The purpose of this study was to assess the need of bone graft or bone substitutes in unstable distal radius fractures (DRF) treated with locking compression plates (LCP).
Patients and methodsAn observational and prospective study was conducted on 60 patients with DRF AO-type A3 and AO-type C3, treated surgically by LCP plates without bone grafts or substitutes. Ranges of motion in flexion (F), extension (E), pronation (P), and supination (S) were measured in the injured wrist and compared with the healthy contralateral wrist. X-ray parameters: palmar tilt (PT), radial inclination (RI), ulnar variance (UV), and radial height (RH) were calculated in the injured wrist one year after surgery and then compared, with those parameters in the healthy contralateral wrist and in the follow-up postoperative X-ray of the injured wrist. PRWE and DASH scores were used to evaluate patient satisfaction.
ResultsThe range of motion loss was F 12°±16.1°, E 9°±13.1°, P 2.5°±7.5°, and S 5°±10°, but they remained within functional parameters. Good results were also obtained in the PRWE and DASH scores (DASH 12.6±14.16 and PRWE 9.5±9.5). All the fractures were healed without significant collapse (IP 0.55±1.7°, IR 0.31±1.5°, VC 0.25±0.8mm, and AR 0.1±0.9mm).
ConclusionsAll fractures healed without problems or with significant loss of reduction. Bone graft and bone substitutes are not mandatory for treatment of unstable DRF with LCP plates. Their use increases the cost and is not exempt of morbidities. This study also reinforces the role of LCP plates in surgical treatment of unstable DRF.
Evaluar la necesidad de injertos o sustitutivos óseos en el tratamiento quirúrgico de las fracturas de radio distal (FDR) con placas bloqueadas (LCP).
Material y métodosEstudio prospectivo observacional de 60 pacientes con FDR A3 o C3 tratadas mediante placa LCP sin aporte de injerto o sustitutivo óseo. Se comparó la movilidad en flexión (F), extensión (E), supinación (S) y pronación (P) de la muñeca fracturada con respecto a la sana; y los parámetros radiográficos de inclinación palmar (IP), inclinación radial (IR), varianza cubital (VC) y altura radial (AR) de la muñeca fracturada al año de la cirugía respecto a la muñeca contralateral sana y a la fracturada en el postoperatorio. Evaluamos el grado de satisfacción del paciente mediante las escalas PRWE y DASH.
ResultadosLas diferencias de movilidad de la muñeca fracturada con respecto a la muñeca contralateral sana fueron F 12°±16,1°, E 9°±13,1°, P 2,5°±7,5° y S 5°±10°, pero se mantuvieron dentro de rangos funcionales y obtuvimos un buen nivel de satisfacción de los pacientes (DASH 12,6±14,16 y PRWE 6,31±9,5). El 100% de FDR consolidaron sin colapso significativo (IP 0,55±1,7°, IR 0,31±1,5°, VC 0,25±0,8mm, AR 0,1±0,9mm).
ConclusionesTodas las fracturas consolidaron sin problemas y la pérdida de reducción no fue estadísticamente significativa. El uso de injertos o sustitutivos óseos no es imprescindible en el tratamiento de las FDR inestables con placas LCP, cuya utilización encarece el procedimiento y no está exenta de morbilidades. Como conclusión secundaria, el estudio afianza el papel de las placas LCP en el tratamiento de las FDR.
Distal radius fractures (DRF) are one of the most frequent pathologies in emergency services and can account for up to 18% of all fractures. They have a bimodal distribution, appearing in young patients due to high-energy trauma or, more frequently, in elderly patients with osteoporotic bones due to low-energy trauma.1
A significant percentage of these lesions, over 40%, are considered unstable, so orthopedic treatment can be insufficient or unsatisfactory in many cases.2
Numerous therapeutic options for its management have been described in the literature, but there is still no uniform scientific evidence to recommend a specific treatment over another depending on the type of fracture.3–8 Nevertheless, the use of palmar locking plates is becoming increasingly extended for the treatment of DRF with associated instability criteria. The mechanical resistance they offer enable the management of both osteoporotic and comminuted bones, as well as initiating early mobilization. Regulated volar approaches facilitate anatomical reduction of fractures and the use of low-profile locking systems reduces the possibilities of conflicts with the material. All of these advantages have led to an increasingly widespread use of this material for the treatment of unstable DRF. The literature contains several studies which report satisfactory functional and radiographic results, but their use is not without associated complications, especially in the hands of inexperienced surgeons.2,9–13 Fragmentation of osteopenic and/or comminuted bone, and the resulting bone defect are frequent problems in these fractures, which can benefit from the use of these types of plates.
On the other hand, the use of bone substitutes and grafts to aid the consolidation process and prevent fracture collapse is also frequent. Nevertheless, the use of these materials is not without complications and also increases the cost of the procedure.14
The combination of volar locking plates associated to bone substitutes or grafts to fill the metaphyseal trabecular defect seems a reasonable solution for the treatment of unstable DRF with greater comminution and/or osteoporotic bone. However, there are no evidence based medicine studies to support this. In its clinical guide for the treatment of these lesions published in 2011, the American Academy of Orthopedic Surgeons (AAOS) did not take a stance regarding the use of bone substitutes or grafts associated to volar locking plate systems.5
The aim of our study was to evaluate the clinical and radiographic results of unstable DRF with considerable comminution (A3 and C3 type DRF cases according to the AO classification) synthesized with volar locking plates, with no bone substitutes or grafts in any of the cases.
Patients and methodologyWe conducted a prospective, observational and descriptive study at the Hand and Wrist Surgery Unit of our hospital.
From January 2009 until January 2013, all unstable DRF cases undergoing surgery at our center were included in a study protocol which collected the following variables:
- -
Demographic data (age, gender, laterality, dominance).
- -
Fracture instability criteria (dorsal angle over 20°, dorsal comminution greater than 50%, radial collapse greater than or equal to 5mm, associated ulnar fracture, joint step sign greater than 2mm, age over 65 years and loss of reduction).
- -
Type of fracture according to the AO classification.
- -
Associated lesions (fractures of carpal bones, instabilities of the distal radioulnar or carpal joints, others).
- -
Intensity of the trauma: high/low energy.
- -
Type of osteosynthesis material used in the radius and, if necessary, the ulna (Kirschner wires, volar plate, dorsal plate, external fixator, screws).
- -
Radiographic variables measured, both in the intervened wrist and in the healthy contralateral wrist (radial inclination, radial height, ulnar variance and palmar tilt).
- -
Immobilization period, rehabilitation.
- -
Measurement of the range of movement in both wrists, healthy and fractured (flexion, extension, pronosupination).
- -
Functional tests: PRWE and DASH.
- -
Evaluation of complications (infections, pseudoarthrosis, tendinopathies, neuropathies, discomfort caused by the material, return to previous activity, etc.).
Out of the 345 unstable distal radius fractures undergoing surgical intervention at our center which were included in the study protocol over the period of 4 years, 60 fulfilled the inclusion criteria and accepted to take part in the study.
The criteria for inclusion in the study were the following:
Skeletally mature patients with unilateral, comminuted (type A3 or C3 in the AO classification) and unstable (with, at least, three criteria for instability) fractures of the distal radius, which were synthesized with palmar locking plates and with no bone substitute or graft. All patients were clinically and radiographically monitored for at least 1 year.
Fractures intervened using a different method, bilateral or with other associated lesions, open fractures, with associated severe systemic pathologies and cases with a follow-up period under 1 year were all excluded.
In all cases, the surgery was carried out with locoregional anesthesia through axillary block from the outset, with patients placed in the supine position with the affected limb on a radiotransparent hand table and under ischemia with a pneumatic tourniquet and intraoperative fluoroscopic support. All the procedures were conducted through the standard volar approach described by Henry.15 The osteosynthesis was carried out using volar locking plates of one of three types: LCP-Synthesz®, Aptus 2.5 – Medartis® Aculoc – Acumed®.
In all cases, we placed a drainage device connected to a vacuum system and removed it 48h after the intervention, coinciding with the first cure, when we also obtained a postoperative radiograph. All patients were immobilized with a dorsal antebrachial cast for 2–3 weeks, according to the judgment of the surgeon. All the surgeons (4) belonged to the Hand and Wrist Unit.
The patients were reviewed in the clinic 2–3 weeks after the surgery to remove stitches and immobilization and to start active wrist mobilization. All the patients were referred to the rehabilitation service of our center. Subsequent reviews took place after 6 weeks and 3, 6 and 12 months of the intervention. Control radiographs in conventional anteroposterior and lateral projections were obtained at each review in order to evaluate the consolidation process and control secondary displacement.
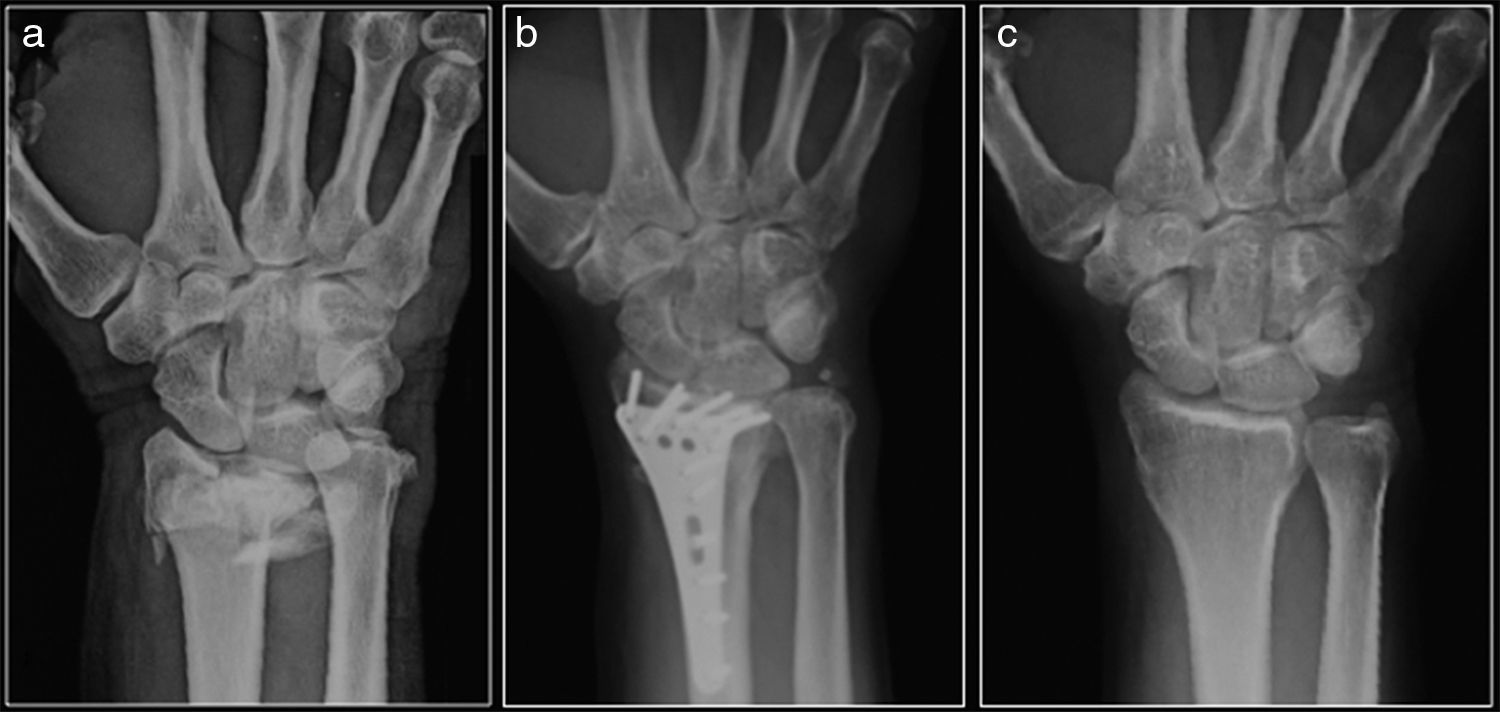
The last radiographic control was compared with the initial postoperative radiographs and with radiographs of the contralateral wrist (Figs. 1 and 2). On the last review, at least 1 year after the intervention, we used the Disabilities of the Arm, Shoulder, and Hand (DASH)16 and Patient Rated Wrist and Hand Evaluation (PRWE)17 scales to evaluate the level of disability suffered by patients and any complications.
Radiograph with the wrist in anteroposterior projection. Type C3 distal radius fracture according to the AO classification. Type C3 distal radius fracture according to the AO classification synthesized with a volar LCP plate. Radiographic control 1 year after the surgery. Mirror image of the healthy contralateral wrist.
Radiograph with the wrist in lateral projection. Type C3 distal radius fracture according to the AO classification. Type C3 distal radius fracture according to the AO classification synthesized with a volar LCP plate. Radiographic control 1 year after the surgery. Mirror image of the healthy contralateral wrist.
The statistical analysis was carried out using the data analysis program SPSS Statistics Version 19 (SPSS Inc., Chicago, Illinois, USA). We carried out descriptive statistics and the T-test pairs procedure to compare two means of matched pairs.
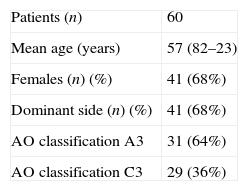
ResultsOut of the 60 patients who fulfilled the inclusion criteria and were monitored for at least 1 year, 41 were female (68.3%) and 19 were male (31.6%), with a mean age of 57 years (range: 23–82 years). The injured wrist was the right in 41 cases (68.3%) and the left in the remaining 19 (31.6%). A total of 63.75% (31) were classified by the surgeon as type A3, whilst 36.25% (n=29) were classified as type C3, using the AO classification system (Table 1).
The osteosynthesis was carried out using volar locking plates: 15 LCP-Synthes® (25%), 38 Aptus 2.5 – Medartis® (63.3%), 7 Aculoc-Acumed® (11.6%). Ulnar osteosynthesis was necessary in five patients, of which three (5%) cases were synthesized using a plate, one with a compression screw and one with cerclage.
Bone substitutes and grafts were not used in the fracture synthesis in any case.
Fracture consolidation was observed in 100% of cases. The majority of patients (80%) did not suffer any associated complications, three of them (5%) suffered tenosynovitis of the flexor tendons, another three (5%) presented symptoms of carpal tunnel syndrome (CTS), there was one case of (1.7%) of tenosynovitis of the extensors, one case of extensor pollicis longus tear and one case (1.7%) of persistent pain in the distal radioulnar joint. The plate had to be removed in six cases (10%) due to CTS complications and mechanical tenosynovitis of the flexors as previously mentioned (Table 2).
Complications.
| Type of complication | n (%) |
|---|---|
| None | 47 (78.3) |
| Infection | 0 |
| Pseudoarthrosis | 0 |
| Extensor pollicis longus tear | 1 (1.7) |
| Tenosynovitis of the flexor tendons | 3 (5) |
| Tenosynovitis of the extensor tendons | 1 (1.7) |
| Distal radioulnar pain | 1 (1.7) |
| Carpal tunnel syndrome | 3 (5) |
| Chronic unspecific pain | 4 (6.7) |
| Extraction of the osteosynthesis material | 6 (10) |
The majority of patients (92%) returned to their daily activity prior to the intervention.
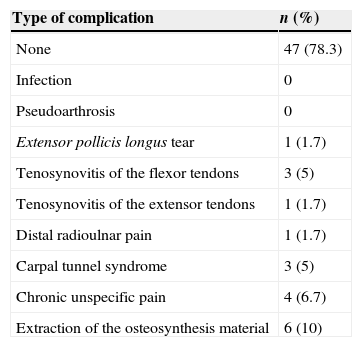
The motion ranges obtained 1 year after the procedure compared with the parameters of the healthy contralateral wrist reflected:
A mean loss of 12±16° flexion in the fractured wrist, which presented a mean value of 49±13°.
The mean extension obtained was of 55±12°, with a mean loss of 9±13° compared to the healthy wrist.
Mean pronation obtained was 78±9° with a mean loss of 2±7.5°, whilst mean supination achieved was 77±14°, with a loss of 5±10° compared to the healthy wrist (Table 3).
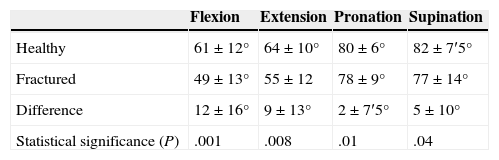
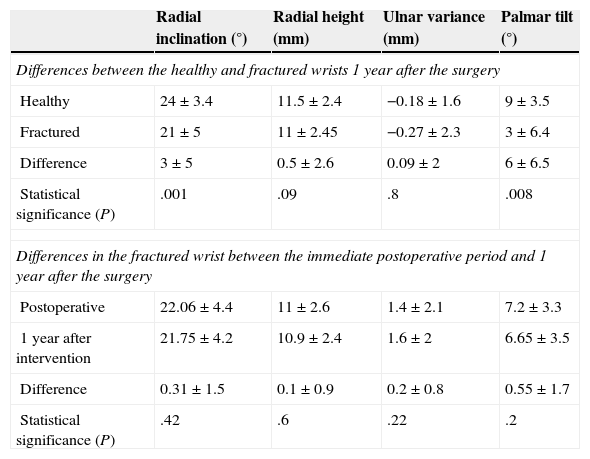
Comparing the radiographic parameters of the fractured wrist in the immediate postoperative period with those of the same wrist after 1 year, we observed a mean loss of 0.31±1.5° in radial inclination, a mean loss of 0.1±0.9mm in radial height, 0.2±0.8mm in ulnar variance and 0.55±1.7° in the palmar tilt of the radius.
Comparing the radiographic parameters of the healthy wrist with the fractured wrist 1 year after the intervention we observed a mean loss of 3±5° in radial inclination compared to the healthy wrist, mean loss of 0.5±2.6mm in radial height, 0.09±2mm in ulnar variance and 6±6.5° in palmar tilt of the radius (Table 4).
Radiographic parameters.
| Radial inclination (°) | Radial height (mm) | Ulnar variance (mm) | Palmar tilt (°) | |
|---|---|---|---|---|
| Differences between the healthy and fractured wrists 1 year after the surgery | ||||
| Healthy | 24±3.4 | 11.5±2.4 | −0.18±1.6 | 9±3.5 |
| Fractured | 21±5 | 11±2.45 | −0.27±2.3 | 3±6.4 |
| Difference | 3±5 | 0.5±2.6 | 0.09±2 | 6±6.5 |
| Statistical significance (P) | .001 | .09 | .8 | .008 |
| Differences in the fractured wrist between the immediate postoperative period and 1 year after the surgery | ||||
| Postoperative | 22.06±4.4 | 11±2.6 | 1.4±2.1 | 7.2±3.3 |
| 1 year after intervention | 21.75±4.2 | 10.9±2.4 | 1.6±2 | 6.65±3.5 |
| Difference | 0.31±1.5 | 0.1±0.9 | 0.2±0.8 | 0.55±1.7 |
| Statistical significance (P) | .42 | .6 | .22 | .2 |
The functional assessment scales (PRWE and DASH) score the level of subjective satisfaction of patients from 0 to 100, evaluating residual pain and function aspects, assuming that higher values indicate a worse result. The patients analyzed reported a good level of subjective satisfaction. The mean values of the studied patients were 6.31±9.5 in the DASH scale and 12.59±14.16 in the PRWE scale.
The mean postoperative hospital stay was 2 days.
Statistical analysis of resultsThe results reflected a statistically significant relationship (P≤.05) between the loss of mobility in flexion, extension, pronation and supination of the fractured wrist 1 year after the surgery and the mobility of the healthy contralateral wrist.
However, when evaluating the degree of fracture collapse, we did not find statistically significant differences in the radiographic parameters of radial inclination (P=.42), radial height (P=.6), ulnar variance (P=.22) and palmar tilt (P=.2), comparing the immediate postoperative radiographic controls with those obtained 1 year after the intervention.
If we evaluate the same parameters in the radiographic controls of the fractured wrist 1 year after the surgery and compare them to the healthy contralateral wrist, we can only observe statistical significance in palmar tilt and radial inclination. On the other hand, the differences observed in radial height (P=.09) and ulnar variance (P=.8) were not statistically significant.
DiscussionThe objective of treating DRF is to achieve a reduction that is as anatomical as possible in order to prevent the appearance of deformities and posttraumatic distal radioulnar and/or radiocarpal arthritis, as well as to achieve a sufficiently stable fixation to enable early rehabilitation. Comparison of the clinical and radiographic results has proven that a correct anatomical reduction enables a good functional result, although clinical and radiographic agreement does not appear to be the rule.18,19
There is a wide range of therapeutic options available for the treatment of DRF. At present, there are no unified criteria to indicate the different types of treatment. Therapeutic options are chosen based on fracture patterns, the functional demands of each patient, bone quality and/or presence of associated lesions.4 The clinical and functional results of the different therapeutic options are not systematically satisfactory, especially among elderly patients with bones that have been weakened by osteoporosis and among young patients with highly comminuted fractures caused by high-energy trauma.3,5–8
At present, the most commonly used osteosynthesis method is with volar locking plates.2,9–13 The main advantages of these type of systems are the possibility of covering the plate with the pronator quadratus, avoiding tendon irritation problems, preserving the dorsal metaphyseal vascularization of the distal radius and a greater ease for anatomical reduction of the fracture, since the volar cortical usually presents less comminution than the dorsal cortical. Nevertheless, there have also been reports of problems with the use of these systems, including intraarticular penetration of screws, particularly when the locking systems are not polyaxial, irritation and tear of extensor tendons caused by friction with the screws and irritation of the flexor tendons when the plates do not have a low profile.2,3,9–13,20,21
Patients with osteoporotic bones usually present fractures with considerable comminution and/or significant metaphyseal defects that can generate problems like loss of reduction and consolidation in erroneous positions, associated to loss of strength, pain and rigidity. In order to avoid these kinds of complications, it is possible to use bone substitutes or grafts to fill the cavities created. This has been proven to avoid collapse and contribute to the consolidation process.22,23 However, these materials should not be used systematically, as each has different biological characteristics and their use is not without associated complications. Moreover, they add a non-negligible cost to the procedure.
From a biological standpoint, autografts are the best option in terms of osteogenic, osteoinductive and osteoconductive capacity. However, they entail a significant risk of complications at the donor site, including pain, hematoma, infection and the possibility of neural lesion. The use of allografts avoids the associated morbidity at the donor site, but lacks osteogenic capacity and adds a risk of disease transmission, although thanks to the regulations governing storage and processing of allografts, this is currently minimal.
Lastly, synthetic materials do not carry the risks of disease transmission and comorbidities for the patient, but their biological properties vary considerably.14,24 This category includes three main groups: ceramics, polymers and metals.
Polymers in the form of methacrylate cements fill the cavities, providing only a support to avoid the collapse of joint surfaces, but they do not integrate into and cannot be replaced by bone. They have the drawback of causing a highly exothermic reaction, with risk of associated tissue necrosis.
Ceramic materials are calcium cements and are in turn divided into three main types: calcium carbonate, calcium sulfate and calcium phosphate. Calcium sulfate is a biocompatible and osteoinductive material that is occasionally used as a vehicle to release antibiotics at the focus of infection. The most commonly employed ceramic substitutes are tricalcium phosphate, apatite and hydroxyapatite. As main differential characteristics we can highlight that tricalcium phosphate is fully remodeled within 6–18 months, whilst apatites remain unaltered for years.24,25 Carbonated apatite has been used in the treatment of distal radius fractures to reduce the fracture on orthopedic tables and injecting Norian SRS® (Synthes) (carbonated apatite) percutaneously into the defect created. Immobilization is maintained with a plaster cast for 2 weeks and wrist mobilization is started after this period.23
Both the data reflected in the literature and the recommendations in the clinical guideline published by AAOS leave to the surgeon the choice of whether or not to use bone substitutes or grafts in DRF synthesized with volar locking plates. This surgical action adds a non-negligible cost to the procedure and is not exempt from associated complications, which made the authors reconsider the need for its use.5,14,22,24
Based on the clinical and radiographic results obtained, the statistical analysis performed and the international medical literature, the authors have reached the conclusion that the use of bone substitutes or grafts is not essential for the primary surgical treatment of unstable DRF with greater osteoporosis and/or comminution using LCP volar plates, and that it makes the treatment more costly and is not exempt from morbidities. The minimal loss of mobility observed in the four main wrist movements agreed with the results reflected in the literature and was within functional ranges. We obtained 100% consolidation of the fractures without observing a significant radiographic collapse in the radiographic parameters studied. As secondary conclusions, the study reinforced the role of LCP volar plates for the treatment of DRF with instability criteria. This is a safe surgical alternative that achieves a stable and anatomical reduction. It enables early mobilization of the wrist and obtains good functional and radiographic results. Nevertheless, it is not exempt from associated complications despite being conducted by experienced surgeons, as reflected by our results and the medical literature.2,9–13
The present study has various limitations. It is a prospective review which describes our results and is therefore limited to presenting a series of clinical cases, without a control group in which bone substitutes or grafts were used in order to compare the results obtained.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Garcés-Zarzalejo C, Sánchez-Crespo MR, Peñas-Díaz F, Ayala-Gutiérrez H, Sanz Giménez-Rico JR, Alfonso-Fernández A, et al. Fracturas de radio distal: ¿es necesario el aporte de injerto o sustitutivo óseo en los casos con osteoporosis o conminución severa? Rev Esp Cir Ortop Traumatol. 2015;59:97–103.