreement with the Biomet company, manufacturer of the Vira system, and Dr. F. Forriol has no conflicts of interest to declare.
Please cite this article as: López-Oliva Muñoz F, Forriol F. Manejo actual de las fracturas intraarticulares del calcáneo. Rev esp cir ortop traumatol. 2011;55(6):476–484.