The prognosis of children with progressive early onset scoliosis has improved considerably due to recent advances in surgical and non-surgical techniques and the understanding of the importance of preserving the thoracic space. The existing techniques and development of new methods have considerably improved the management of this condition. Derotational casting can be considered in children with documented progression of a <60° curve without previous surgical treatment. Both single and dual growing rods are effective, but the latter seem to offer better results. Hybrid constructs may be a better option in children who require a low-profile proximal anchor. The vertical expandable prosthetic titanium rib (VEPTR®) appears to be beneficial for patients with congenital scoliosis and fused ribs, and thoracic Insufficiency Syndrome. Children with medical comorbidities who may not tolerate repeated lengthenings should be considered for Shilla or Luque Trolley technique. Growth modulation using shape memory alloy staples or other tethers seem promising for mild curves, although more research is required to define their precise indications.
El pronóstico de los niños con escoliosis de aparición precoz progresiva ha mejorado considerablemente gracias a los recientes avances en las técnicas quirúrgicas y no quirúrgicas, y al reconocimiento de la trascendencia de preservar la cavidad torácica. La mejora de técnicas ya existentes y el desarrollo de otras nuevas han modificado sustancialmente el tratamiento de esta entidad. Los yesos derrotatorios pueden indicarse en niños con curvas <60° y progresión constatada, a los que no se ha realizado tratamiento quirúrgico previo. Tanto los tallos de crecimiento únicos como dobles son eficaces, aunque los últimos parecen ofrecer un mejor resultado. Los sistemas híbridos se plantean como mejor opción en niños que requieren un anclaje proximal con un perfil bajo. El vertical expandable prosthetic titanium rib (VEPTR®) puede ser útil en pacientes que presentan escoliosis congénita con fusiones costales y síndrome de insuficiencia torácica asociado. Los niños no tributarios de elongaciones repetidas por sus comorbilidades pueden ser candidatos a una técnica de Shilla o trolley de Luque. La modulación del crecimiento utilizando grapas de memoria o tirantes resulta prometedora en curvas menores, aunque se requieren más trabajos para definir su indicación precisa.
In recent years, early-onset scoliosis (EOS) has generated considerable controversy in the field of orthopedic surgery. The unfavorable natural history of this entity, associated to the unfavorable effects of early spinal fusion, have led orthopedic surgeons treating these patients to use an arsenal of surgical techniques in an attempt to prevent, delay or limit spinal fusion. These growth friendly techniques enable control of the disease whilst allowing the spine to continue growing. The development of these new techniques and implants has brought about a gradual incorporation of children into the field of vertebral instrumentation, whilst also facilitating the correction of considerable spinal deformities. Nevertheless, in very young patients the correction of the curve does not always imply the correction of the disease. Although the initial results are promising, the lack of long-term results, the impossibility of establishing precise indications and contraindications for each method and the lack of large series of patients due to the relative rarity of this condition, mean that such results should be regarded with certain caution.
Throughout the last decade there has been substantial progress in understanding the natural history and treatment options for EOS. There are a number of basic concepts which transcend the simple recognition of the importance of lung function, and whose understanding is essential in the analysis of the advances that have occurred in the management of EOS. At 8 years of age the bronchial tree and alveoli are fully developed, and at 10 years the thoracic volume has reached 50% of the volume expected as an adult.1,2 In addition, the T1–S1 length increases dramatically in the first 5 years of life (2.2cm/year), more slowly during the next 5 years (1cm/year) and then increases once again with the onset of puberty (1.8cm/year).3 Reaching a T1–T12 length of at least 18cm at the time of maturity is associated with improved lung function.4
At present, we know that, if untreated, progressive EOS can lead to severe pulmonary complications, including thoracic insufficiency syndrome (TIS), which was defined by Robert Campbell as the inability of the thorax to maintain normal lung growth and respiratory function.5 In addition, it has been observed that the fusion of multiple segments of the pediatric spine, particularly in the thoracic region, can lead to an even worse outcome by preventing normal growth of the spine and the thorax.4 Moreover, Vitale et al.6 have shown the adverse effects of early fusions on lung function. However, the recent contribution of Kotani et al.7 has relativized the thoracic impact of early spinal fusions in patients with congenital scoliosis.
A statistically significant increase in mortality risk has also been observed in relation to respiratory failure in children with infantile or juvenile scoliosis compared with children with adolescent idiopathic scoliosis.8
The recent development of growth-preserving techniques has provided orthopedic surgeons with revolutionary therapeutic options for the treatment of progressive EOS. Nevertheless, the limited amount of evidence-based information on EOS entails that treatment decisions are based largely on the clinical experience and knowledge of each individual surgeon. Therefore, there is considerable variability among surgeons when selecting one treatment or another.9,10 A recent work has shown that increasing surgeon experience also increases the use of non-fusion techniques.11 The optimal choice of treatment is even more complex due to the different causes of EOS.
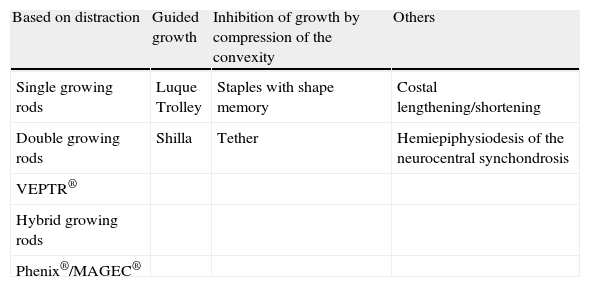
Skaggs et al.12 have proposed a classification of growth-preserving techniques according to the mechanism by which they modulate spinal and thoracic wall growth (Table 1). This classification includes some techniques based on distraction, compression and guided growth.
Classification of growth-preserving techniques.
| Based on distraction | Guided growth | Inhibition of growth by compression of the convexity | Others |
| Single growing rods | Luque Trolley | Staples with shape memory | Costal lengthening/shortening |
| Double growing rods | Shilla | Tether | Hemiepiphysiodesis of the neurocentral synchondrosis |
| VEPTR® | |||
| Hybrid growing rods | |||
| Phenix®/MAGEC® |
Source: Skaggs et al.12
The purpose of this work is to review current growth-preserving techniques for the treatment of EOS.
Derotational castingCasting techniques were habitually employed for the treatment of scoliosis before the development of spinal instrumentation. At present, this technique is most commonly indicated for patients who have not undergone any surgical treatment and present a proven progression of the curve (between 10° and 20° progression or a curve beyond 25°), but with a low magnitude in the coronal plane (<60°), or with a clear expected progression: costovertebral angle difference >20° or rib in Mehta phase 2. Both parameters were described by Mehta in 1972.13
The costovertebral angle is that existing between the apical vertebra and its corresponding rib. An initial line is drawn perpendicularly to the superior or inferior margin of the apical vertebra. Next, another line is drawn which connects the midpoint of the rib head with the midpoint of the neck thereof. This second line is extended proximally up to its intersection with the first line and between them they define the costovertebral angle on that side. The costovertebral angle difference is the difference between the costovertebral angles of the convexity and concavity of the curve. Under normal conditions, both angles must be equal or their difference should be zero.
On the other hand, an anteroposterior radiograph of a normal spine or one in the initial stages of development of scoliosis should show a space between 2 and 4mm between the head of the apical rib of the convexity and the upper corner of the corresponding vertebra. This position is defined as phase 1. When the rib head overlaps the upper corner of the apical vertebra we have a phase 2 rib.
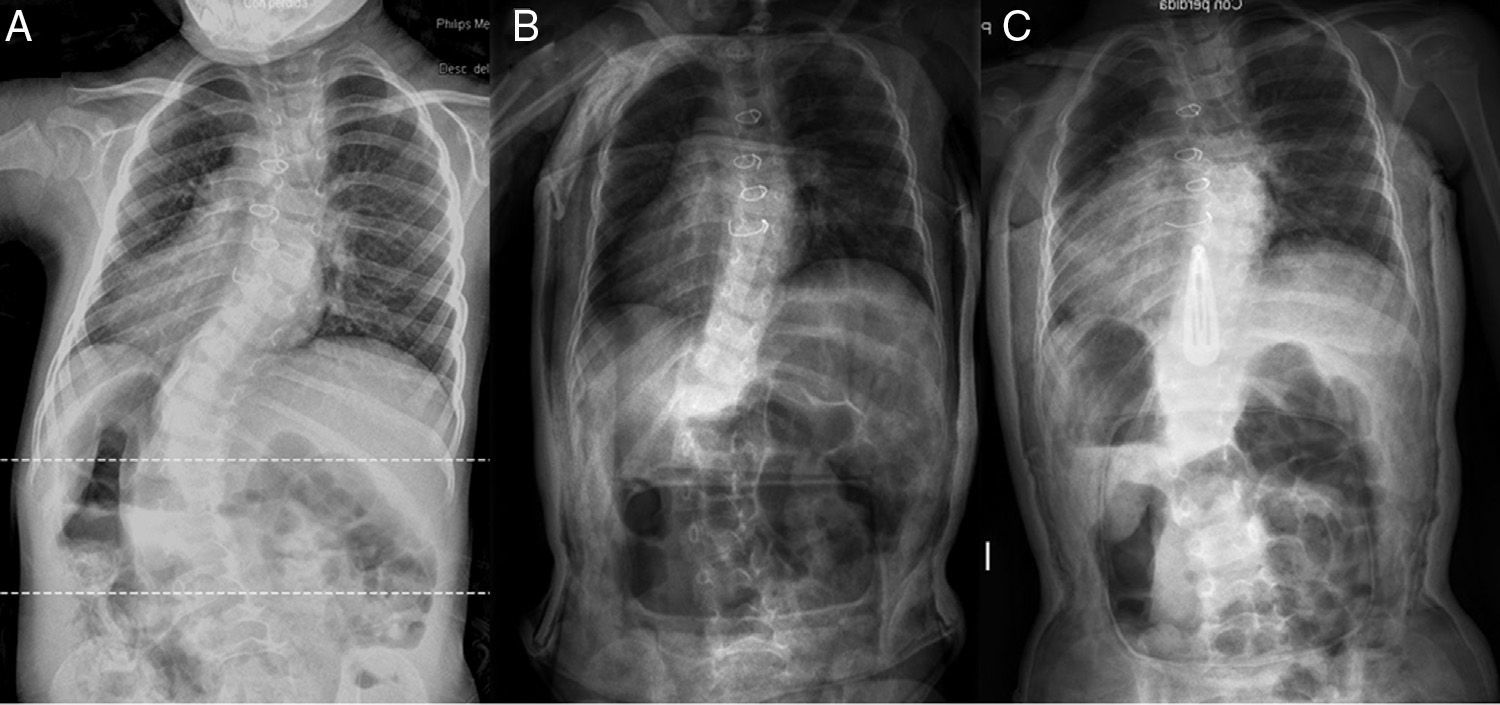
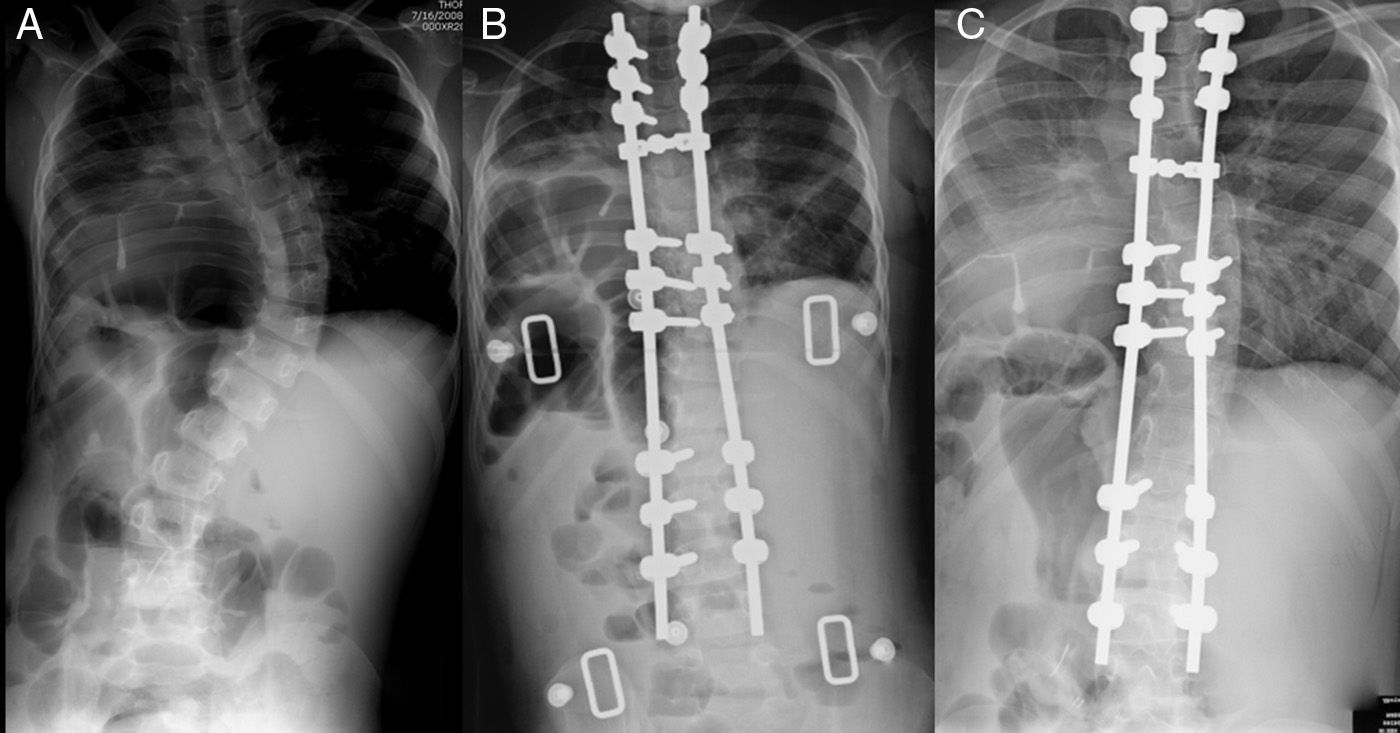
Treatment using casts has been associated with multiple complications.14 The derotatory technique popularized by Mehta15 has largely solved these problems, basically associated with the Risser technique with 3 support points. The cast is placed under general anesthesia, using a specially designed table which allows the application of proximal and distal distraction, supports the head, arms and legs, and leaves the thorax exposed to facilitate placement of the plaster cast (Fig. 1). The ribs are not pushed toward the spine, but are rotated by applying an anterior force on one side and a posterior force on the opposite side. The cast is changed every 2–4 months, interrupting the treatment or replacing the cast by an orthosis when the curve falls below 10°–20°. Children with poor lung function or sensory anomalies may not tolerate the cast.
Several recent series have confirmed the positive results of treatment with derotational casts.15–18 In one of these series,15 the results were correlated with age and severity of the curve at the time of starting treatment. Out of a total 136 patients, 94 (group 1) presented complete correction of the deformity. Patients in this group 1 had been referred for treatment with a mean age of 19 months and presented a mean curve of 32° according to the Cobb angle. The 42 patients in group 2 had been referred for treatment with a mean age of 30 months and presented a mean curve of 52° according to the Cobb angle. A total of 15 patients (35.7%) in group 2 required definitive spinal fusion. This work and other previous ones found that the prognosis improved when the difference between the costovertebral angles was <20°.13 Other favorable prognostic factors are curves <60° and an idiopathic etiology (Fig. 2A–C). Baulesh et al.19 have observed a preservation of the normal thoracic longitudinal growth during the cast period, along with the expected positive effect on lung function. Serial casts are also a viable alternative to non-fusion surgical techniques in cases with moderate and severe EOS, as they are capable of delaying or even avoiding a subsequent surgical intervention.20
Despite the positive results obtained with this conservative technique, it is not without risks.14,21 A transient increase in maximum inspiratory pressure22 during application of casts was recently described. However, the complication rate is considerably inferior compared to other options involving surgery.18
Before proceeding with growth-preserving surgical techniques we should make a special mention of preoperative traction with halo, a technique which is used occasionally in large-magnitude curves prior to instrumentation, in an attempt to reduce neurological risks, achieve a better correction and improve respiratory function before surgery.23 Recent publications have described the use of traction in EOS before growth-preserving instrumentation in curves >80° and when there is an association with kyphosis.24
Surgical techniques based on distractionThese techniques correct and maintain the correction of spinal deformity through distraction of the vertebral column. The implants can be anchored to the spine, ribs or pelvis, depending on the age of the patient, the characteristics of the curve and the quality of bones. Costal proximal fixation is usually more convenient in younger patients in whom there is an attempt to avoid or delay spinal fusion and in whom vertebral anchoring is limited by the immaturity of the vertebral column and the possible complications which this situation can lead to. These techniques can be considered in progressive deformities in which conservative treatment is contraindicated. In general, implants are distracted every 6 months, making this an undesirable option for children with significant comorbidities due to the risk of developing a complication in any of the multiple surgical procedures.
Growing rodsHarrington25 originally introduced the concept of a long, subcutaneous, single rod (or stem) which bypassed a non-fused portion of the spine, although other authors have subsequently modified the technique.26–28 The principle underlying techniques based on distraction is the anchoring of spinal instrumentation at a proximal level, and vertebral or pelvic at a distal level, thus avoiding exposure of the affected vertebral segment. Growth occurs through this intermediate spinal segment, with the deformity being controlled through repeated elongation procedures which make the column “grow”.
The initial results28 were associated with a high rate of complications including equipment failure, loss of fixation of the anchor points and spontaneous spinal fusion with a consequent growth limitation of the thorax and the column itself. Introducing safer anchorage points mounted as a “claw” formed by a descending sublaminar or transverse process hook and a sublaminar or pedicular ascending hook placed 1 or 2 segments distally with fusion limited to these mounting segments has improved results. Another option is mounting with pedicular screws,29 followed by implantation of a single rod left purposefully long (4–5cm) above or below the proximal or distal construct, depending on the location of the curve. This stem is then used for periodic distractions. Another possibility is to employ 2 overlapping stems in the center which are connected by a laterolateral connector. A definitive posterior spinal fusion may be performed once the patient has reached an adequate age and size, or alternatively an anterior spinal fusion associated with a posterior spinal fusion with segmental vertebral instrumentation.
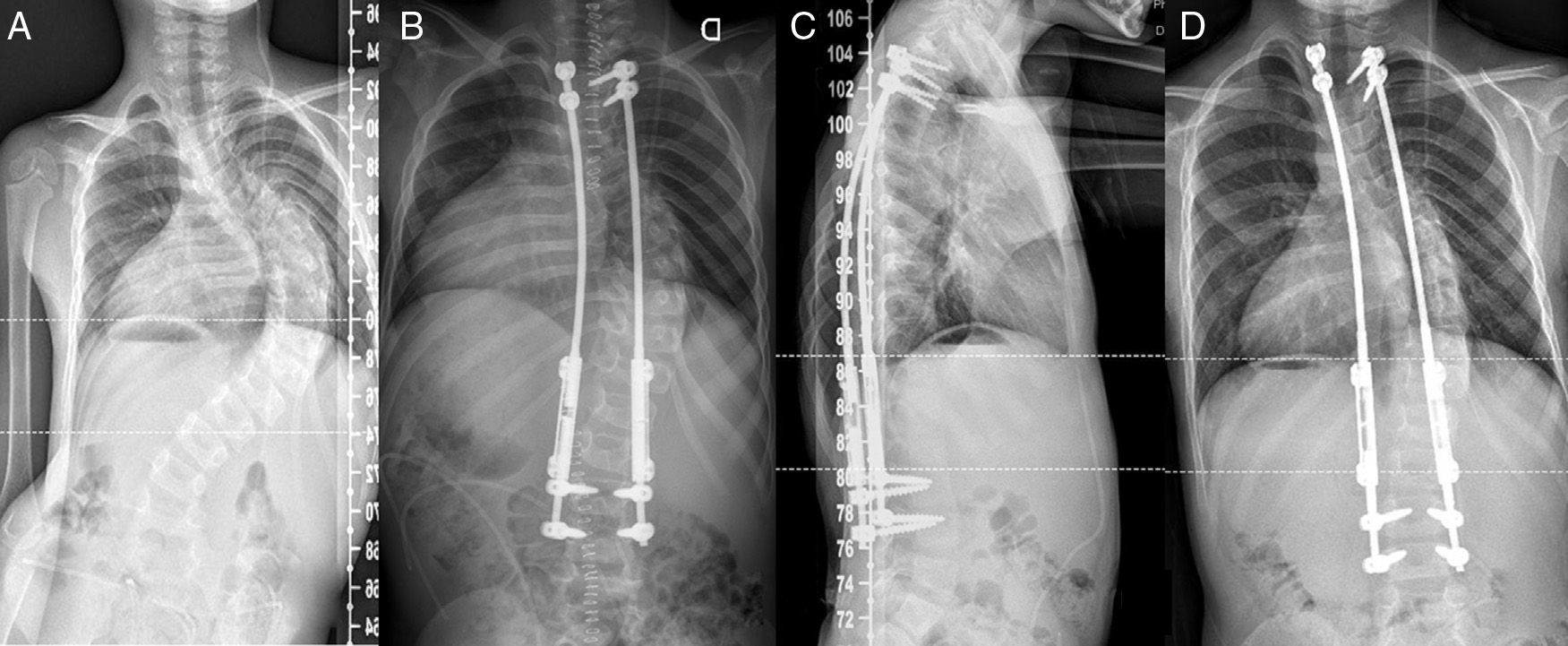
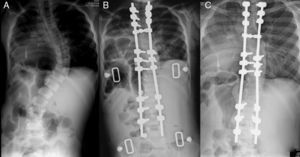
Double growing rods are based on this same principle, but they offer greater stability and a better correction of the deformity.30,31 Each rod is formed by 2 sections which are interconnected by a terminoterminal tandem connector through which stretching is carried out. Mounting is done with pedicular screws or “claws” formed by hooks and these anchor points are fused (Fig. 3A–D). The possibility of a pelvic fixation should be evaluated for the distal anchor in neuromuscular patients. Other authors have shown a significantly better correction of pelvic obliquity and coronal deformity using double stems and iliac screws, compared to other forms of pelvic fixation.32 In turn, Shah et al33 have reported an improvement of the sagittal profile which was independent of the number of elongations performed. The stems are distracted every 6–9 months approximately, regardless of the progression of the curve, in order to maintain the correction achieved.
(A) PA radiograph of a 6+9 boy diagnosed with early onset idiopathic scoliosis with a right thoracolumbar curve of 106°. (B) After placement of the double growth stems the curve decreased to 44°. (C) The sagittal profile was correctly preserved. (D) The patient is now 8+4 and, after 3 extensions, the curve is of 1031°.
In 2005, Akbarnia et al.30 published one of the largest series of double growing rods and reported an improvement of the mean magnitude of the curve from 82° preoperatively to 38° after the first surgery and 36° at the end of the follow-up period. The rods were elongated a mean total of 6.6 times, leading to a mean increase of the T1–S1 distance of 1.2cm/year, with 56% of complications. Another, more recent series, has shown a slightly better correction of the curve and an increase in the length gained when the elongations were performed at intervals <6 months.31
This has been proven to be a relatively safe procedure, although complications are commonplace34 and mostly related to the prolonged period of treatment required by techniques based on distraction. A thorough analysis of the complications of single-stem and double-stem assemblies indicated that 58% of patients suffered at least 1 complication.35 There were fewer complications related to instrumentation in double-stem assemblies compared to single-stem assemblies, and patients with stems implanted subcutaneously presented more wound complications, greater prominence of implants and underwent unforeseen surgical procedures more often compared to patients with stems implanted submuscularly. Wound complications are more frequent when the elongations are performed at more frequent intervals, whilst complications related to implants are more common when elongations are performed at longer intervals.36 In neurological terms, the technique of growing rods seems to be extremely safe, with an overall incidence of changes in neurophysiological monitoring of 0.9%.37 Finally, a law of diminishing returns seems to apply to the repeated elongations of growing rods. Sankar et al38 found that the mean gain of T1–S1 length in the first elongation was 1.04cm and that this parameter gradually decreased in successive elongations.
Vertical Expandable Prosthetic Titanium RibThe Vertical Expandable Prosthetic Titanium Rib (VEPTR®) is a longitudinal costal distraction implant made of a titanium alloy. Being a distraction-based implant, it requires repeated elongations, like growing rods. The primary indication of this implant is for the treatment of skeletally immature patients suffering from TIS.39,40 It was originally designed by Robert Campbell to treat children with TIS secondary to rib fusions and congenital scoliosis, and has gradually increased its indications to include all etiologies of progressive EOS (congenital, neuromuscular and syndromic, associated or not to costal fusions), always with the aim of avoiding or minimizing direct exposure of the spine. There are many entities which can evolve into TIS, especially flabby chest syndrome, constrictive chest wall syndrome with rib fusions and scoliosis, hypoplastic thorax syndrome (which includes Jeune syndrome, achondroplasia, Jarcho-Levin syndrome and Ellis van Creveld syndrome) and progressive scoliosis with a congenital or neurogenic origin without rib anomalies. Syndromic or idiopathic infantile EOS may also be included among these entities if there is constrictive chest wall syndrome, defined by the presence of a windswept deformity of the thorax at the apex of the curve in a computerized tomography scan.41
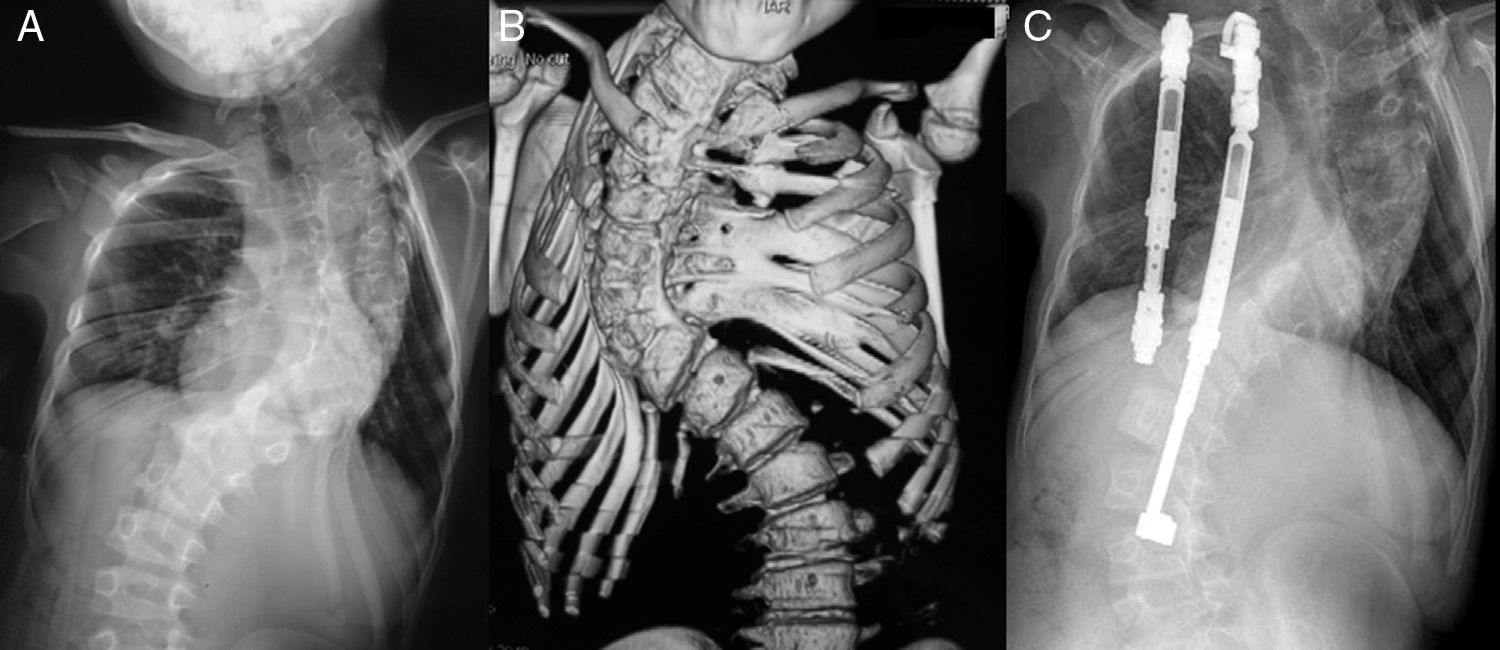
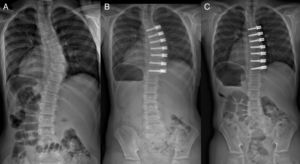
The VEPTR® technique offers the possibility of performing different types of constructs, depending on the diagnosis. In patients with fused ribs and secondary scoliosis, the objective of treatment is to maximize thoracic volume and the symmetry of the deformed thorax through a transversal wedge-shaped thoracotomy opening on the side of the concavity, either through an osteotomy of the fused ribs or by section of the intercostal muscles40 (Fig. 4A–C). The thoracotomy corrects the scoliosis indirectly. Stabilizing the thoracic reconstruction can be accomplished by a costopelvic or costovertebral VEPTR® construct and another costocostal VEPTR® (Fig. 4) which maintains the expansion obtained by the wedge thoracotomy. The implants have to be expanded every 4–6 months. Another alternative is using the VEPTR® implant without an associated thoracotomy. This option can be used in cases where there is a possibility of developing TIS, such as myelodysplasia, where TIS is developed due to the collapse of the thorax in the interior of the abdomen. Placing 2 costopelvic mountings through 3 incisions enables expansion of the thorax using the pelvis as a foundation.
(A) PA radiograph of a 6+9 boy diagnosed with congenital scoliosis in the context of a VATER association with a right thoracic curve of 96°. (B) Three-dimensional CT reconstruction showing multiple vertebral anomalies and costal fusions. (C) Current radiograph. The patient is now 9+5 and after 5 interventions the curve is of 97°.
Campbell et al.40 studied 27 children with congenital scoliosis associated to rib fusions, noting a mean correction of scoliosis of 74°–49°. The rate of complications was 193%, with the most frequent being “asymptomatic” proximal migration of the implant through the ribs. Subsequently, Hasler et al.42 reviewed children with non-congenital EOS and observed a correction of the Cobb angle from 68° (preoperative) to 54° at the end of the follow-up period, with an incidence of 100%, highlighting the existence of wound complications and those associated with the implant. The rate of complications appears to be inversely proportional to the age of patients, without reducing the degree of correction.43 Nevertheless, some authors have found that, despite the significant reduction of the Cobb angle and the consequent increase in the space available for the lung obtained through the use of VEPTR®, objective measurements of lung function do not show an improvement over the expected results.44 Computed tomography scans have shown the absence of correction, as well as a stabilization of the deformity only in the transverse plane expected from the TIS. On the other hand, other authors have found an improvement in lung function.45
The use of VEPTR® seems relatively safe, with a low mortality even among patients with greater involvement and worse prognosis.45 However, compared to double growing rods, VEPTR® presents a higher rate of complications and an undesirable increase of kyphosis.46
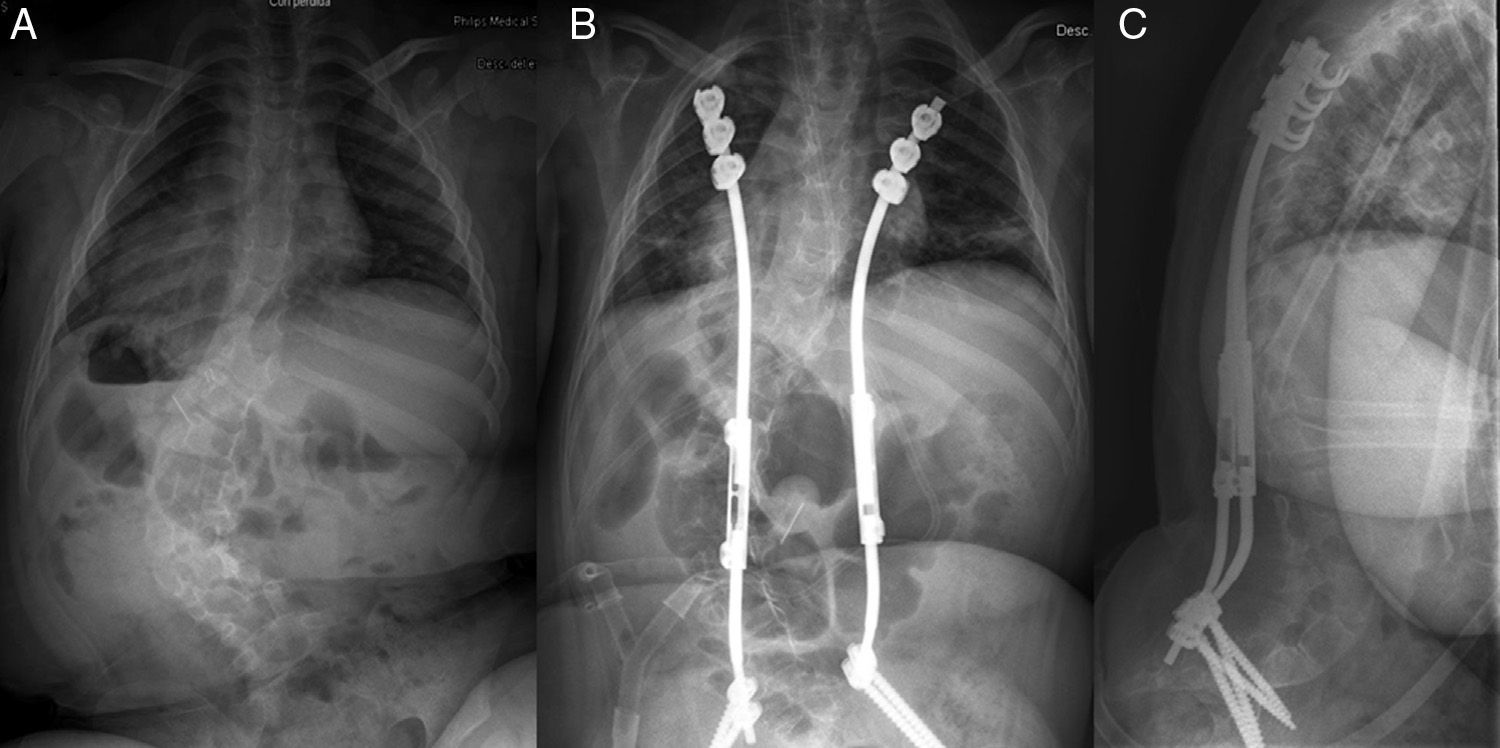
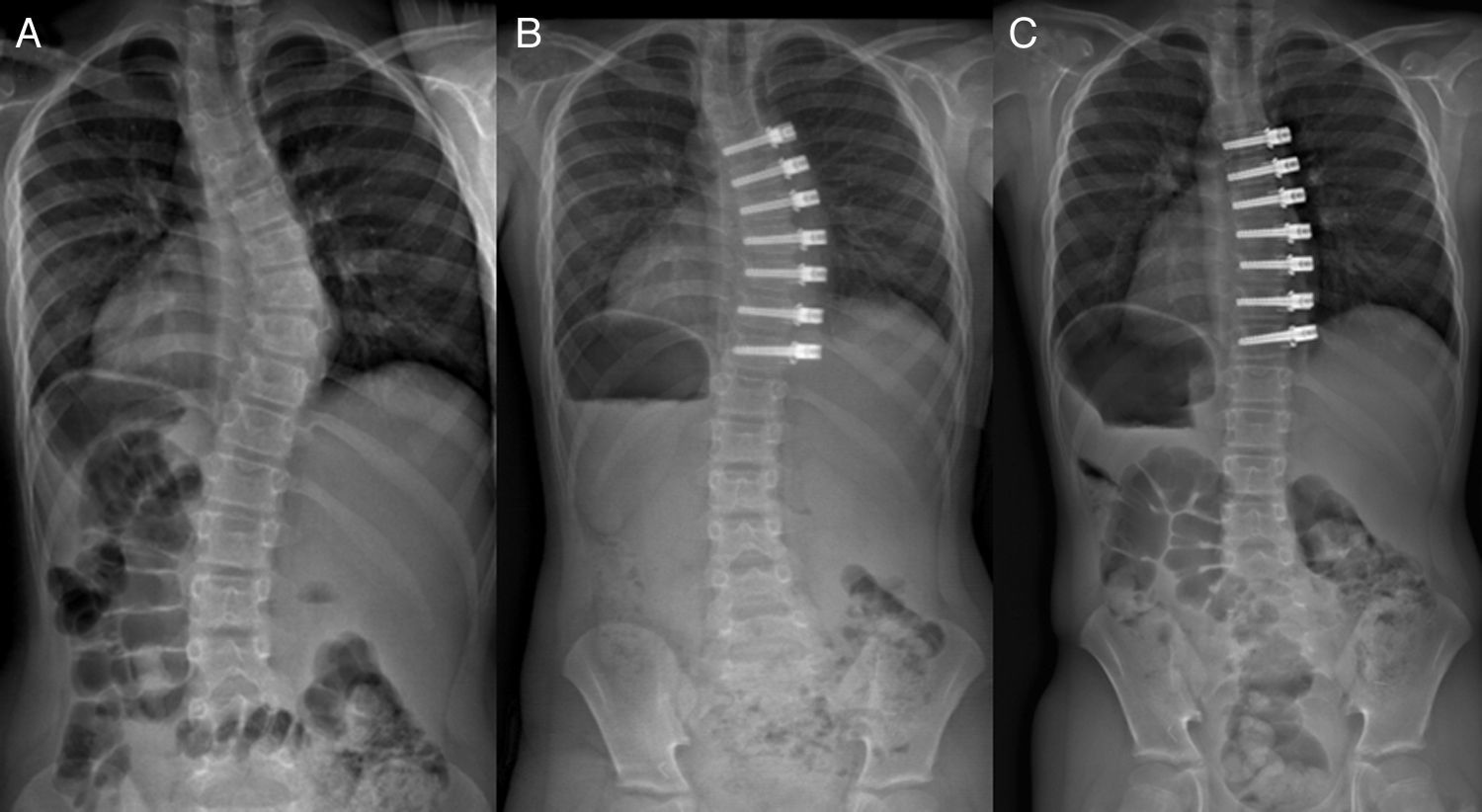
Hybrid growing rodsIt has been shown that the current procedure of fusion of the superior thorax, with proximal anchors in growing rods, affects lung function negatively.4 Thus, in order to avoid this fusion, hybrid systems use conventional hooks anchored in the ribs as proximal anchors. As a distal anchor they use a construct with pedicular screws or hooks, and can even use a pelvic construct (Fig. 5A–C). Coverage of the hooks by soft tissues is usually best when they are placed in the ribs, rather than anchored in the vertebrae. The hooks should be placed on the ribs close to the transverse process, thus being located in the space between the column and the scapula.47 One of the theoretical advantages of these assemblies is that the mobility of the rib-hook interface, as well as of the costovertebral joint, could perhaps reduce the risk of autofusion. In a multicenter study, Skaggs et al.48 have shown that bilateral hybrid growing rods generate a mean T1–S1 growth of 1.2cm/year, which is comparable to that observed with double growing rods and superior to that achieved with VEPTR®. In a comparative study with similar patient populations, hybrid instrumentation presented a complication rate of 0.86/patient, double growing rods of 2.3/patient and VEPTR® of 2.37/patient.38
(A) PA radiograph of a 6+1 girl diagnosed with early onset scoliosis of a neuromuscular origin and with a left thoracolumbar curve of 80°. (B) After the proximal hooks came loose several times we chose to convert the construct into a hybrid system. (C) The sagittal profile is correctly conserved.
The theoretical advantage of a spinal implant based on distraction whose elongation does not require a surgical approach is the reduction of the multiple complications associated with surgery, such as infection, coverage defects, etc. Furthermore, the application of a more constant and frequent force should supposedly improve the mechanics of correction and growth.
Phenix® and MAGEC® implants allow growth by a remote control. They can be especially useful in children with comorbidities, in whom the multiple surgical procedures required by conventional distraction systems represent an excessive risk.
Preliminary results49,50 are very promising, as it has been observed that this is a safe and effective growth-preserving technique which also associates a considerably lower rate of complications. Using double stems significantly improves the initial correction and spinal length gained with distraction procedures.50 Nevertheless, its disadvantages include an inability to mold the implants in the sagittal plane and their relatively large size.
Guided growthThese techniques correct spinal deformity through the anchoring of multiple vertebrae, typically including the apical vertebra, with 2–4 bars. Correction is achieved through translational forces acting both at the time of the initial surgery and subsequently through the growth of the vertebral column, as it does not employ rigid anchors (sliding screws or sublaminar wires). One advantage of these procedures is that they do not require repeated distractions.
These techniques can be considered in cases of progressive deformities when treatment with a cast or brace has failed or is contraindicated. Since they do not require multiple distractions, along with their corresponding anesthesias, they seem to be a better choice than distraction techniques in children with significant medical comorbidities.
Modern Luque TrolleyThe classical concept of the Luque Trolley51 is a construct on which a number of sublaminar wires are placed through minimal subperiosteal dissection. Next, these wires are anchored to conventional bars, thus achieving correction of the scoliosis at the time of surgery, whilst also allowing the column to continue growing longitudinally as the wires slide over the bars.
Initially, these techniques had high rates of complications for the management of patients with EOS.52,53 This circumstance, along with the development of new surgical options based on distraction, meant that their use became secondary. However, the observation of numerous complications associated with the latter techniques in relation to the multiple elongation procedures required has led to a new evolution in the concept of guided growth, especially with the emergence of new versions of the Luque Trolley.
Recently, Mehdian et al.54 have described segmental self-growing rod constructs enabling a segmental correction of the deformity in both planes, thus avoiding the morbidity associated with multiple reoperations, adjustments of implants and premature end of spinal growth. In a study of 16 patients who suffered EOS with a neuromuscular origin, they observed a substantial improvement of the curve from a mean preoperative value of 68.9° to a mean postoperative value of 9.6°, as well as a reduction in kyphosis (from a mean of 62° to 28.5°). The mean growth of the column was 1.034mm, with a mean follow-up period of 3.2 years (79% of the expected growth). Complications included a superficial infection and a loss of distal fixation.
Shilla techniqueThe Shilla technique, developed by Richard McCarthy, is based on a system of stems and conventional pedicular screws, except that the proximal and distal pedicular screws do not fix the bar and allow it to slide. A construct and fusion of 3–4 vertebrae using pedicular screws fixed to the stems is established at the level of the apex of the deformity. Theoretically, correction and stabilization of the most deformed apical segment generates less stress on the anchor points at the ends of the assembly. Control of the sagittal plane is done by the molding of the bars prior to their placement. Between 4 and 6 “sliding” pedicular screws are placed at each of these ends (Fig. 6A–C). These screws are implanted without subperiosteal exposure in order to reduce the risk of unintentional fusion in these proximal and distal segments. It is essential to have a good fluoroscopic technique and specific material, because placement of the proximal and distal anchor screws is not aided by anatomical references. Stems are left long at the ends in order to allow them to slide through the screws as the column grows. The sagittal profile is preserved and the anchor screws slide cranially and caudally on the double rods as the patient grows.
(A) PA radiograph of a patient with idiopathic, early onset scoliosis. (B) Postoperative radiograph showing the correction achieved. (C) The last follow-up image showed how the correction was largely maintained and confirmed the growth of the vertebral column by sliding of the rods on the sliding screws. (Courtesy of Dr. David Skaggs).
McCarthy and McCullough55 presented their results with 40 patients who underwent this technique after 5 years of follow-up and pointed to the preservation of spinal growth and an increase of the space available for the lung, requiring fewer surgeries than expected with conventional techniques based on distraction and with an acceptable number of complications.
Surgical techniques based on compression of the convexitySystems based on compression correct the spinal deformity by applying a compressive force on the convexity of the curve, causing the inhibition of growth in this region. This compressive force may be applied intraoperatively at the time of implant placement, as well as over time as a result of longitudinal growth of terminal growth plates restrained by the spinal implants. Therefore, these techniques based on the Hueter-Volkman law, would correct scoliosis through the growth of the concavity. Classically, inhibition of the growth of the convexity was performed through an anterior and posterior hemiepiphysiodesis technique,56–58 although this procedure was primarily used for congenital scoliosis. More recently, posterior hemiepiphysiodesis with pedicular screws59 has generated interest, as have alloy staples with shape memory,60,61 tethers62–64 and transpedicular modulation of growth of the neurocentral joint.65–67
Hemiepiphysiodesis of the convexityAnterior and posterior hemiepiphysiodesis of the convexity is a known surgical alternative in the treatment of congenital scoliosis.56–58 It has the advantage of being a single procedure and the drawback of requiring a double anterior and posterior approach. Furthermore, the result can sometimes be unpredictable. Hemiepiphysiodesis of the convexity with pedicular screws59 has the advantage of avoiding the anterior procedure and postoperative immobilization. Moreover, it can be applied from 15 months of age. It also allows acute correction of the deformity and the subsequent modulation of growth it exerts can contribute to the correction.
Anterior alloy staples with shape memoryCandidates for this technique must have at least 1 year of growth and a deformity susceptible of treatment with a brace. According to Betz et al., the thoracic and lumbar curves must be <45° with a minimal rotary component and flexible to <20°. The sagittal thoracic curve must be <40°.61
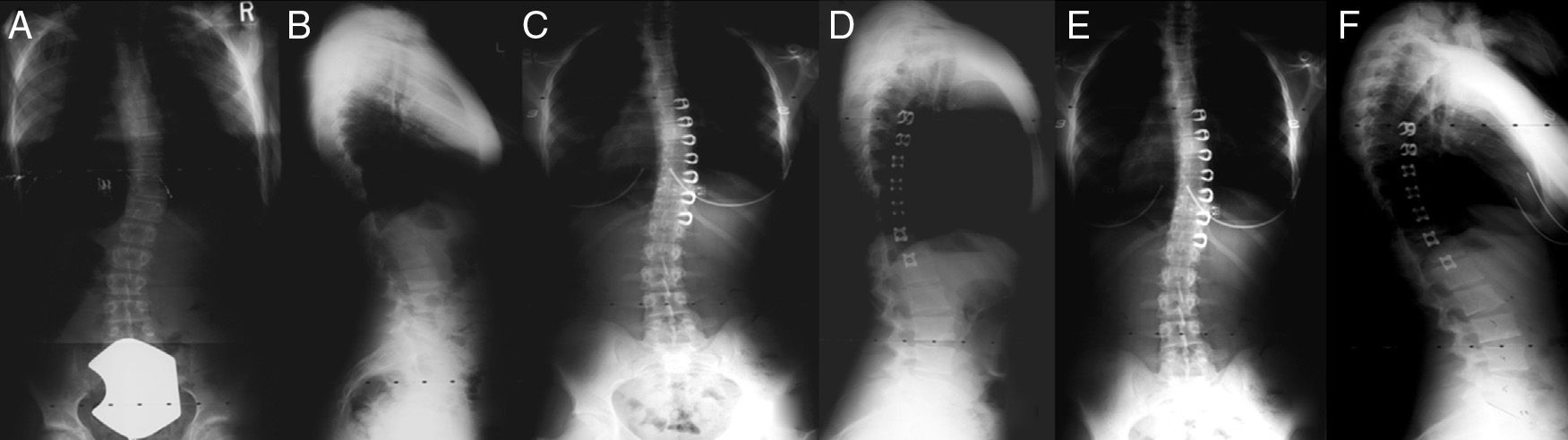
Problems with loss of anchoring described with the initial vertebral staples68 seem to have been resolved through the use of nitinol staples. When these staples are cooled, their legs adopt a straight shape; however, once they are within the bone and warmed by body temperature, they adopt a “C” shape and become stabilized (Fig. 7A–F). Betz et al61 reviewed 28 patients with curves between 20° and 45°, and a Risser sign of 0 or 1 who were operated on using the technique with vertebral nitinol staples. In thoracic curves, out of those which were less than 35° at the time of placement of the staples, 78% became stabilized or improved. Out of those curves above this figure, 75% improved. A success rate of 75% was achieved in patients under 10 years of age with thoracic curves of any magnitude. The same study also found that the use of the staples seemed to have a positive effect on the sagittal profile in patients with kyphosis. Complications included the rupture of a previously undetected diaphragmatic hernia, hypercorrection of the curve in 1 case, atelectasis and 1 case of superior mesenteric artery syndrome.
(A) PA radiograph of a 12+0 patient diagnosed with idiopathic scoliosis with a right thoracic curve of 29°. (B) Lateral radiograph with a thoracic kyphosis of 15°. (C) Postoperative radiograph with an initial correction up to 19°. (D) Lateral projection showing the correct placement of the staples. (E) PA projection after 4+1 from the surgery with a curve of 17°. (F) Lateral projection showing a kyphosis of 28°. (Courtesy of Dr. Randal Betz).
The tether consists of a flexible cord attached to different vertebrae, typically by screws. Supposedly, like staples, it corrects the curve by inhibiting the growth of the convexity, but it uses flexible connections between the vertebral anchor points. Theoretically, it is less likely to injure the intervertebral discs compared to rigid devices. The conservation of the disks has been observed in animal models,62 but although both the tether and the staples cause chemical, cellular and vascular changes in the disks and vertebral endplates,63 the implications of these changes are not currently known.
Recently, Braun64 compared alloy staples with shape memory with the anterolateral tether and found a better initial correction and subsequent control of the progression of the curve with the use of the tether.
Experimental therapiesA number of techniques for the treatment of various etiologies of scoliosis by methods which preserve the growth of the spine are currently being investigated. Asymmetric epiphysiodesis of the neurocentral synchondroses has shown promising results in experimental studies.65–67 Shortening and elongation of the ribs has also been performed experimentally and clinically.69,70
ConclusionsEOS continues to pose a challenge for orthopedic surgeons due to the need to act early because of the potential for long-term morbidity of this entity. Nonsurgical options, including derotatory casts, can be used to “buy time” in young patients (4–5 years old) before a surgical intervention is required. In very young patients (under 2 years of age) they have the potential to correct the deformity permanently. Non-fusion techniques, including double growing rods and VEPTR®, preserve spinal growth but require multiple elongation procedures and entail a relatively high risk of complications, as well as a progressively lower elongation rate with each new elongation. Hybrid systems are considered as the best option for patients who require a proximal anchor with a low profile. Patients who are not eligible for repeated elongations due to significant comorbidities may be candidates for the Shilla technique or the Luque Trolley. Growth modulation using staples with shape memory or tethers is promising in minor curves with an idiopathic etiology, although further work is required to define their specific indications (Fig. 8).
Level of evidenceLevel of evidence V.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Farrington DM, Tatay-Díaz Á. Escoliosis de aparición precoz. ¿Qué opciones tengo? Rev Esp Cir Ortop Traumatol. 2013;57:259–370.