Ankle fractures account for up to 10% of total fractures. Most of them require surgical fixation, which involves an important risk of wound complications. The aim of this study was to determine whether a silver-impregnated occlusive surgical dressing (Aquacel Ag Extra®) was effective in reducing the rates of wound complications after ankle fracture open reduction and internal fixation compared to standard sterile dressing.
MethodsWe prospectively reviewed 233 patients who underwent ankle fracture open reduction and internal fixation. Surgeons switched from using a standard dressing to an Aquacel Ag Extra® from July 2017 to February 2018, without other major changes in perioperative management. We compared skin complications between both groups after 3 months’ follow-up.
ResultsThe statistical analysis showed that there is no difference in the prevalence of skin complications between both groups.
ConclusionsThe theoretical advantages of silver impregnated dressings need further prospective randomised controlled studies to assess the appropriate indications for their use in orthopaedic surgery.
Las fracturas de tobillo representan un 10% del total de fracturas. La mayor parte requieren tratamiento quirúrgico, que conlleva un importante riesgo de complicaciones de la herida. El objetivo de este estudio ha sido determinar si los apósitos impregnados con plata (Aquacel Ag Extra®) reducen la tasa de complicaciones de la herida quirúrgica tras el tratamiento de las fracturas de tobillo en comparación con el uso de gasas estériles.
MétodosDe forma prospectiva se han reunido 233 pacientes con fracturas de tobillo subsidiarias de tratamiento quirúrgico. Desde el inicio del estudio en julio de 2017 hasta febrero de 2018, los traumatólogos participantes en el estudio cambiaron el uso de la gasa estéril estándar para cubrir la herida quirúrgica tras su cierre por Aquacel Ag Extra®, manteniendo el resto del protocolo pre- y posquirúrgico igual. Se comparan la tasa de complicaciones cutáneas en ambos grupos, tras un seguimiento de 3 meses.
ResultadosEl análisis estadístico no reflejó diferencias significativas entre ambos grupos.
ConclusionesSe necesitan ensayos clínicos aleatorizados para demostrar las ventajas teóricas de los apósitos impregnados con plata y su indicación en Traumatología.
Ankle fractures account for 10% of all fractures. Most require open reduction and internal fixation (ORIF) for anatomical reduction of the joint.1 In spite of the fact that the results are generally good, treatment of surgical site complications remains a problem for the traumatologist.2 Wound complications include dehiscence, necrosis and infection.3 The incidence of surgical site infection, the most feared skin complication, ranges between 1.4% and 5.5%, depending on the publication.4 Risk factors linked to such infections include open fractures, diabetes mellitus, tobacco habit and advanced age.5–10 Their treatment varies depending on the severity, including from local treatment up to removal of the tissue and intravenous antibiotic treatment. The most frequently isolated microorganisms are Staphylococcus aureus, Coagulase-Negative Staphylococci and Pseudomonas aeruginosa. In recent years, the rate of multi-resistant strains has increased greatly, to the point of being isolated in 60% of the infections.11 Due to the increase in both personal and economic costs that these complications entail, several preventative measures have been investigated.12,13
Some studies suggest that the type of dressing used can create a barrier that decreases the access of the bacteria to the surgical site wound.14 Theoretically, dressings impregnated with silver are antimicrobial and, thanks to their capacity to absorb exudates, prevent the skin from macerating, promoting healing.15
The main objective of this study was to determine if treating the surgical site after open reduction and internal fixation of an ankle fracture with silver-impregnated dressings would reduce the incidence of wound complications in comparison with sterile dressing treatment.
MethodsAfter obtaining the approval of our Ethics Committee, the personal, radiographic and medical data of 233 patients that had undergone interventions for ankle fracture in our hospital between July 2017 and February 2018 were collected. The inclusion criteria for the study were as follows: age between 18 and 80 years and signed informed consent. All the patients with open, tibial pilon or Maisonneuve fractures, polytrauma cases and patients with dermatological pathology in the area of the surgical approach were excluded.
From 1 July 2017, a group of traumatologists began to apply silver-impregnated dressings (Aquacel Ag Extra®), thereby creating two cohorts based on whether the patient underwent an intervention before or after the beginning of the study: patients on whom sterile dressings were used and those on whom silver-impregnated dressings were used to cover the surgical site. The rest of the operating theatre protocol was the same for both groups: use of tourniquet on the thigh, antibiotic prophylaxis with cefazolin 1g an hour before performing the incision, antithrombotic prophylaxis with low molecular weight heparin and skin preparation by cleansing with chlorhexidine. The first treatment carried out from 2 to 6 days postoperatively was supervised by a specialised nurse who filled out the ASEPSIS wound scoring scale for each patient. The patients were also followed up in office visits with the Traumatologist for 3 months. The ASEPSIS scale is a scale for evaluating the state of a postoperative wound, published in The Lancet journal in 1986, as a useful tool to standardise how a wound is described (Appendix B, Supplementary material appendixes 1 and 2).
Statistical analysis was carried out with the IBM Statistical Package program version 19.0. The Mann–Whitney and Chi-square tests were used to detect statistically significant differences (P<.05) between the 2 groups.
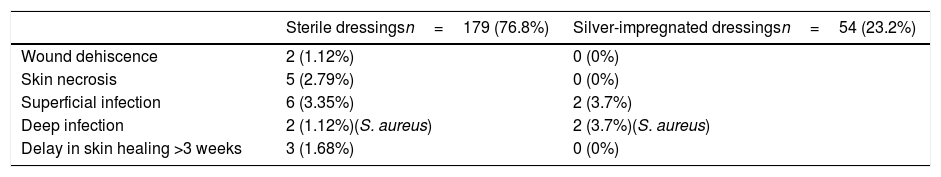
ResultsFor 3 months, 54 patients in the cohort in which silver-impregnated dressings were used and 179 patients in the cohort in which sterile dressings were used were followed up. The incidence of surgical site complications in the first group was 7.4% (4/54), while it was 10% (18/179) in the second group. The complications were mostly minor and were handled with local treatments and oral antibiotics. There was only 1 infection that required surgical debridement and intravenous antibiotic treatment. None of the complications recorded were attributed to patient characteristics, use of immobilizations or wound treatment method. All the data collected on the different complications are presented in Table 1.
Complications in both groups during the follow-up period.
| Sterile dressingsn=179 (76.8%) | Silver-impregnated dressingsn=54 (23.2%) | |
|---|---|---|
| Wound dehiscence | 2 (1.12%) | 0 (0%) |
| Skin necrosis | 5 (2.79%) | 0 (0%) |
| Superficial infection | 6 (3.35%) | 2 (3.7%) |
| Deep infection | 2 (1.12%)(S. aureus) | 2 (3.7%)(S. aureus) |
| Delay in skin healing >3 weeks | 3 (1.68%) | 0 (0%) |
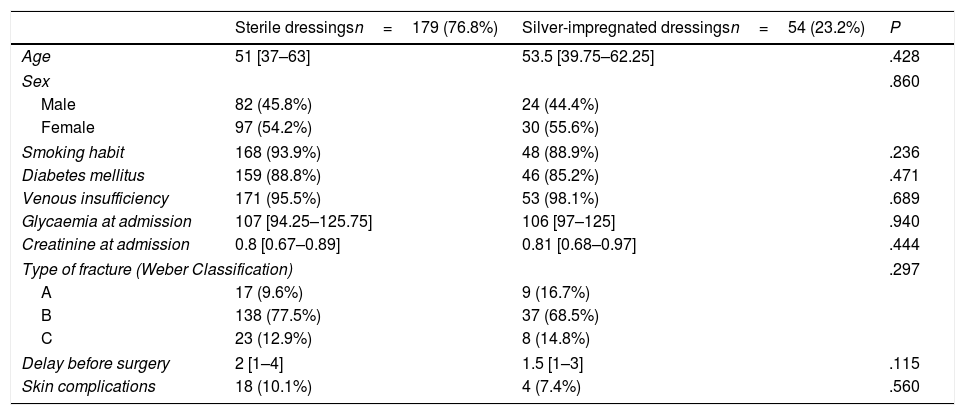
Statistical analysis did not show any statistically significant differences between the 2 groups. The independent variables analysed can be seen in Table 2.
Statistical analysis of independent variables analysed in the two groups.
| Sterile dressingsn=179 (76.8%) | Silver-impregnated dressingsn=54 (23.2%) | P | |
|---|---|---|---|
| Age | 51 [37–63] | 53.5 [39.75–62.25] | .428 |
| Sex | .860 | ||
| Male | 82 (45.8%) | 24 (44.4%) | |
| Female | 97 (54.2%) | 30 (55.6%) | |
| Smoking habit | 168 (93.9%) | 48 (88.9%) | .236 |
| Diabetes mellitus | 159 (88.8%) | 46 (85.2%) | .471 |
| Venous insufficiency | 171 (95.5%) | 53 (98.1%) | .689 |
| Glycaemia at admission | 107 [94.25–125.75] | 106 [97–125] | .940 |
| Creatinine at admission | 0.8 [0.67–0.89] | 0.81 [0.68–0.97] | .444 |
| Type of fracture (Weber Classification) | .297 | ||
| A | 17 (9.6%) | 9 (16.7%) | |
| B | 138 (77.5%) | 37 (68.5%) | |
| C | 23 (12.9%) | 8 (14.8%) | |
| Delay before surgery | 2 [1–4] | 1.5 [1–3] | .115 |
| Skin complications | 18 (10.1%) | 4 (7.4%) | .560 |
Surgical site infection constitutes the most frequently acquired hospital infection, accounting for 38% of the nosocomial infections.16 There are several studies that encourage the use of dressings impregnated with silver to reduce the incidence of these complications because they optimise wound healing thanks to their capacity to eliminate dead spaces and absorb exudates. They are also a barrier against exogenous bacteria.
A systematic review carried out by Cochrane in 2014 included 20 controlled randomised trials to determine if dressings with silver were useful to reduce surgical wound infections after operations with primary closure. However, the conclusion was reached that the evidence to support this was too limited to establish whether any type of dressing reduced these complications.17
Kadar et al.18 published a prospective randomised clinical trial in which the efficacy of silver-impregnated dressings for both reducing skin colonisation after hip fracture surgery in the elderly and reducing infection of the surgical site wound remained unproven.
Galli et al.15 carried out a prospective study with 59 patients that had foot and ankle surgery with incisions larger than 1cm. The incidence of wound complications in the group treated using sterile dressings (26.67%) was significantly greater than that of the group treated with silver-impregnated dressings (3.45%) (P=.03).
Grosso et al.19 published a study that found a significant reduction of periprosthetic infection after using treatments with silver-impregnated dressings compared with standard sterile dressings. In 2018, the American Academy of Orthopaedic Surgery stated that using silver-impregnated dressings was useful in reducing periprosthetic infection following primary arthroplasty.20
The main limitations of this study are the limited number of patients in the cohorts and the lack of randomisation. However, the strong points of the study include the fact that it is a prospective study and that all the patients have been treated in the same hospital, following a standardised protocol. On another note, cost-effectiveness studies would be necessary to demonstrate whether the possible reduction in the rate of surgical site complications from using silver-impregnated dressings in all surgically-treated ankle fractures would be greater than the expense of using them.
ConclusionsSurgical site complications after ankle fracture surgery continue to be one of the main complications of this surgery. However, reducing their incidence can lead to a relevant improvement in functional results and patient satisfaction, consequently leading to a decrease in costs. Despite the fact that the use of silver-impregnated dressings has increased in recent years, the evidence as to their efficacy in Orthopaedic Surgery and Traumatology is limited. Most of the studies present a low level of evidence (this article has a level of evidence II) and there are very few controlled and randomised clinical trials. In our opinion, further controlled randomised trials are needed to make it possible to establish the indication for the use of silver-impregnated dressings in our speciality.
FundingThis research has not received any specific funding from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestsThe authors have no conflicts of interest to declare.
We wish to thank the nursing team and the Traumatologists that have participated for their collaboration, as well as thanking Manuela Expósito, a member of the Department of Statistics at the Hospital Universitario Virgen de las Nieves, for hers.
Please cite this article as: Luque-Valenzuela M, Sánchez-Aguilera AJ, Martín-Vivaldi-Jiménez A, Jódar-Graus R, Prados-Olleta N. ¿Disminuyen las complicaciones cutáneas tras la cirugía de fracturas de tobillo con el uso de Aquacel Extra Ag®? Rev Esp Cir Ortop Traumatol. 2019;63:342–345.